Dr ghazi F.Haji
CardiologistLeprosy
Agenda
IntroductionEpidemiology
Immunology
Classification of leprosy
Signs &symptoms
Laboratory Studies
Treatment
Prognosis
Introduction
Leprosy is a chronic infection caused by the acid-fast, rod-shaped bacillus Mycobacterium leprae.Leprosy can be primarily affect superficial tissues, especially the skin and peripheral nerves.
A mycobacterial infection causes a wide array of cellular immune responses.
The social and psychological effects of leprosy, as well as its highly visible debilities and sequelae have resulted in a historical stigma associated with leprosy
Exposure: The incubation period of leprosy is long, ranging from a few months to 20-50 years.
Epidemiology
Leprosy is rarely fatal, no racial predilection is known. Leprosy is generally more common in males than in females, Leprosy can occur at any ageWorldwide, leprosy is considered the most common cause of crippling of the hand, foot
Nerve involvement results in loss of sensory and motor function(peripheral neuropathy ), which may lead to frequent trauma and amputation.
Travel: Leprosy should be considered in anyone who has lived in the tropics or who has traveled for prolonged periods to endemic areas
clawing, contracture
Immunology Leprosy can manifest in different forms, depending on the host response to the Individuals
1-who have a vigorous cellular immune response to M leprae have the tuberculoid form of the disease that usually involves the skin and peripheral nerves.
The number of skin lesions is limited, and they tend to be dry and hypoesthetic. Nerve involvement is usually asymmetric. as paucibacillary leprosy because of the low number of bacteria in the skin lesions (ie, < 5 skin lesions, with absence of organisms on smear). Results of skin tests with antigen from killed organisms are positive in these individuals.
2-Individuals with minimal cellular immune response have the lepromatous form of the disease, which is characterized by extensive skin involvement. Skin lesions are often described as infiltrated nodules and plaques, and nerve involvement tends to be symmetric in distribution. The organism grows best at 27-30°C; therefore, skin lesions tend to develop in the cooler areas of the body, with sparing of the groin, axilla, and scalp. as multibacillary leprosy because of the large number of bacteria found in the lesions (ie, >6 lesions, with possible visualization of bacilli on smear). Results of skin tests with antigen from killed organisms are nonreactive.
3-Patients may also present with features of both categories; however, over time, they usually evolve to one or the other (indeterminate or borderline leprosy).
Classification of leprosy
2 classification schemas:.
1-Ridley-Jopling: Depending on the host response to the organism, leprosy can manifest clinically along a spectrum bounded by the tuberculoid and lepromatous forms of the disease. Most patients fall into the intermediate classifications, which include borderline tuberculoid leprosy, and borderline lepromatous leprosy..
2-WHO system:according to the number of lesions and the presence of bacilli on a skin smear. This method is useful in countries where biopsy analysis in unavailable.
Paucibacillary leprosy is characterized by 5 or fewer lesions with absence of organisms on smear. Paucibacillary leprosy generally includes the tuberculoid and borderline lepromatous categories from the Ridley-Jopling system.
Multibacillary leprosy is marked by 6 or more lesions with possible visualization of bacilli on smear.
Lepromatous leprosy, borderline lepromatous leprosy, and midborderline leprosy on the Ridley-Jopling scale are included in the multibacillary leprosy category.
SYMPTOMS
Painless skin patch accompanied by loss of sensation but not itchiness (Loss of sensation is a feature of tuberculoid leprosy, unlike lepromatous leprosy, in which sensation is preserved.)Wasting and muscle weakness.
Foot drop or clawed hands
; Ulcerations on hands or feet
iridocyclitis, corneal ulceration,
and/or secondary cataract
:Symptoms in reactions
Type 1 (reversal) - Sudden onset of
skin redness and new lesions
Type 2 (erythema nodosum leprosum
.
