SMALL INTESTINE
Dr. ZAID MUWAFAQ AL-HAMIDMRCS England(UK), FJMC Jordan, HSM SURGERY Jordan, MBChB Mosul
Specialist Laparoscopic SurgeonSMALL BOWEL OBSTRUCTION
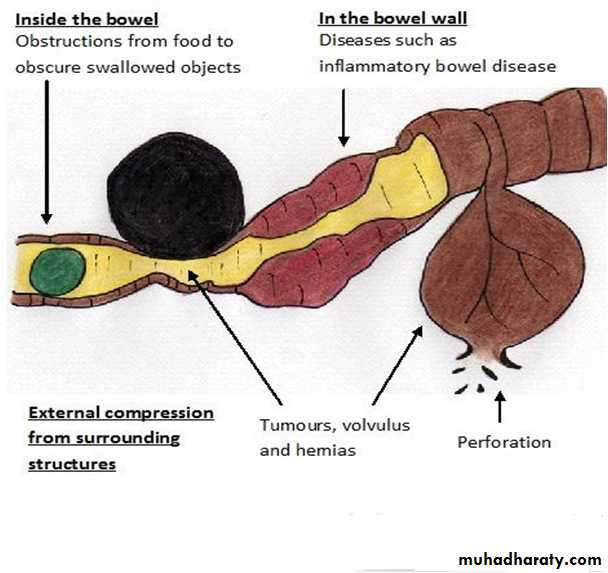
Mechanical small bowel obstruction is the most frequently encountered surgical disorder of the small intestine.Aetiology:
1. Intraluminal (e.g., foreign bodies, gallstones, or meconium)2. Intramural (e.g., tumors, Crohn’s disease–associated inflammatory Strictures, Diverticulitis, Meckel’s diverticulum, Hematoma), Congenital abnormalities (e.g., webs, duplications, and malrotation)
3. Extrinsic (e.g., adhesions, hernias(ext. or internal), or carcinomatosis or local invasion by intraabdominal malig.) Volvulus, Intussusception
Intra-abdominal adhesions related to prior abdominal surgery account for up to 75% of cases of small bowel obstruction.
Less prevalent etiologies for small bowel obstruction include hernias, malignant bowel obstruction(extrinsic compression or invasion by advanced malignancies arising in organs other than the small bowel), and Crohn’s disease.
Pathophysiology
Obstruction gas and fluid accumulate proximal to the site of obstruction the intestinal activity increases to overcome the obstruction colicky pain .gas swallowed air, some is produced within the intestine.
fluid swallowed liquids and gastrointestinal secretions (obstruction stimulates intestinal epithelial water secretion).
More gas and fluid accumulation the bowel distends
intraluminal and intramural pressures riseThe intestinal motility reduced , lumine small bowel (sterile) organisms grows Translocation of bacteria
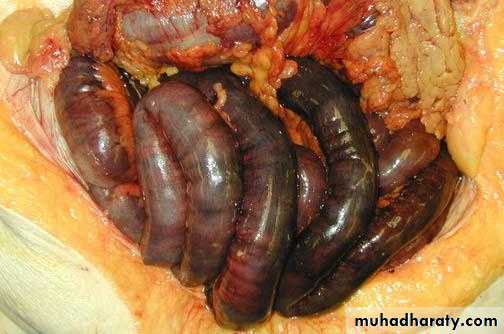
intramural pressure high enough intestinal ischemia , necrosis strangulated bowel obstruction.
partial small bowel obstruction
only a portion of the intestinal lumen is occluded.
Progression is slower .
strangulation is less likely.
Continued passage of flatus and/or stool beyond 6 to 12 hours after onset of symptoms is characteristic of partial obstruction
closed-loop obstruction in which a segment of intestine is obstructed both proximally and distally (e.g., with volvulus) leading to a rapid rise in luminal pressure and a rapid progression to strangulation.
Clinical Presentation
The symptoms of small bowel obstruction are1- colicky abdominal pain. Is the first symptom ,sudden and severe in umbilical region . Continuous sever pain suggestive of strangulation.
2- nausea, vomiting
Vomiting is a more prominent symptom with proximal obstructions than distal.
The vomitus usually bile stained and when it is more feculent, suggesting a more established obstruction.
3- obstipation(absolute constipation)
4-abdominal distention, which is most pronounced if the site of obstruction is in the distal ileum and may be absent if the site of obstruction is in the proximal small
intestine.
5- Bowel sounds may be hyperactive initially, but in late stages , minimal bowel sounds may be heard.
The patient is dehydrated
Laboratory findings reflect intravascular volume depletion and consist of hemoconcentration and electrolyte abnormalities. Mild leukocytosis is common.
1- abdominal pain often disproportionate to the degree of abdominal findings,
2- tachycardia
3- localized abdominal tenderness
4- fever
5- marked leukocytosis
6- acidosis
Any of these findings should alert the clinician to the possibility of strangulation and need for early surgical intervention.
Features of strangulated obstruction include:
1- History : prior abdominal operations
abdominal disorders (e.g., intra-abdominal cancer or inflammatory bowel disease)2-Examination, for hernias (particularly in the inguinal and femoral regions)and the presence of abdominal scar.
Signs of dehydration, tachycardia , hypotension, may be fever(in strang.)
3- Radiological:
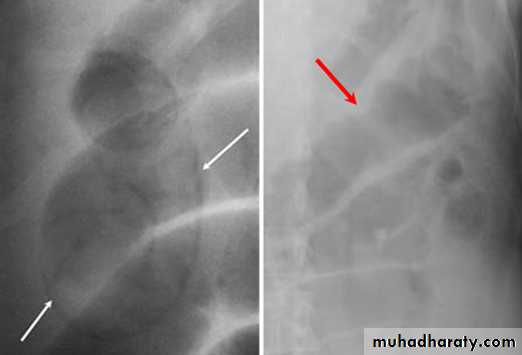
- upright films: dilated small bowel loops (>3 cm in diameter), air-fluid levels, and a paucity of air in the colon.
