HYPERTENSION
Dr. Sabah ZanganaHYPERTENSION
DEFINITIONEPIDEMIOLOGY
AETIOLOGY-PATHOGENESIS
PATHOLOGY-TARGET ORGAN DAMAGE
CLINICAL MANIFESTATION
INVESTIGATION-EVALUATION
MANAGEMENT
SPECIAL ISSUES
QUESTION ABOUT HYPERTENSION
Is the patient hypertensive?(diagnosis)How to measure BP
(What is Home and ambulatory blood pressure recordings )
In the epidemiology,what is the control rate?
In symptomatology --What is the relation of headache to HT?
Why to treat hypertension?(Objective)
How to Evaluate a patient with Hypertension
Is their sudden lowering of BP??
When to treat (Threshold)?
What treatment targets we should reach?
What choice of antihypertensive drug ?
When to use adjuvnt drugs like aspirin or statins
What is central (vs.peripheral )BP
WHY WE TREAT HYPERTENSION?
OBJECTIVE
Reduce the incidence of
adverse Cardio-Vascular events55-year-old woman
65-year-old manexactly the same BP150/90
average BP150/90
Not smoker
Smoker
Not diabetic
diabetic
total:HDL cholesterol of 6
total:HDL cholesterol of 8
Normal ECG
ECG changes of LVH
predicted 10-year CHD risk < 14%;
10-year CHD risk = 68%
AHT prevent fewer than 3 events per 1000 patient years of treatmentAHT(assuming 20% relative risk reduction) prevent 14 coronary events for every 1000 patient years of treatment
Questionable
Advisable
Definition
A condition in which arterial BP is
chronically elevated.
BP occurs within a continuous range
cutoff levels -- defined according to their effect on patients' risk
Clinical definition
practical definition of hypertension is 'the level of BP at which the benefits of treatment outweigh the costs and hazards'
Ranges of blood pressure
normal range <----- hypertension
High blood pressure is a trait as opposed to a specific disease - represents a quantitative rather than a qualitative deviation from the norm. Any definition of hypertension is therefore arbitrary
-
Clinical Criteria
1-average of two or more seated blood pressure readings
2-during each of two or more outpatient visits.
Recent classification
normal blood pressure,prehypertension,
hypertension (stages I and II), and
isolated systolic hypertension
DEFINITION OF HYPERTENSION
Category Systolic BP Diastolic BP
1-BP
Optimal < 120 < 80
Normal < 130 < 85
High normal(PRE)130-139 85-89
2-Hypertension
Grade 1 (mild) 140-159 90-99
Grade 2 (mod.) 160-179 100-109
Grade 3 (sev.) ≥180 ≥110
3-Isolated S.HT
Grade 1 140-159 < 90
Grade 2 ≥160 < 90
-
• 180
• 179
• 160
• 159
• 140
• 139
• 129
• 119
• 110
• 109
• 100
• 99
• 90 95
• 89
• 85
• 80
Epidemiology
1/4th.
50 million USA
1 billion worldwide
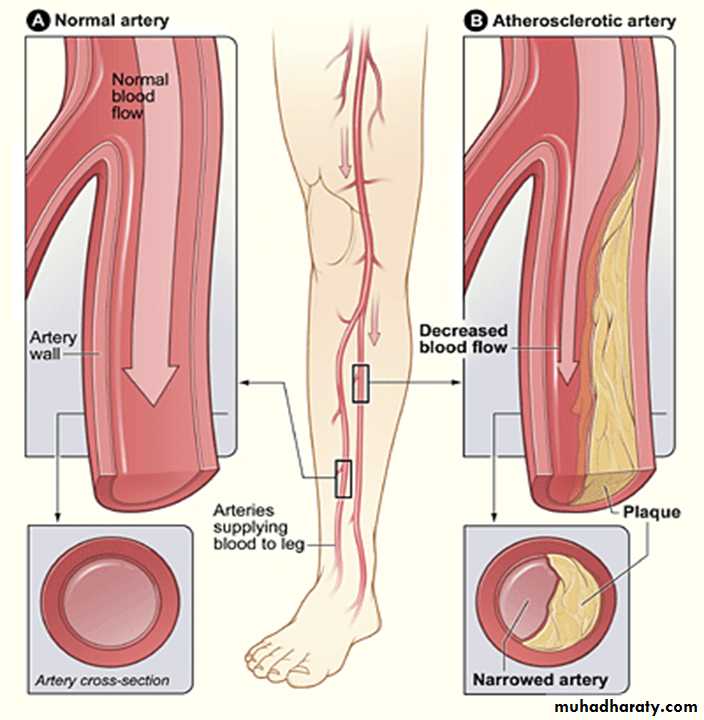
Most widely recognized treatable risk factor for
stroke ,myocardial infarction ,
heart failure ,
peripheral vascular disease ,
aortic dissection ,and
chronic renal failure
Aetiology
1-ESSENTIAL- 95%,2-SECONDARY-5%
RENAL
ENDOCRINE
DRUGS
Alcohol Obesity Pregnancy Co-arct.
CAUSES OF SECONDARY HYPERTENSION
Alcohol
Obesity
Pregnancy (pre-eclampsia)
Renal disease
Renal vascular disease
Parenchymal renal disease, particularly glomerulonephritis
Polycystic kidney disease
Endocrine disease
Phaeochromocytoma
Cushing's syndrome
Primary hyperaldosteronism (Conn's syndrome)
Hyperparathyroidism
Acromegaly
Primary hypothyroidism
Thyrotoxicosis
Congenital adrenal hyperplasia due to 11-β-hydroxylase or 17-hydroxylase deficiency
Liddle's syndrome
11-β-hydroxysteroid dehydrogenase deficiency
Drugs
Oral contraceptives containing oestrogens,
anabolic steroids,
corticosteroids,
non-steroidal anti-inflammatory drugs,
carbenoxolone,
sympathomimetic agents
Coarctation of the aorta
MECHANISM
• HYPERTENSION
• CARDIAC OUTPUT
• PER. RESISITANCE
• STROKE VOLUME
• HEART RATE
• LUMEN DIAMETER
MECHANISM
1-Intravascular VolumeSodium is predominantly an extracellular ion and is a primary determinant of the extracellular fluid volume.
