Poor progress in labour
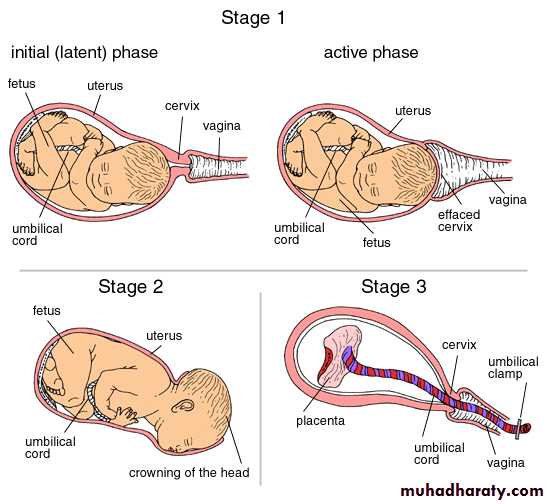
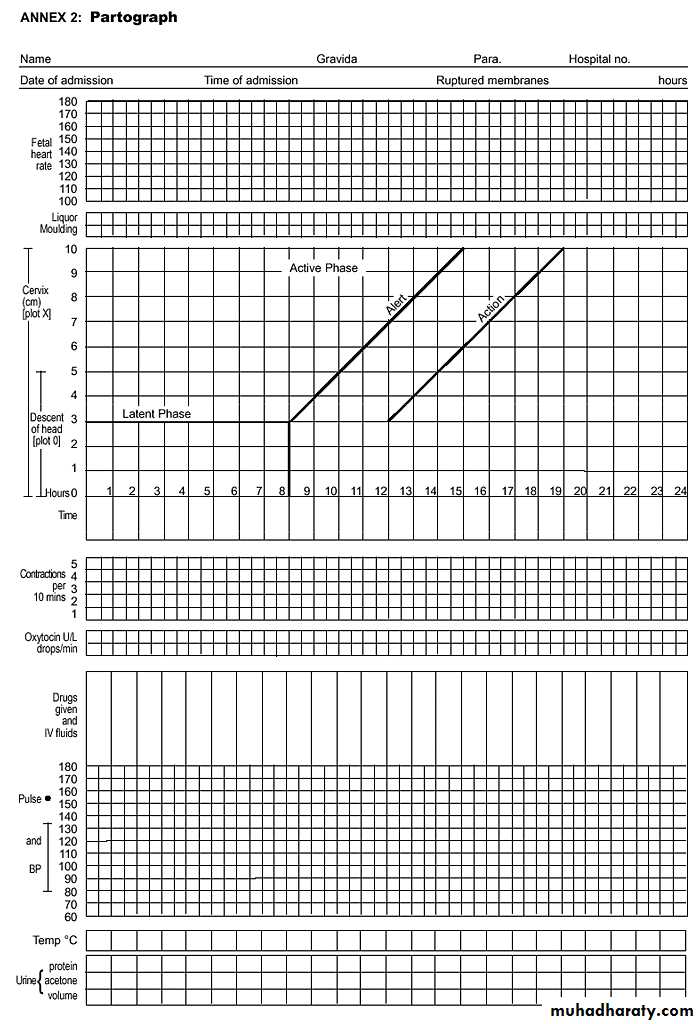
first stage of labour is the time of cervical dilatation and /or effacement and fetal presenting part descent.Plotting the finding of serial vaginal examinations on the partogram will help to highlight poor progress in first stage.
A progressive change in the cervix over a few hours will confirm established labour, and so a vaginal examination at the time of admission to the labour ward is important to establish a baseline.
Stages of labour:
partograph
second stage of labour is the time of descent of presenting part. It is important to diagnose fully dilated cervix to confirm diagnosis of second stage.
Risk factors for poor progress in labour:
Small woman.Big boy.
Malpresentation.
Malposition.
Early membrane rupture.
Soft-tissue / pelvic malformation.
Progress in labour is dependent on three variables:
• abnormalities in one or more of these factors can slow normal progress of labour.
