DR. SAMER ALWAZNI
MB.CH.B., DMRD, FCABMS-RAD.Physics of X-ray
Lecture object
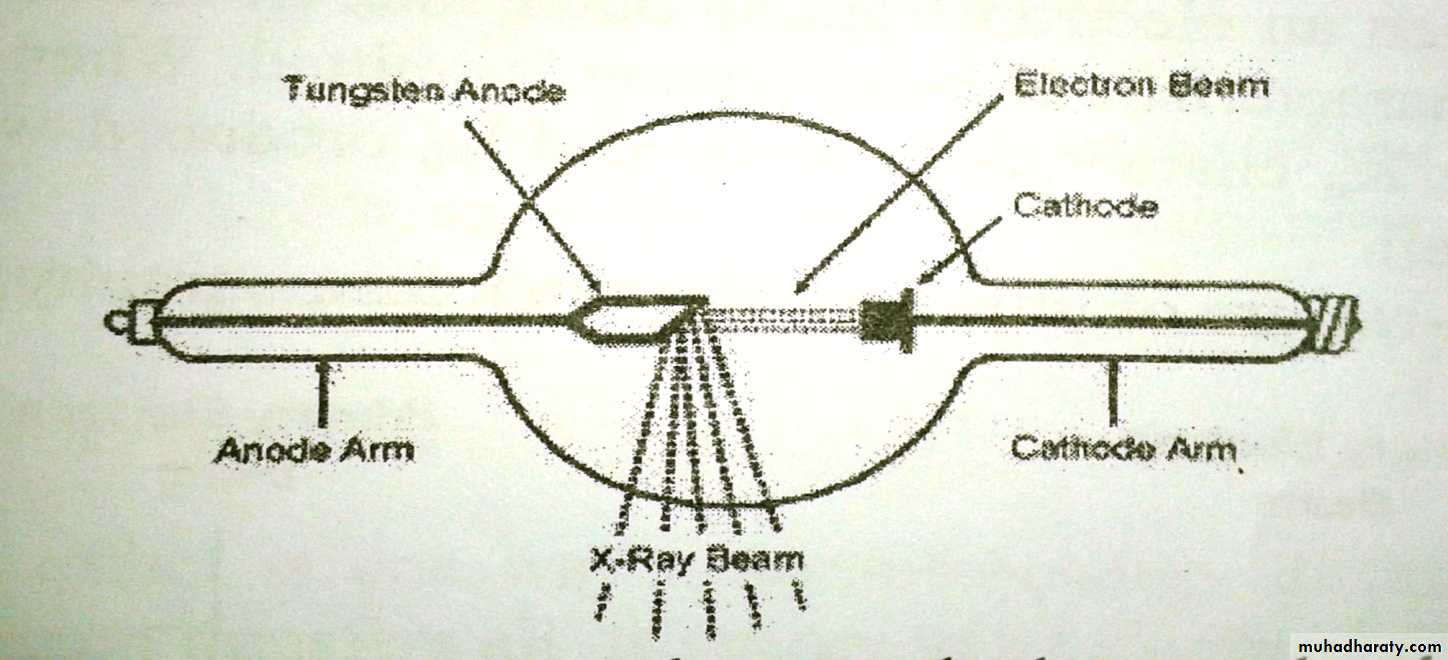
X-ray productionComponent of X-ray tube
Types of X-Ray
X-ray interaction with matter
X-Ray cassette
Fluoroscopy
CT
Production of X-ray
A high speed electron can convert some or all of its energy into an x-ray photon when it strikes an atom, and thus we need to speed up electrons to produce x-rays.Trying to speed up an electron in air is difficult since here are so many electrons on the atom. Its thus necessary to eliminate most of electrons and this done by using a glass bulb (x-ray tube ) from which most of the atoms have been evacuated.
The main component of an x-ray unit are:
• A source of electron ( a filament)• An evacuated space in which to speed up the electrons
• A high positive potential to accelerate the negative electrons
• A target ( anode) which the electrons strike to produce x-ray
The number of electrons accelerated toward the anode depends on the temperature of the filament and the maximum energy of the x-ray photons produced is determined by the accelerating voltage (kilovolt peak kVp)
The intensity of the x-ray beam produced when electron strikes the anode is highly dependent on the anode material. In general the higher the atomic number (Z) of the target the more efficiency x-rays are produced. The target material used should also have a high melting point since the heat produced when the electrons are stopped in the surface of the target is substantial. Nearly all x-ray tubes use tungsten target. The Z number of tungsten is 74 and its melting point is about 3400 ο C.
