Floppy Baby Syndrome
Supervised by:Dr. Nibal
Presented by:
Jafar Alaa
Aya Abdulhaleem
Hasan Haider
Tuqa Hazim
Jafar Alaa
Sign of both benign andserious conditions
Exhaustive differential diagnosis
Rare disorderOverwhelming advances in diagnosis and management
Diagnostic challenge
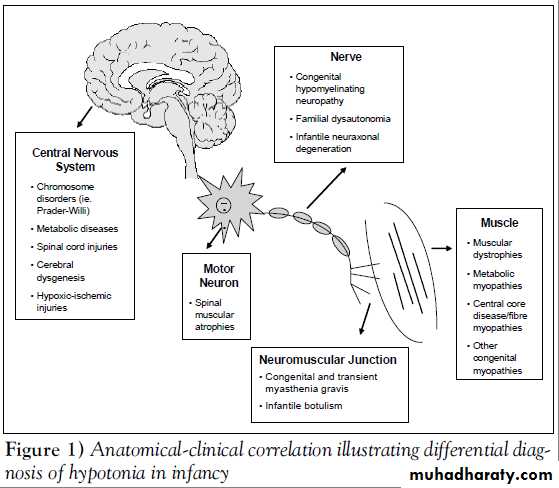
The maintenance of normal tone requires intact central and
peripheral nervous system . Hence hypotonia is a commonsymptom of neurological dysfunction and occurs in diseases
of the brain, spinal cord, nerves, and muscles.Differential diagnosis
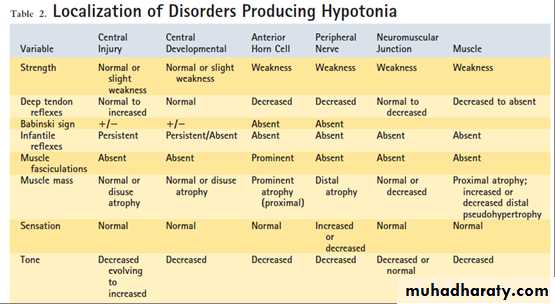
Common causes of hypotoniaTwo categories - Central and peripheral disorders .
Peripheral causes include abnormalities in the motor unit , specifically in the anterior horn cell (ie, spinal muscular atrophy), peripheral nerve , neuromuscular junction , and muscle
Central causes account for 60% to 80% of hypotonia cases and the peripheral causes occur in 15% to 30%.
Considerable overlap of involvement and clinical manifestations
Differential diagnosis for hypotoniaThe most common central cause of hypotonia is hypoxic encephalopathy / cerebral palsy in the young infant. However, this dysfunction may progress in later infancy to hypertonia.
The most common neuromuscular causes, although still rare, are congenital myopathies, congenital myotonic dystrophy, and spinal muscular atrophy.
Disorders with both central and peripheral manifestations ex acid maltase deficiency (Pompe disease).
Central and peripheral causes
Cerebral insult – Hypoxic ischemic encephalopathy , intracranial haemorrhageBrain malformations
Chromosomal disorders – Praderwilli syndrome , Down syndrome
Peroxisomal disorders – cerebrohepatorenal syndrome ( Zellweger’s syndrome) , Neonatal adrenoleukodystrophy
Other genetic defects – familial dysautonomia , oculocerebrorenal syndrome ( Lowe syndrome )
Neurometabolic disorders – Acid maltase deficiency , infantile GM1 gangliosidosis
Drug effects ( ex Maternal Benzodiazepines )
Benign congenital hypotonia
Causes of Cerebral hypotonia (Central causes)
Infantile spinal muscular atrophy
Traumatic myelopathy ( esp following breech delivery )Hypoxic ischemic myelopathy
Peripheral causes:1) Anterior horn cell disorders
Congenital hypomyelinating neuropathyGiant axonal neuropathy
2) Congenital neuropathies
Myasthenia gravis ( Transient acquired neonatal myasthenia ,congenital myasthenia )
Infantile botulism3) Neuromuscular junction disorders
Congenital myopathy
Nemaline myopathy4) Myopathies
Congenital muscular dystrophy with merosin deficiency
Congenital muscular dystrophy without merosin deficiencyCongenital muscular dystrophy with brain malformations or intellectual disability
Dystrophinopathies
Early infantile facioscapulohumeral dystrophy Congenital myotonic dystrophy
5) Muscular dystrophies
Disorders of glycogen metabolism ( ex Acid maltase deficiency )Severe neonatal phosphofructokinase deficiency
Severe neonatal phophorylase deficiency
6) Metabolic and multisystem disease
Aya Abdulhaleem
History&
Clinical evaluation
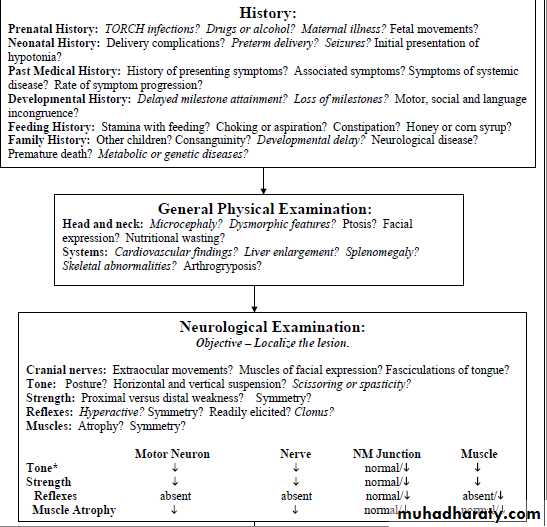
Identify cause and the timing of onset
Maternal exposures to toxins or infections suggest a central causeInformation on fetal movement in utero, fetal presentation, and the amount of amniotic fluid.