Causes of poor progress of labour:
Any faults in one or more of these can cause poor progress of labourFaults in the powers, inefficient uterine action or incoordinate uterine action (irregular).
It should be considered first.
Assessment of uterine contractions is carried out by clinical examination and by using External tocography
internal tocography using an intrauterine pressure sensor may be best but has never really progressed beyond a research tool.
Treatment:
if poor uterine action is suspected steps should be taken to improve it.A. Maternal rehydration.
B. Artificial rupture of membrane (ARM) if membrane intact.
C. Intravenous oxytocin is the cornerstone of therapy if no contraindication and after full evaluation. As it increase contraction and treat inco-ordinate uterine contractions.
Faults in the passages:
may come from distortion in the maternal bony pelvis by disease, damage or deformity.There is little that can be done to over come these, and unless they present only marginal difficulty, delivery by Caesarean section is usually required.
The soft tissues of the birth canal – cervix, vagina, perineum, may, if rigid, obstruct progress.
The passenger:
Fetus may be uncooperative by being excessively large, in the wrong position or presentation.If no contraindication, maximize the quality of uterine contractility which may often over come minor problems of the passages or the passenger or both. If these problems persist then Caesarean section is necessary.
Patterns of abnormal progress in labour:
Prolonged latent phase (poor progress in active phase of labour).Primary dysfunctional labour. (<1cm /hour cervical dilatation).
Secondary arrest. When progress in active phase is initially good but then sloes or stops after 7 cm dilatation.
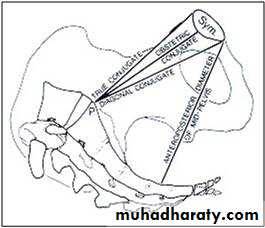
Cephalopelvic disproportion
It implies anatomical disproportion between fetal head and maternal pelvis. It can be due to a large head, small pelvis or a combination of two.
Diagnosis of CPD antenatally:
Past orthopaedic and obstetric history:History of disease or fracture of spine, hips or pelvis should alert about possibility of pelvic
In multipara ask about weight of largest baby previously delivered, details of her previous labours including duration and mode of delivery outcome, birth weight and subsequent progress of child.
General examination:general disease of skeleton or disease of lower limbs or spine should be noted.
Small woman.
FAULTY DEVELOPMENT:
Abdominal examination
In late pregnancy engagement should be examined.In primigravidae the head normally engaged between 36-38 weeks. In multipara engagement often dose not occur until labour starts.
Although engagement of head after 37 weeks in a primigravida is reassuring, failure to do so does not necessarily mean the presence of CPD.