The power put into the surface of the target can be quite large. About 1% of this power converted to x-ray photons and over 99% of this power appears as heat. In an x-ray tube this power is concentrated in an anode area of only a few square millimeters, making overheating a serious problem
Most x-ray tubes have two filaments that can be interchanged to produce either large or small focal spot. The way to increase the area on the target struck by electrons to avoid overheating without increasing the blurring of the x-ray image is called line-focus principle.
The second big breakthrough in designing anodes to avoid overheating was the development of the rotating anode x-ray tube. The normal rotational rate of the anode is 3600 rpm and the heat is spread over a large area as the anode rotate
Types of X-ray
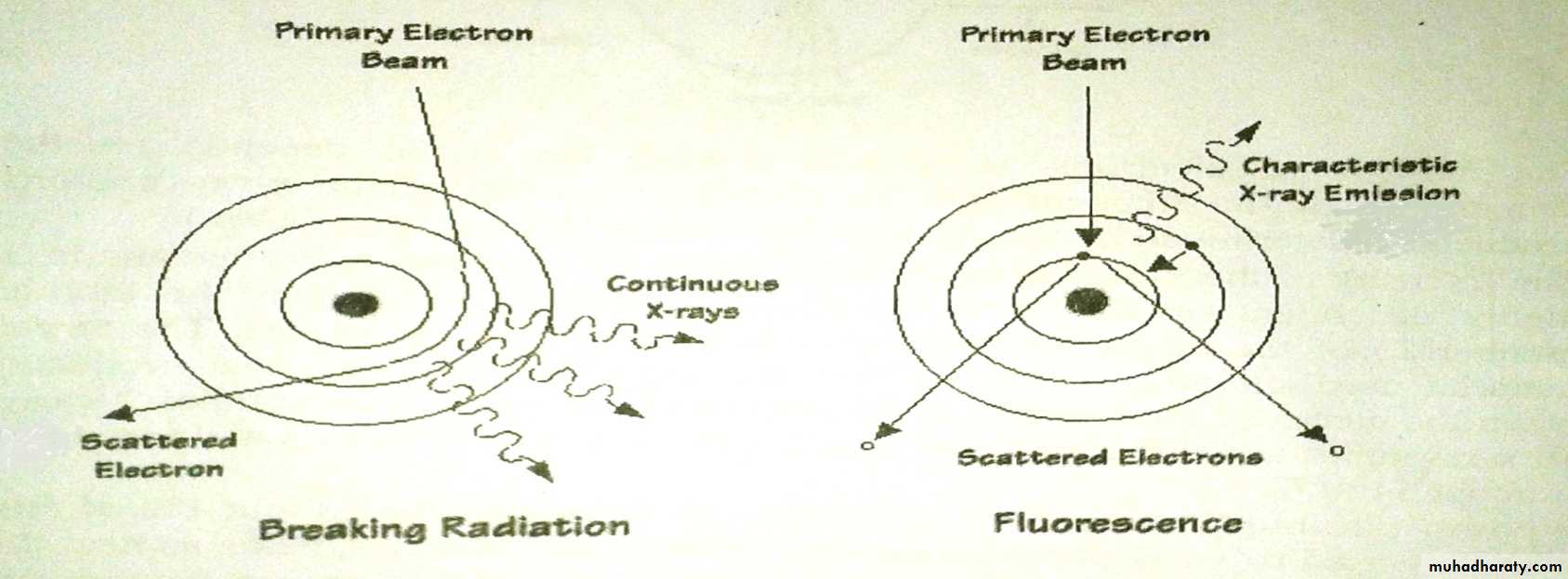
While the energy of most of the electrons striking the target is dissipated in the form of heat, the remaining few electrons produce useful x-rays. Many times one of these electrons get close enough to the nucleus of the target atom to be diverted from its path and emits an x-ray photon that has some of its energy. X-ray produced in this way called bremsstrahlung or breaking radiation. The amount bremsstrahlung produced for a given number of electrons striking the anode depends upon:• The Z of the target ( )
• The kilovolt peak ( )
Sometimes a fast electron strikes a K electron in the target atom and knocks it out of its orbit and free of the atom. The vacancy in the k shell is filled almost immediately when an electron from an outer shell of the atom falls into it and in this process a characteristic K x-ray photon is emitted. When an electron falls from L to K produce Kα characteristic x-ray and Kβ produced when the electron falls from M to K shell
Characteristic x-ray are of little use except in mammography
Interaction of x-ray with matter
X-rays are not absorbed equally well by all materials (if they were, they would not be very useful in diagnosis). Heavy element such as calcium are much better absorbers of x-ray than light elements such as carbon, oxygen and hydrogen. As a result, structures containing heavy element stand out clearly. The soft tissues (fat, muscles and tumors) all absorb about equally well and are thus difficult to distinguish from each other on an x-ray image. Of course air is poor absorber of x-ray (black on an x-ray image)The attenuation of an x-ray beam is its reduction due to the absorption and scattering of some of the photon out of the beam. The lower energy x-rays are absorbed more readily than the higher energy x-rays. The intensity of a monoenergetic x-ray beam would decrease exponentially with the thickness of absorber
I=Iοe-μx
Where e=2.718,x is the thickness of the attenuator and μ is the linear attenuation coefficient of the attenuator which is dependent on the energy of the x-ray photon (as the beam becomes harder, it decreases)
The mass attenuation coefficient μm is used to remove the effect of density when comparing attenuation in several materials.
