Pleural Effusion
DefinitionCauses
Clinical presentation
Investigation
Treatment
* Regarding pleural effusion: all false except.
1- PE definied as accumulation of non-serous fluid within the pleural space
2- Myxoedema is one of the common causes of PE which is always bilateral.
3- In progression of disease , pleural rub often precede the development of an effusion.
4-Around 200 mL of fluid is required to be detectable on ultrasound or CT.
5- if Pleural fluid aspiration reveal; protein :serum protein ratio > 0.5 that represent transudate pleural effusion.
Pleura
The pleura is a thin membrane that covers the entire surface of the lung as well as the inner surface of the rib cage, diaphragm, and mediastinum.
There are two pleural membranes: the visceral pleura, and the parietal pleura, space between them is the pleural space.
A small amount of fluid normally in this space
Pleural fluid serves as a lubricant for the visceral and parietal pleura as they move against each other during inspiration and expiration.
The pressure within the pleural space is subatmospheric during quiet breathing.
Pleural fluid usually contains a small amount of protein and a small number of cells that are mostly mononuclear cells.
.
Definition of pleural effusion: The accumulation of serous fluid within the pleural space is termed pleural effusion.
While:
-The accumulation of frank pus is termed empyema
-The accumulation of blood is haemothorax,
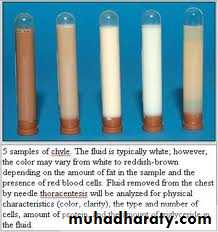
-The accumulation of chyle is chylothorax.
-Pleural fluid accumulates as a result of two ways either:
1-Transudative effusion: increased hydrostatic pressure or decreased osmotic pressure (as seen in cardiac, liver or renal failure),
2- Exudative effusion: increased micro vascular pressure due to disease of the pleural surface itself or injury in the adjacent lung.
Causes of pleural effusion Common causes
Pneumonia ('para-pneumonic effusion')
Tuberculosis
Pulmonary infarction*
Malignant disease
Cardiac failure*
Subdiaphragmatic disorders (subphrenic abscess, pancreatitis etc.)
Uncommon causes
Hypoproteinaemia* (nephrotic syndrome, liver failure, malnutrition)
Connective tissue diseases* (particularly systemic lupus erythematosus (SLE) and rheumatoid arthritis)
Acute rheumatic fever -- Post-myocardial infarction syndrome
Meigs' syndrome (ovarian tumour plus pleural effusion)
Myxoedema* Uraemia*
Asbestos-related benign pleural effusion
Clinical presentation
Signs and symptomThe onset either acute or may be insidious.
Breathlessness is the only symptom related to the effusion itself, and its severity depends on the size and rate of accumulation
Decrease chest expansion
Stony dullness in percussion
Diminish air entry on auscultation
Signs of pleurisy (a pleural rub) often precede the development of an effusion, especially in patients with underlying pneumonia, pulmonary infarction or connective tissue disease.
What findings on physical examination are suggestive of a pleural effusion?
&Small effusions (< 500 mL) frequently have minimal findings.
&Larger effusions: dullness to percussion, diminished breath sounds, and reduced tactile and vocal fremitus over the involved hemithorax.