Pelvic examination:
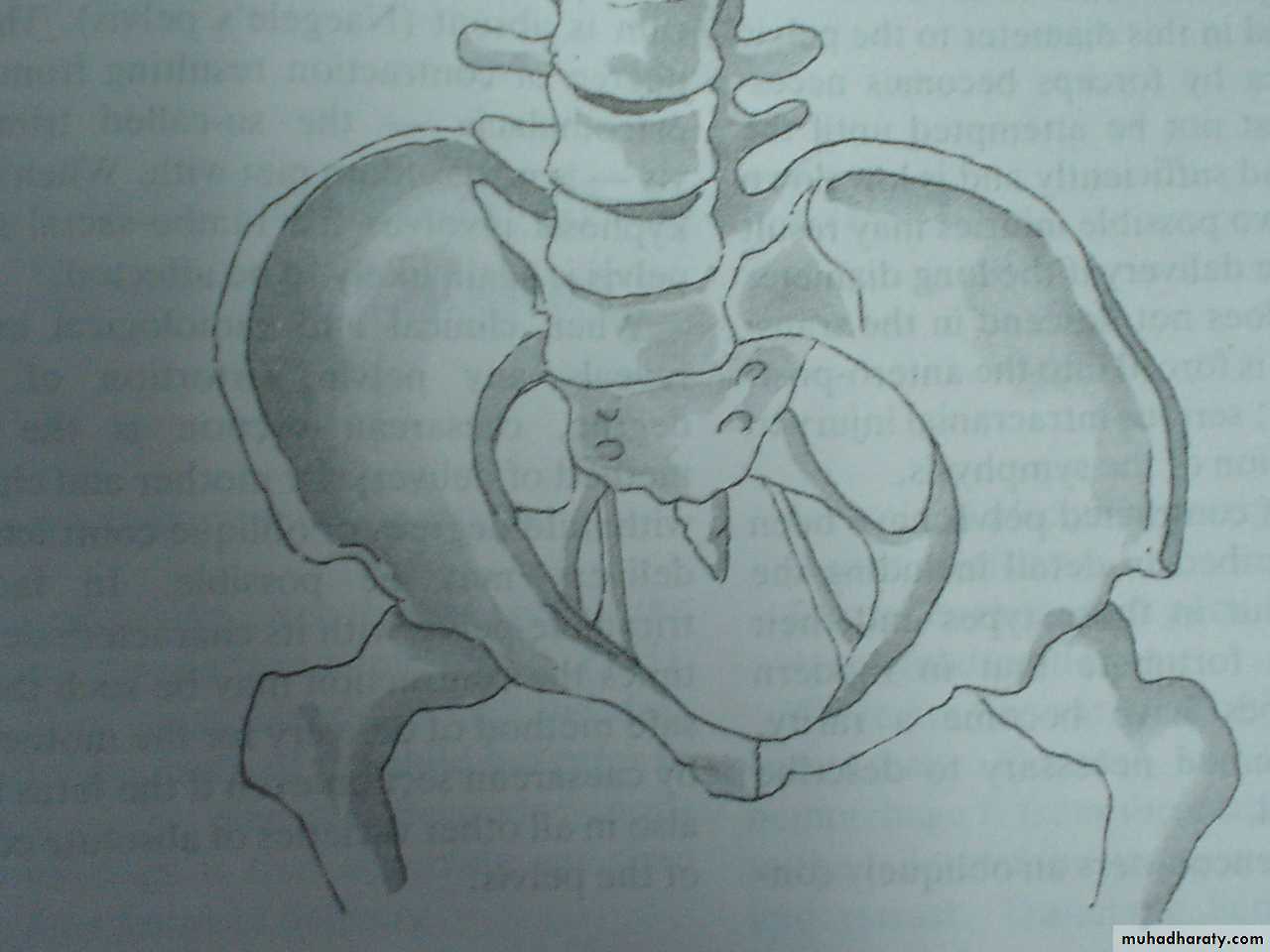
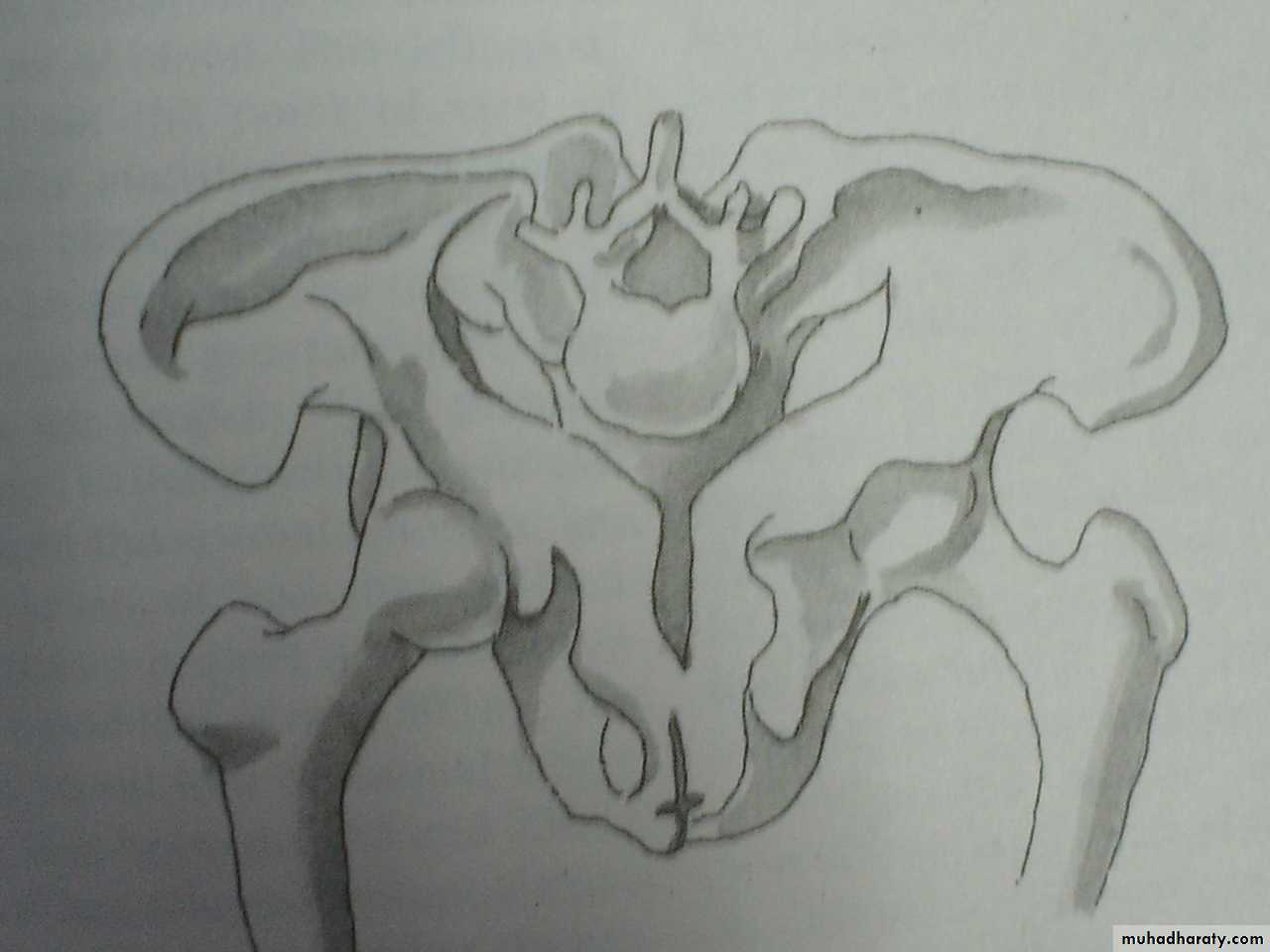
Signs suggestive of an inadequate pelvis:
Sacral promontory reached easily in contracted pelvis.
straightness of sacrum.
Convergence of side walls of pelvis.
prominent Ischial spines.
Biischial diameter is less than 8 cm.
Distance between ischial tuberosities less than 8 cm.
Distance between ischial tuberosities is less than a closed –hand fist.
Subpubic angle does not admit two fingers comfortably.
Diagnosis of disproportion during labour:
CPD is suspected in labour if:Progress is slow or arrested despite efficient uterine contractions.
Signs suggestive of CPD during labour are:
Abdominal examination:Large fetal size.
Fetal head failed to descend.
Pelvic examination:
Cervix shrinking after amniotomy.
appearance of fresh meconium
Edema of cervix.
Head not well applied against the cervix.
Caput formation.
Progressive excessive moulding.
Deflexion of head (easily palpable anterior fontanelle)
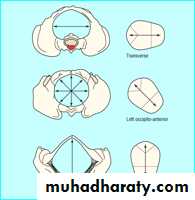
Asynclitism (sagital suture not in the middle of pelvis)
Others:
Maternal pushing before cervical dilatation.Early decelerations.
The best diagnosis of CPD is a trial of labour. The diagnosis of cephalopelvic disproportion is usually retrospective after a well-conducted trial of labour.
