
1
Inguinal hernia
The most common hernia in men and women. Its types:
Lateral (oblique, indirect), congenital
Medial (direct), acquired hernia
Sliding
Walls of the Inguinal Canal
The anterior wall of the canal is: formed along its entire length by the aponeurosis
of the external oblique. It is reinforced in its lateral third by the origin of the
internal oblique from the inguinal ligament. This wall is therefore strongest where
it lies opposite the weakest part of the posterior wall namely the deep inguinall
ring.
The posterior wall of the canal is formed along its tire length by the fascia
transversalis. It is reinforced in its' the tendon Of 9 third by the conjoint tendon,
the common tendon of insertion Of the internal Oblique and transversus which is
attached to the pubic crest and pectineal line. This wall is therefore strongest
where it lies opposite the weakest part of the anterior wall namely the superficiall
inguinal ring.
The inferior wall or floor Of the canal is formed by the rolled-under inferior edge
of the of the external oblique muscle, namely the inguinal ligament and at its
medial end, the lacunar ligament.
The inguinal canal
In the male contains the testicular artery, veins, lymphatics and the vas deferens.
In the female, the round ligament descends through the canal to end in the vulva.
Three important nerves: the ilioinguinal, the iliohypogastric and the genital branch
of the genitofemoral nerve also pass through the canal.
As the testis descends, a tube of peritoneum is pulled with the testis and wraps
around it ultimately to form the tunica vaginalis.

2
This peritoneal tube should obliterate ,fails to fuse either in part or totally, Inguinal
hernia in neonates and young children is always of this congenital type
An indirect hernia is lateral as its origin is lateral to the inferior epigastric vessels
Direct inguinal hernia
The second type of inguinal hernia, referred to as direct or medial, is acquired
It is a result of stretching and weakening of the abdominal wall just medial to the
inferior epigastric (IE).
Hasselbach’s triangle, whose three sides are the IE vessels laterally, the lateral
edge of the rectus abdominus muscle medially and the pubic bone below
This area is weak as the abdominal wall here only consists of transversalis fascia
covered by the external oblique aponeurosis.
More likely in elderly
Unlikely to strangulate
Sliding hernia.
Acquired hernia due to weakening of the
Abdominal wall but this occurs at the deep inguinal ring lateral to the IE vessels.
However the sac has formed secondarily
On the left side, sigmoid colon may be pulled into a sliding hernia and on the right
side the caecum
Occasionally, both lateral and medial hernias are present in the same patient
(pantaloon hernia).
Classification
The European Hernia Society has recently suggested a simplified system of:
• Primary or recurrent (P or R);
• Lateral, medial or femoral (L, M or F);
• Defect size in finger breadths assumed to be 1.5 cm.
A primary, indirect, inguinal hernia with a 3-cm defect size would be PL2.
Diagnosis of an inguinal hernia
Usually these hernias are reducible presenting as intermittent swellings, lying
above and lateral to the pubic tubercle with an associated cough impulse
If an inguinal hernia becomes irreducible and tense there may be no cough
impulse
Require urgent investigation by either ultrasound or CT scan
Differential diagnosis

3
1. lymph node groin mass
2. abdominal mass
3. hydrocoele
4. testicular swelling.
5. saphena varix
6. varicocoele.
Management of inguinal hernia
Herniotomy and herniorrhaphy
Open suture repair
Sutures are now placed between the conjoint tendon above and the inguinal
ligament below(Bassini’s repair)
Open flat mesh repair
Lowered hernia recurrence rates and accelerated postoperative recovery
Open plug/device/complex mesh repair
Emergency inguinal hernia surgery only 5 per cent present as an emergency with a
painful irreducible hernia which may progress to strangulation and possible bowel
infarction.
