Dr.asad
1
st
lecture
medicine
Pyrexia of unknown origin (PUO)
The range for normal human body temperatures, taken orally, is 36.8±0.5 °C.
The
normal human body temperature is often stated as 36.5–37.5 °C.
1-Hypothermia
<35.0 °C (95.0 °F)
2-Normal
36.5–37.5 °C (97.7–99.5 °F)
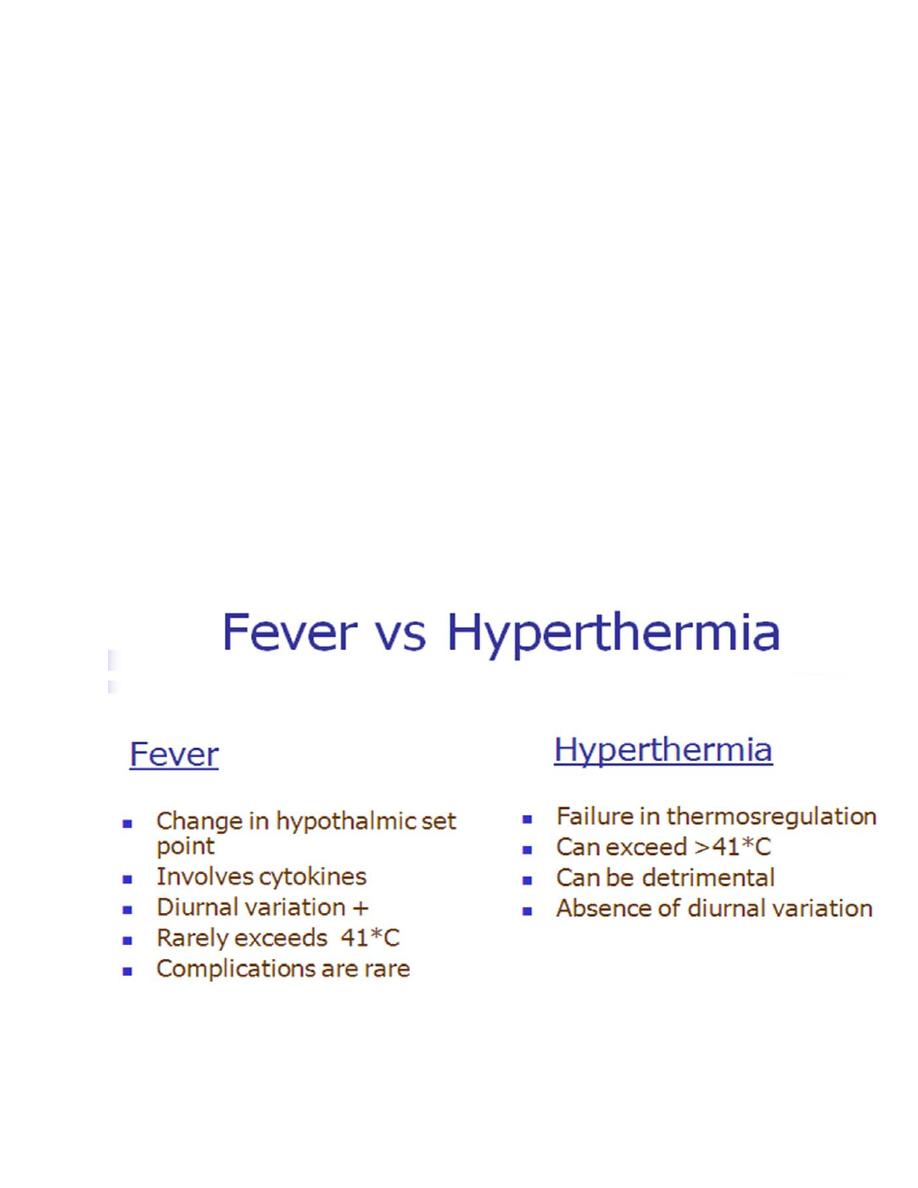
3-Fever
>37.5 or 38.3 °C (99.5 or 100.9 °F)
4-Hyperthermia
>37.5 or 38.3 °C (99.5 or 100.9 °F)
5-Hyperpyrexia >40.0 or 41.5 °C (104.0 or 106.7 °F)
Dr.asad
1
st
lecture
medicine

Dr.asad
1
st
lecture
medicine
In 1961, Petersdorf and Beeson defined a fever of unknown origin (FUO) as the
following:
(1) a temperature greater than 38.3°C (101°F) on several occasions,
(2) more than 3 weeks' duration of illness, and
(3) failure to reach a diagnosis despite 1 week of inpatient investigation.
later revised, is “a fever of 38.3°C (101°F) or more lasting for at least three weeks
for which no cause can be identified after three days of investigation in hospital
or after three or more outpatient visits.