Treatment
Failure to progress due to cephalopelvic disproportion in the first stage and in the second stage when the station is high, delivery is accomplished by caesarean section.Obstructed Labourimpending uterine rupture
labour is said to be obstructed when there is no progress in spite of strong uterine contractions. It shown by failure of cervix to dilate or failure of presenting part to descend through birth canal. It is a most dangerous condition if it is untreated and can be fatal to both mother and fetus.Aetiology
A. Maternal conditions:
1. Contraction or deformity of bony pelvis.
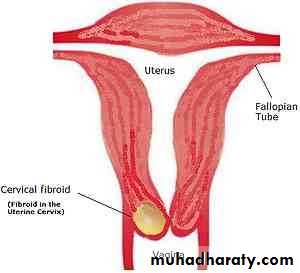
2. Pelvic tumours ( uterine fibroids, ovarian tumours, tumour of rectum.
Bladder or pelvic bones).
3. Pelvic kidney.
4. Abnormality of uterus or vagina:
Stenosis of cervix or vagina.
Obstruction by one horn of double uterus.
Contraction ring of uterus.
B. Fetal condition:
Large fetus.Malposition or malpresentation
Persistant occiptoposterior or transverse position.
Mentoposterior position.
Breech presentation.
Shoulder presentation
Compompound presentation
Locked twins.
congenital abnormalities of fetus
hydrocephalous.
fetal ascitis or abdominal tumours.
hydrops fetalis.
conjoined twins.
Diagnosis
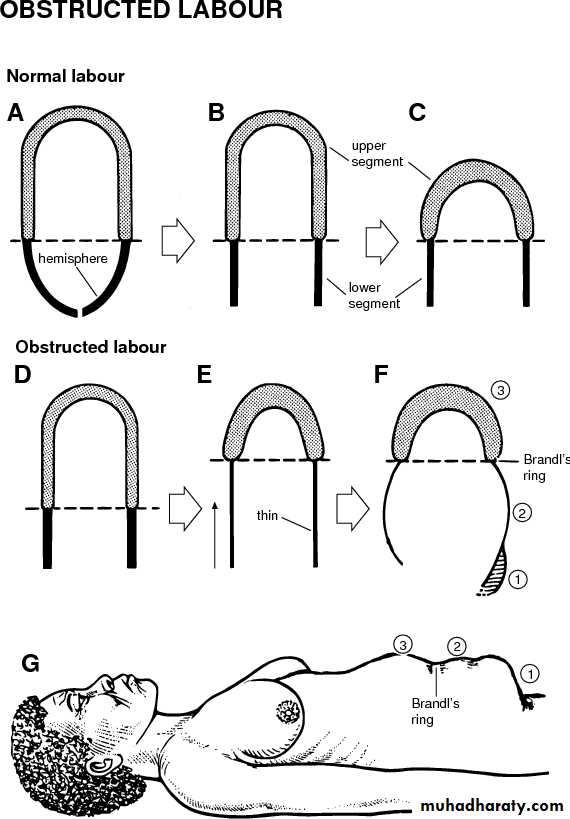
the importance of early detection of possible obstruction is obvious as labour if allowed to reach point of absolute obstruction will lead to death of fetus and endangered mother life.In a primigravida complete obstruction leads within 2-3 days to a state of uterine exhusation or secondary hypotonia.
In Multigravida, obstruction becomes established much sooner and progressive thinning of lower segment may lead to uterine rupture in a few hours.
General examination
Deterioration in patient's general condition:It shows signs of maternal distress and looks tired and anxious, exhausted and loss her ability to cooperate.* high temperature (38°C), * rapid pulse,* signs of dehydration: dry tongue and cracked lips.
Abdominal examination
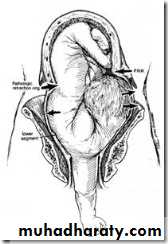
* The uterus is hard and tender,frequent strong uterine contractions with no relaxation in between (tetanic contractions).rising retraction ring is seen and felt as an oblique groove across the abdomen called retraction ring of Bandle which can be seen and felt in abdominal examination.In advanced obstructed labour the uterus is found to be molded to shape of fetus
presenting part is often above or at level of pelvic brim.fetal parts cannot be felt easily.severe fetal distress due to interference with the utero-placental blood flow or absent fetal heart.
