PULMONARY VASCULAR DISEASE
Dr .Ghazi F. HajiSenior lecturer of cardiology
Al-Kindy College of Medicine
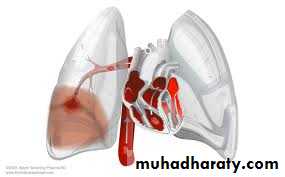
Deep venous thrombosis (DVT) and pulmonary embolism (PE)
Definition: Blockage of the pulmonary artery or it is tributaries due to dislodgment of thrombus from lower limb(90%) or pelvic vein or from heart or from pulmonary vein itself, might be come from left side of the heart if there is defect like VSD,ASD,PDA*Rare causes include septic emboli (from endocarditis affecting the tricuspid or pulmonary valves), tumour (especially choriocarcinoma), fat, air, amniotic fluid and placenta.
Vircow triad : one of the following (stasis ,injury , increase coagulation)
.Venous thromboembolism (VTE)
Immobility
Surgery Major abdominal/pelvic surgery -Hip/knee surgery Pregnancy/puerperiumCOPD -Congestive cardiac failure
Lower limb problems : Fracture -Varicose veins
Malignant disease
Miscellaneous
Increasing age -Previous VTE-
dehydration- Nephrotic syndrome -obesity-Thrombotic disorders –polycythemia –Trauma –drug contraceptive pill
Risk factors
Deep vein thrombosis :
SwellingTenderness
Warmth
Redness
DD? Cellulites – rupture baker cyst -lymphadenitis- hemoarthrosis
Clinical features
*Symptoms :sudden death- Faintness or collapse, crushing central chest pain, apprehension-sweating, severe dyspnoea if more severe after 2 days might be due to ARDS
*Signs :Major circulatory collapse: tachycardia, hypotension,↑ JVP, right ventricular gallop rhythm, loud P2, severe cyanosis, ↓urinary output sometime presented like asthma (wheezes )
Acute massive pulmonary embolism:.*
(sometime severe illness despit small pulmonary atery occleded ;this severity not due to occlusion but due to ARDS because of injuery to lung tissue)Pulmonary infarction; :Occlusion of segmental pulmonary artery → infarction ± effusion
*Symptoms :Pleuritic chest pain, restricted breathing, haemoptysis*Signs : Tachycardia, pleural rub, raised hemidiaphragm, crackles, effusion (often blood-stained), low-grade fever. Cough,cripitation
*
Acute small/medium PE
Pathophysiology :Chronic occlusion of pulmonary microvasculature,
Symptoms :Exertional dyspnoea. Late symptoms of pulmonary hypertension or right heart failureSigns :May be minimal early in disease. Later: RV heave, loud P2. Terminal: signs of right heart failure
Chronic PE
Ultra- sound (Doppler )Venogram
D dimer
chest radiography
Spiral CT
MRI
ECG
V/Q
ECHO
Pulmonary angiography
Investigations
*Clinical suspicion from history(surgery .previous DVT or PTE) et---
*Examination: swollen ,hot, tender leg unilateral
*Venogram :most of PTE is due to DVT; So venogram to calf thigh veins or pelvic vein (filling defect)is diagnostic
*Ultra- sound (Doppler ) :Colour Doppler ultrasound of the leg veins remains the investigation of choice
Non invasive, simple and easy to use
Chest radiography (for diagnosis and exclude DD)
Normal appearances in an acutely breathless and hypoxaemic patient should raise the suspicion of PTEA variety of non-specific appearances have been describe:
@Pulmonary opacities ,wedge shap opacity ,
@Horizontal linear opacity,pleural effusion usually bloody ,
@Oligemia (WESTERMARK SIGN),enlarged pulmonary artery.elevated diphragm. Hamptoms hump
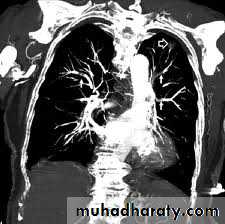
CT scan and angiogram – it is comfirmative and can detect the pulmonary artery and it is branches (As contrast may be nephrotoxic, care should be taken in patients with renal impairment and the use of iodinated contrast media should be avoided in those with a history of allergy to it).
