Short Stature
Dr.athal - pediatric - 5th stageNormal growth is the final common pathway of many factors, including endocrine, environmental, nutritional, metabolic and genetic influences.
Maintenance of a normal linear growth pattern is good evidence of overall health and can be considered a "bioassay" for the well-being of the whole child.
Definition
Short stature: is defined as subnormal height relative to other children of the same sex and age, taking family heights into consideration.It can be considered as the height below -2SD for age and gender, which is far below the 3rd percentile.
OR SS defined as height more than 2 SD below the midparental target height.
Etiology
1. Variations of Normal:Constitutional SS.
Genetic (familial SS)
2. Endocrine Disorders:
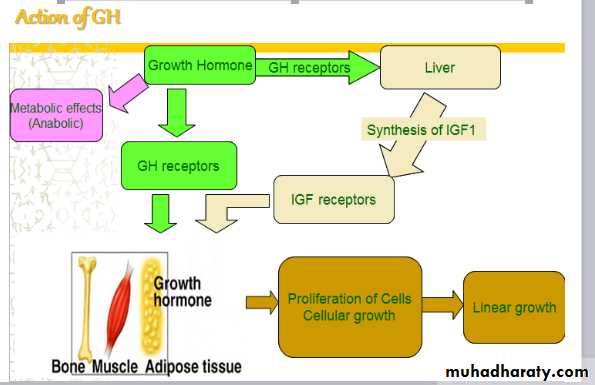
GH deficiency (congenital or acquired)GH insenstivity (Laron dwarfism)
Hypothyroidism
Glucocorticoid excess
Diabetes mellitus under poor control
3. Malnutrition:
Kwashiorkor & marasmus
Iron deficiency
Zinc deficiency
4. Chronic systemic disease:
Cardiac disorders, e.g. HFPulmonary disorders, e.g. asthma
Gastrointestinal disorders, e.g. celiac
Hepatic disorders
Renal disorders, e.g. CRF
Hematologic disorders, e.g. thalassemia
Rheumatologic disorder, e.g. SLE
Chronic infection, e.g. TB, AIDS
5. Skeletal Dysplasias:
Osteogenesis imperfecta
Osteochondroplasias
6. Lysosomal Storage Diseases:
MucopolysaccharidosesMucolipidoses
7. Syndromes of Short Stature:
Down syndrome
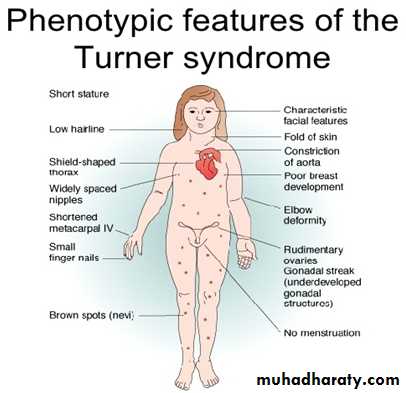
Turner syndrome
Approach to child with SS
Is the child short? Take accurate assesment of growth & plotting on growth chartTake Full history
Make complete physical examination
Investigation
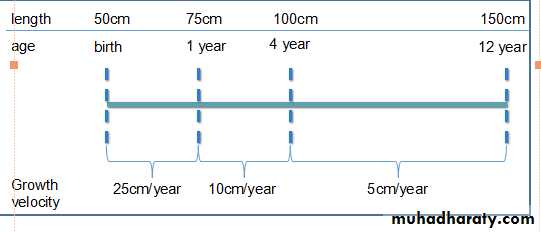
Assessment of Growth- Length/Height:
Accurate measurement is a critical component of growth assessment.For baby < 2 years, length is most accurately measured by two examiners, with the child supine on a measuring board.
The measurement should be obtained in the “Frankfurt plane” which places children in the supine position in full extension and the line between outer canthus of the eyes and the external auditory meatus perpendicular to the long axis of the trunk.
For older children, the measure is stature or height, taken without shoes, using a stadiometer.
At measuring the stature:
The child should be Bare feet.Four points touching the vertical plane of the stadiometer (back of the head, thoracic spine, buttocks, and heels.