- Computed tomography (CT) scanning :
^ transition zone
^ proximal dilation of bowel
^ distal decompression of bowel
^ intraluminal contrast that does not pass beyond the transition zone, and a colon containing little gas or fluid.
^ Strangulation, closed loop obstruction and the etiology of obstruction can be suggested.
Diagnosis
4- Complete blood count (hemoconcentration,leukocytosis)
serum electrolytes(vomiting of intestinal contents result in hypokalemia, ischemia and renal failure result in hyperkalemia)
renal function test (bl.urea, serum creatinine)
Small bowel obstruction
-The dilated bowel loops centrally located and lie transversely.-No/minimal gas is seen in the colon.
-valvulae conniventes,which completely pass across the width of the bowel
-ladder pattern
Multiple air fluid level, small and centrally located.
-Dilated loops of bowel
-periphery located.
-Larger bowel diameter
-Huastration (incomplete line)
-longer length airfuid level , less in number
Large bowel obstruction
1- NPO
2- fluid resuscitation, Isotonic fluid should be given intravenously3- Nasogastric (NG) tube: The stomach should be continuously evacuated of air and fluid to decreases nausea, distention, and the risk of vomiting and aspiration.
4- an indwelling bladder catheter may be placed to monitor urine output.
5- Central venous or pulmonary artery catheter monitoring may be necessary to assist with fluid management in patients with underlying cardiac disease and severe dehydration.
6- Broad-spectrum antibiotics ???
Therapy
close observation and serial exams.
“the sun should never rise and set on a complete bowel obstruction.”If there is any evidence of closed-loop obstruction or intestinal ischemia , surgical exploration should be performed.
Conservative Therapy is commonly recommended for:
1. Partial small bowel obstruction(for 48 hours)
2. Obstruction occurring in the early postoperative period (2-3 weeks)
3. Intestinal obstruction due to Crohn’s disease
4. Carcinomatosis
All those periods of conservative therapy should be coupled with close observation and if signs of complete obstruction or intestinal ischemia occurs , urgent surgical exploration should be performed.
The operative procedure performed for small bowel obstruction varies according to the etiology of the obstruction.
Adhesions are lysed(adhesiolysis)
Tumors are resected,
Hernias are reduced and repaired.
Criteria suggesting viability of small intestine are
normal color, peristalsis, marginal arterial pulsations.
Regardless of the etiology, the affected intestine should be examined.
1- Nonviable bowel resected.
2- Viable healthy bowel left intact.
3- Questionable viability: should be packed with gauze(socked with warm saline) and rexamined for viability. If viability is questionable and the patient is hemodynamically stable:
- short lengths of bowel of questionable viability should be resected and primary anastomosis.
- long length of the intestine is in question, should be left intact and the patient re-explored in 24 to 48 hours in a “secondlook” operation. At that time, definitive resection of nonviable bowel is completed.
Prevention of postoperative adhesion:
1- good surgical technique.2- careful handling of tissue
3- minimal use and exposure of peritoneum to foreign bodies.
4- use of laparoscopy rather than open surgery.
Prevention
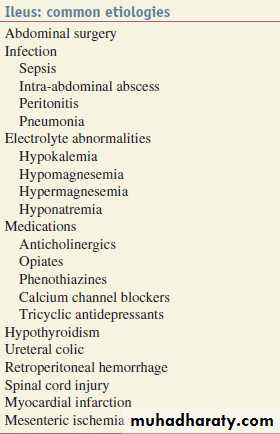
Paralytic ileus
failure of transmission of peristaltic waves secondary to neuromuscular failure with absence of a lesion-causing mechanical obstruction.
The resultant stasis leads to accumulation of fluid and gas within the bowel, with associated distension, vomiting, absence of bowel sounds and absolute constipation.
Ileus and intestinal pseudo-obstruction
Ileus is a temporary motility disorder that is reversed with time as the inciting factor is corrected.
Chronic intestinal pseudo-obstruction comprises a spectrum of specific disorders associated with irreversible intestinal dysmotility.
Following celiotomy
– small bowel- 24h, stomach- 48h, colon- 3-5d
The most frequently encountered factors are :
Abdominal operationsinfection
inflammation,
Electrolyte-abnormalities
drugs
Clinical Presentation
Paralytic ileus takes on a clinical significance if, 72 hours after laparotomy:• there has been no return of bowel sounds on auscultation;
• there has been no passage of flatus.
Abdominal distension becomes more marked and tympanitic.
Colicky pain is not a feature.
Distension increases pain from the abdominal wound.
In the absence of gastric aspiration, effortless vomiting may occur.
Radiologically, the abdomen shows gas-filled loops of intestine with multiple fluid levels (if an erect film is felt necessary).
Management
Paralytic ileus is managed with :
1- Nasogastric suction
2- NPO
3- Electrolyte balance must be maintained.
4- If a primary cause is identified, this must be treated.
• There is no place for the routine use of peristaltic stimulants.
• If paralytic ileus is prolonged, CT will demonstrate any intraabdominal sepsis or mechanical obstruction --laparotomy.
Small intestinal pseudo-obstruction
This condition may be primary (i.e. idiopathic or associated with familial visceral myopathy)or secondary.
The clinical picture consists of recurrent subacute obstruction.
The diagnosis is made by the exclusion of a mechanical cause.
Treatment consists of initial correction of any underlying disorder.
Metoclopramide and erythromycin may be of use.
