MALABSORPTION SYNDROME
This occurs when the normal digestion and absorption of food is interrupted1. Pathogenesis
2. Causes3. Consequences
4. Clinical features
5. Investigations
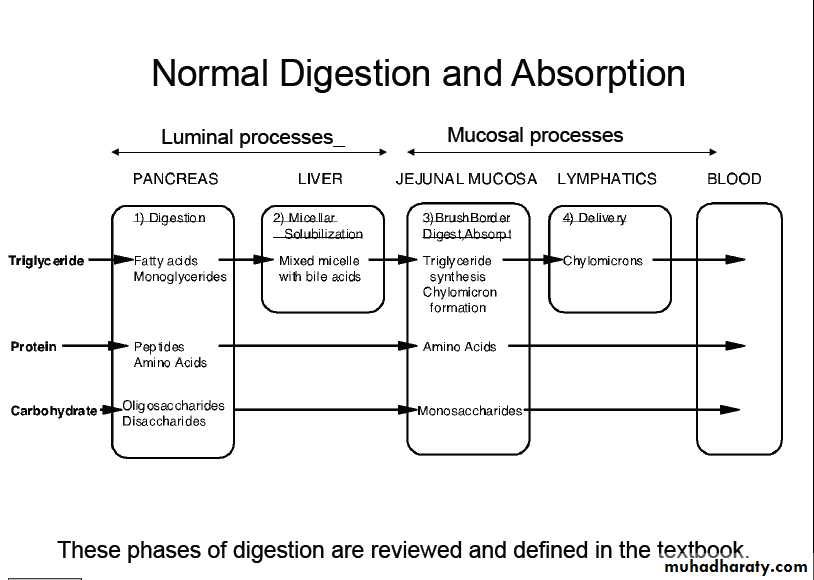
Luminal digestion
1. Sufficient pancreatic enzymes (lipase, trypsin, chymotrypsin, amylase)2. Conjugated bile acids from the liver
Mucosal digestion
It requires:Small bowel brush border enzymes
Mucosal absorption
It requires:
1. Adequate surface of normally functioning small bowel mucosa.
2. Normal intestinal lymphatics.
2.Causes of malabsorption
• Inadequate digestion:• Postgastrectomy steatorrhea.
• Exocrine Pancreatic insufficiency.
• Reduced bile salt concentration in intestine:
• I.) Liver Disease
• II.) Cholestasis
• III.) Bacterial overgrowth
• IV.) Interruption of enterohepatic circulation of bile salt.
• Inadequate absorptive surface:
• 1. Resection• 2. Diseased intestine:
• Celiac disease
• Tropical sprue
• Crohn’s disease
• Disaccharide Deficiency
• Lymphoma
• TB
•
c. Lymphatic obstruction.
e.g LymphomaD. Decreased availability of ingested nutrients and cofactors for absorption.
i) Vitamin B12 malabsorption: intrinsic factor deficiency e.g. gastrectomy, atrophic gastritis( antiparietal cell Ab).
ii) Bacterial overgrowth –can bind B12.
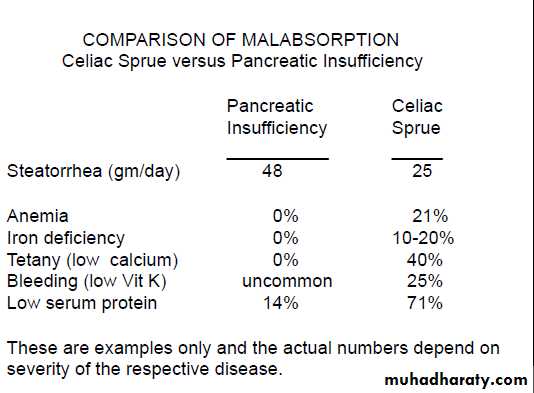
3.Consequences of malabsorption
1. Fat malabsorption: steatorrhea (flow of fat, diarrhea of fat)It will result in weight loss because fat has
the high caloric content.
2. Fat soluble vitamins malabsorption:
(ADEK) A,D,E, and K.
3. Impaired protein absorption: protein malnutrition
4. Impaired carbohydrate absorption: clinically apparent carbohydrate malabsorption and diarrhea5. Impaired absorption of iron, folate, and B12.