Vaginal examination* Vulva: is oedematous. * Vagina: is dry and hot.* Cervix: is fully or partially dilated, oedematous.* The membranes: are ruptured.*The presenting part: is high and not engaged or impacted in the pelvis. If it is the head it shows excessive moulding and large caput.* The cause of obstruction can be detected.
Complications
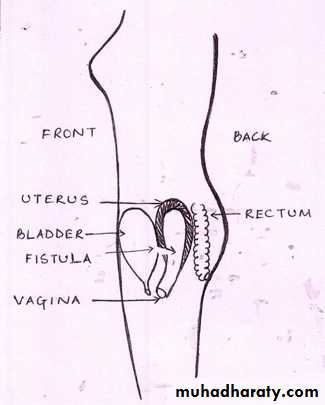
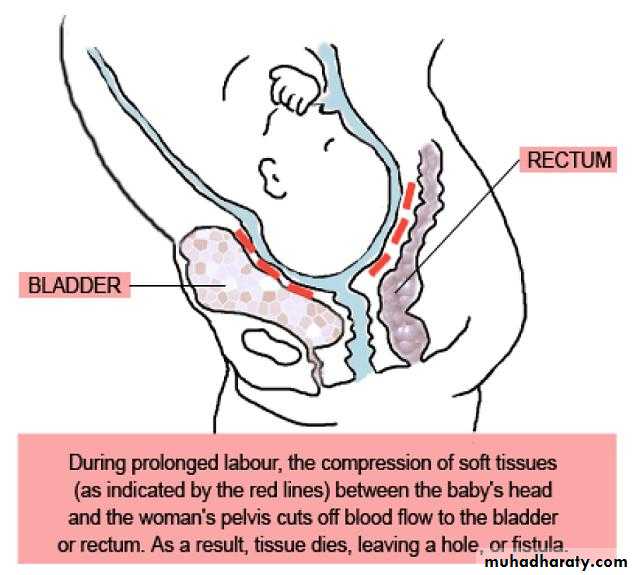
a.Maternal complications:1. Maternal distress and ketoacidosis.2. Rupture uterus.3. Necrotic vesico-vaginal fistula. The fetal presenting part becomes impacted in maternal pelvis and causing ischemia of maternal soft tissues that lie between presenting part and walls of maternal pelvis which if neglegted can lead to tissue necrisis and formation of vesicivaginal or rectovaginal fistule.4. Infections as chorioamnionitis and puerperal sepsis.5. Postpartum haemorrhage due to injuries or uterine atony.
Complication
b. Fetal complications:1. Asphyxia. 2. Intracranial haemorrhage from excessive moulding.3.Birth injuries.4. InfectionsManagement
Curative measures:Caesarean section is the safest method even if the baby is dead as labour must be immediately terminated and any manipulations may lead to rupture uterus.There is risk of puerperal sepsis so appropriate antibiotics should be given.
Management
Preventive measures:good antenatal care and plane of action can be made before labour.Careful observation, proper assessment,using partograph, early detection and management of the causes of obstruction.
Shoulder dystocia
Difficulty with delivery of fetal shoulder. Occurs in 0.2-1.2 % .