Complications of inguinal hernia surgery
Immediate complications
Bleeding (which may be due to accidental
Damage to the inferior epigastric or iliac vessels)
Urinary retention
Anesthetic related
Next week: Seroma formation and wound infection
In the longer term: hernia recurrence and chronic pain
Evidence shows that mesh repairs have lower recurrence rates than suture
repairs
Damage to the testicular artery can lead to testicular infarction
Femoral hernia
The iliac artery and vein pass below the inguinal ligament to become the femoral
vessels in the leg. The vein lies medially and the artery just lateral to the vein with
the femoral nerve lateral to the artery.
Just medial to the vein is a small space containing fat and some lymphatic tissue
(node of Cloquet).
This space which is exploited by a femoral hernia
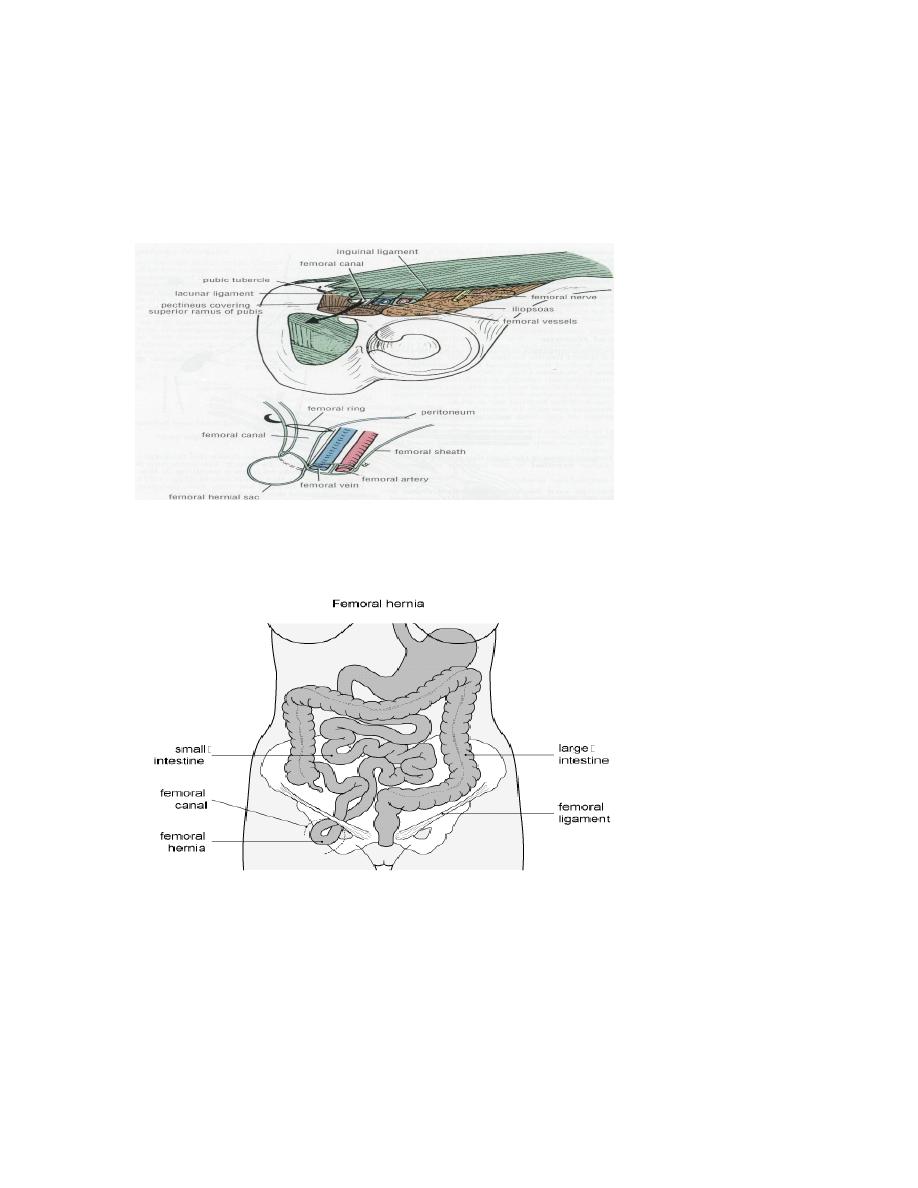
4
The walls of a femoral hernia are the femoral vein laterally,the inguinal ligament
anteriorly, the pelvic bone covered by theileopectineal ligament (Astley Cooper’s)
posteriorly and the lacunar ligament (Gimbernat’s) medially
Diagnosis of femoral hernia
Less common than inguinal hernia
It is more common in females than in males
Easily missed on examination
Fifty per cent of cases present as an emergency with very high risk of strangulation

5
The hernia appears below and lateral to the pubic tubercle and lies in the upper leg
rather than in the lower abdomen.