This happen only small intetsinal mucosal disease and is not a feature of pancreatic insufficiency.5. CLINICAL MANIFESTATIONS
History:
Diarrhea/steatorrhoea Weight loss Symptoms of anaemia
Diarrhoea – bulky, floating, malodorous stool – difficult to flush.
Weight loss – may be profound.
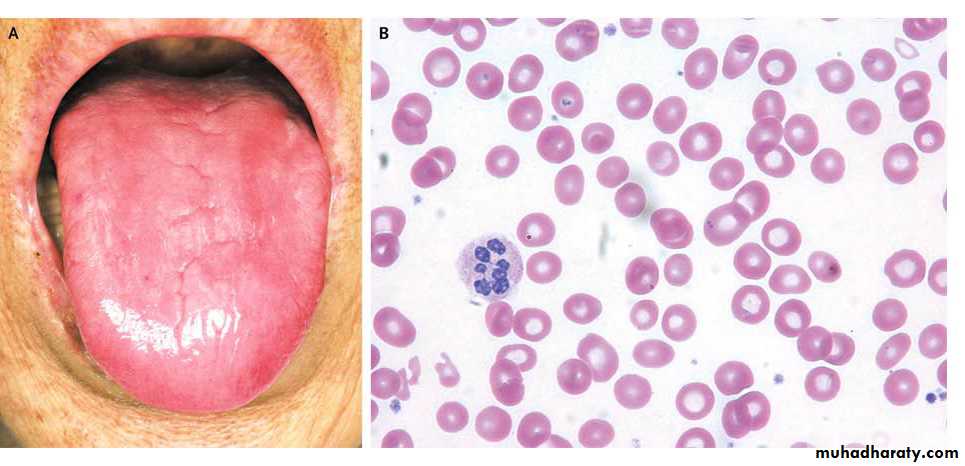
Anaemia – B12, iron, folate malabsorption.
Patient may complain of dizziness, dyspnoea and fatigue
Important part of history:
1. Ethanol abuse2. Drugs
3. Previous gastric or intestinal surgery
4. Positive family history (Celiac)
4. Pulmonary manifestations (cystic fibrosis)
5. Fever and weight loss (TB, lymphoma, Crohns disease of small bowel)
O/E:
Normal.Pallor - muscle wasting
Sign of vitamin deficiency
glossitis – B deficiency
ecchymoses
parasthesia
tetany
Clinical approach:
1. Identify nutritional deficiency:single, multiple or generalized
2. Document impaired digestion and or absorption
3. Identify underlying cause
4. Treat appropriately.
Investigations
1. Screening tests.2. Specific diagnostic tests
3. Tests to identify the underlying cause.
Screening test)) Investigations:
General:- CBC
- Blood film
- Ca.
- B12, folate
- Iron study
- LFT, PT, PTT
6. Investigations:
Specific:
Tests of fat absorption:
Quantitative fecal fat
Patient should be on daily diet containing 80-100 grams of fat.
Fecal fat estimated on 72 H collection.
6 grams or more of fat/day is abnormal.
May be due to: - Pancreatic
- Small intestinal
- Hepatobiliary disease
Sudan Black Test:
This test has replaced fecal fat estimationIt is much easier, done on single specimen of stool.
It will be positive if abnormal amount of fat present in the stool.
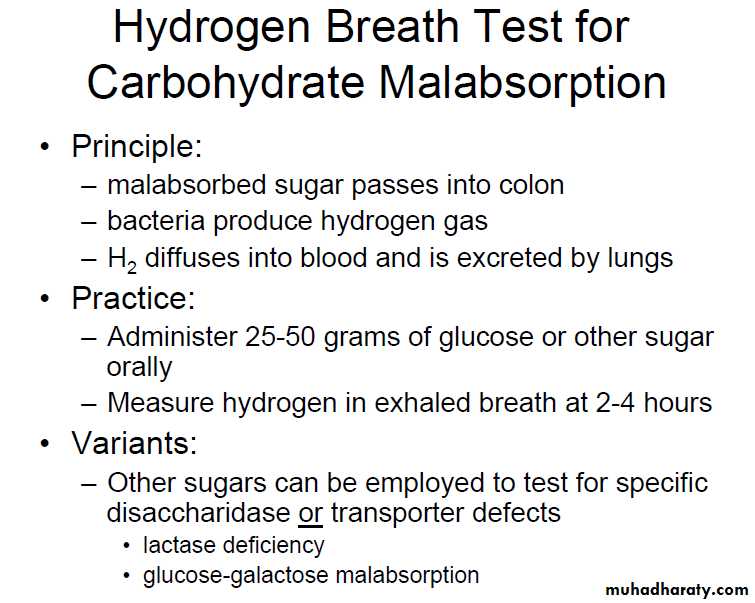
Carbohydrate absorption test
1) Hydrogen breath testHydrogen excretion ↑ in
bacterial overgrowth
small intestinal malabsorption
2. D-xylose test:
An oral- labelled simple sugar that does not undergo any digestionOnly need normal bowel mucosa to be absorbed and excreted in the urine.