Special types of intestinal mechanical obstruction
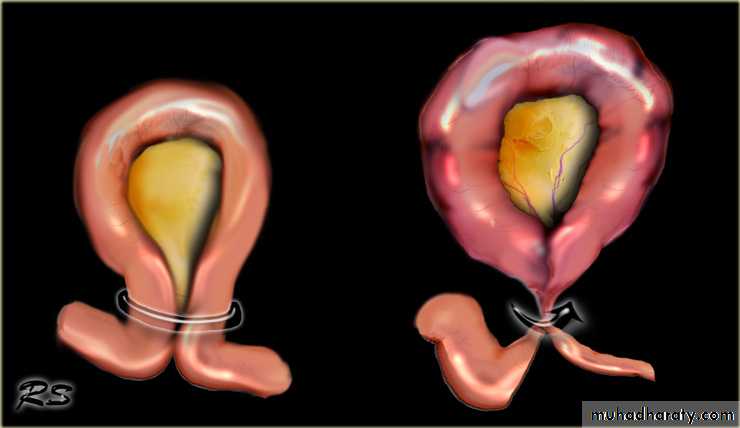
Volvulus
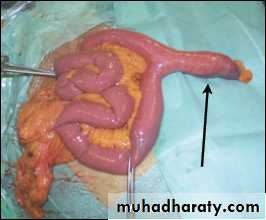
A volvulus is a twisting or axial rotation of a portion of bowel about its mesentery. The rotation causes obstruction to the lumen (>180° torsion) and if tight enough also causes vascular occlusion in the mesentery (>360° torsion).Bacterial fermentation adds to the distention and increasing intraluminal pressure impairs capillary perfusion. Mesenteric veins become obstructed as a result of the mechanical twisting and thrombosis results and contributes to the ischaemia.
Volvuli may be primary or secondary.
The primary occurs secondary to congenital malrotation of the gut, abnormal mesenteric attachments or congenital bands. Examples include volvulus neonatorum, caecal volvulus and sigmoid volvulus.A secondary volvulus, which is the more common variety, is due to rotation of a segment of bowel around an acquired adhesion or stoma
Treatment :
Resuscitation(NPO, IV fluid, NG tube , antibiotic)Surgery
untwist the bowel
resect non viable bowel and anastamose.
Volvulus neonatorum
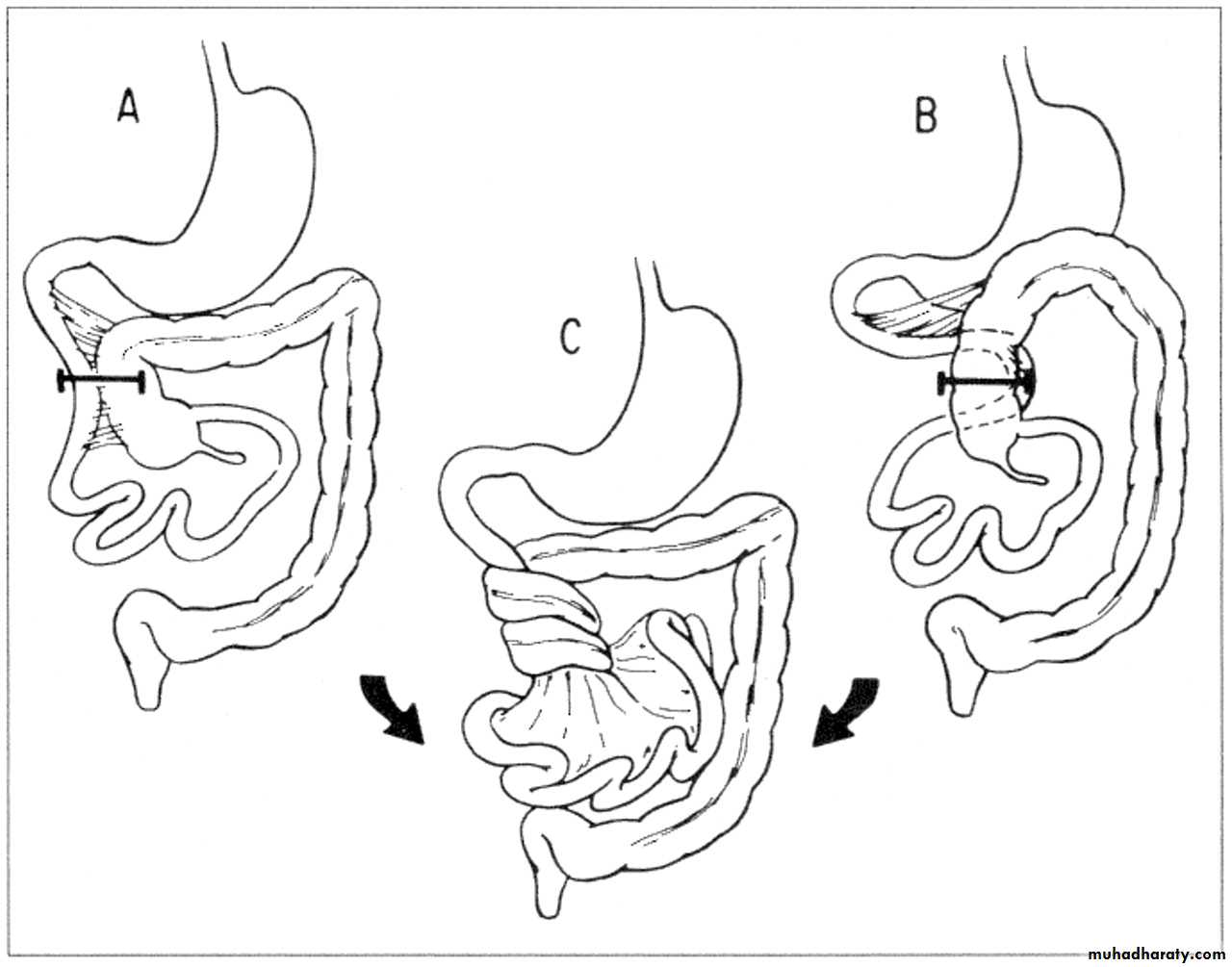
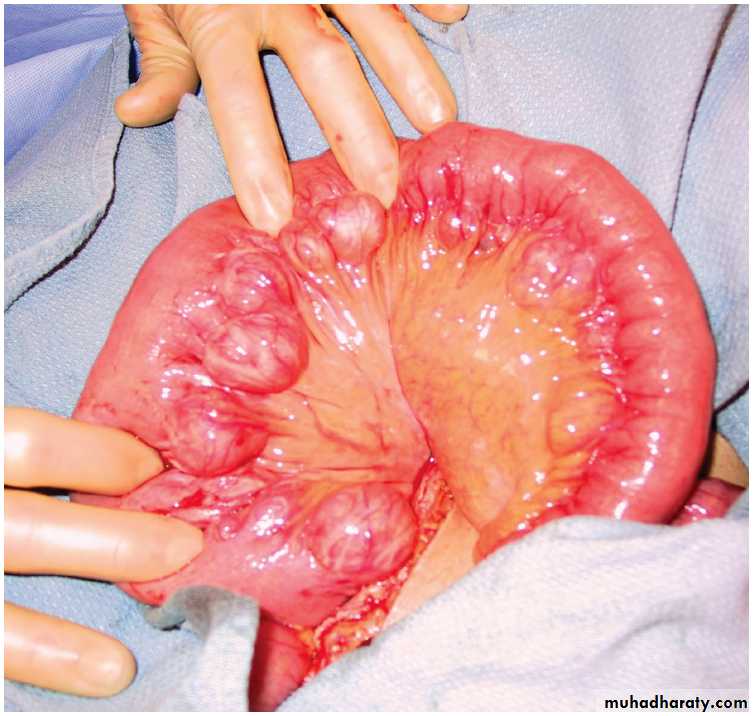
This occurs secondary to intestinal malrotationand is potentially catastrophic.less than one year old with bilious vomitingurgent surgical exloration(ladd procedure)Acute intussusception
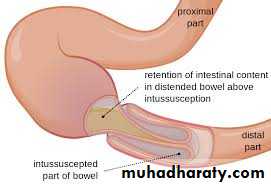
one portion of the gut invaginates into an immediately adjacent segment.Most in children, peak five and ten months.
Causes:
- idiopathic(most common)(associated upper respiratory tract infection or gastroenteritis may precede the condition) (hyperplasia of Peyer’s patches in the terminal ileum )
leading point could be Meckel’s diverticulum, polyp, duplication, Henoch–Schönlein purpura or appendix occur in older age.
Adult cases are invariably associated with a lead point, which is usually a polyp (e.g. Peutz–Jeghers syndrome), a submucosal lipoma or other tumour.
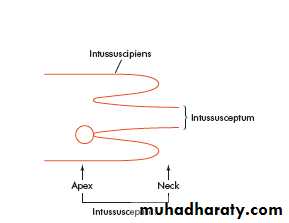
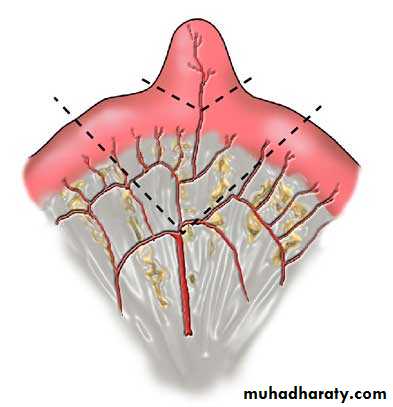
Pathology
is composed of three parts :• the entering or inner tube (intussusceptum);
