VIRAL HEMORRHAGIC FEVERS
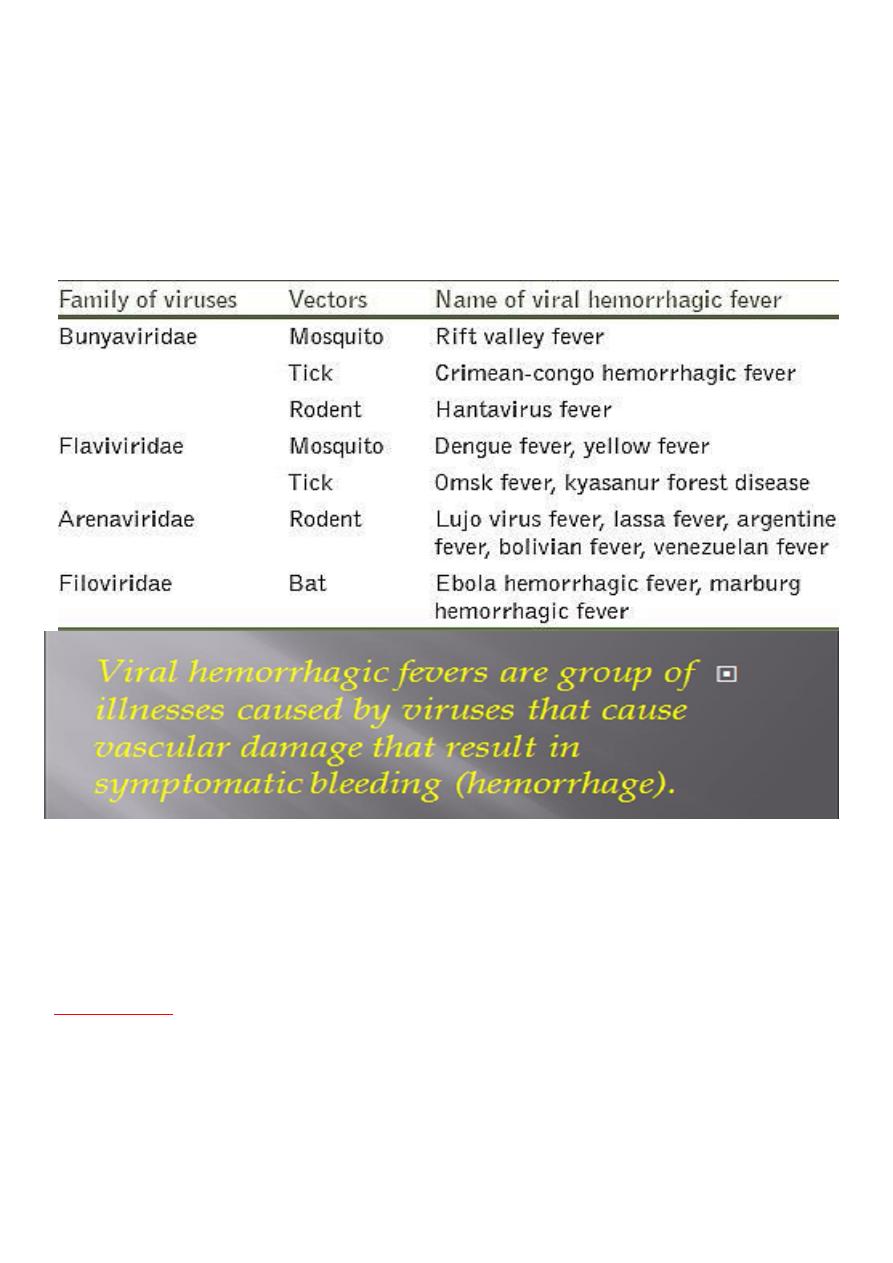
Viral hemorrhagic fever is a nonspecific syndrome that can be caused by several
different viruses, from the
families Flaviviridae, Bunyaviridae, Arenaviridae, and
Filoviridae
All contain RNA, and most are zoonotic. However,
.
their
they differ in
modes of transmission, animal reservoirs, and ability to be transmitted directly
from human to
human. Both arthropod-borne and rodent-associated viruses
cause
viral hemorrhagic fevers.
do not require an
The rodent-associated viruses
arthropod vector but are transmitted directly to vertebrates by infectious excreta
or secretions of the rodent.