It is normal in pancreatic causes of malabsorption
25 grams given
Urine collected for 5 hoursNormally 25% is excreted
In patients with fat malabsorption, this test
differentiates pancreatic from small intestinal malabsorpton.
Tests to identify underlying cause:
1. Small bowel cause2. Pancreatic cause
A. Small bowel tests
1. D-xylose
2. Small bowel biopsy
3. Serological tests for celiac disease
4. Radiology: barium follow-through
B. Pancreatic functions
1. Direct:Secretin stimulation test: It stimulate the pancreas to release bicarbonate.
After which duodenal fluid is collected and analyzed to quantify normal pancreatic secretory content (ie, enzymes, and bicarbonate).
2. Indirect:
fecal fat estimationSudan black
3. Radiographic techniques:
- Plain abdominal X-ray
- U/S abdomen
- ERCP
- CT abdomen
- MRI & MRCP
- Endoscopic ultrasound
4. Fecal elastase measurement:
It is the most sensitive and specific, especially in the early phases of pancreatic insufficiency.
Values less than 200 mcg/g are suggestive of pancreatic insufficiency
Diseases causing malabsorption
1. Celiac disease2. Exocrine pancreatic insufficiency
3. Disaccaharidase deficiency (lactase deficiency)
4. Tropical sprue
5. Small intestinal bacterial overgrowth.
6. Whipples disease.
7. Intestinal lymphangiectasia
Disaccharides malabsorption
The terminal phase of digestion of ingested complex carbohydrate such as oligosaccharides and disaccharides including lactose occurs at the brush border membrane of intestinal absorptive cells where disacharideases enzymes are located.Lactose malabsorption
1. Congenital lactase deficiency2. Acquired:
The most common cause of carbohydrate intolerance in adults.
Low mucosal lactase levels are observed in over 90% of Asians
Pathogenesis
Fermentation of unabsorbed lactose by intraluminal bacteria.
Clinical features & diagnosis
History:Diarrhea
Abdominal discomfort
Flatulence
following the ingestion of dairy products or other foods rich in lactose.
2. The diagnosis is confirmed by:
lactose breath hydrogen test.
oral lactose intolerance test.
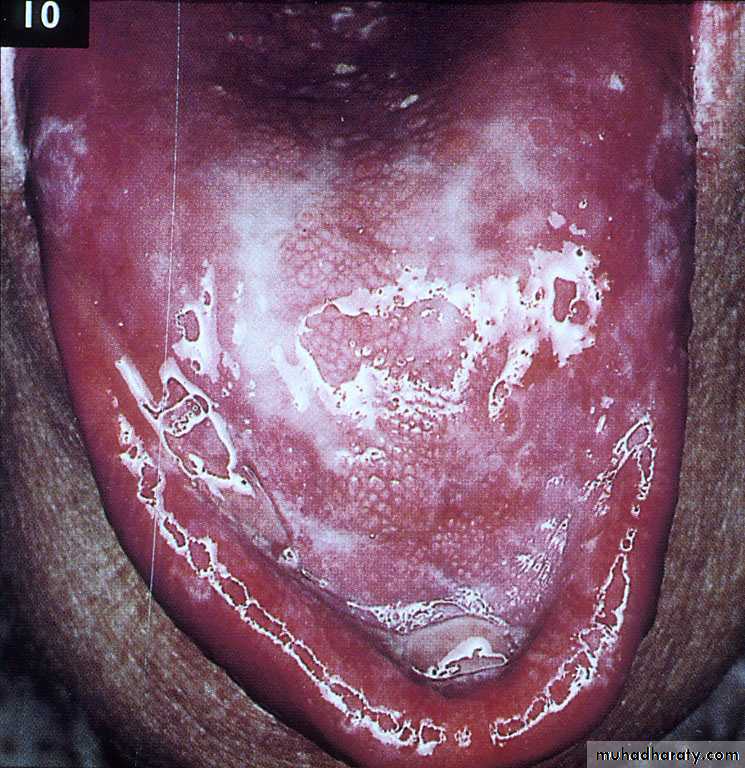
Tropical Sprue
Occurs among natives of, visitors to selected countries located in the tropics (major epidemics have been described in south Indian villages)Cause:
Most probably infectious
(no single causative pathogen has been identified)
Clinical features
Non specificDiarrhea, steatorrhoea, weight loss, nausea, and anorexia.