2-Autonomic Nervous System
The autonomic nervous system maintains cardiovascular homeostasis via pressure, volume, and chemoreceptor signals. Adrenergic reflexes modulate blood pressure over the short term, and adrenergic function, in concert with hormonal and volume-related factors, contributes to the long-term regulation of arterial pressure
3-Renin-Angiotensin-Aldosterone
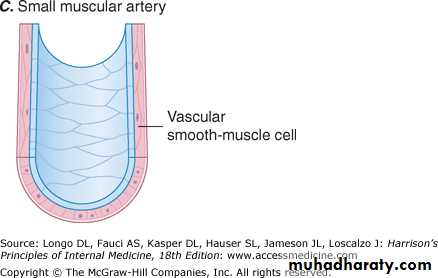
4-Vascular Mechanisms
Resistance to flow varies inversely with the fourth power of the radius
pathogenesis
factors contributing,renal function,
the peripheral resistance vessel tone,
endothelial dysfunction ,
autonomic tone,
insulin resistance and
neurohumoral.
Genetic- 40-60%.
Environmental factors
high salt intake,
heavy consumption of alcohol,
obesity,
lack of exercise and
impaired intrauterine growth.
Initial Evaluation for Hypertension
HISTORY,PHYSICAL EXAM.&INVESTIGATIONS
STEP 1:
ACCURATE ASSESSMENT OF BLOOD PRESSURESTEP 2:
CARDIOVASCULAR RISK STRATIFICATION
target organ damage
co-morbid conditions (for atherosclerosis)
STEP 3:
IDENTIFICATION OF SECONDARY (IDENTIFIABLE) CAUSES
History
Causes and complicationsFamily history,
lifestyle (exercise, salt intake, smoking habit)
other risk factors.
drug- or alcohol-induced hypertension
symptoms of other causes of
secondary hypertension
complications
Examination
Causes and complications,
causes of secondary hypertension
Radio-femoral delay (coarctation of the aorta,
enlarged kidneys (polycystic kidney disease),
abdominal bruits (renal artery stenosis)
characteristic facies and habitus of Cushing's syndrome
important risk factors
central obesity
hyperlipidaemia (tendon xanthomas etc.). .
Non-specific findings –
left ventricular hypertrophy (apical heave),accentuation of the aortic component of the second HS, and
fourth heart sound.
The optic fundi are often abnormal
evidence of generalised atheroma or
specific complications e.g. aortic aneurysm or peripheral vascular disease
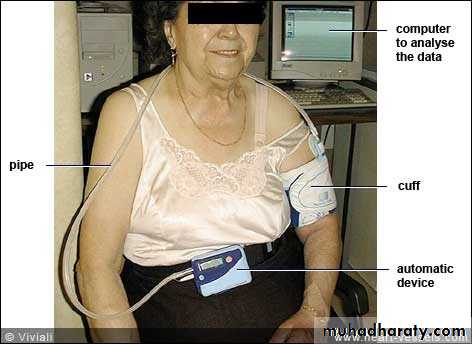
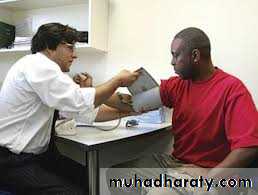
STEP 1MEASUREMENT OF BLOOD PRESSURE
1-OFFICE BLOOD PRESSURE. .2-HOME BLOOD PRESSURE MONITORING
3-AMBULATORY BLOOD PRESSURE MONITORING
Measurement of blood pressure
MEASUREMENT OF BLOOD PRESSURE
Office BPMachine validated, well maintained and properly calibrated
Sitting routinely +standing BP
in elderly and diabetic
possible postural hypotension
Remove tight clothing
Support the arm at the level of the heart
Use a cuff of appropriate size > two-thirds of the arm)
Lower the mercury slowly (2 mm per second)
Read the BP to the nearest 2 mmHg
phase V (disappearance of sounds) = measure diastolic BP
Take two measurements at each visit
-
Home and Ambulatory BP recording
Transient rise in BP
Exercise,
anxiety,
discomfort
unfamiliar surroundings.
Unrepresentative surge in BP ('white coat' hypertension )
20% of patients with apparent hypertension in the clinic may have a 'normal BP' when it is recorded by automated devices used in their own home.
helpful in patients with
1-unusually labile blood pressure,2-those with refractory hypertension,
3- those who may be experiencing symptomatic hypotension
4-those in whom white coat hypertension is suspected
-
2-AMBULATORY BP recording
over 24 hours.
measurements correlate more closely with evidence of target organ damage than casual BP measurements.
treatment thresholds and targets must be adjusted downwards because ambulatory BP readings are systematically lower (approximately 12/7 mmHg) than clinic measurements;
3- HOME BP recording
real value = not well established
STEP 2 CARDIOVASCULAR RISK STRATIFICATION
Co-morbidity (for atherosclerosis)Smoking
Hypercholesterolaemia
Diabetes mellitus
Physical activity Obesity Alcohol
Target organ damage
Chronic=
Acute= malignant
The adverse effects of hypertension(TARGET ORGAN DAMAGE)
1-DIRECT-vascular changes2-INDIRECT-ATHEROSCLEOSIS
ON
1-BLOOD VESSLES
2-HEART
3-CNS AND RETINA
4-KIDNEYS
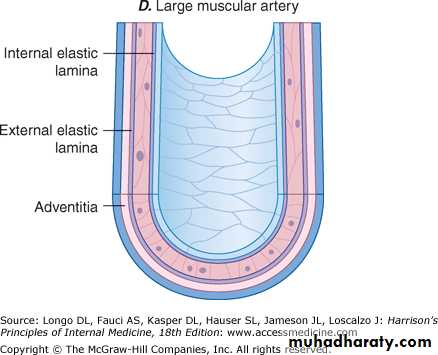
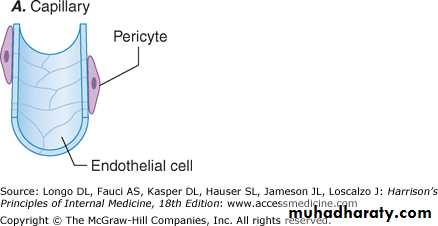
1-Blood vessels (peripheral)
In larger arteries (over 1 mm in diameter)
IEL &Muscle
dilate
tortuous
walls less compliant.