Both length and height should be measured three times.
upper-to-lower (U/L) body segment ratio should measured.
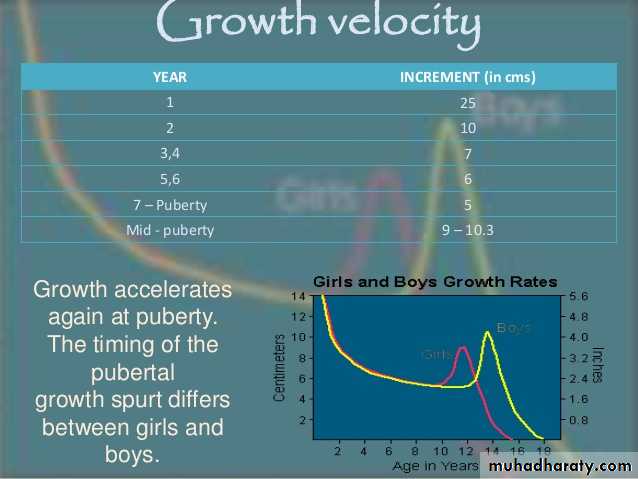
Assessment of growth – Height velocity (HV)
Serial measurements taken to assess growth velocity should be obtained by the same individual to eliminate variations between examiners or equipment. Recording of data over 12 months is preferable (minimum 6 months)
Statural growth is a continuous but not linear process.
Assessment of growth -Body proportions
OFC, sitting height, upper-to-lower (U/L) body segment ratio, and arm span are useful in the assessment of short stature, and markedly delayed or disproportionate growth.
Detection of U/L ratio above expected is characteristic of short stature owing to some genetic conditions (eg, Turner syndrome). whereas a ratio below expected is observed in short stature due to spinal irradiation.
Megalocephaly & rhizomelia (shortness of proximal legs &arms) are observed in patient with achondroplasia.
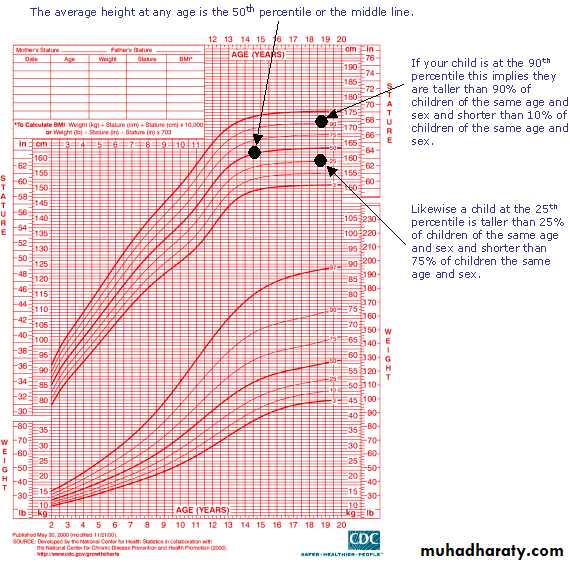
Growth Charts
Measurement of the child should plotted accurately on given chart.Growth charts should always be selected based on gender, whether height or length will be plotted, and, if relevant, underlying syndrome.
Prediction of Adult Height and Parental Target Height
Assessment of the PAH is frequently used in conjunction with the mid-parental target height (MPH), which takes into account the familial genetic factors in growth and height potential.The MPH(target):
Girls: ( father's height - 13 cm) + mother's height2
Boys: ( mother's + 13 cm) + father's height height 2
Disparity in the child’s growth percentile (ie, ±10 cm) from the MPH percentile should prompt further investigation.
Predicted Height:
Calculation of predicted height on the basis of:
current height, bone age, MPH
History
Complete pre, peri & postnatal history including birth length.Developmental & school performances.
Parental & child growth concerns(height relative to the peer group in school).
Systemic review to exclude any chronic disease as a cause of SS.
Nutritional history
Drug that can impair growth (as corticosteroid).
Psychosocial impact on SS.
Family history.