Classifications of pyrexia of unknown origin
1-
Classic pyrexia of unknown origin:
Pyrexia for ≥3 weeks with no identified
cause after evaluation in hospital for 3 days or ≥3 outpatient visits.

Dr.asad
1
st
lecture
medicine
2-
Nosocomial pyrexia of unknown origin
:
Pyrexia in patients hospitalized for
>48 hours with no infection present or incubating at admission, and in
whom the diagnosis remains uncertain after ≥3 days of appropriate
evaluation, which includes microbiological cultures that have been
incubating for ≥2 days.
3-
Immunodeficient (neutropenic) pyrexia of unknown origin
:
Pyrexia in a
patient with <500 neutrophils/µl in whom the diagnosis remains uncertain
after ≥3 days of appropriate evaluation, which includes microbiological
cultures that have been incubating for ≥2 days.
4-
HIV-associated pyrexia of unknown origin:
Pyrexia in a patient with
confirmed HIV infection lasting for >4 weeks as an outpatient or >3 days as
an inpatient, in whom the diagnosis remains uncertain after ≥3 days of
appropriate evaluation, which includes microbiological cultures that have
been incubating for ≥2 days.
How common is pyrexia of unknown origin?
The true incidence and prevalence of pyrexia of unknown origin are uncertain.
A study of 153 patients reported the prevalence in hospitalized patients in the
1980s to be around 3%. However, in the past two decades technological
advances in diagnosis, particularly sophisticated imaging and improved culture
techniques, have reduced the proportion of cases where the cause is
unknown.
Aetiology of pyrexia of unknown origin :
The commonest cause of PUO IS Common disease presenting ATYPICALLY. PUO
is caused by:
1. Infections (30%)
2.Neoplasms (20%)
3.Connective tissue diseases (15%)
4. Miscellaneous diseases (20%).
5. Undiagnosed(15%).

Dr.asad
1
st
lecture
medicine
Infection:
Abdominal abscess, Extrapulmonary/disseminated tuberculosis
,Infective endocarditis , Osteoarticular infections ,Typhoid/enteric fevers ,Endemic
mycosis , Epstein-Barr virus infection ,Cytomegalovirus infection ,Brucellosis
,Leishmaniasis , Prostatitis ,Malaria ,Rickettsial infections ,Dental abscess ,Chronic
sinusitis.
Neoplasm:
Lymphoma , Leukaemia , Colon cancer , Pancreatic cancer ,
Hepatoma , Hepatic metastasis , Renal cell carcinoma.
Connective tissues disorder:
Systemic lupus erythematosis , Adult
onset Still’s disease , Vasculitic disorders (including polyarteritis nodosa,
rheumatoid disease with vasculitis and Wegener's granulomatosis) , Mixed
connective tissue disease , Polymyalgia rhematica , Sarcoidosis , Polymyositis ,
Behçet's disease.
Miscellaneous:
Drug fever , Factitious fever , Mediterranean familial fever ,
Deep vein thrombosis/pulmonary embolism , Hyperthyroidism , Inflammatory
bowel disease , Autoimmune hepatitis , Atrial myxoma , Sarcoidosis , Alcoholic
liver disease.
In children, infections are the most frequent cause of FUOs. Neoplasms and
connective-tissue disorders are more frequent in the elderly. In patients with
FUOs lasting more than 1 year, infections and neoplasms decline in frequency,
and granulomatous diseases become the most frequent etiology.
Data from several large prospective studies suggest that infective causes are
becoming less common, probably because advanced imaging techniques and
improved culture methods have become more widely available. For similar
reasons, the proportion of cases of pyrexia of unknown origin attributed to
neoplasia has steadily decreased over recent years. These trends do not hold true
in less developed societies where infection, often with mycobacteria, remains
common and advanced diagnostic techniques are often unavailable.

Dr.asad
1
st
lecture
medicine
History:
1-Verify the presence of fever.