50%
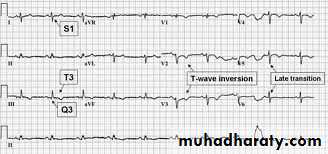
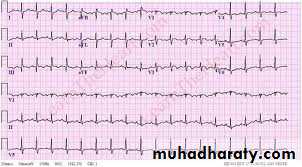
The ECG is often normal :
but is useful in excluding other important differential diagnoses such as acute myocardial infarction and pericarditis.
The most common abnormalities in PTE include:
*Sinus tachycardia
Incomplet or complet RBBB
*Anterior T-wave inversion but are non-specific; *Right heart strain revealed by an S1Q3T3 pattern,
the appearance of right bundle branch block &RVH
Electrocardiography
Radioactive scanning procedures :
Technitium scan can show PTE;but bronchogenic carcinoma ,pneumonia ,pulmonary edema all mimic PTE :
SO it better to do ventilation- perfusion scan then match them --- in PTE not matching
Arterial blood gases
Arterial blood gases typically show a reduced PaO2, a normal or low PaCO2,
D-dimer is a specific degradation product released into the circulation when cross-linked fibrin undergoes endogenous fibrinolysis . SENSETIVE 90%
low D-dimer levels (< 500 ng/mL measured by ELISA), particularly where clinical risk is low, have a high negative predictive value(no DVT/PET)
NEGATIVE PREDICTIVE VALUE
The D-dimer level >.500 ng/ml (if high risk ;should treated .if low risk should do another investigation including doppler study ,CT scan ,V/P mismatching)
*Other circulating markers : troponin I and brain natriuretic peptide, are under investigation.
D-dimer and other circulating markers
#Right ventricular enlargement or hypokinesis, especially free wall hypokinesis, with sparing of the apex (the McConnell sign) ,and thrombus (embolism in transit) may be visible( Direct visualization of thrombus (more likely with transesophageal echocardiography))
#Tricuspid regurgitation
Echocardiography
Pulmonary angiography
may be used in selected settings or for delivering catheter-based therapies.Preventive measures :avoid prolong bed rest (use stocking to prevent DVT)
*Treated the risk factors like dehydration ,congestive heart failure*Prophylaxis : in patient at risk to develops PTE and need to do surgery (should give anticoagulant but ask surgeon to cure from bleeding ) we give heparin 5000 iu /12h to prevent DVT or give iv dextran during operation
Preventive .
*If the patient has DVT with recurrent PTE and resistance to therapy( who has suffered massive hemorrhage on anticoagulation, or recurrent VTE despite anticoagulation, if the anticoagulation is contraindicated) --- mechanical measure use like inferior vena cava plication(interruption) (filter).
Oxygen
dopaminealfa phenylpherine
fluid with cuation if right ventricular dysfunction
Opiates
External cardiac massage
Anticoagulation(Heparine ,LMWH,warfarin)
Thrombolytic therapy -alteplase – urokinase
Embolectomy
Treatment
@If massive PTE :Oxygen should be given to all hypoxaemic patients
@Circulatory shock should be treated with intravenous fluids or plasma expander
@Diuretics and vasodilators should also be avoided, as they will reduce cardiac output.@Opiates may be necessary to relieve pain and distress but should be used with caution in the hypotensive patient.
@Resuscitation by external cardiac massage may be successful –to dislodging and breaking up a large central embolus
@Unfractionated heparin (UFH)antithrombine III inhibitor-Heparin 1000 iu /h during 24h ;follow up by PTT (partial thromboplastin time) 2-3 times than normal control
@subcutaneous low molecular weight heparin-inhibition of thrombin and Xa. The dose is based on the patient's weight and there is usually no requirement to monitor tests of coagulation
The duration of LMWH treatment should be at least 5 days, during which time oral warfarin is commenced. LMWH should not be discontinued until the international normalised ratio (INR) is greater than 2.
AnticoagulationIt is most easily administered as :
INR-is the ratio of the patient's prothrombin time to that of a normal control, raised to the power of the international sensitivity index (ISI, derived by comparison with an international reference standard material).(side effect is HIT-heparin induce thrompocytopenia).