&Large effusions (> 1500 mL), with concomitant atelectasis: bronchial breath sounds, egophony,
&Pleural friction rubs may be noted in the early stages or near resolution
Investigations imaging
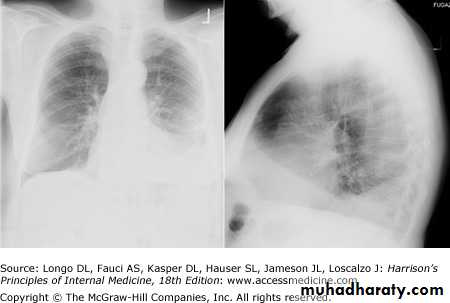
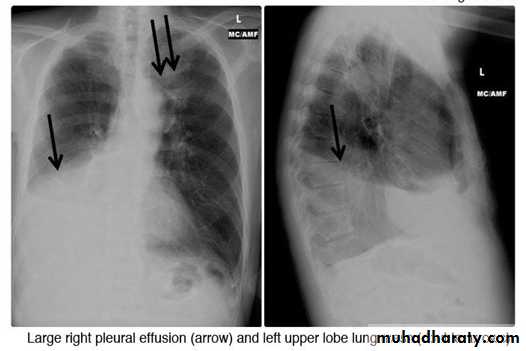
- (CXR) :The classical appearance of pleural fluid on the erect PA chest film is of a curved shadow at the lung base, blunting the costophrenic angle and ascending towards the axilla
Fluid appears to track up the lateral chest wall.
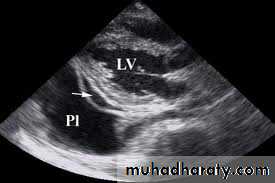
Around 200 mL of fluid is required to be detectable on a PA chest X-ray, but smaller effusions can be identified by ultrasound or CT.
Pleural fluid localised below the lower lobe ('subpulmonary effusion') simulates an elevated hemidiaphragm.
Fluid localised within an oblique fissure may produce a rounded opacity, simulating a tumour.
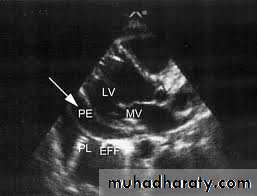
-Ultrasonography is more accurate than plain chest radiography for determining the volume of pleural fluid and frequently provides additional helpful information.
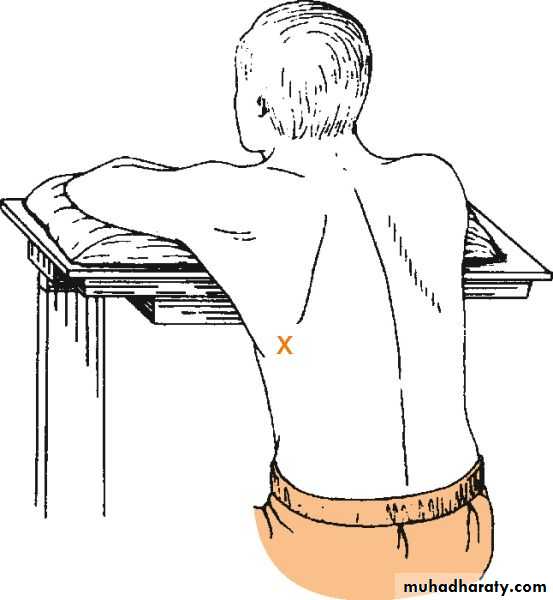
Visualization of fluid facilitates skin marking to indicate a site for safe needle aspiration and guides pleural biopsy, increasing diagnostic yield
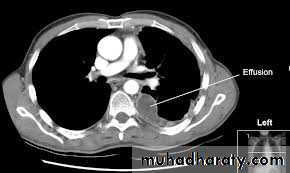
-CT displays pleural abnormalities more readily than either plain radiography or ultrasound, and may distinguish benign from malignant pleural disease
What other diagnostic procedures are available?
-Bronchoscopy, if the patient has a parenchymal abnormality on chest x-ray or CT scan.-Thoracoscopy, which allows direct visualization of the pleural surface, and guided or open pleural biopsy.