Examination
Anthropometric measurements
Undress the child … and watch
- proportions, skin, skeletal, hands, scars,rash …
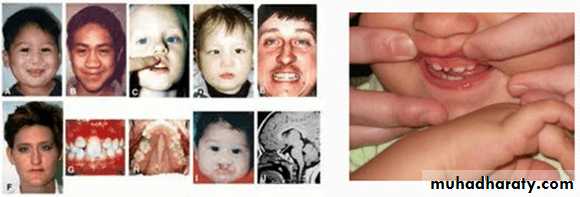
Dysmorphic features - facial dysmorphy(feature of turner,prader willi...ect)
Pubertal signs
Thyroid goiter
Midline structural abnormalities e.g.bifid uvula, central maxillary incisor--- hypopituitarism.
Investigation
Step 1:CBP & differential count, ESR.
RBS
GUE
Ca++, phosphate
Ferrtine level
Renal function test
Liver function test
Serology & jujenal biopsy for celiac
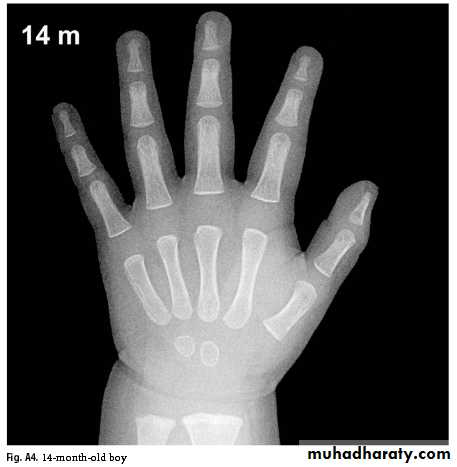
Wrist x-ray for bone age
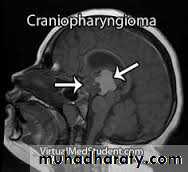
Skull x-ray to exclude intracranial pathology
Bone Age
Greulich & Pyle: Radiographic Atlas of Skeletal Development of the Hand and Wrist, This method involves a complex comparison of all the bones in the hand and wrist against reference radiographs of different ages.Delay of 2 years or more in bone age is significant.
Skull X-ray & MRI of brain:
Not routineTo assess:
pituitary
Any malformations
exclude masses
Step2:
Thyroid function testGrowth factors: IGF1, IGH_BP3
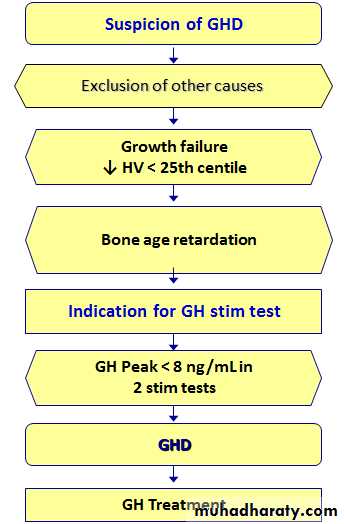
Growth hormone stimulation test
Familial (Genetic) SS
hallmarks of familial (genetic) short stature is normal bone age, normal growth velocity, and predicted adult height appropriate to the familial pattern.
Ht age < chronological age
Bone age = chronological age
Puberty at normal time
Constitutional SS
It is consider as normal variation in growth, more in male.Positive family history of the same pattern.
constitutional growth delay is characterized by delayed bone age and predicted adult height appropriate to the familial pattern.
Between 12 and 28 months of age, usually there is slow linear growth and by 3 years of age begin to display normal growth velocity for age.
Final height is usually within the normal range because of the longer period of growth prior to bone maturation but usually in the lower part of the MPH.
Growth hormon deficiency :
Growth hormon deficiency
Congenital: (isolated or multiple pituitary hor def)Acquired: (CNS tumer, CNS infection, cranial irradiation, head injury)
Criteria indicative for GHD
Infancy:
hypoglycemia
prolonged jaundice
obesity
Microphallus
Fontanelle closure is often delayed
The voice infantile because of hypoplasia of the larynx
Associated midline defects may be present as cleft-palate and lip.
normal birth length!
Childhood & Puberty:
Delayed bone age.
height velocity < 25th centile
Other:
Consanguinity and/or affected family member