• the returning or middle tube;• the sheath or outer tube (intussuscipiens).
The part that advances is the apex
the mass is the intussusception
the neck is the junction of the entering layer with the mass.
In most children, the intussusception is ileocolic.
In adults, colocolic intussusception is more common .
Paroxysms of crampy abdominal pain (screaming)and intermittent vomiting.
Between attacks, the infant may act normally, but as symptoms progress, increasing lethargy develops.Bloody mucus (“red currant jelly ” stool) may be passed per rectum.
if reduction is not accomplished, gangrene of the intussusceptum occurs, and perforation Peritonitis
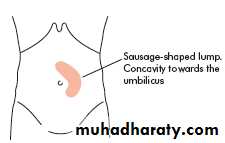
Clinical picture:
Physical examination:
- mass in the right upperquadrant or epigastrium
- absence of bowel
in the right lower quadrant (Dance’s sign).
Rarely, the apex of intussusception may pass the colon to protrude through anus
The mass may be seen on plain abdominal x-ray/US/CT (target sign) but is more easily demonstrated on air or contrast enema.
Treatment
NPO, IV fluid, IV antibioticsabsence of peritonitis radiographic(pneumatic) reduction(air/barium enema is diagnostic and curative)
Peritonitis or systemically ill child, ileoileal, pathological leading point urgent laparotomy
Reduction
(by gentle distal pressure, where the intussusceptum
is gently milked out of the intussuscipiens)
+ Non viable bowel resected
and primary anastamosis
+ Appendectomy(for ileocolic)
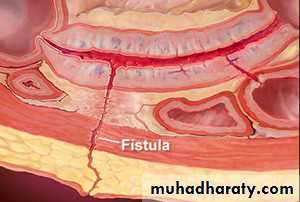
A fistula is defined as an abnormal communication between two epithelialized surfaces.
1- internal fistula : The communication occurs between two parts of the GI tract or adjacent organs (e.g., enterocolonic fistula or colovesicular fistula).2- An external fistula (e.g., enterocutaneous fistula or rectovaginal fistula) involves the skin or another external surface epithelium.
low-output fistulas : Enterocutaneous fistulas that drain less than 500 mL of fluid per day.
high-output fistulas that drain more than 500 mL of fluid per day .
INTESTINAL FISTULAS
1- Over 80% iatrogenic: complications of enterotomies or intestinal anastomotic dehiscences( inadvertent small bowel injury at the time of abdominal closure).