In smaller arteries (under 1 mm)
hyaline arteriosclerosislumen narrows
aneurysms.
Widespread atheroma coronary and/or cerebrovascular disease,
structural changes in the vasculature perpetuate and aggravate hypertension (by increasing peripheral vascular resistance and reducing renal function).aortic aneurysm and aortic dissection
2- Retina-BV
linked to severity of hypertension;indication of arteriolar damage occurring elsewhere
TYPE OF LESION
'Cotton wool' exudates -associated with retinal ischaemia or infarction, and fade in a few weeks .
'Hard' exudates (small, white, dense deposits of lipid) and microaneurysms ('dot' haemorrhages) are more characteristic of diabetic retinopathy)
Hypertension =associated with central retinal vein thrombosis
HYPERTENSIVE RETINOPATHY
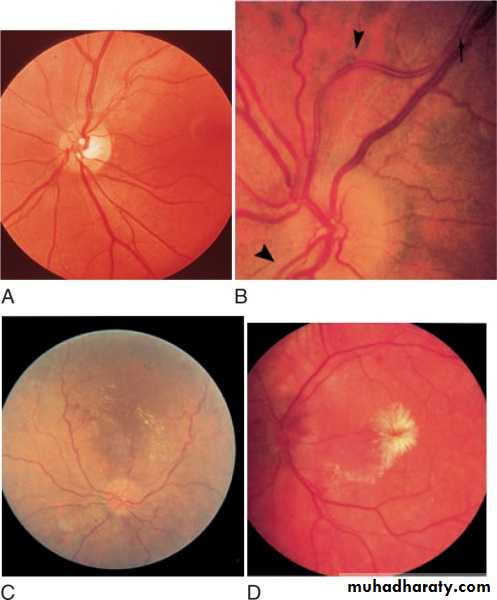
Grade 1 Arteriolar thickening, tortuosity and increased reflectiveness ('silver wiring')Grade 2 Grade 1 plus constriction of veins at arterial crossings ('arteriovenous nipping')Grade 3 Grade 2 plus evidence of retinal ischaemia (flame-shaped or blot haemorrhages and 'cotton wool' exudates)•Grade 4 Grade 3 plus papilloedema