Anemia is common (megaloblastic or dimorphic)
Diagnosis & Treatment
Mucosal biopsy of the small intestine reveals a nonspecific lesion of variable severity.
Treatment:
Antibiotic such as tetracycline and high-dose folic acid.
Response is prompt.
Treatment lasting 6 months- 1 year
Small intestinal bacterial overgrowth
Under normal circumstances the proximal small intestinal lumen harbors less than 105 bacteria per milliliter of intestinal contents.Overgrowth of bacteria in the small intestine (there may be 108-1010/mL organisms)
.
Pathogenesis
1. Bacteria deconjugate the bile salts2. The bacteria produce toxins and proteolytic enzymes that damage the mucosa specially the brush border.
3. The bacteria bind and metabolize B12 preventing its absorption in the distal ileum.
Causes
1. Motility disordersScleroderma, amyloidosis, vagotomy, diabetic visceral neuropathy.
2. Structural abnormalities
Diverticula, strictures, afferent loop stasis, vascular.
3. Hypochlorhydria or achlorhydria
4. Hypogammablobulinemia or agammaglobulinemia
•
Clinical features
Watery diarrhoea and/or steatorrhoea
Anaemia due to B12 deficiency
Diagnosis
1. Quantitative culture of the duodenal fluid is the diagnostic gold standard.2. Breath tests utilizing lactulose, xylose, and
Glucose
3. Serum vitamin B12 concentration is low, whilst folate levels are normal or elevated because the bacteria produce folic acid.
4. Response to antibiotics
Treatment
Antibiotics are the treatment of choice.Amoxicillin–clavulanate alone or with metronidazole 2-week course of therapy (prolonged remission)
Frequent intermittent courses of antibiotics when symptomatic may be required in some patients.
Whipple's disease
A rare condition characterized by infiltration of small intestinal mucosa by 'foamy' macrophagesThe disease is a multisystem one and almost any organ can be affected, sometimes long before gastrointestinal involvement becomes apparent
Middle-aged men are most commonly affected
Cause
Infection with the Gram-positive bacillus Tropheryma whipplei
Clinical features
The presentation depends on the pattern of organ involvement1. GIT:
Diarrhoea (75%), steatorrhoea, weight loss (90%), bloating, protein-losing enteropathy, ascites, hepatosplenomegaly (< 5%)
2. Mscloskeletal:
Seronegative large joint arthropathy, sacroiliitis
3. Cardiovascular:Pericarditis, myocarditis, endocarditis, coronary arteritis .
4. Neurological:
Apathy, fits, dementia, myoclonus, meningitis, cranial nerve lesions5. Pulmonary:
Chronic cough, pleurisy, pulmonary infiltrates
6. Hematological:
Anaemia, lymphadenopathy
7. Other:Fever, pigmentation
Diagnosis
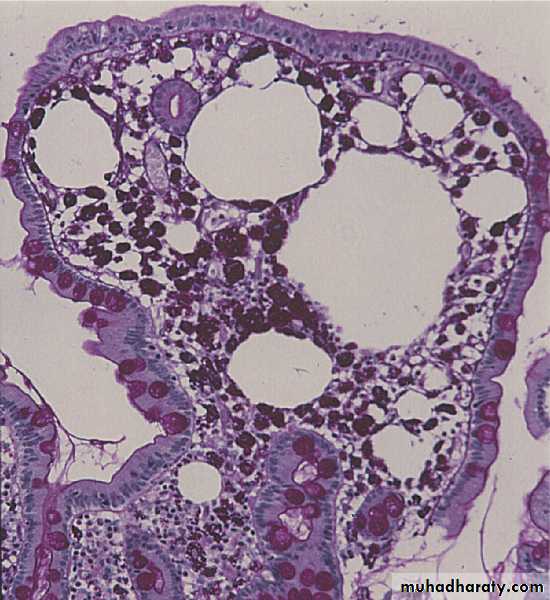
Upper GI endoscopy and biopsyVilli are widened and flattened; densely packed macrophages occur in the lamina propria.