2- Trauma: gunshot wounds, stabbing or motor vehicle accident.
3- Spontaneously without antecedent iatrogenic injury are caused by:
-Crohn’s disease
- Cancer.
- Radiotherapy.
Etiology
Iatrogenic enterocutaneous fistulas occurs between fifth and tenth postoperative days.
1- Fever, leukocytosis.2- prolonged ileus.
3- abdominal tenderness.
4- wound infection are the initial signs.
The diagnosis becomes obvious when
drainage of enteric material through the abdominal wound or through existing drains occurs.
These fistulas are often associated with intra-abdominal abscesses.
Low-resistance enteroenteric fistulasmalabsorption.
Enterovesical fistulas recurrent urinary tract infections.
Enterocutaneous fistulas are irritating to the skin and cause excoriation.
High-output fistulas originating from the proximal small intestine dehydration, electrolyte abnormalities, and malnutrition.
Clinical Presentation
1. Stabilization.
Fluid and electrolyte resuscitation .Nutrition (TPN), parenteral route initially.
Sepsis is controlled with antibiotics and drainage of abscesses.
The skin is protected from the fistula effluent with ostomy appliances.
The somatostatin analogue octreotide??
2. Investigation. The anatomy of the fistula is defined using the CT scanning, or fistulogram
3. Definitive management: if 2-3 months of conservative therapy fails then definitive surgical procedure should be performed .(Resection of the fistula tract + resection of intestinal segment from which the fistul arise)
4. Rehabilitation.
Management
Over 50% of intestinal fistulas close spontaneously.
Factors inhibiting spontaneous closure(FRIENDS)Fistulas have the potential to close spontaneously. Causes of failure to close include:
1-malnutrition, immune suppression , steroids.
2- sepsis
3- inflammatory bowel disease(crohn’s)
4- cancer
5- radiation
6- obstruction of the intestine distal to the origin of the fistula
7- foreign bodies,
Gastric, Duodenal fistula, High output, short fistulous tract (<2 cm) and epithelialization of the fistula tract are less likely to closespontaneously.
Outcome
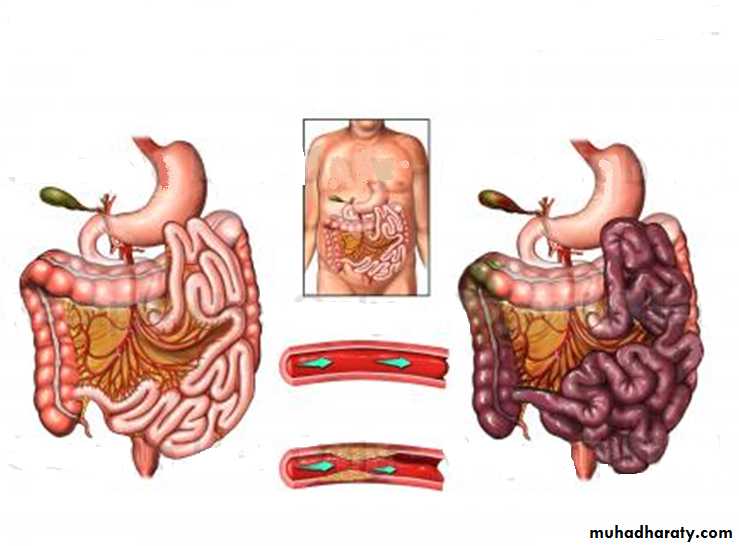
two distinct clinical syndromes:
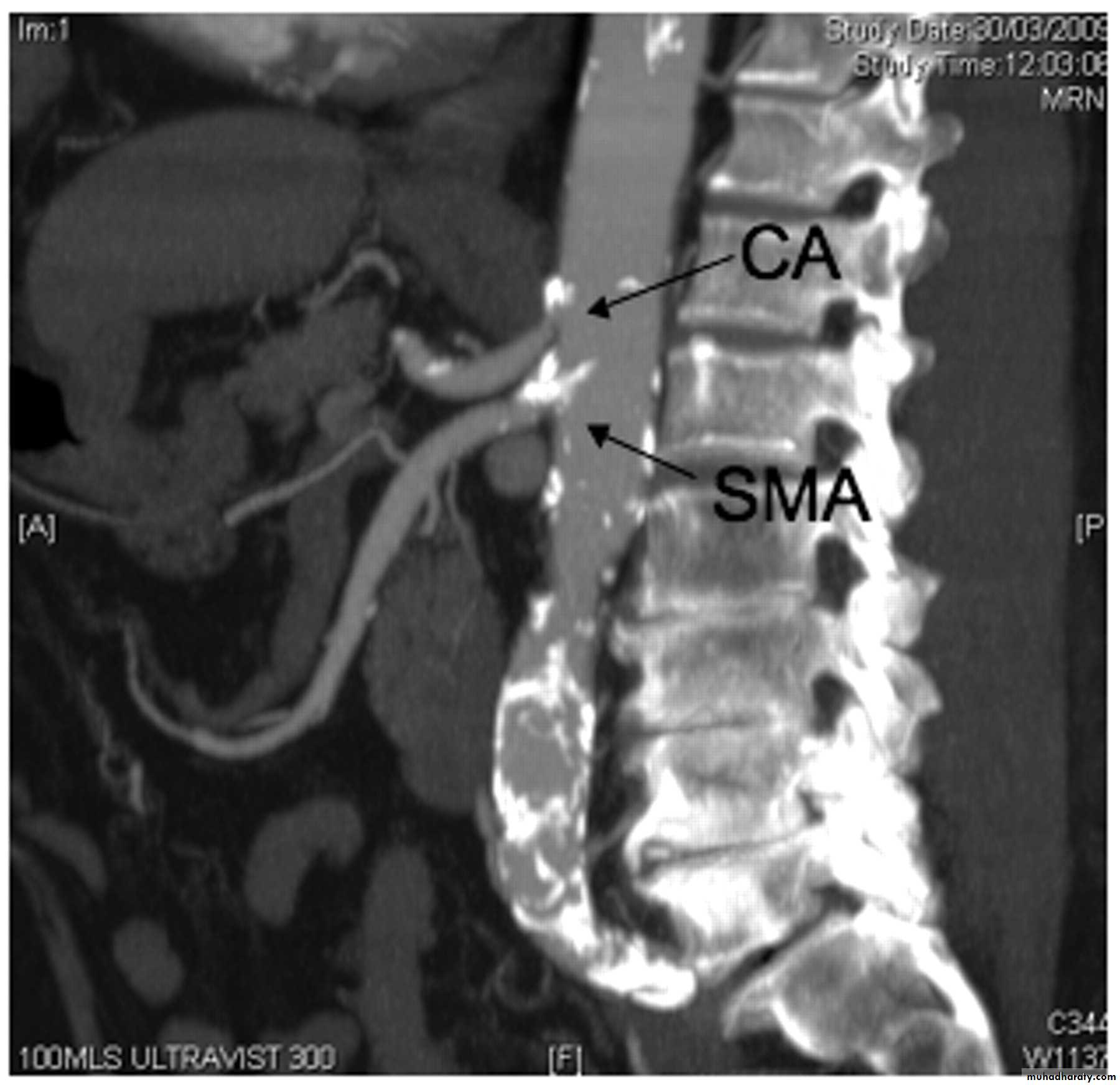
1- acute mesenteric ischemia (embolus or thrombus)2- chronic mesenteric ischemia.