A= Grade 1 Increased tortuosity of a retinal vessel and increased reflectiveness (silver wiring) B= Grade 2 = 1 + “nipping” of venules at A-V crossings C= Grade 3 grade 2 plus flame-shaped retinal hemorrhages and soft “cotton wool” exudates D= grade 4 swelling of optic disc (papilledema), retinal edema , and hard exudates around the fovea, producing a typical “macular star
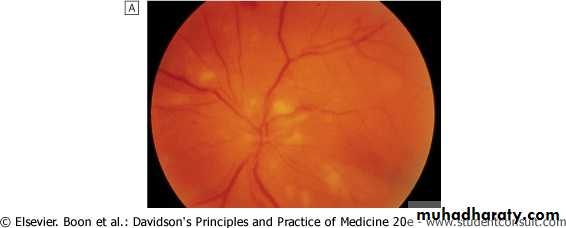
Grade 4 hypertensive retinopathy showing swollen optic disc, retinal haemorrhages and multiple cotton wool spots (infarcts).
Central retinal vein thrombosis -- swollen optic disc and widespread fundal haemorrhage, =systemic hypertension
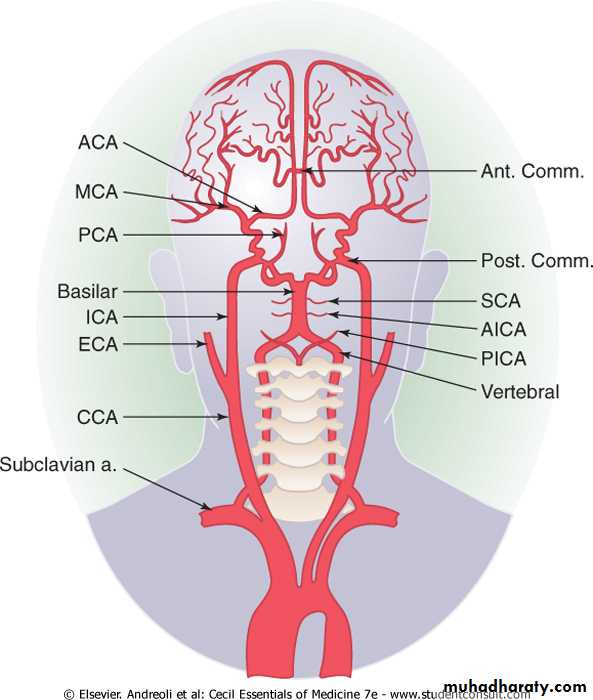
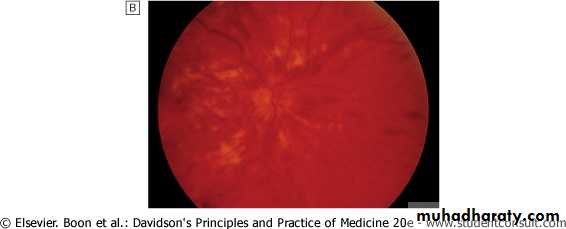
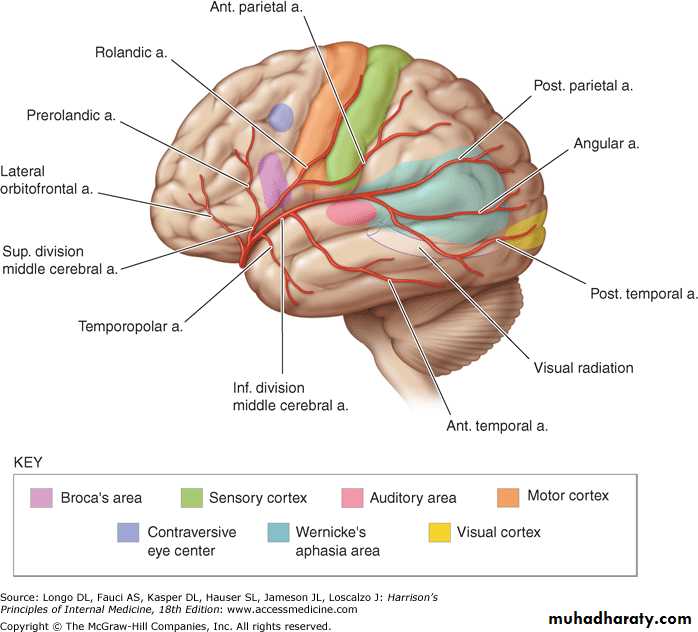
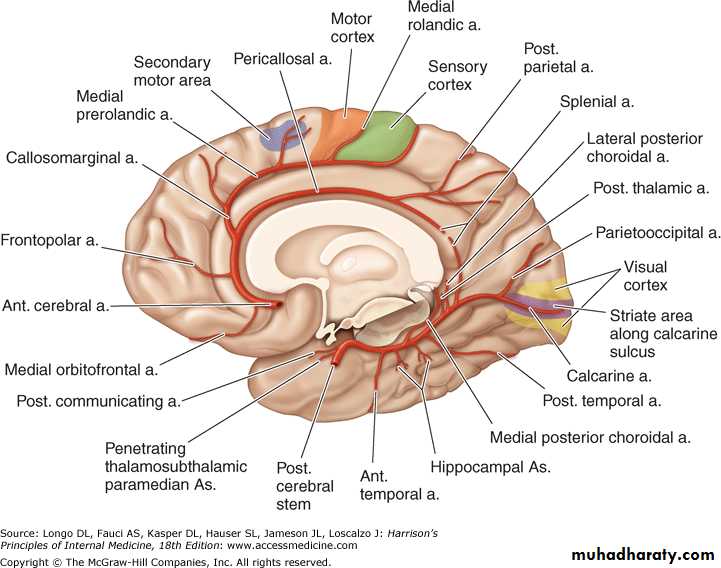
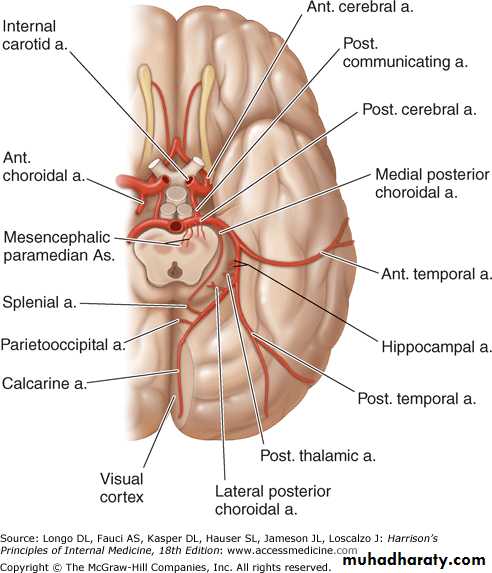
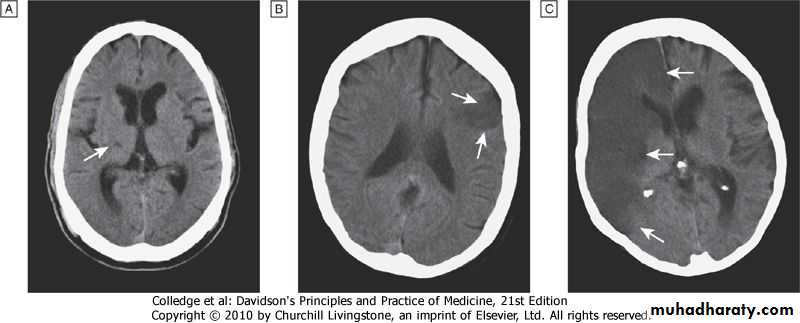
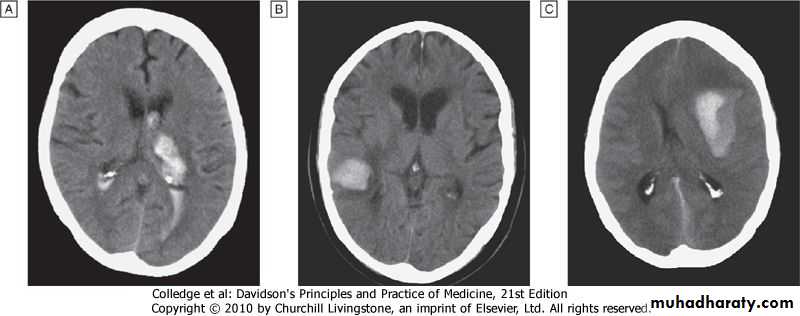
3-CNS
3-Central nervous systemBV+PARENCHYMA
1-Stroke -2- Carotid atheroma + transient cerebral ischaemic attacks.