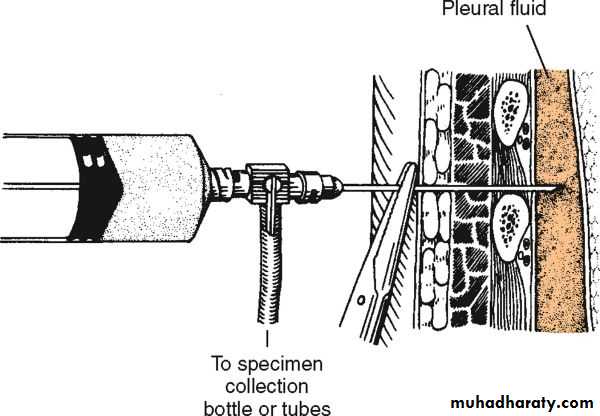
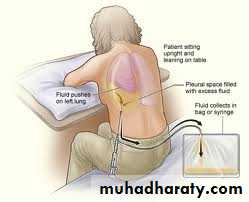
-Pleural aspiration and biopsy
-Combining pleural aspiration with biopsy increases the diagnostic yield, particularly when guided by either ultrasound or CT..
Simple aspiration provides information
-colour and texture of fluid and on appearance alone may immediately suggest an empyema or chylothorax. Or infection TB
The presence of blood is consistent with pulmonary infarction or malignancy, but may represent a traumatic tap.
Biochemical analysis allows differentiation of transudates from exudates
Gram stain may indicate parapneumonic effusion.
Cytological examination is essential, as the predominant cell type provides useful information.
A low pH suggests infection but may also be seen in rheumatoid arthritis, ruptured oesophagus or advanced malignancy.
Pleural aspiration and biopsy
((Light's criteria for distinguishing pleural ((exudate from transudatePleural fluid is an exudate if one or more of the following criteria are met:
1-Protein <3 g/dL
2-Pleural fluid protein:serum protein ratio > 0.5
3-Pleural fluid LDH:serum LDH ratio > 0.6
4-Pleural fluid LDH > two-thirds of the upper limit of normal serum LDH
Pleural effusion: main causes and features
otherPredominant cell
type
Appearance
Cause
Positive tuberculin testIsolation of M. tuberculosis from pleural fluid (20%) Positive pleural biopsy (80%)
Lymphocyte
exudate
Serous .usually amber
tuberculosis
Positive pleural biopsy (40%)Evidence of malignant disease elsewhere
Serosal cells and lymphocytes
Often clumps of malignant cells
Exudate
Serous, often blood-stained
Malignant disease
Other evidence of left ventricular failureResponse to diuretics
Few serosal cells
Transudate
Serous, straw-coloured
Cardiac failure
Evidence of pulmonary infarctionSource of embolism
Red blood cellsEosinophils
Exudate (rarely transudate)
Serous or blood-stained
Pulmonary infarction
Other manifestations of SLEAntinuclear factor or anti-DNA in serum
Lymphocytes and serosal cells
Exudate
Serous
SLE
chylomicron
non
Milky
Chyle
Obstruction of thoracic duct
High amylase in pleural fluid (greater than in serum)
No cells predominate)
Exudate
Serous or blood-stained
Acute pancreatitis
Management
Therapeutic aspiration may be required to palliate breathlessness, but removing more than 1.5 L in one episode, is inadvisable as there is a small risk of re-expansion pulmonary oedema.
An effusion should never be drained to dryness before establishing a diagnosis, as further biopsy may be precluded until further fluid accumulates.
Treatment of the underlying cause-for example, heart failure, pneumonia, pulmonary embolism or subphrenic abscess-will often be followed by resolution of the effusion.
What is the significance of a parapneumonic effusion?
. A parapneumonic effusion is any effusion associated with pneumonia. Up to 40% of all pneumonias may be associated with a pleural effusion. Morbidity and mortality rates are higher in pneumonias with effusion than in pneumonia alone.Most effusions resolve without specific intervention. However, the effusion may be complicated and require tube thoracotomy (chest tube) or surgical decortication
Single choice
Regarding pleural effusion: all false except.
1- The accumulation of non-serous fluid within the pleural space
2- Myxoedema is always bilateral and common cause
3- a pleural rub often precede the development of an effusion
4-Around 200 mL of fluid is required to be detectable on ultrasound or CT.
5- Pleural fluid protein:serum protein ratio > 0.5 represent transudate pleural effusion.