2-Duration of Fever.
3-Travel to an area known to be endemic for certain disease.
4-Drug and Toxin History (Almost any drug can cause fever).
5-Localizing Symptoms: may Indicate the source of fever.
6-Family History (TB or FMF).
7-Past Medical Condition (lymphoma, Rh.fever).
8-Exposure to sexual partner … Acute HIV.
9-Illicit drug abuse (IV) … infective endocarditis, Hepatitis & HIV.
Physical Examination:
Detailed examination should be repeated at
regular intervals to detect emerging features.
-Document the Fever: Significant and persistent for more than ONE occasion.
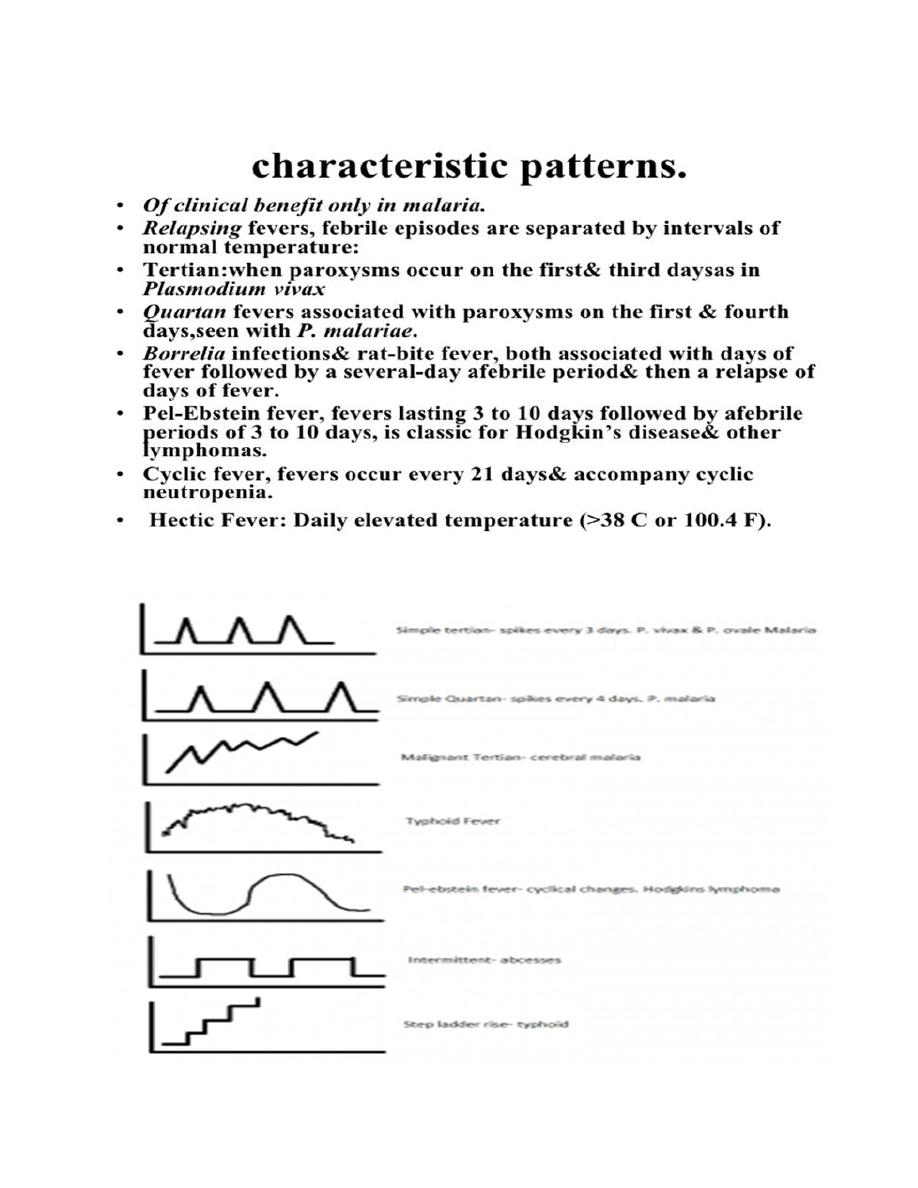
-Analyzing the Pattern: Neither specific Nor sensitive enough to be considered
diagnostic … EXCEPT( Malaria).