I=Iοe-(μp)(px) =Iοe-μm(px)
Where p is the absorber density,μm is the mass attenuation of the absorber. The half-value layer (HVL) for an x-ray beam is the thickness of a given material that will reduce the beam intensity by one half.
HVL=0.0693/ μ or HVL=0.0693/ μm
FIVE BASIC DENSITIES SEEN ONCONVENTIONAL RADIOGRAPHY
Density AppearanceAir Absorbs the least x-ray and appears “blackest” on conventional radiographs
Fat Gray, somewhat darker (blacker) than soft tissue
Fluid or soft tissue Both fluid (e.g., blood) and soft tissue (e.g., muscle)have the same densities on conventional radiographs
Calcium The most dense, naturally occurring material(e.g., bones); absorbs most x-rays
Metal Usually absorbs all x-rays and appears the “whitest”(e.g., bullets, barium
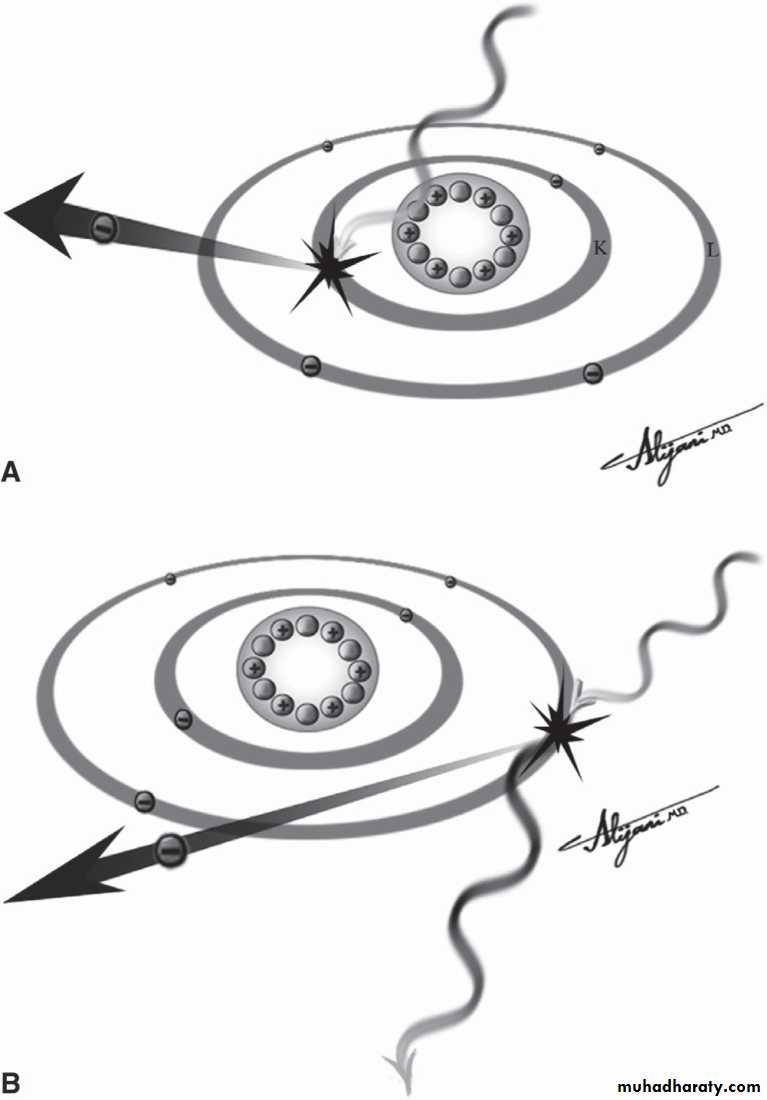
The photoelectric effect is one way x-ray lose energy in the body. It occurs when the x-ray photon transfers all its energy to an electron (mostly K electron) which then escapes from the atom. It is more common in element with which high Z than in those with low Z. for a given electron to be liberated by photoelectric effect, its binding energy must be slightly lower than the energy of the x-ray photon
Another important way x-ray lose energy in the body is by the Compton effect. In Compton effect an x-ray photon can collide with a loosely bound outer electron. At the collision, the electron receives part of the energy and the reminder is given to Compton photon which travels in a direction different from that of the original x-ray photon. The number of Compton collisions depend only on the number of electron per cubic centimeter, which is proportional to the density. The fraction of x-rays that lose energy by the Compton effect is greater in low Z elements.