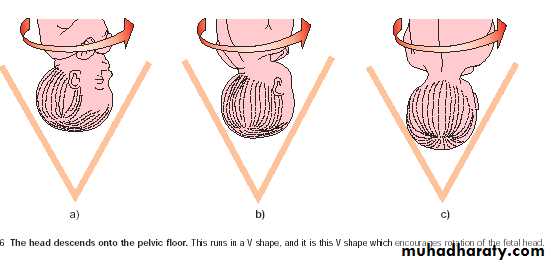
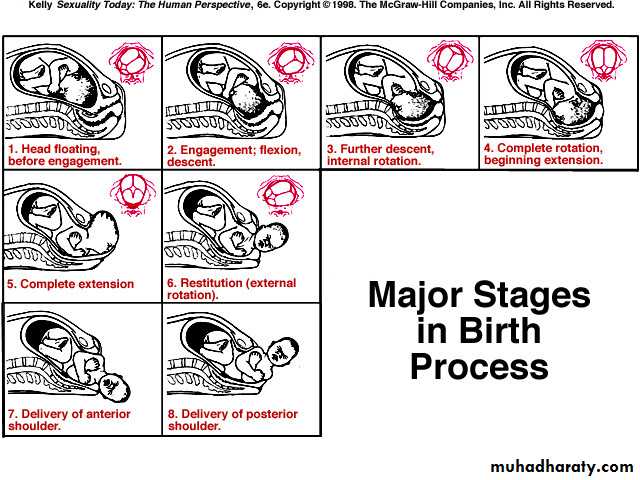
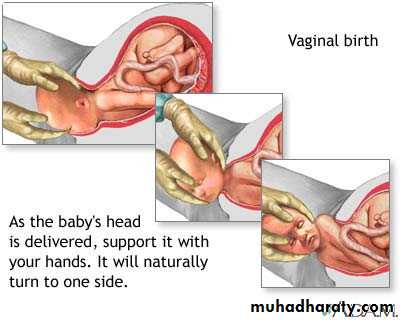
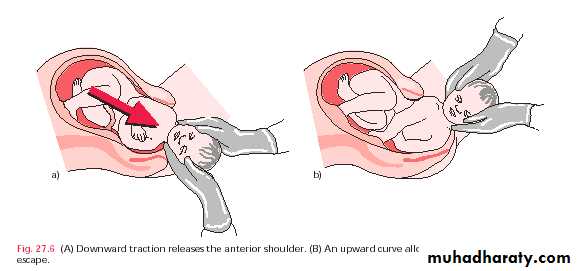
The fetal head and shoulder rotate to make use widest diameters of pelvis. After delivery of head, resititution occurs and the shoulders rotate into anterior-posterior (AP) diameter. This make use of widest AP diameter of pelvic outlet. However if shoulders have not entered pelvic inlet, the anterior shoulder may become caught above maternal symphysis pubis. Occasionally both shoulders may remain above pelvic brim.
Risk factors:
• Large baby.• Small mother.
• Maternal obesity.
• Diabetes mellitus.
• Post-maturity.
• Previous shoulder dystocia.
• Prolongation of first stage of labour.
• Prolonged second stage of labour.
• Assisted vaginal delivery.
Prediction and prevention:
Shoulder dystocia can only be completely avoided by caesarean section.
In the majority of cases, recognition of risk factors should lead to an experienced obstetricans being present at delivery to manage the problem.
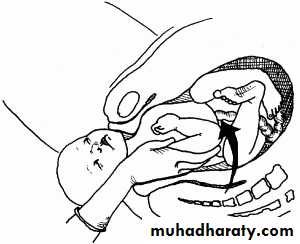
As serious traction causing stretching of brachial plexus and nerve damage. Erb's palsy is a likely consequence. Up to 25% associated with fetal morbidity and mortality.
Management:
All in labour ward should have training to treat this.Reduce interval between time of delivery of head to delivery of body. after 5 minutes, there is risk of cerebral damage.
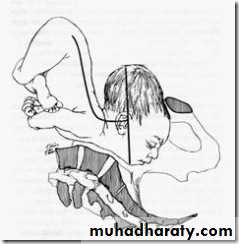
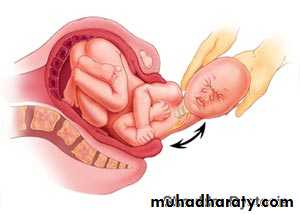
Shoulder dystocia is managed by a sequence of maneuvers designed to facilitate delivery without fetal damage.
Large episiotomy
Clear infant's mouth and nose.
Initial gentle attempt at traction, assisted by maternal expulsive efforts is recommended.Flex and abduct patient's hips on her abdomen (McRobert's position).
Apply suprapubic pressure pushing on fetal shoulder towards fetal chest.
If above failed, attempt to rotate the shoulders by putting hand into vagina and pushing on front aspect of posterior shoulder.