Four distinct pathophysiologic mechanisms can lead to
acute mesenteric ischemia:
1. Arterial embolus(acute): most common, (left atrial(AF) or ventricular thrombi or valvular lesions), occlude the superior mesenteric artery(mid , distal).
2. Arterial thrombosis(acute or chronic): (proximal) mesenteric arteries.
3. Vasospasm (also known as nonocclusive mesenteric ischemia[NOMI]) , result of vasospasm from vasospastic drugs.
4. Venous thrombosis: 10% of cases of acute mesenteric ischemia and involved the superior mesenteric vein.
MESENTERIC ISCHEMIA
Sudden onset of Severe mid-abdomen pain, out of proportion to the degree of tenderness on examination, is the hallmark of acute mesenteric ischemia.
in patients with underlying cardiac or atherosclerotic disease
Associated symptoms can include nausea, vomiting, and diarrhea.
Physical findings are characteristically absent early in the course of ischemia.
Fever, passage of bloody stools, Diffuse abdominal tenderness, rebound, and rigidity are late signs and usually indicate bowel infarction and necrosis.
Acute mesenteric ischemia
presents insidiously(because of collateral).
Postprandial abdominal pain is the most prevalent symptom, (“food fear”)
weight loss.
Persistent nausea and occasionally diarrhea may coexist
Usually misdiagnosed.
Chronic mesenteric venous thrombosis
asymptomatic, because of extensive collateral venous drainage.
incidental finding on imaging studies.
some patients present with bleeding from esophagogastric varices.
Chronic mesenteric ischemia
an elderly + multiple comorbidities + digitalis or vasoconstrictor such as epinephrine.
70% abdominal pain.30% no abdominal pain , progressive abdominal distention , acidosis impending infarction.
Nonocclusive mesenteric ischemia
Laboratory evaluation is not sensitive not specific
1-hemoconcentration and leukocytosis.2-Metabolic acidosis.
3-Elevated serum amylase.
4- in the late stages :increased lactate levels, hyperkalemia, and azotemia.
Diagnosis
Plain abdominal radiographs
- to exclude other causes of abdominal pain
-Pneumoperitoneium , pneumatosis intestinalis, and gas in the portal vein may indicate infarcted bowel.
-ileus with a gasless abdomen.
Duplex ultrasonography
CTA and MRA
Mesenteric arteriography
(definitive diagnosis)
Has therapeutic role,
infusion of vasodilating agents,
such as papaverine, thrombolytic??
chronic intestinal angina develop acute abdomen and peritonitis immediate exploration + assessment of intestinal viability and vascular reconstruction is the best choice.
(arteriography is time consuming)
IV fluid resuscitation
systemic anticoagulation with heparinSignificant metabolic acidosis not responding to fluid resuscitation should be corrected with sodium bicarbonate.
A central venous catheter and Foley catheter
antibiotics
immediate surgical exploration, avoiding the delay required to perform an arteriogram
Acute Embolic Mesenteric Ischemia.
Surgery :
Arteriotomy+ embolectomy+ an assessment of intestinal viability+ nonviable bowel must be resected.
A second-look procedure(24 to 48 hr)in many patients to reassess the remaining bowel viability.
Same preoperative management
Surgery: SMA bypass graft may originate from either the aorta or iliac arteryChronic Mesenteric Ischemia.
Endovascular Balloon dilatation or stent placement
Surgical: transaortic endarterectomy or mesenteric artery bypass.
Acute Thrombotic Mesenteric Ischemia
mesenteric arterial catheterization and infusion of vasodilatory agents, such as tolazoline or papaverine.
cessation of other vasoconstricting agents
intravenous heparin
Surgical exploration is indicated if the patient develops signs of continued bowel ischemia or infarction
Nonocclusive Mesenteric Ischemia.
Diverticula (hollow out-pouchings) are a common structural abnormality that can occur from the oesophagus to the rectosigmoid junction (but not usually in the rectum).
They can be classified as:
• Congenital. All three coats of the bowel are present in thewall of the diverticulum, e.g. Meckel’s diverticulum.
• Acquired. There is no muscularis layer present in the diverticulum, e.g. sigmoid diverticula.