3- Subarachnoid haemorrhage
4-Hypertensive encephalopathy
high blood pressure+ neurological symptoms,
Papilloedema is common.
CT scan = haemorrhage in and around basal ganglia
neurological deficit = usually reversible
if hypertension is properly controlled
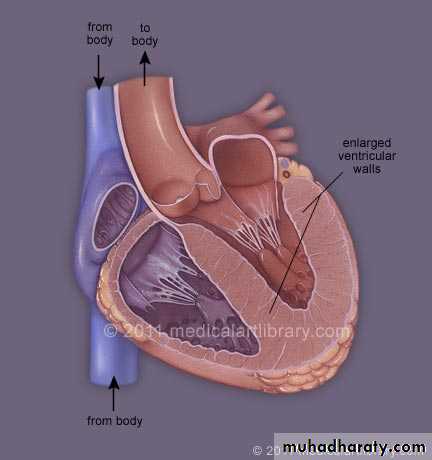
4-Heart
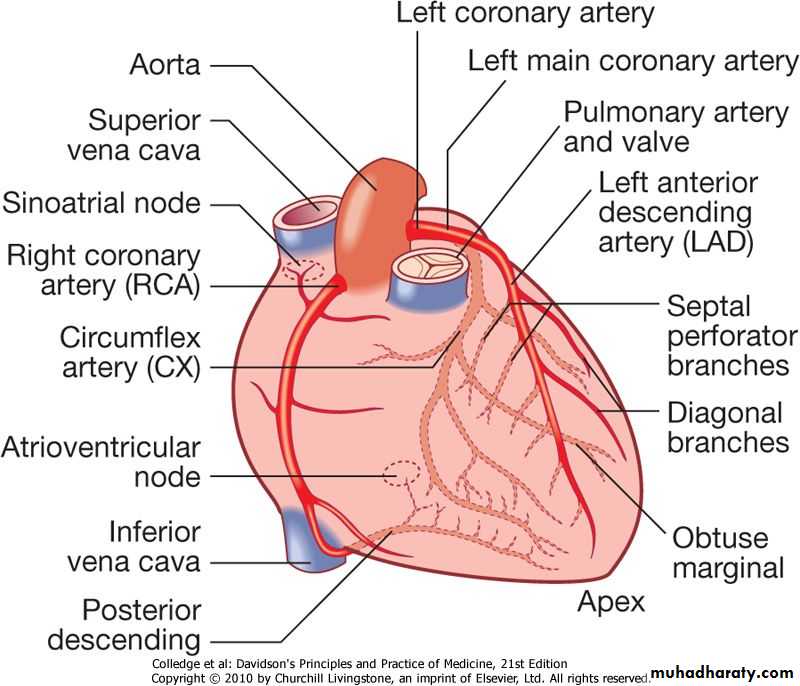
INDIRECTHigher incidence of CAD.
DIRECT
1-High blood pressure left ventricular hypertrophy
forceful apex beat
S4.
ECG or echocardiographic =risk assessment.
2-Severe hypertension => left ventricular failure3-Atrial fibrillation= common =
diastolic dysfunction caused by
left ventricular hypertrophy or
effects of coronary artery disease
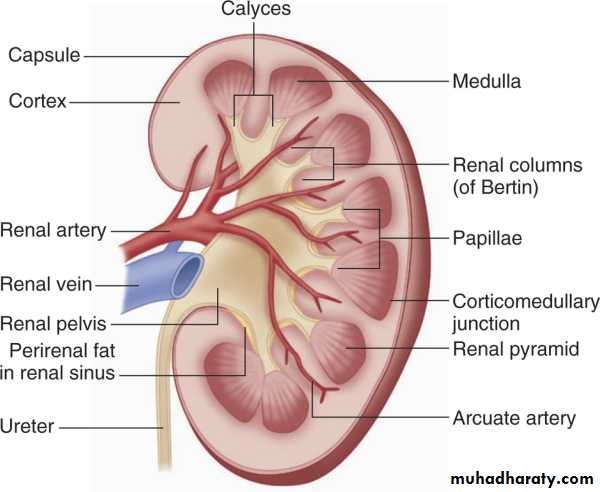
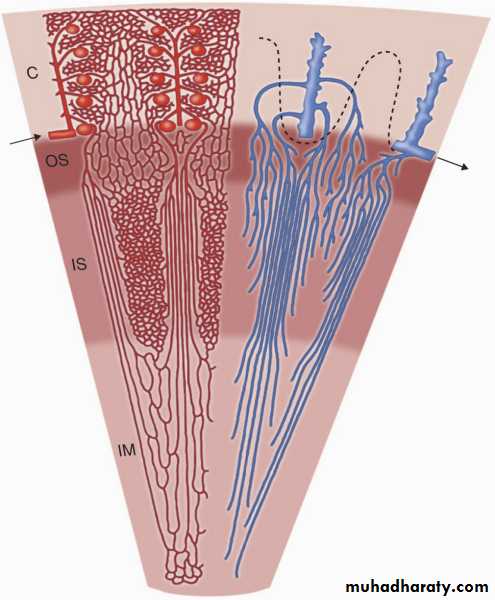
5-KIDNEYS
5- Kidneys-BV
Long-standing hypertension (by damaging renal vasculature) proteinuria
progressive renal failure
TYPES
1-Direct=Hypertensive nephropathy-
small and large arteries=chronic renal ischaemia
2-Indirect=Progressive nephroscleosis-atheroscletotic vascular dis. like cornary a. and cerbral a.
Proteinuria = severity of chronic kidney disease
1-Preglomerular arterioles, Atherosclerotic => ischemic changes in glomeruli and postglomerular structures.2- Glomerular injury = direct damage to glomerular capillaries hyperfiltration, hypertrophy, and focal segmental glomerular sclerosis.
Glomerular pathology glomerulosclerosis, ->renal tubules may also become ischemic and gradually atrophic
-
.