-Examine for Lymphadenopathy if generalized→ look for hepatomegaly &
splenomegaly.
-Examine the Skin: Rash.
-Examine the thyroid and look for peripheral signs of thyrotoxicosis.
-Examine for Oral Ulcer (SLE,Behcet’s Syndrome).
-Examine for Arthritis.

Dr.asad
1
st
lecture
medicine
-Examine the Fundus (Roth’s spots, choroidal lesion).
-New or Changing Murmur.
-Temporal Artery … nodular, weakly pulsatile.
-Sinus Tenderness.
-Thyroid Enlargement or Tenderness
.
Roth's spot:
A hemorrhage in the retina with a white center. Originally
associated with bacterial endocarditis, may be seen in leukemia, diabetes,
collagen-vascular diseases,
Diagnostic Testing:
Complete Blood Count
-Anemia if present → suggest a serious underlying disease
-Leukocytosis with bands → occult bacterial infection
-Lymphocytosis & atypical Lymphocyte → Infectious mononucleosis
-Leucopenia and Lymphopenia → advanced HIV
-Leukoerythroblastic Anemia → Disseminated TB
-Thrombocytopenia → Malaria/Leukemia
-Peripheral Blood → Malaria
Urinalysis, Urine Culture:-Stool for ova, cysts and parasites.
-ESR (If elevated → significant inflammatory process).
Serology Test
**Brucella Titer,CMV & EBV antibody test, HIV testing).
** Anti-nuclear Antibodies & Rheumatoid Factor

Dr.asad
1
st
lecture
medicine
Cultures:
Blood: (Obtain more than 3 blood cultures from separate venipunctures over 24
hr period if you are suspecting inf. Endocarditis prior antimicrobial use.Incubate
the blood for 4 weeks, to detect the presence of SBE & Brucellosis).
Sputum: For Tuberculosis
Any normal sterile: CSF/urine/pleural or peritoneal fluid
Bone marrow aspirate Tuberculosis/Brucellosis.
Imaging Studies:
Chest x-ray:
**Military shadows → disseminated tuberculosis
**Pleural effusion.
**Mediastinal mass → Lymphoma/Tuberculosis/ Sarcoid
**If CXR is (N) → Repeat on weekly basis.
Echocardiography:
to detect vegetations of IE.
Ultrasound:
CT scan
:Mediastinal mass → Tuberculosis/Lymphoma/ Sarcoidosis
Dorsal Spine → Spondylitis and disc space disease
CT-Scan Abdomen → very effective to visualize
All types of abscesses
Retroperitoneal tumor, lymph node or haematoma
Dr.asad
1
st
lecture
medicine
MRI:
spleen, lymph node and the brain.
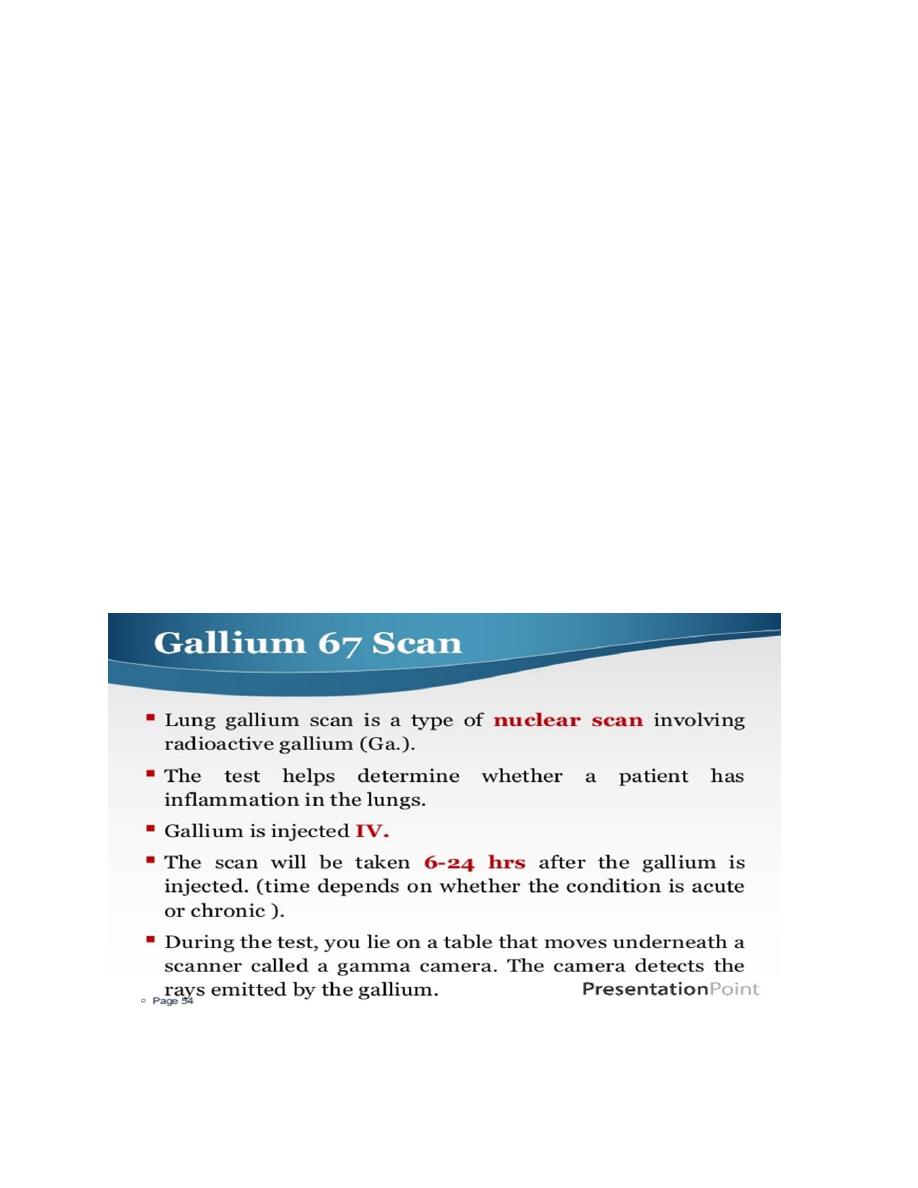
Radionuclear Scanning:
Bone TC-scan → osteomyelitis (skeletal).