Low Apgar scores may suggest floppiness from birth
Breech delivery or cervical
position – cervical spinal cord
trauma
Obstetric history
A term infant who is born healthy but develops floppiness after 12 to 24 hours – suspect inborn error of metabolism
Infants suffering central injury usually develop increased tone and deep tendon reflexes.
Central congenital hypotonia does not worsen with time but may become more readily apparent
Course of illness
Motor delay with normal social and language development decreases the likelihood of brain pathology.
Loss of milestones increases the index of suspicion for neurodegenerative disorders.
Developmental historyA dietary/feeding history may point to diseases of the neuromuscular junction, which may present with sucking and swallowing difficulties that ‘fatigue’ or ‘get worse’ with repetition.
Dietary / Feeding history
Developmental delay (a chromosomal abnormality)
Delayed motor milestones (a congenital myopathy) andPremature death (metabolic or muscle disease).
Family history
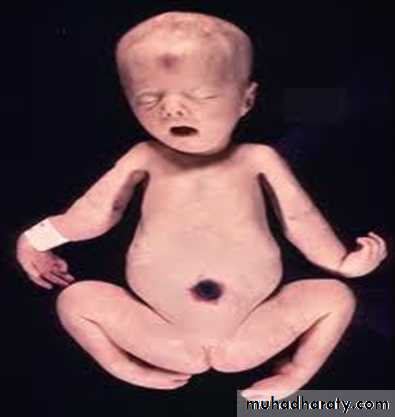
When lying supine, all hypotonic infants look much the same, regardless of the underlying cause or location of the abnormality within the nervous system.
Lack spontaneous movement
Full abduction of the legs places the lateral surface of the thighs against the examining table, and the arms lie either extended at the sides of the body or flexed at the elbow with the hands beside the head.
General examination
General examination
Hip dislocation - The forceful contraction of muscles pulling the femoral head into the acetabulum is a requirement of normal hip joint formation.Pectus excavatum indicates long standing long-standing weakness of the chest wall muscles
Infants who lie motionless eventually develop flattening of the occiput and loss of hair on the portion of the scalp that is in constant contact with the crib sheet.Hip subluxation or arthrogryposis suggest hypotonia in utero .
Arthrogryposis varies in severity
from clubfoot, the most common manifestation, to symmetricalflexion deformities of all limb joints.
Joint contractures - a nonspecific consequence of intrauterine immobilization.
As a rule, newborns with arthrogryposis who require respiratory assistance do not survive extubation unless the underlying disorder is myasthenia.
Arthrogryposis
High-pitched or unusual-sounding cry - suggests CNS pathology
A weak cry - diaphragmatic weaknessFatigable cry - congenital myasthenic syndrome.
Quality of cryHasan Haider
Detailed neurologic assessment - tone, power, and reflexesCan also points toward specific cause (e.g. hyperreflxia in central causes and hyporeflexia in peripheral causes)
Neurologic examination
Evaluation of hypotoniaTraction response
Vertical suspension
Horizontal suspension
Further evaluation
Of
Hypotonia
• The Traction Response
The most sensitive measure of postural tone
Child in supine position grasp the arms and pull the infant toward a sitting position
A normal term infant lifts the head from the surface immediately with the bodyDuring traction, the examiner should feel the infant pulling back against traction and observe flexion at the elbow, knee, and ankle.