INTESTINAL DIVERTICULA
mucosal herniation at the point of entry of the blood vessels.
vary in size and are often multiple.Presentation:
1- Asymptomatic (incidental finding at surgery or on
radiological imaging )
2- Malabsorption, as a result of bacterial stasis
3- Acute abdominal emergency if they become inflamed or perforate.
4- Bleeding from a jejunal diverticulum is a rare .
Treatment :
Asymptomatic need no treatment
Elective resection of an affected small bowel segment that is causing malabsorption.
If perforated jejunal diverticulitis is found at emergency laparotomy, a small bowel resection + anastomosis /stoma formation.
Extensive jejunal diverticulosis can be very difficult to treat.
Jejunal diverticula
A Meckel’s diverticulum is a persistent remnant of the vitellointestinal duct and is present in about 2 per cent of the population.
- on the antimesenteric side of the ileum
- 60 cm from the ileocaecal valve
- 5 cm long.
- contains all three coats of the bowel wall and has its own blood supply.
- In around 20 per cent the mucosa of a Meckel’s diverticulum contains heterotopic epithelium of gastric, colonic or pancreatic type.
Meckel’s diverticulum
A Meckel’s diverticulum can present clinically in the following ways:
1- Asymptomatic(mostly)2- Haemorrhage
If gastric mucosa is present, peptic ulceration can occur and present as melaena.
3- Diverticulitis
presents like appendicitis.
4- Intussusception
It can be the lead point for ileoileal or ileocolic intussusception.
5- Chronic ulceration
Pain is felt around the umbilicus, as it is midgut in origin.
6- Intestinal obstruction
A band between the apex of the diverticulum and the may cause obstruction directly or by a volvulus around it.
7- Perforation. may resemble a perforated duodenal ulcer.
The finding of a Meckel’s diverticulum in an inguinal or femoral hernia has been described as Littre’s hernia.
Usually diagnosed incidentally(intraoperatively)
- Radionuclide scans (99mTc-pertechnetate)- Angiography can localize the site of bleeding
Diagnosis
Incidental finding of Meckel’s can safely be left if it has a wide mouth and is not thickened. When there is doubt, it can be resected.
If symptomatic: Excise the diverticulum
(by resecting it and suturing the defect at its base, or with a linear stapler-cutter)
limited small bowel resection of the involved segment + anastomosis,
1-If the base of the diverticulum is indurated , inflamed or perforated.
2- in bleeding
3- if the divertic. contains a tumor .
Meckel’s diverticulectomy
rare and <10 per cent of gastrointestinal neoplasia.
BenignMost small bowel neoplasms are benign:
adenomas, lipomas, haemangiomas and neurogenic tumours.
frequently asymptomatic and identified incidentally,
May present with:
- intussusception
- small bowel obstruction
- bleeding that may cause anaemia or may even be overt.
Diagnosis:
- CT
- small bowel contrast studies do not show them easily.
- Capsule endoscopy or small bowel endoscopy
Treatmen:
Symptomatic lesions can be treated by small bowel resection and anastomosis.
TUMOURS OF THE SMALL INTESTINE
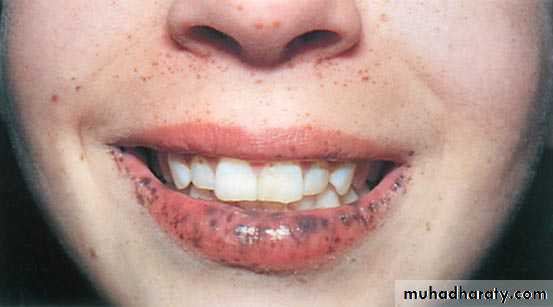
Peutz–Jeghers syndrome
autosomal dominant
melanosis of the mouth and lips + multiple hamartomatous polyps in the small bowel and colon .Melanin spots on digits and perianal skin.
Malignant change in the polyps rarely occurs and, in general the polyps can be left alone.
Resection may be indicated for heavy and persistent or recurrent bleeding or intussusception.
Polyps may be removed by
- enterotomy or laparotomy
- snared via a colonoscope introduced via an enterotomy.
Heavily involved segments of small intestine may occasionally be resected.
Peutz–Jeghers syndromerare and present late, most often diagnosed after surgery for small bowel obstruction.
Adenocarcinoma
carcinoid tumours
lymphomas
mesenchymal tumours (gastrointestinal stromal tumours(GIST)
Malignant small intestinal tumor
more in jejunum
more with Crohn’s disease, coeliac disease, familial adenomatous polyposis (FAP) and Peutz-Jeghers syndrome.They present with anaemia,
gastrointestinal bleeding
intussusception or obstruction.
Prognosis is poor as tumours often present late
the surgical treatment:
Resection of small bowel and the affected mesentery.
A right hemicolectomy for tumours of the distal ileum.
1-Adenocarcinoma
2- Carcinoid tumour
most in appendix, ileum and rectum in decreasing order .arise from Kulchitsky cells
Small +/- significant lymph node metastases
may be multiple.
produce a number of vasoactive peptides, most commonly
5-hydroxytryptamine (serotonin), but also histamine, prostaglandins and kallikrein.
When they metastasise to the liver, the carcinoid syndrome can become evident, because the vasoactive substances escape the filtering actions of the liver.
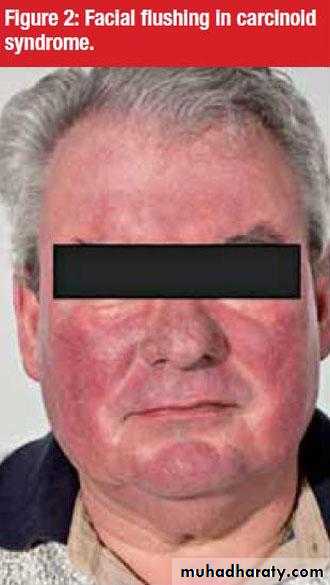
The clinical syndrome itself consists of:
- reddish-blue cyanosis
- flushing attacks(induced by alcohol)
- diarrhoea, borborygmi
- asthmatic attacks
- pulmonary and tricuspid stenosis .
octreotide scanning detect primary and secondary tumours.