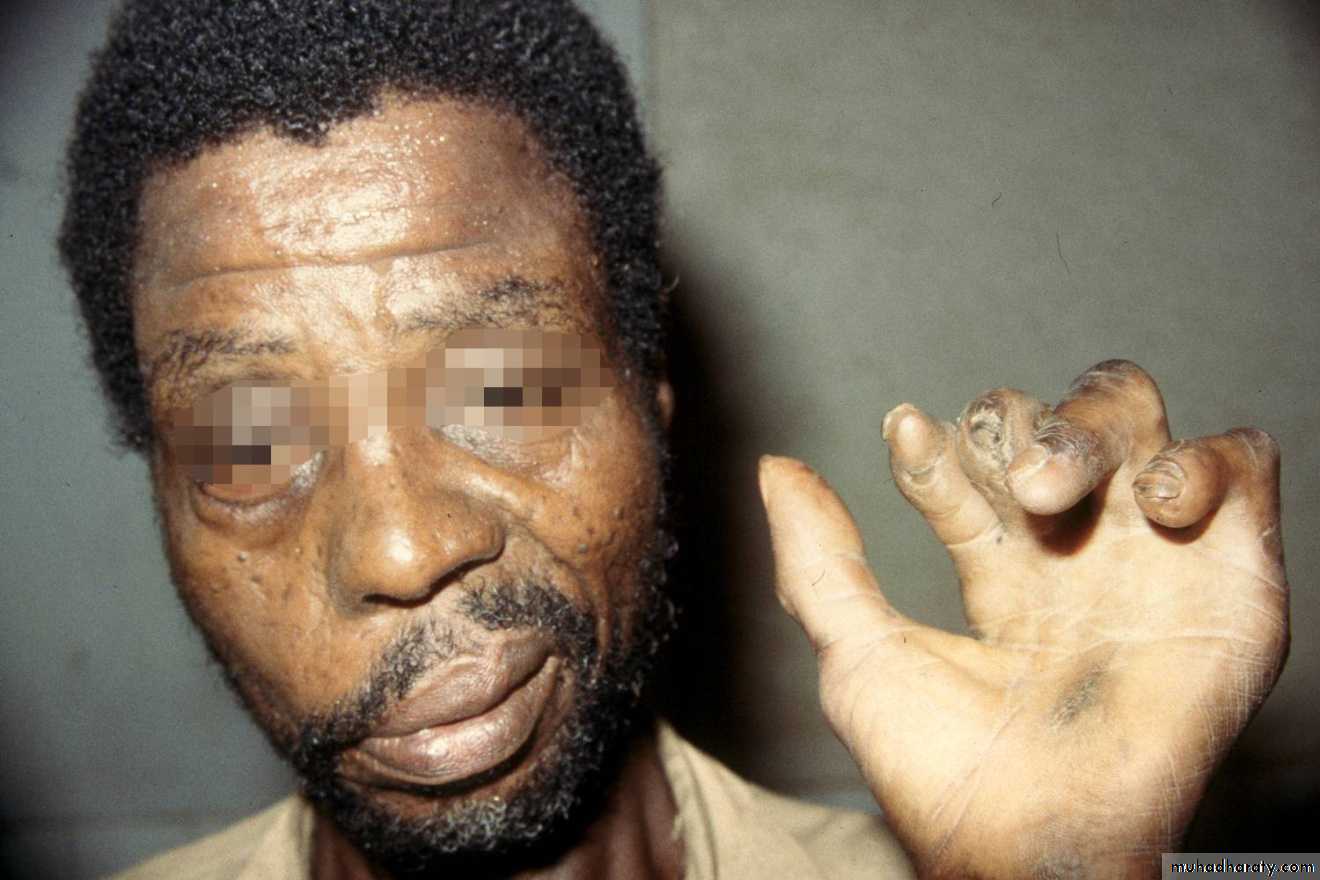
Patient with facial nerve palsy and contractures of the hand
Chronic insensate patch due to leprosy infection
Characteristic clawed hand deformity caused by ulnar involvement in leprosy
Chronic nonhealing ulcer at the metatarsal head resulting from loss of sensation in the feet
Multiple flat hypopigmented lesions on shoulder and neck, suggestive of multibacillary leprosy. Note ulceration of hypothenar area of hand, indicative of ulnar neuropathy
Man with advanced deformities caused by unmanaged leprosy. Keratitis, loss of eyebrow, thickened skin, and typical hand impairments
Laboratory Studies
1-Skin smear positive for acid-fast bacilli2-Laboratory studies include the following:
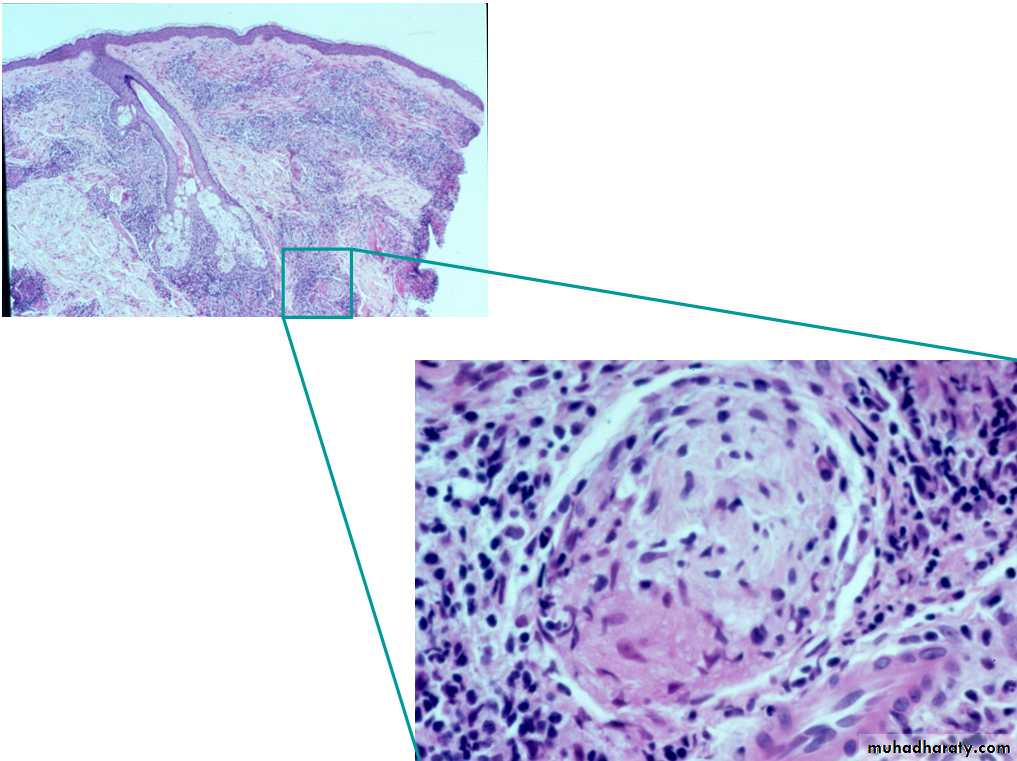
A-Skin biopsy, nasal smears, or both are used to assess for acid-fast bacilli
B-Serologic assays.
3-Laboratory tests related to drug treatment follow-up include the following:
a-CBC count
b-Creatinine level
c-Liver function tests
#Large numbers of acid-fast bacilli (in clusters) in histiocytes and within nerves. Fite-Faraco stain
Treatment
Type of LeprosyDaily, Self-Administered
Monthly Supervised
Months of Treatment
Paucibacillary
Dapsone 100 mg
Rifampicin 600 mg
6-12
Multibacillary
Dapsone 100 mg,Clofazimine 50 mg
Rifampicin 600 mg,Clofazimine 300 mg
24
Pediatric
Dapsone 2 mg/kg,Clofazimine 1 mg/kg
Rifampicin 10 mg/kg,Clofazimine 6 mg/kg#Corticosteroids have been used to treat nerve damage associated with leprosy,
Same as in adults
Increased pigmentation on the face due to clofazimine therapy
Patient with erythema nodosum leprosum type 2 reaction several weeks after initiation of drug therapy
Prognosis
Recovery from neurologic impairment is limited, but skin lesions generally clear within the first year of therapy. Discoloration and skin damage typically persist.Physical therapy, reconstructive surgery, nerve and tendon transplants, and surgical release of contractures have all contributed to increasing the functional ability in patients with leprosy.
A common residual deformity is insensitive feet, as seen in persons with diabetes.