The Traction Response
The traction response is not present in premature newborns of less than 33 weeks' gestation
The presence of head lag and of failure to counter traction by flexion of the limbs in the term newborn is abnormal and indicates hypotonia.
By 1 month, normal infants lift the head immediately and maintain it in line with the trunk.
Traction response
Vertical Suspension
• Normal AbnormalThe examiner places both hands in the infant's axillae and, without grasping the thorax, lifts straight up
The muscles of the shoulders should have sufficient strength to press down against the examiner's hands and allow the infant to suspend vertically without falling through
Normal response – Head erect in the midline with flexion at the knee, hip, and ankle joints.
When a hypotonic infant is suspended vertically, the head falls forward, the legs hanging, and the infant may slip through the examiner's hands because of weakness in the shoulder muscles
Vertical Suspension
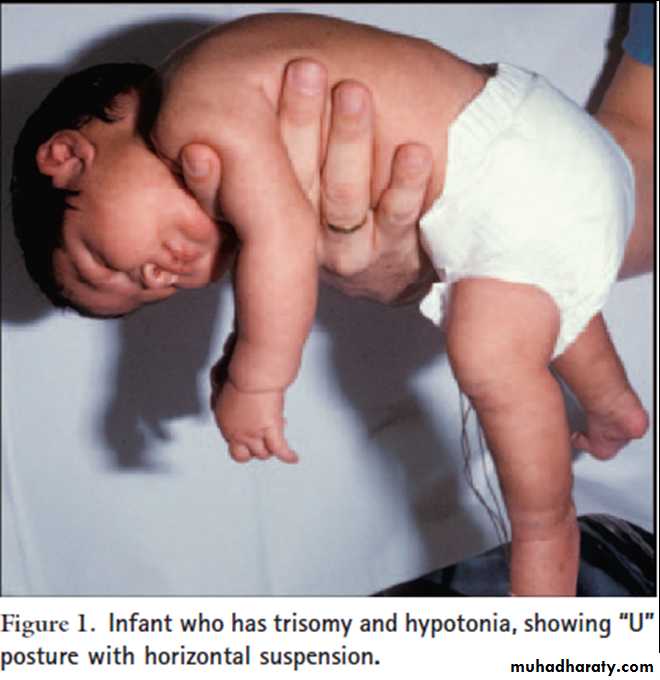
Horizontal (Ventral) Suspension
Horizontal (Ventral) SuspensionNormal infant - keeps the head erect, maintains the back straight, and flexes the elbow, hip, knee, and ankle joints
Baby suspended in the prone position with the examiner’s palm underneath the chest
Hyptonia - infants drape over the examiner's hands, with the head and legs hanging limply
Differentiating central
From
Peripheral hypotonia
Dysmorphic features
Depressed level of consciousness or lethargyAbnormal eye movements or inability to track visually
Early onset seizures
Predominant axial weakness
Normal Power with hypotonia
Scissoring on vertical suspension
Fisting of the hands
Hyperactive or normal reflexes
Malformations of other organs
Clues to Central hypotonia
Alert infant and appropriate response to surroundings
Normal sleep-wake patterns
Associated with profound weakness
Hypotonia and hyporeflexia/ areflexia
Other features - muscle atrophy, lack of abnormalities of other organs, the presence of respiratory and feeding impairment, and impairments of ocular or facial movement
Characteristics of peripheral causes of hypotonia
Usually spares extraocular muscles, while diseases of the neuromuscular junction may be characterized by ptosis and extraocular muscle weakness .Anterior horn cell diseases Versus neuromuscular junction disorders
Tuqa Hazim
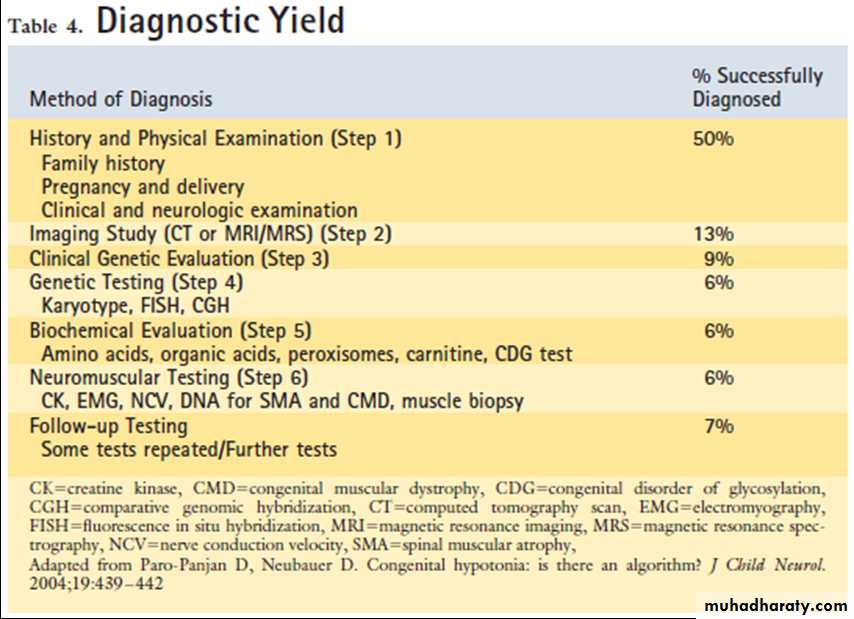
Laboratory evaluation
Rule out sepsis first - complete blood count , (blood culture, urine culture, cerebrospinal fluid culture and analysis);Measurement of serum electrolytes – calcium and magnesium