The hernia often rapidly becomes irreducible and loses any cough impulse due to
the tightness of the neck.
Easily be mistaken for a lymph node
If there is uncertainly then ultrasound or CT should be requested.
Plain x-ray
Differential diagnosis
1. Direct inguinal hernia
2. Lymph node
3. Saphena varix
4. Femoral artery aneurysm
5. Psoas abscess
6. Rupture of adductor longus with haematoma
Surgery for femoral hernia
1. Low approach (Lockwood
2. The inguinal approach (Lotheissen
3. High approach (McEvedy
4. Laparoscopic approach
6
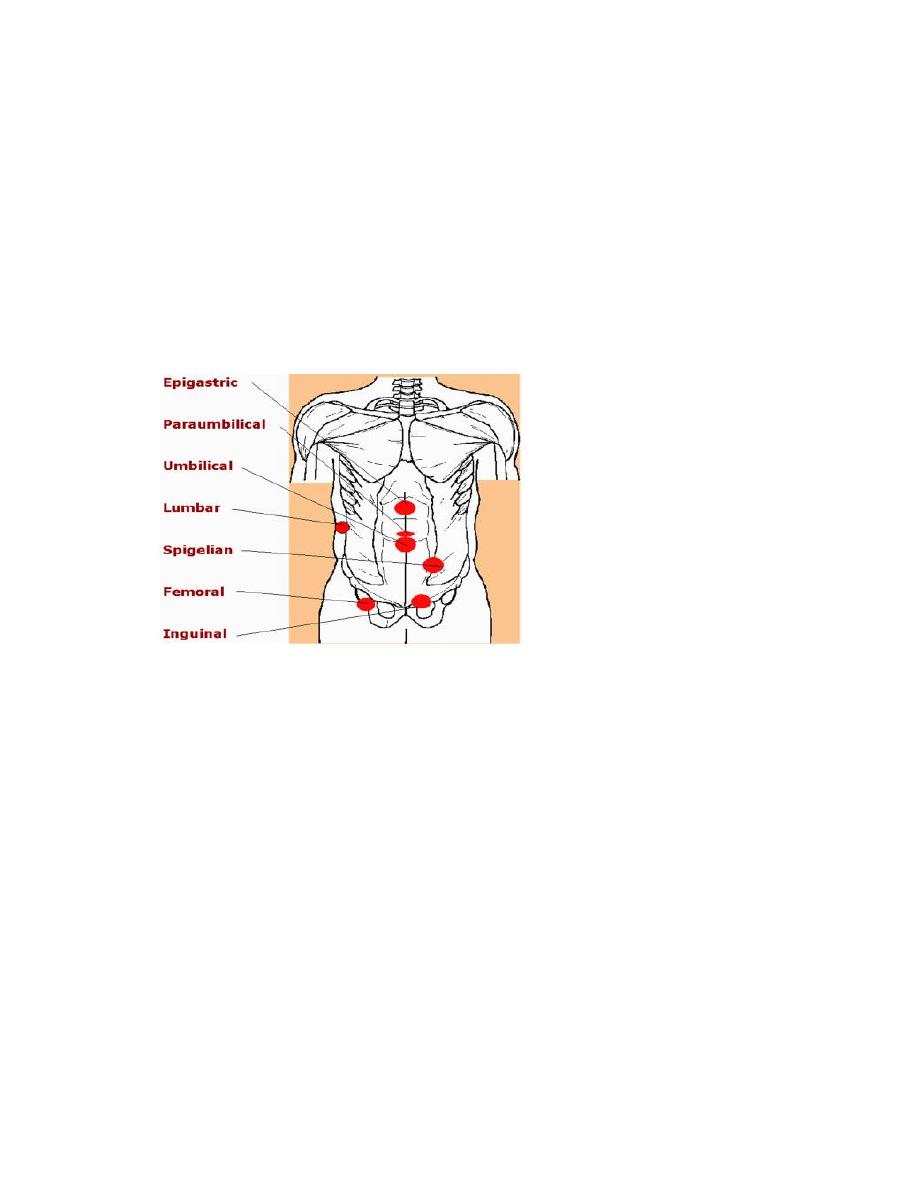
Ventral hernia
1. Umbilical – paraumbilical
2. Epigastric
3. Incisional
4. Parastomal
5. Spigelian
6. Lumbar
7. Traumatic
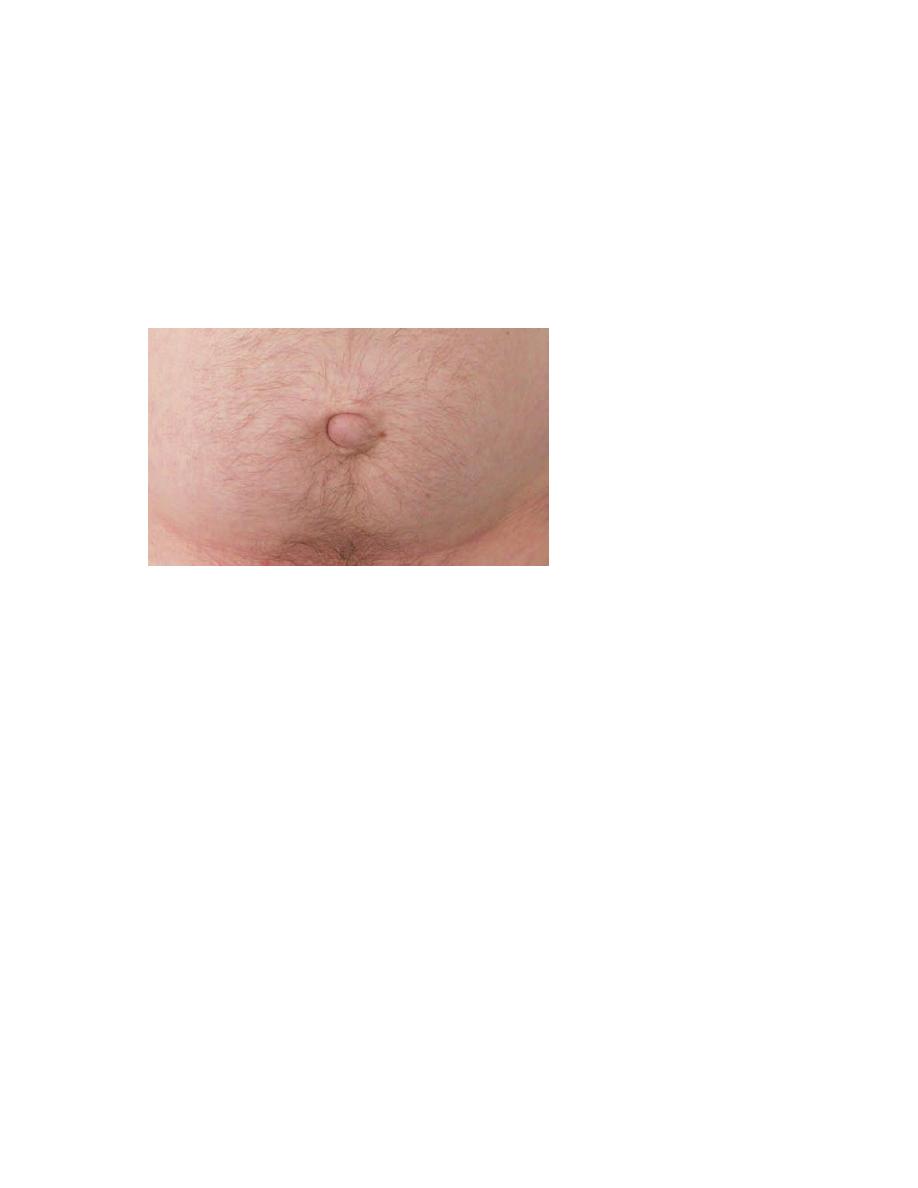
Umbilical hernia
The umbilical defect is present at birth but closes as the stump of the umbilical
cord heals, usually within a week of birth.