CHRONICCardiac,Cerebrl,Renal
Effects of HTACUTE Malignant hypertension
Pathologically= fibrinoid necrosis of afferent arterioles, sometimes extending into the glomerulus, focal necrosis of glomerular tuft.
Clinically
macroalbuminuria
or microalbuminuria early markers of renal injury.
'Malignant' or 'accelerated' phase hypertension
RareAccelerated microvascular damage with
1-necrosis in walls of small arteries and arterioles ('fibrinoid necrosis') and
2- by intravascular thrombosis.
Diagnosis is based on
1- evidence of high blood pressure and
2-rapidly progressive end organ damage such as
retinopathy (grade 3 or 4),
renal dysfunction (especially proteinuria) and/or
hypertensive encephalopathy .
Left ventricular failure may occur and, if this is untreated, death occurs within months
Investigations
All hypertensive patients should undergo a limited number of investigations.
Additional investigations are appropriate in selected patients.
HYPERTENSION: A-INVESTIGATION OF ALL PATIENTS
Urinalysis for blood, protein and glucoseBlood urea, electrolytes and creatinine
N.B. Hypokalaemic alkalosis ---primary hyperaldosteronism
--- diuretic therapy
Blood glucose
Serum total and high-density lipoprotein (HDL) cholesterol
12-lead ECG (left ventricular hypertrophy, coronary artery disease
HYPERTENSION: B-INVESTIGATION OF SELECTED PATIENTS
Chest X-ray:cardiomegaly, heart failure, coarctation of the aorta
Ambulatory BP recording:
to assess borderline or 'white coat' hypertension
Echocardiogram:
left ventricular hypertrophy
Renal ultrasound:
renal disease
Renal angiography:
renal artery stenosis
Urinary catecholamines:
phaeochromocytoma
Urinary cortisol and dexamethasone suppression test:
Cushing's syndrome
Plasma renin activity and aldosterone:
primary aldosteronism
MANAGEMENT
Quantification of cardiovascular risk
Threshold for intervention
Treatment targets
Non-drug therapy
Antihypertensive drugs
Choice of antihypertensive drug
Adjuvant drug therapy
Special situations=
1-Emergency treatment of accelerated phase or malignant HT2-Refractory hypertension
MANAGEMENT
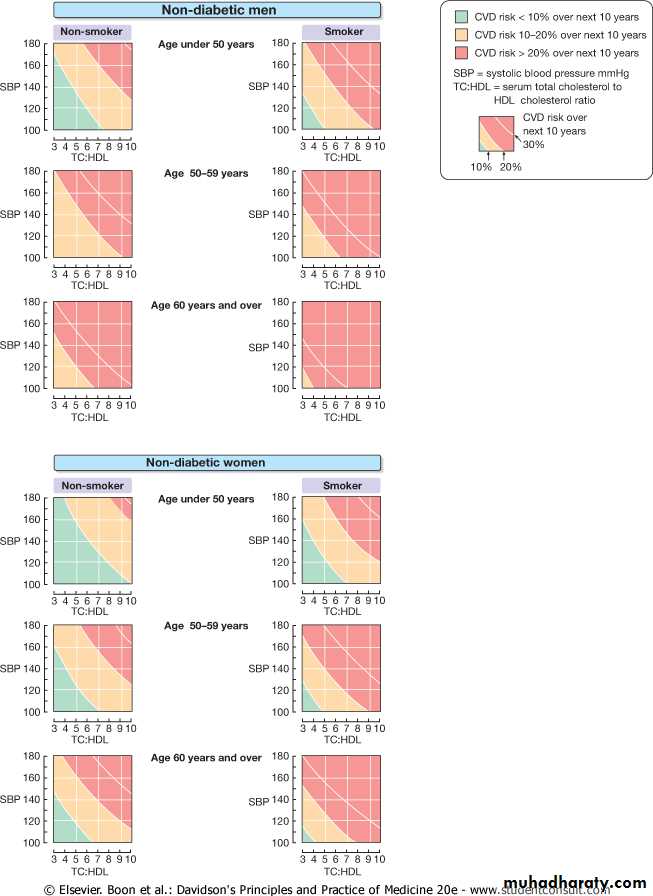
1-QUANTIFICATION OF CV RISKObjective
reduce incidence of adverse cardiovascular events
coronary heart disease / stroke and /heart failure.
Formal estimate of absolute cardiovascular risk
All the relevant risk factors and not just BP.
Most of excess morbidity and mortality associated with hypertension is attributable to CAD
many treatment guidelines based on estimates of the 10-year CAD risk.
Total cardiovascular risk = CAD risk X 4/3
ex. if coronary heart disease risk is 30%, cardiovascular risk is 40%.
Examples------
55-year-old woman
65-year-old man
exactly the same BP150/90
average BP150/90
Not smoker
Smoker
Not diabetic
diabetic
total:HDL cholesterol of 6
total:HDL cholesterol of 8
Normal ECG
ECG changes of LVH
predicted 10-year CHD risk < 14%;
10-year CHD risk = 68%
AHT prevent fewer than 3 events per 1000 patient years of treatmentAHT(assuming 20% relative risk reduction) prevent 14 coronary events for every 1000 patient years of treatment
Questionable
Advisable
-
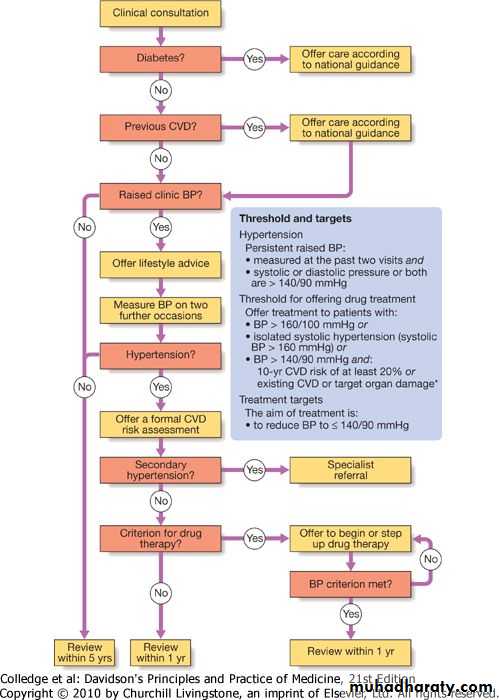
CLINICAL CONSULTATION
DM offer carePrevious CVD offer care
Raised clinic BP
offer lifestyle advise
measure BP on 2 further occasions
1-IS THE PT. HYPERTENSION??(definition?)