A: Photoelectric effect showing the total absorption of the incidentx-ray photon and the ejection of a K-shell electron. B: Compton scatter showing theincident photon transferring kinetic energy to an outer shell electron and beingscattered with a longer wavelength (i.e., lower photon energy).
Pair production is third major way x-rays give up energy. When a very energetic photon enters the intense electric field of the nucleus, it may be converted into two particles (electron & positron). Since a minimum of 1.02MeV is necessary for a pair production, this type of interaction is not important in diagnostic radiology. Pair production is more apt to occur in high Z element than in low Z elements.
Contrast media
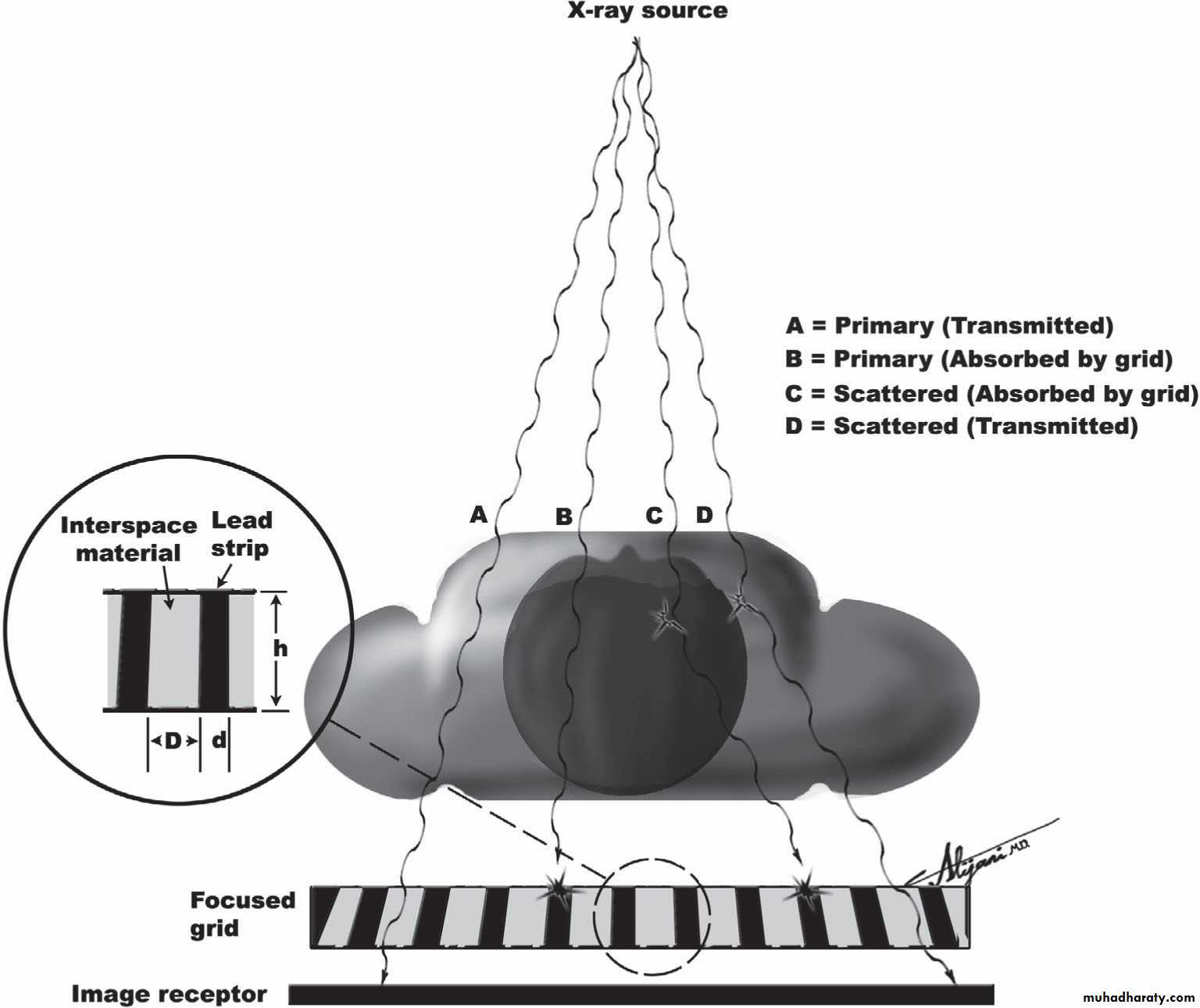
The photoelectric effect is more useful than the Compton effect because it permits us to see bones and other heavy elements. At 30keV bone absorbs x-rays about 8 times better than tissue due to the photoelectric effect. To make further use of the photoelectric effect radiologists often inject high Z materials (contrast media) into different parts of the body. Contrast media either compounds containing iodine injected into the blood stream to show the arteries or barium compounds given orally to se parts of GIT.Grids
The most significant way of reducing the amount of scattered radiation striking the film by using a grid consisting of a series of lead and plastic strips. The strips are aligned so that unscattered x-ray from the source will go through the plastic strips and strike the film while most of the scattered radiation will strike the lead strips and be absorbed. The use of grid will require a large exposure to the patient.Grids reduce the amount of scattered radiation that reaches the film.The lead strips of a focused grid are designed to be parallel to the incoming beam.
Filtration
One of the most important determinants of the radiation to the patient is the amount of filtration in the beam. Few millimeters of aluminum filtration are the most effective in reducing the patient exposure and most states require that the filtration for conventional x-ray equipment be at least equivalent of 2.5mm Al.Collimators
Collimators are devices used to collimate the x-ray beam to the size of the film being used. Collimators are used to reduce the x-ray exposure to the patient.X-ray film and cassette