which stain positive with periodic acid-Schiff (PAS) reagent
These may obstruct lymphatic drainage, causing fat malabsorption
Treatment
Antibiotics:1. Intravenous ceftriaxone 2 gm, iv daily for 2 weeks
2. Followed by oral co-trimoxazole for at least 1 year.
Symptoms usually resolve quickly
Long-term follow-up is essential, as relapse occurs in up to one-third of patients.
Intestinal lymphangiectasia
A. Primary:due to impaired lymphatic formation during development.
B. Secondary: lymphatic obstruction
1. Infection such as TB or filariasis.
2. Neoplasm (lymphoma)
3. Retroperitoneal fibrosis.
4. Constrictive pericarditis
Consequences
Rupture of the lymphatics result in:
1. leakage of lymph which is rich in fat, protein
fat soluble vitamins and lymphocyte into the gut lumen.
2. Impaired transport of dietary lipids to the systemic circulation.
Clinical features
1. Weight loss, diarrhea, steatorrhea.2. Edema, chylous ascites, and chylous pleural effusions
Chyle: Milky-white fluid , rich in triglycerides
Investigations
1. Biochemical:Hypoalbuminemia
Reduced serum immunoglobulin concentrations
2. Hematological: lymphocytopenia
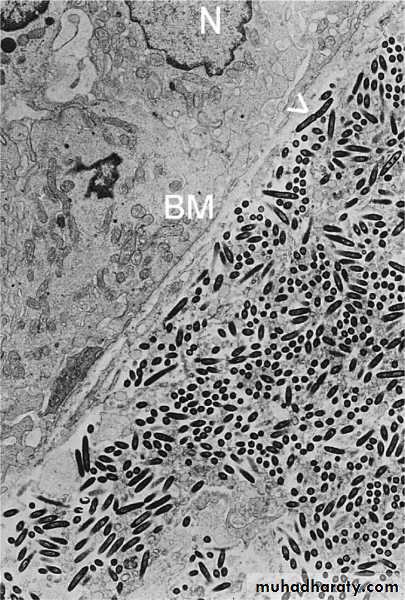
3. Histological: Jejunal biopsies show greatly dilated lacteals.
4. Lymphangiography: may localize the site of lymphatic lymphatic obstruction or show leakage
Treatment
1. Low-fat diet with medium-chain triglyceride (transported in the portal blood)2. A high protein diet.
3. Reduction of dietary long-chain triglycerides that stimulate lymph formation, increasing
intralymphatic pressure and predisposing to lymphatic rupture and lymph leakage.
4. Treatment of the cause.
Short Bowel Syndrome
The small intestine has sufficient reserve Resection of 50% is well-tolerated provided that the duodenum and proximal jejunum and the distal 100 cm of the ileum are not removed and are free of disease
Extensive resection or disease of small intestine will result in maldigestion and malabsorption.
Consequences
Depend on site and extent of resectionDigestion and absorption are normally completed within the first 100 cm of jejunum,
Extensive resection will cause maldigestion and malabsorption
.
Pathogenesis
1. Reduction of the available absorptive surface.2. Acid hypersecretion that induces intestinal mucosal damage and can inactivate pancreatic lipase ( postoperative hypergastrinemia)
3. Depletion of the bile salt pool.
4. Small intestinal bacterial overgrowth.
Clinical features
Symptoms:Resection of 70–80% of the small intestine often produces catastrophic malabsorption with massive diarrhea and steatorrhea.
Signs:
Dehydration and signs of hypovolaemia are common
Weight loss, loss of muscle bulk and malnutrition
Causes
Small bowel resection due to:
a. Acute mesenteric ischemia
b. long-standing Crohn,s disease
c. Radiation enterocolitis
d. Malignant disease of the small bowel
Treatment
1. Parenteral nutrition initially.2. Early initiation of continuous enteral
feedings to minimize intestinal mucosal atrophy
and maximize adaptive mucosal hyperplasia.