2- WHEN TO START TREAT.??—THRESHOLD
3-WHERE TO REACH??—TARGET BP?
4-WHAT SORT OF TREATMENT?—
CHOISE
EMERGENCY REDUCTION???
5-FOLLOWUP??
6-ADJUNAT
=
HYPERTENSION definition
Persistant raised BP=
measured at t past 2 visits+systolic or diast.P or both >140/90
Offer CVD risk assessment
Threshold for treatment
1- BP>160/100
2-Isolated systolic HT=systolic BP>160
3-BP>140/90 +
10 Y CV risk>12%
existing CVD
Target organ damage
Threshold for intervention
1-Systolic BP and diastolic BP ( predictors of cardiovascular risk).Utilize both readings
Initiate treatment if they exceed the given threshold .
TARGETS
Patients with diabetescardio-vascular disease
Renal involvement-nephrosclerosis
lower (≥ 140/90)
3-Thresholds in elderly =
same as for young
Treatment target
The optimum = 139/83 mmHg,
lower in patients with diabetes
In the UK the rule of halves
Follow up, typically at 3-month intervals,
to monitor blood pressure,
minimise side-effects and
reinforce lifestyle advice
OPTIMAL TARGET B. P. DURING ANTIHYPERTENSIVE TREATMENT
No diabetes DiabetesClinic measurements
< 140/85 < 140/80
Mean day-time
ambulatory or home measurement
< 130/80 < 130/75
N.B. Both systolic and diastolic values should be attained.
HYPERTENSION IN OLD AGE
Prevalence:
affects more than half of all people over the age of 60 (including isolated systolic hypertension).Risks:
hypertension is the most important risk factor for MI, heart failure and stroke in older people.
Benefit of treatment:
absolute benefit from anti-hypertensives is greatest in older people (at least up to 80 years).
Target BP:
similar to that for younger patients.
Tolerance of treatment:
tolerated as well as in younger patients.
Drug of choice:
low-dose thiazides, but in the presence of coexistent disease (e.g. gout, diabetes) other agents may be more appropriate.
A- Non-drug therapy
Appropriate lifestyle measures1-may obviate need for drug therapy in patients with borderline hypertension,
2- reduce dose and/or number of drugs required in patients with established hypertension, and
3- directly reduce cardiovascular risk.
A- Correcting obesity,
B-reducing alcohol intake,
C- restricting salt intake,
D- taking regular physical exercise and
E- increasing consumption of fruit and vegetables
F-quitting smoking,
G-eating oily fish and
H-adopting a diet that is low in saturated fat
can all lower blood pressure.
may produce further reductions in cardiovascular risk.B- Antihypertensive drugs
1-Thiazide and other diuretics.1- mechanism of action - incompletely understood,
2-may take up to a month for the maximum effect
3-A daily dose of
2.5 mg bendroflumethiazide or
0.5 mg cyclopenthiazide
4- More potent loop diuretics,
furosemide 40 mg daily or
bumetanide 1 mg daily,
have few advantages over thiazides in treatment
unless
substantial renal impairment or
used in conjunction with an ACE inhibitor.
=
2--Angiotensin-converting enzyme (ACE) inhibitors.
inhibit conversion of angiotensin I to angiotensin II
usually well tolerated.
Ex. enalapril 20 mg daily,
ramipril 5-10 mg daily
lisinopril 10-40 mg daily
particular care in patients - impaired renal function or renal artery stenosis =can reduce filtration pressure in glomeruli and precipitate renal failure.
Electrolytes and creatinine checked before and 1-2 weeks after
S.E = 1ST-dose hypotension, cough, rash, hyperkalaemia , renal dysfunction.
Angiotensin receptor blockers.
block angiotensin II type I receptor
have similar effects to ACE inhibitors but do not cause cough
better tolerated
Ex. losartan 50-100 mg daily,
valsartan 40-160 mg daily)
-
4-Calcium antagonists.
A-The dihydropyridines
Ex- amlodipine 5-10 mg daily
nifedipine 30-90 mg daily
effective and usually well-tolerated antihypertensive
particularly useful in the elderly.
S.E. = flushing, palpitations and fluid retention.
B- Rate-limiting non-dihydropyridines calcium antagonists
Ex Diltiazem 200-300 mg daily,
Verapamil 240 mg daily
useful when hypertension coexists with angina
may cause bradycardia.
main side-effect of verapamil -- constipation.
5-Beta-adrenoceptor antagonists (β-blockers).
No longer first line drug,except in patients with another indications (e.g.angina)
EX-
Cardioselective -> preferentially block the cardiac β1-adrenoceptors,
( as opposed to the β2-adrenoceptors = vasodilatation and bronchodilatation
Metoprolol (100-200 mg daily),
Atenolol (50-100 mg daily) and
Bisoprolol (5-10 mg daily).
Combined β- and α-adrenoceptor antagonists
sometimes more effective than pure β-blockers.
Labetalol (200 mg-2.4 g daily in divided doses)
Carvedilol (6.25-25 mg 12-hourly)
Labetalol can be used as an infusion in malignant phase hypertension
Other drugs.