Crimean-Congo Hemorrhagic Fever
Crimean-Congo hemorrhagic fever is caused by a virus of the
Nairovirus genus, family
. The virus has a single-stranded RNA genome, is enveloped and
Bunyaviridae
spherical, and replicates in suckling mice
and several cell culture systems.
Epidemiology
Crimean-Congo hemorrhagic fever is a tick-borne infection whose distribution includes
parts of the former Soviet Union, the Balkan nations, Iraq, Iran, the Indian
subcontinent, Afghanistan, northwestern China, the Middle East, and most of sub-
Saharan Africa, including South Africa. The disease was first characterized in the
Crimean in 1944 as Crimean hemorrhagic fever. It was recognized in 1969 as the
cause of illness in the Congo, thus the current name.
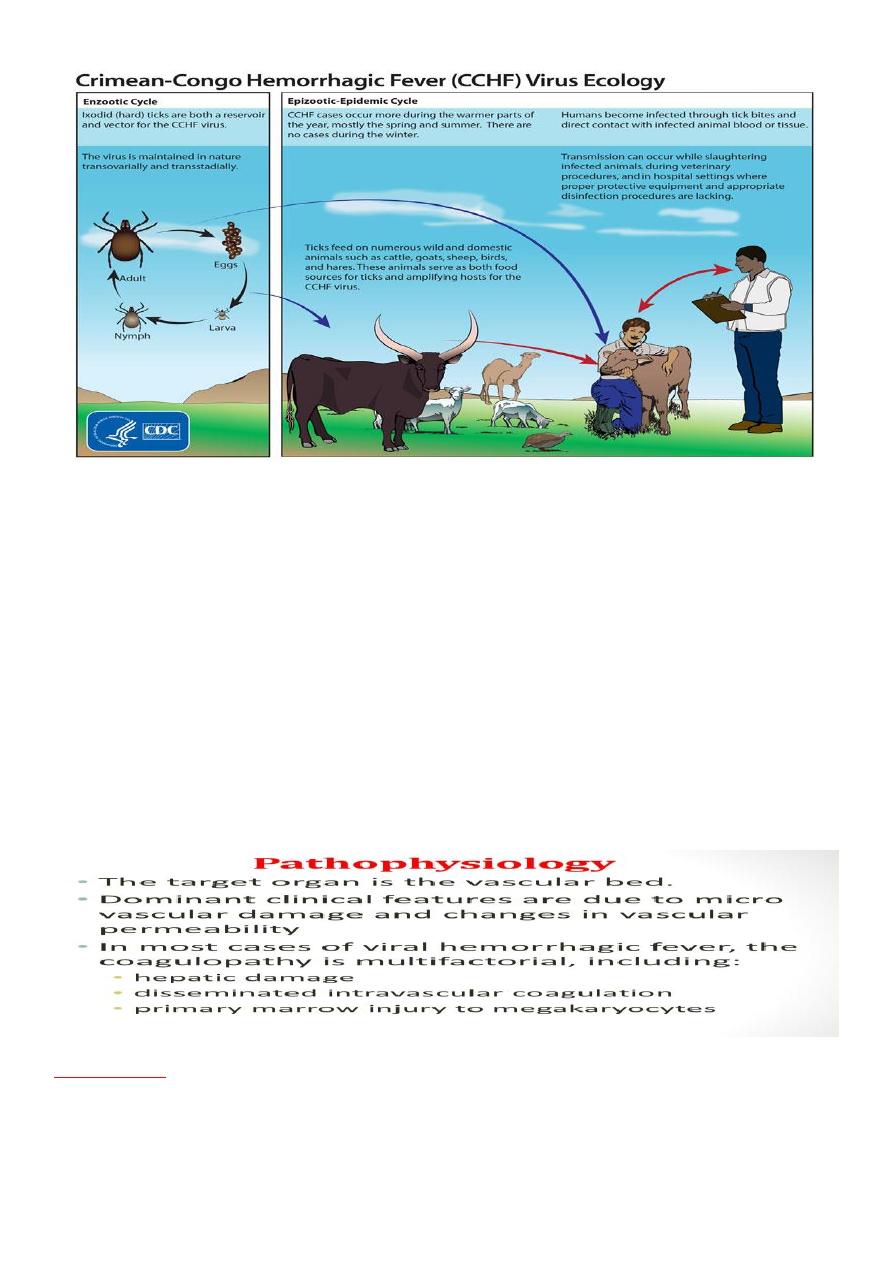
The virus is harbored and transmitted in nature, principally by ixodid ticks(hard
ticks family) of the genus Hyalomma (not soft ticks)
including
The virus is transmitted among ticks, with amplification in vertebrates,
sheep, and cattle. In Africa, antibodies against Crimean-Congo hemorrhagic fever
have been found in giraffes, buffalos, zebras, and dogs.