This process may be delayed, leading to the development of herniation in the
neonatal period.
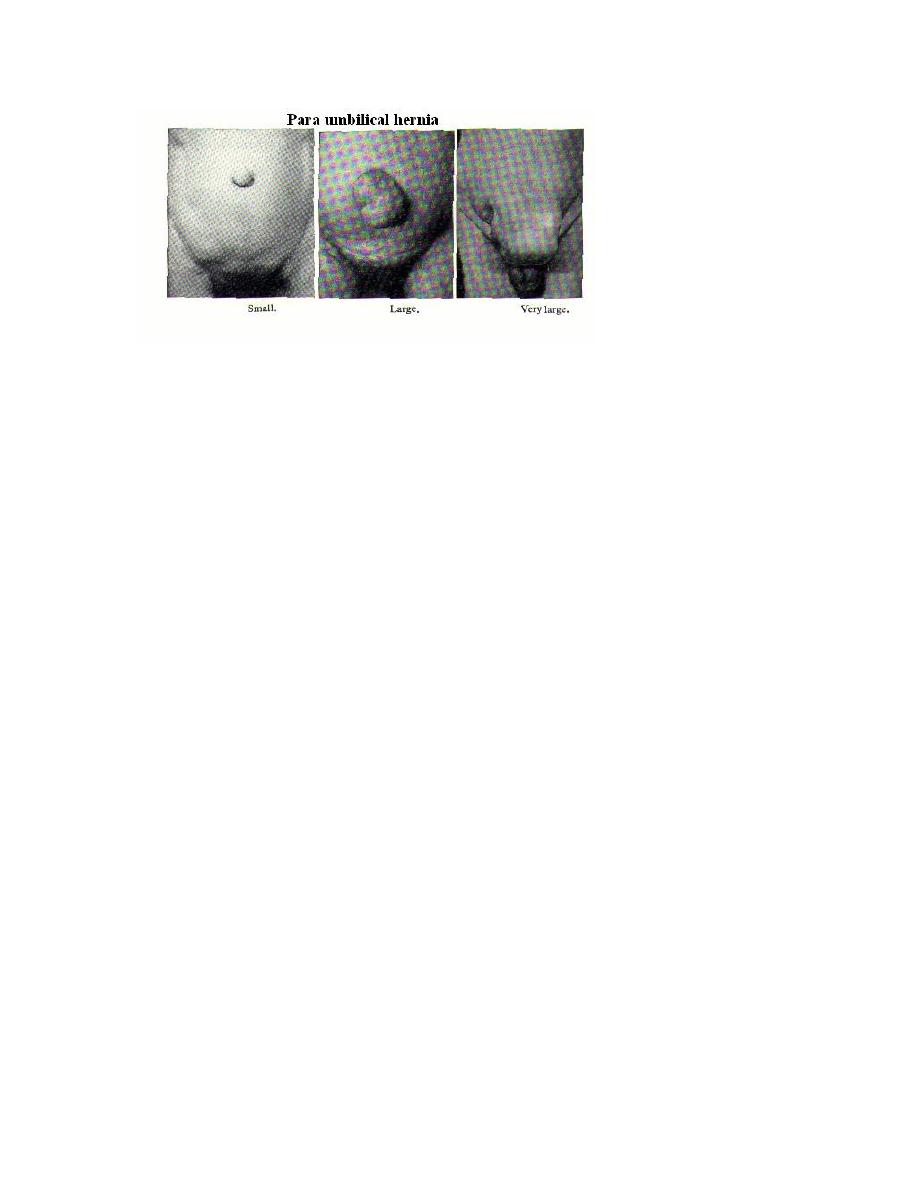
Umbilical hernia in adults
Conditions which cause stretching and thinning of the midline raphe (linea alba),
such as pregnancy, obesity and liver disease with cirrhosis, predispose to
reopening of the umbilical defect
Small umbilical hernias often contain extraperitoneal fat or omentum. Larger
hernias can contain small or large bowel
7
Clinical features
Commonly overweight
The bulge is typically slightly to one side of
the umbilical depression, creating a crescent-shaped appearance to the umbilicus
Women are affected more
Pain due to tissue tension or symptoms of intermittent bowel obstruction
Overlying skin may become thinned,stretched and develop dermatitis.