Plasma markers chromogranin A concentration (markers of recurrence and prognostic value).primary disease Surgical resection (significant recurrence).
metastatic diseasehepatic resection+octreotide (a somatostatin analogue).
Primary or more common secondary to systemic lymphoma.
more common in patients with Crohn’s disease and immunodeficiency syndromes.Hodgkin’s lymphoma(rare ) to affect the small bowel and most western-type lymphomas are non-Hodgkin’s B-cell lymphomas.
Clinical presentation: -anaem -anorexia
-weight loss -Bleeding - perforation
Coeliac disease T-cell lymphoma .
North Africa and the Middle East Mediterranean lymphoma (widespread ).
Burkitt’s lymphoma can aggressively affect the ileocaecal region, particularly in children.
Treatment :
Chemotherapy
obstruction, perforation or bleeding surgery .
3-Lymphoma
These are mesenchymal tumours
benign or malignant.(difficult to distinguish)Increased size and high levels of c-kit (CD117) staining malignant potential.
most commonly in the stomach, but can be found in other parts of the gut.
50- to 70-year age group.
Patients may be asymptomatic.
Symptoms include: lethargy
pain
nausea
haematemesis
or melaena.
Treatment :
Surgical excision
Glivec (imatinib)(adjuvant)
4-Gastrointestinal stromal tumours
is a chronic, idiopathic segmental transmural inflammatory disease with a propensity to affect the distal ileum
any part of the alimentary tract can be involved.
small bowel affected in 80%
Both genetic and
environmental factors
Crohn’s disease
Pathology:
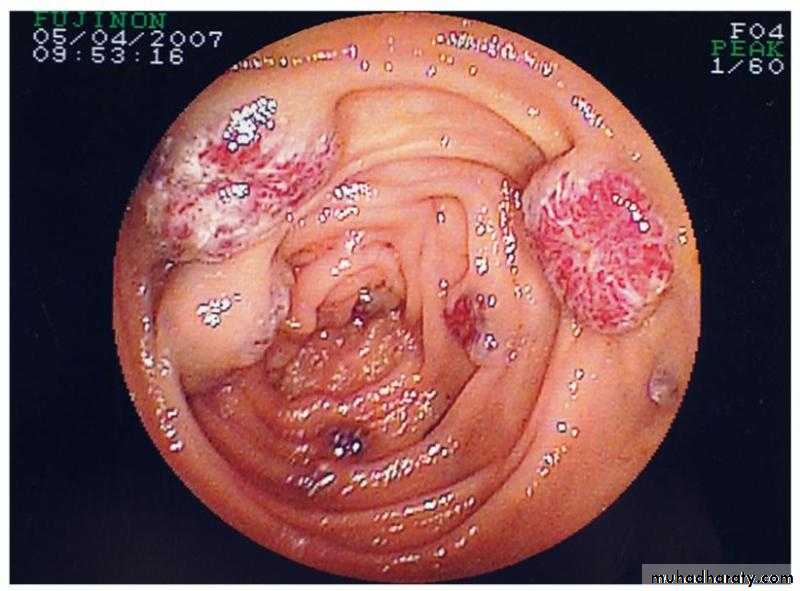
transmural inflammation of the intestineaphthous ulcer.
Noncaseating granulomas
multiple ulcers in intestinal mucosa
cobblestoned appearance of the mucosa
Serosal involvement , adhesion to other loops of bowel or other adjacent organs
fibrosis with stricture formation, intra-abdominal abscesses, fistulas, and, rarely, free perforation.
“skip lesions”
fat wrapping(pathognomonic)
Risk for malignant transforamtion
(a) fibrostenotic disease
(b) fistulizing disease(c) aggressive inflammatory disease.
Abdominal pain(RIF mimcking appendicitis) , diarrhea, and weight loss
waxing and waning course
Constitutional symptoms (weight loss and fever, or growth retardation in children)
Complication (obstruction, fistula, abscess, perforation, perianal abscess or fistula)
Extraintestinal manifestation
Clinical presentation
Diagnosis
Radiographic, Endoscopic, and PathologicColonoscopy with intubation of terminal ileum, Esophagoscopy, capsule endoscopy ulcerations, cobblestone appearance, Skip areas
Contrast examination strictures , ulcers, fissures
CT scanning abcsess , free perforation
Biopsy with endoscopy
no curative, palliate symptoms
Medical therapy :induce and maintain remission.
Surgery -Complication
obstruction
perforation
complicated fistulas
Haemorrhage
Malignancy
-Failure of medical therapy
Conserve as much as you can of the Bowel (open/laparoscopy)
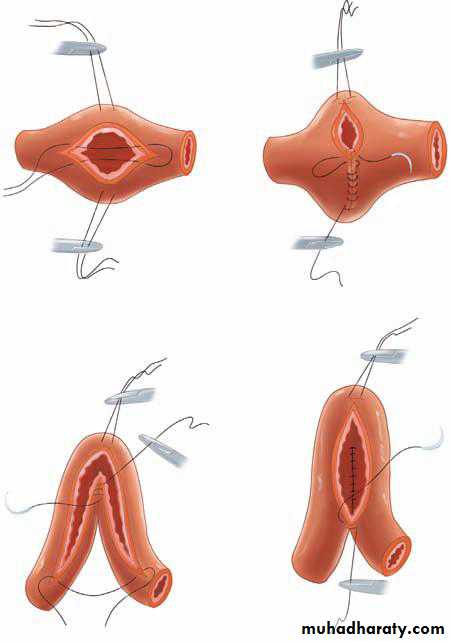
Segmental intestinal resection of gross disease +primary anastomosis
stricturoplasty
Therapy