occurs through
Transmission to humans
contact with infected animal blood or ticks.
Crimean-Congo hemorrhagic fever can be transmitted from one infected human to
Outbreaks have been
another by contact with infectious blood or body fluids.
reported in military personnel, campers, and persons tending sheep and cattle..
•
Health care personnel have been infected through contact with infectious human blood
and tissue. Health care–associated spread as a result of improper sterilization of
medical equipment, reuse of injection needles, and contamination of medical supplies
has been documented
Pathobiology
After initial inoculation, the virus is spread by
blood and the lymphatic
circulation and
achieves high levels in multiple organs, including the
liver
. Diffuse foci of necrosis
and hemorrhage are seen, with Councilman's bodies in hepatocytes. DIC occurs
within the first 3 days of illness.

Clinical Manifestations
After an incubation period of 2 to 9 days,
patients have a sudden onset of fever with
symptoms that include headache, myalgia, pharyngitis, conjunctivitis, nausea,
vomiting, diarrhea, and abdominal pain.
Petechiae
may be seen on the soft palate,
and
jaundice and
hepatomegaly
may be present. In severe cases, mood alterations
and confusion may be noted.
As the illness progresses, large ecchymoses, severe epistaxis, and persistent bleeding at
injection sites can be seen,
and
usually beginning on about the fourth day of illness
lasting approximately 2 weeks. Aminotransferase and serum bilirubin levels are
often elevated in late illness. Evidence of DIC is seen (abnormal prothrombin,
activated partial thromboplastin, and thrombin times and increased fibrin
degradation products). Multiple organ system failure may lead to death, usually
during the second week of illness.
Other potentially lethal complications include
.
severe blood loss, cerebral hemorrhage, and pulmonary edema
Diagnosis
Laboratory diagnosis can be made by a
1. Positive serologic test result,
Antibodies are detectable by
in surviving patients. Specific IgM and
immunofluorescence and ELISA
IgG are present by days 7 to 9 of illness.
2. evidence of
viral antigen in tissue by
immunohistochemical staining and
microscopic examination
.
3.
Identification of viral RNA sequences in blood or tissue
in a
by PCR
patient with a clinical history compatible with Crimean-Congo
hemorrhagic fever. Virus or nucleic acid is easily detected during the
first 8 days of illness.

Treatment
Treatment is supportive, including:
1. Monitoring and correction of volume status and electrolyte imbalances
Careful fluid management is necessary to avoid fluid overload..
2. Support of the coagulation system.
3. Careful sedation, and pain control.
Prevention
Measures to prevent tick attachment, including repellents(
)طارد للحشرات
and
protective clothing, should be used by individuals in high-risk settings, such
as livestock enclosures in affected areas. Treatment of livestock
مواشي
to
reduce the tick burden may reduce transmission to humans.
Handling of
should be minimized and undertaken
blood and tissue of sick sheep and cattle
with appropriate safety and hygiene precautions.
, including appropriate
Standard precautions for infection control should be used
management of sharp items such as injection needles, appropriate protection
against contact with blood and body fluids, and the use of barriers to prevent
splashes onto mucous membranes when procedures are performed.
Prognosis
Although improvement is usually seen on approximately
, patients may
day 10
remain weak and restless for more than a month. Patients who recover do not
demonstrate sequelae.
The case-fatality rate has ranged from 15% to as high
ks.
as 70% in some outbrea