Vasodilatorsα1-adrenoceptor antagonists (α-blockers
e.g. prazosin (0.5-20 mg daily in divided doses),
indoramin (25-100 mg 12-hourly) and
doxazosin (1-16 mg daily), and
Drugs acting directly on vascular smooth muscle,
e.g. hydralazine (25-100 mg 12-hourly) and
minoxidil (10-50 mg daily).
Side-effects include first-dose and postural hypotension, headache, tachycardia and fluid retention. Minoxidil also causes increased facial hair and is therefore unsuitable for female patients.
Centrally acting drugs,
E.g. methyldopa (initial dose 250 mg 8-hourly) and
clonidine (0.05-0.1 mg 8-hourly), are effective antihypertensive drugs but cause fatigue and are usually poorly tolerated.
THE INFLUENCE OF COMORBIDITY ON THE CHOICE OF ANTIHYPERTENSIVE DRUG THERAPY
α-blockers
Compelling Ind. Possible ind. Caution Comp. contraind.
Benign PH heart failure P. hypotension, U. incontinence
β-blockersM. infarction, Heart failure Peripheral VD DM (except CAD)
Asthma or
Heart failure COPD
Heart block
-
Angiotensin-converting enzyme (ACE) inhibitors
Compelling Ind. Possible ind. Caution Comp. contraind.
Heart failureHeart failure CH.R.dis Renal impaiR. Pregnancy
L. V dysfunction, Type 2 D neph. PVD Renovascular dis.
post-MI or
established CAD
Type 1 D. nephropathy
Sec.y stroke prevention
Angiotensin II receptor blockers
Compelling Ind. Possible ind. Caution Comp. contraind
ACE inhibitor intolerance LV dys.-MI R. impair. Pregnancy
Type 2 diabetic nephr. Intol of other AHD PVD
Hypertension with LVH Proteinuric RD
Heart f. in ACE-intolerant chronic RD
after myocardial infarction
-
Calcium channel blockers
(dihydropyridine)
Compelling Ind. Possible ind. Caution Comp. contraind
Elderly patients, Angina
isolated sys HTCalcium channel blockers
(rate-limitingAngina Elderly P. Comb. BB AV block,
heart failure
Thiazides or thiazide-like diuretics
Compelling Ind. Possible ind. Caution Comp. contraind
Elderly patients, - Gout
isolated SHT, heart failure,
sec.stroke prevention-
emergency treatment of accelerated phase or malignant hypertension
RULES1-Unwise to lower blood pressure too quickly
compromise tissue perfusion (due to altered autoregulation)
cerebral damage, including occipital blindness, and
coronary or renal insufficiency.
2-Even in presence of cardiac failure or hypertensive encephalopathy, a controlled reduction,
to a level of about 150/90 mmHg,
over a period of 24-48 hours is ideal.
In most patients it is possible to avoid parenteral therapy and bring blood pressure under control with bed rest and oral drug therapy.
DRUGS
1- IV or intramuscular labetalol (2 mg/min to a max. of 200 mg),
2-IV glyceryl trinitrate (0.6-1.2 mg/hour),
3-IM hydralazine (5 or 10 mg aliquots repeated at half-hourly intervals)
4-IV sodium nitroprusside (0.3-1.0 μg/kg body weight per minute)
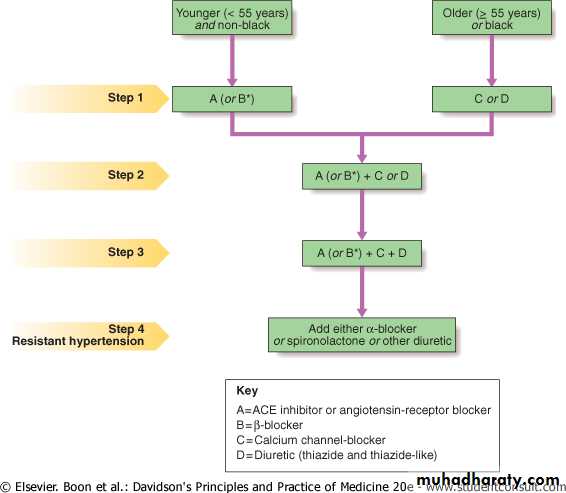
Choice of antihypertensive drug
No consistent or important differences in outcome, efficacy, side-effects or quality of life .Choice of antihypertensive therapy usually dictated by
cost/ convenience/ response to treatment /freedom from side-effects.
Co morbid conditions = important influence on initial drug selection e.g.
β-blocker most appropriate treatment for a patient with angina unless there is also a history of asthma.
Thiazide diuretics and dihydropyridine calcium antagonists = most suitable for elderly
Combination therapy
often required to achieve optimal blood pressure control.desirable for other reasons; e.g.,
low-dose therapy with two or three drugs may produce fewer unwanted effects than treatment with the maximum dose of a single drug.
some drugs have complementary or synergistic actions e.g., thiazides increase activity of renin-angiotensin system while ACE inhibitors block it.
Refractory hypertension
Common causes of treatment failure1- non-adherence with drug therapy,
2- inadequate therapy, and
3-failure to recognise an underlying cause
such as renal artery stenosis or
phaeochromocytoma;
No easy solution to compliance problems, but
1- simple treatment regimens, attempts to improve rapport with the patient and
2-careful supervision
Adjuvant drug therapy
Aspirin.
Antiplatelet therapy =powerful means of reducing cardiovascular risk (but may cause bleeding, particularly intracerebral haemorrhage, in a small number of patients).
benefits of aspirin therapy ==outweigh the risks in hypertensive patients
Aged 50 or over + well-controlled blood pressure and either
1-Target organ damage,
2- Diabetes or
3- 10-year coronary heart disease risk of more than 15%.
Statins.
Treating hyperlipidaemia produce a substantial reduction in CV risk.strongly indicated in patients who have
1-established vascular disease, or
2- hypertension with a high (> 15% in 10 years) risk of developing coronary heart disease