3. Proton pump inhibitor to control acid hypersecretion during the early period.
4. loperamide or codeine to decrease intestinal transit time and hence contact of nutrients with the intestinal mucosa
5. Transition to oral feedings, starting with multiple small meals while tapering parenteral
nutrition is often feasible as intestinal adaptation progresses over time (morphological,length and diameter)
6. Small intestinal transplantation:
In patients in whom adaptation is not adequate and long-term parenteral nutrition is not feasible.
Lymphoma (NHL)
GIT may be involved:
1. As part of more generalised disease.
2. Primary gut lymphoma (rare)
The small intestine being most commonly affected.
Lymphomas occur with increased frequency in patients with:
Coeliac disease, AIDS and other immunodeficiency states.
Age: most often in middle-aged men
Site: usually focal with a predilection for the ileumTwo variants of small intestinal lymphoma regularly cause malabsorption:
1. Immunoproliferative small intestinal disease-associated lymphoma (IPSID)
2. Enteropathy-associated T-cell lymphoma (EATL).
IPSID (Mediterranean lymphoma)
Age: young adults ,native Middle-Eastern populations as well as in South Africa and Pakistan.Its cause is unknown
It has been suggested that bacteria or other antigens cause excessive proliferation of lamina propria immunocompetent cells in people with poor hygiene
Clinical features
1. Early:Abdominal pain
Diarrhea and steatorrhea
Anorexia and weight loss.
2. Advanced:
Edema, ascites
Hepato-splenomegaly
Palpable abdominal masses may become evident.
Investigations
IPSID is associated with the production of an unusual IgA heavy chain protein, called α heavy chain, which is secreted by plasma cells
1. Immunoglobulin electrophoresis:
It will reveal the presence of a paraprotein consisting of the Fc portion of IgA (heavy chain), devoid of light chains, as a broad band on protein electrophoresis
Histology
2. OGD and biopsy:In the early stages:
Diffuse infiltration of the mucosa and submucosa with B lymphocytes and plasma cells.
As the disease progresses the infiltrating cells develop histologically malignant characteristics and mesenteric nodes become involved
Treatment
1. Antibiotics: (long-term)Such as, tetracycline, ampicillin, and metronidazole
Prolonged remissions can be obtained and even cure.
2. Chemotherapy :
for those who fail to respond or who have aggressive disease.
Gut infection
1. Intestinal tuberculosis.2. Giardiasis
Intestinal tuberculosis
Usually results from human M. tuberculosis which is swallowed after coughing.
The area most commonly affected is the ileocaecal region
Clinical features
Abdominal pain can be acute or of several months' duration2. Diarrhoea : less common
3. Low-grade fever is common
Diagnosis
1. Barium follow-through2. Colonoscopy and terminal ileoscopy
3. Histological confirmation(caseation of granulomas is not always seen )
4. Culture ( may take 6 weeks )
5. PCR-based techniques on biopsy specimens.
Treatment
Chemotherapy with four drugs (2 months)Isoniazid
Rifampicin
pyrazinamide
ethambutol
Continue isoniazid and rifampicin for 4 more months
Giardia lamblia
The most common protozoal infestation
Once cysts are ingested, the distinctive trophozoites are released in the upper small intestine
The trophozoites attach to the intestinal
epithelium and can produce significant enteritis with mucosal inflammation and architectural changes.
Clinical features
1.Asymptomatic:Approximately 50% of individuals infested with G lamblia have no symptoms (asymptomatic carriers)
2. Symptomatic:
Diarrhea, flatulence, abdominal cramps, and epigastric pain and nausea and vomiting.
3. Some patients present with steatorrhea and weight loss.
Diagnosis
1. Stool examination:Concentrated, iodine-stained wet stool preparations
Because cysts and trophozoites are present only intermittently in the stool, however, the sensitivity is only approximately 50%, even with examination of multiple specimens
2.Stool immunoassays (Molecular tests )including an ELISA with reported sensitivities and specificities approaching 100%.
3. Direct sampling of duodenal contents (e.g., duodenal aspiration or the “string test”), sensitivity can be improved to approximately
80%
4. OGD and duodenal biopsy:
Identification of trophozoites with small intestinal biopsy specimens
Treatment
Metronidazole, 250 mg orally three times a day for 5 daysA single 2-g dose of tinidazole has been reported to be 90% effective