Treatment
Because of the high risk of strangulation, operation should be advised in cases
where the hernia contains bowel
Surgery may be performed open or laparoscopically.
Open umbilical hernia repair: for defects larger than 2 cm in diameter, mesh
repair is recommended
The mesh may be placed in one of several anatomical planes:
Within the peritoneal cavity
In the retromuscular space
In the extraperitoneal space
In the subcutaneous plane (onlay mesh)
8
Epigastric hernia
• arise through the midline raphe (linea alba) anywhere between the
xiphoid process and the umbilicus, usually midway
• begin with a transverse split
• in contrast to umbilical hernias, the defect
is elliptical.
• defect occurs at the site where small blood vessels pierce the linea
alba
• More likely, that it arises at weaknesses due to abnormal decussation
of aponeurotic fibres related to heavy physical activity
• Epigastric hernia defects are usually less than 1 cm in maximum
diameter
• commonly contain only extraperitoneal fat
• gradually enlarges, spreading in the subcutaneous plane to resemble
the shape of a mushroom.
• When very large they may contain a peritoneal sac but rarely any
bowel.
• More than one hernia may be present.
Clinical features
• patients are often fit, healthy males between 25 and 40 years of age.
• can be very painful
• The pain may mimic that of a peptic ulcer
soft midline swelling
• unlikely to be reducible because of the narrow neck
• A cough impulse may or may not be felt.

9
• Very small epigastric hernias disappear
Spontaneously
• surgery should only be offered if the hernia
is sufficiently symptomatic.
• open or laparoscopic surgery
Incisional hernia
• These arise through a defect in the musculofascial layers of the
abdominal wall in the region of a postoperative scar
• Incidence 10–50 per cent after surgery
1–5 per cent of laparoscopic port-site
incisions.
Predisposing Factors
• Patient factors (obesity, general poor healing due to malnutrition,
immunosuppression or steroid therapy, chronic cough, cancer
• wound factors (poor quality tissues, wound infection)
• Surgical factors (inappropriate suture material, incorrect suture
placement
• starts as disruption of the musculofascial
layers of a wound in the early postoperative period.
• The classic sign of wound disruption is a serosanguinous discharge.
Clinical features
• localized swelling involving a small portion of the scar but may
present as a diffuse bulging of the whole length of the incision
• increase steadily in size with time
• Strangulation is less frequent ,incisional hernias are broad-necked
Treatment
• Asymptomatic incisional hernias may not require treatment at all.
The wearing of an abdominal binder or belt may prevent the hernia
from increasing in size.
Principles of surgery
• The repair should cover the whole length of the previous incision.
• Approximation of the musculofascial layers should be done with
minimal tension
• prosthetic mesh should be used
• Mesh may be contraindicated in a contaminated field,

10
Operations
• Open repair
• Retromuscular sublay mesh repair
• Laparoscopic repair