Liver function tests
Urine drug screen
Thyroid function tests
TORCH titers (toxoplasmosis, rubella, cytomegalovirus infection, herpesvirus infections) and a urine culture for cytomegalovirus ( hepatosplenomegaly and brain calcifications )
Karyotype – Dysmorphism
EEG – helps in prognostication
Genetic studies - Array comparative genomic hybridization study, methylation study for 15q11.2 (Prader-Willi/Angelman) imprinting defects, and testing for known disorders with specific mutational analysis
Labortary evaluation
Complex multisystem involvement on clinical evaluation suggests - inborn errors of metabolism
Presence of acidosis - plasma amino acids and urine organic acids (aminoacidopathies and organic acidemias)
Serum lactate in disorders of carbohydrate metabolism, mitochondrial disease
Pyruvate and ammonia in urea cycle defects
Acylcarnitine profile in organic acidemia, fatty acid oxidation disorder
Very long-chain fatty acids and plasmalogens - specific for the evaluation of a peroxisomal disorder.
Labortary evaluation – Inborn error of metabolism
MRIDelineate structural malformations
Neuronal migration defectsAbnormal signals in the basal ganglia (mitochondrial abnormalities) or brain stem defects (Joubert syndrome)
Deep white matter changes can be seen in Lowe syndrome, a peroxisomal defect
Abnormalities in the corpus callosum may occur in Smith- Lemli-Opitz syndrome
Heterotopias may be seen in congenital muscular dystrophy.
Magnetic resonance spectroscopy
Magnetic resonance spectroscopy also can be revealing for metabolic disease.Radiologic evaluation
Creatine kinase (levels need to be interpreted with caution in the newborn, as levels tend to be high at birth and increase in the first 24 hours, they also increase with acidosis).
Repeat after few days , if initial value is elevated
Elevated in muscular dystrophy but not in spinal muscular atrophy or in many myopathies.
Creatine kinase
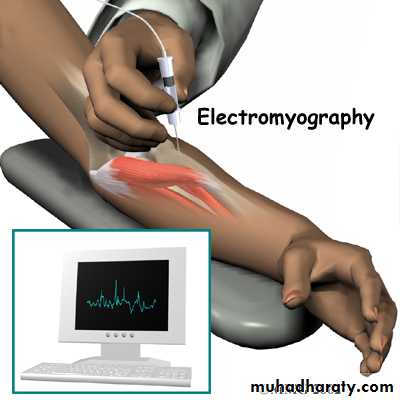
DNA studies and electrophysiologySpecific DNA testing - for myotonic dystrophy and for spinal muscular atrophy ( SMN gene )
Electrophysiological studies - Shows abnormalities in nerves, myopathies, and disorders of the neuromuscular junction
Normal EMG usually suggest central hypotonia , with few exceptions
Helps to differentiate a primary myopathy from a neurogenic disorder
Helps to differentiate myopathies from muscular dystrophiesUseful in the work-up of undiagnosed weakness
Muscle biopsy with immunohistochemical staining