Gallium scan → occult inflammation.
Indium labeled WBC-scan → occult abscesses.
Laparoscopy:
To visualize and biopsy the pathology in the abdomen suggestive
of:e.g.Tuberculous peritonitis, Peritoneal carcinomatosis.
Biopsy:
Enlarged lymph node (Granulomatous disease in Tuberculosis or
Metastatic carcinoma).

Dr.asad
1
st
lecture
medicine
Bone Marrow
Granuloma ± Tubercle Bacilli → Tuberculosis
blast Cells → Leukemia
Leishmania Bodies → Kala-Azar
Atypical Cells → Lymphoma
Atypical Plasma Cells → M. myeloma
Temporal Artery → Giant Cell Arteritis
Pleural or Pericardial → Tuberculosis
Therapeutic Trials:
Limitation and risk of empirical therapeutic trials:
1.Rarely specific
2.Underlying disease may remit spontaneously false impression of success.
3.Disease may respond partially and this may lead to delay in specific diagnosis.
4.Side effect of the drugs can be misleading.
Empiric Drug:
Tuberculosis
Culture-negative Endocarditis
Vasculitis … Temporal Arteritis
Treatment:
Once a diagnosis has been established specific treatment can be started. For
patients in whom a cause for the fever is not found and who are clinically well,

Dr.asad
1
st
lecture
medicine
watching and waiting is reasonable. During this time of observation re-assess the
history and physical examination.Approximately 5-15% of patients remain
undiagnosed, even after extensive evaluations.Careful review of the literature
shows that patients usually have a benign long-term course, especially in the
absence of substantial weight loss or other signs of a serious underlying disease
.
Factitious Fever:
False fever: thermometer manipulation using external heat or substitute
thermometer.
Genuine fever (self induced)
Administration of pyrogenic substances (bacterial suspensions) Generally young
women with connection to health care … often NURSES.
Clues to the diagnosis of factitious fever:
1. A patient who looks well
2. Bizarre temperature chart with absence of diurnal variation and/or
temperature-related changes in pulse rate
3. Temperature > 41°C
4. Absence of sweating during defervescence
5. Normal ESR and CRP despite high fever
6. Evidence of self-injection or self-harm
7. Normal temperature during supervised (observed) measurement and of freshly
voided urine.
By:TWANA NAWZAD