X-ray film is photographic film consisting of light sensitive emulsion (silver bromide crystal) that is usually coated on both sides of a transparent sheet of plastic called the base.In cassette, the x-ray film sandwiched tightly between two intensifying screens which are cardboard covered with a thin coating of crystals that absorb x-rays well and give off visible or UV light fluoresce when struck by x-ray.
Cross section of a typical screen–film cassette containing doubleemulsion film and two screens.
Fluoroscopy
It is the process of producing live x-ray images. Fluoroscopy techniques are useful where motion such as the movement of contrast media in digestive tract must be studied. In fluoroscopy the image receptor is the image intensifier tube which consist of:• Input phosphor and photocathode
• Electrostatic focusing lens
• Accelerating anode
• Output phosphor
• The light photons from the output phosphor screen viewed by movie camera or a television camera.
Computed Tomography
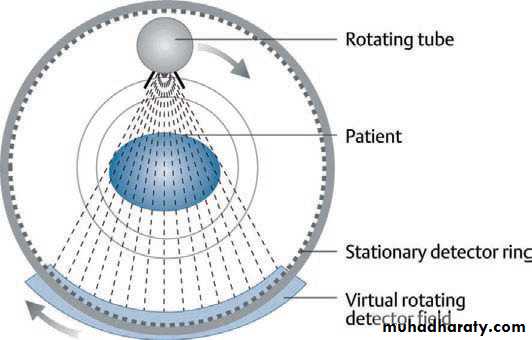
In computed tomography the x-ray tube continuously rotates around the cranio-caudal axis of the patient.A beam of radiation passes through the body and hits a ring or moving ring segment of detectors.
The incoming radiation is continuously registered, the signal is digitized and fed into a data matrix taking into account the varying beam angulations
The data matrix can then be transformed into an output image.
In today’s modern CT machines
the tube rotation continues as the patient is fed through the ringlike CT gantry, thus generating not single slice scans but spiral volume scans of larger body segments.For each picture element (pixel) the attenuation
of the radiation is calculated and expressed as Hounsfield units (HU). Water has, by definition, a Hounsfield unit value of 0.
This is a modern volume CT scanner
The x-ray tube rotates continuously around the longitudinal axis of the patient. A rotating curved detector field oppositeto the tube registers the attenuated fan beam after it has passed through the patient. Taking into account the tube position at eachtime point of measurement, the resulting attenuation values are fed into a data matrix and further computed to create an image.