There is difference between LMWH and UFH
warfarin (coumoarine) Vitamin K antagonis-orally before stopping heparin :because it is effect appear after 3days – the PT must be 2-3 time than normal control
Patients with a persistent prothrombotic risk or a history of previous emboli should be anticoagulated for life, whereas those with an identifiable and reversible risk factor usually require only 3 months of therapy.
#Thrombolytic therapy(lysis thrombus) streptokinase loading dose 250000-500000 iu then every hour 150000iu for 2days—
#Direct tissue plasminogen activator in catheter
#Thrombolysis is indicated in any patient presenting with acute massive PE accompanied by cardiogenic shock. (Patients must be screened carefully for haemorrhagic risk, as there is a high risk of intracranial haemorrhage).
#Surgical pulmonary embolectomy may be considered in selected patients but carries a high mortality risk
5-10% Of dead in hospital due to pulmonary thromboemolism
PrognosisMaternal mortality: VTE is the leading cause.
CTPA: may be performed safely with fetal shielding .It is important to consider the risk of radiation to breast tissue (particularly if family history of breast carcinoma) and the risk of iodinated contrast media to mother and fetus (neonatal hypothyroidism).V/Q scanning: greater radiation dose to fetus but less to maternal breast tissue.
Warfarin: teratogenic, so VTE should be treated with LMWH during pregnancy.(heparin in first and third trimester while warfarin in second trimister)
VTE and pregnancy
Pulmonary hypertension (PH) is defined as a mean pulmonary artery pressure > 25 mmHg at rest or 30 mmHg with exercise.Further classification is based on the degree of functional disturbance according to the New York Heart Association (NYHA) grades I-IV.
Although respiratory failure due to intrinsic pulmonary disease is the most common cause of pulmonary hypertension,
.
Pulmonary hypertension
#Hypertrophy of both the media and intima of the vessel wall,.
#marked narrowing of the vessel lumen#in situ thrombosis leads to an increase in pulmonary vascular resistance and pulmonary hypertension
Pathological features include
Pulmonary arterial hypertension
1-Primary pulmonary hypertension sporadic and familial (PPH) is a rare but important disease that affects young people, predominantly women, aged between 20 and 30 years
Related to: connective tissue disease (limited cutaneous systemic sclerosis)
2-Pulmonary venous hypertension
Left-sided atrial or ventricular heart disease /Left-sided valvular heart disease -Pulmonary veno-occlusive diseaseSClassification of pulmonary hypertension
3-Pulmonary hypertension associated with disorders of the respiratory system and/or hypoxaemia
COPD -DPLD -Sleep-disordered breathing -Alveolar hypoventilation disorders -Chronic exposure to high altitude -Severe kyphoscoliosiS
4-Pulmonary hypertension caused by chronic thromboembolic disease -Sickle cell disease
Pulmonary hypertension presents insidiously and is often diagnosed late.@Typical symptoms include:
breathlessness, chest pain, fatigue, palpitation and syncope.
@Important signs include elevation of the JVP (with a prominent 'a' wave if in sinus rhythm), a parasternal heave (RV hypertrophy), accentuation of the pulmonary component of the second heart sound and a right ventricular third heart sound.
Clinical features
#ECG :show a right ventricular 'strain' pattern
#Chest X-ray :shows enlarged pulmonary arteries, peripheral pruning and right ventricle enlargement.
#Transthoracic echocardiography; Doppler: assessment of the tricuspid regurgitant jet provides a non-invasive estimate of the pulmonary artery pressure.
#Right heart catheterisation to assess pulmonary haemodynamics and measure vasodilator responsiveness, to guide further therapy.
Investigations
Pulmonary hypertension is incurable but new treatments have delivered significant improvements in exercise performance, symptoms and prognosis.
@All patients should be anticoagulated with warfarin, and oxygen, diuretics and digoxin prescribed as appropriate.
Specific treatment options include:
high-dose calcium channel blockers ,
PDE5 inhibitor- sildenafil,
prostaglandins such as epoprostenol (prostacyclin) or iloprost therapy,,
oral endothelin antagonist- bosentan. .
Management
@Selected patients can be referred for heart-lung transplantation
@pulmonary thrombo-endarterectomy may be contemplated in those with chronic proximal pulmonary thromboembolic disease.
@Atrial septostomy (the creation of a right to left shunt) decompresses the right ventricle and improves haemodynamic performance at the expense of shunting and hypoxaemia