Unit 2: Bacteriology
105
Lecture 1+2+3 - Enteric gram-
negetive rods (enterobacteriaceae)
Enteric bacteria or coliform
General Characteristics:
A large heterogeneous group of G-ve rods (non-spore
forming), natural habitat is the G.I.T. of humans and
animals, motile with peritrichous flagella or non-motile,
aerobes and facultative anaerobes, ferment not oxidize
carbohydrate, catalase +ve, oxidase-ve.
It most common cultured in laboratory, includes more
than 25genera & 110 spp., only 20-25 spp. are clinically
significant. the most common are :
1) Escherichia coli (part of intestinal normal flora) cause
disease incidentally.
2) Klebsiella-Enterobacter-Serratia group.
3) Proteus-Morganella-Providencia group.
4) Citrobacter (2,3,4,are as intestinal normal flora and
incidentally cause disease but less than E.coli).
5) Shigella
6) Salmonella (Both Shigella & Salmonella are regularly
pathogenic for humans)
7) Other Enterobac.:Yersinia, Edwardsiella, Ewingella,
Hafnia, Cedecea, Kluyvera
Enteric bacteria produce a variety of toxins and
other virulence factors and enzymes, include:
1) LPS (endotoxin) have pathophysiological effects: fever,
leukopenia, hypotension, hypoglycemia, activation the
complement cascade, and disseminated intravascular
coagulation (DIC).
2) Most of G-ve rods produce exotoxins such as
enterotoxins and these toxins, has 2 types:
A. heat-labile exotoxin (LT Exotoxin): under genetic
control transmissible plasmid .
LT exo. Contains 2 subunits (A&B): subunit B binds
toGmI ganglioside at the brush border of epithelial cells
of the small intestine and facilitates the entry of subunit
A, which activates adenylyl cyclase → increase the
concentration of cAMP and → hypersecration of
sodium and lead to the diarrhea.
B. Heat-stable enterotoxin (ST Enterotoxin): activates
guanylyl cyclase in enteric epithelial cells and stimulate
fluid secretion and lead to the diarrhea.
3) R-factor (R plasmid) & colonization or adherence
factors.
4) Bactriocins (Colicins): Virus-like bactericidal substances
are produced by certain strains of bacteria against other
strains of the same or closely related spp.; their production
is controlled by plasmid . It can be used for typing of
bacteria because bacteriocin-producing strains are
resistant to their own bacteriocin .
Antigenic structure
1) antigen (Somatic Ag):
•
Side chain of the cell wall LPS, consist of
polysacchride heat-stable.
•
Eneric bac. are classified by more than 150 O–
Ags. Antibodies to these Ags. are IgM.
2) K–Ag. (Capsular Ag): external to O–Ags. on some
bacteria, heat-labile polysacchride or proteins , more than
100 K-Ags. Associated with virulence, Salmonella typhi
→ capsular Ag.(Vi Ag.).
3) H- Ag. (Flagellar Ag): a protein heat-labile or alcohols,
more than 50 H – Ags., Abs. to H-Ags. are IgG.
Diseases caused by enteric bacteria:
Generally as normal flora in intestine or upper
R.T.,pathogenic only when they reach tissues (U.T.,biliary
T., other abdominal sites,lungs,bone, meninges,prostatic
G.) ,and may cause bacteremia.
Either hospital- or community- acquired infection
1) Escherichia coli
General Characteristics:
• Lactose fermented (pink colonies→ MacConkey`s agar),
green metallic sheen colonies on EMB agar.
• Fermentative for mannitol & glucose with gas production.
• Hemolysis on blood agar, only when isolated from urine (UTIs)
Pathogenesis:
Depends on the site of infection, cannot differentiated by
symptoms from other bacteria.
-The main infections are:

Unit 2: Bacteriology
106
1) UTIs (urinary tract infections):
E.coli is the most common of UTIs.(90% in young
women).The symptoms includes: urinary frequency,
dysuria , hematuria , pyuria , & flank pain with upper UTIs.
UTIs can result in bacteremia with clinical sings of sepsis.
Nephropathogenic E.coli
(have specific O-Ags types &
produce hemolysin).
Pyelonephritis (have a specific types of pilus, P pilus).
2) Diarrheal disease:
Classified according to their virulence factors to :
A. EPEC (Enteropathogenic E.coli): diarrhea in infants &
outbreaks diarrhea in nurseries in developing countries .
Virulence factors: chromosomally mediated factors cause
tight adherence of EPEC to the mucosal cells of the small
intestine, entry to these cells →watery diarrhea (self-
limited or chronic), can treated by antibiotics. EPEC have
specific serotypes of O&H Ags.
B. ETEC (Enterotoxigenic E.coli): traveler`s diarrhea &
infants diarrhea in developing countries.
Virulence factors: colonization factors adherence it to
epithelial cells of small intestine, some strains produce LT
exotoxin others ST enterotoxin & some produce both of
them.
C. STEC (Shiga toxin producing E.coli) or EHEC
(Enterohemorrhagic E.coli): has been associated with-
1. hemorrhagic colitis (a severe form of diarrhea)
2. hemolytic uremic syndrome (a disease resulting in
acute renal failure, microangiopathic hemolytic
anemia, and thrombocytopenia)
• (E.coli O157:H7 strain).There are at least 2 antigenic
forms of the shiga-like toxin (shiga-like toxin -1 & -2).
D. EIEC (Enteroinvasive E.coli):
diarrhea in children in developing countries & traveler`s
to these countries (invading intestinal mucosal cells).
E. EAEC (Enteroaggregative E.coli):
acute & chronic diarrhea in developing countries & as a
food – borne illness in industrialized countries .Suggested
that it adheres to the intestinal mucosa & elaborates
enterotoxin & cytotoxin →mucosal damage →secretion
mucous & secretory diarrhea .
3) Sepsis:
When host defenses are inadequate, E.coli may reach the
bloodstream & cause sepsis in newborns & as a secondary
to UTI in adults.
4) Meningitis: E.coli & group B streptococci are the leading
causes of meningitis in infant (neonatal meningitis).75% of
E.coli from meningitis cases have K1 Ag.
*NOTE: the presence of E.coli in the water (colony count
above 4/dLin drinking water) unacceptable feacal
contamination, killed by chlorination of water.
2- Klebsiella-Enterobacter-Serratia Group
General Characteristics:
K.: lactose Fermentaion rapidly, viscous (mucoid)
colonies because it have a large capsule, non-motile.
E.: lactose F. rapidly, raised colonies (small capsule), motile
S.: lactose F. slowly, may be pigmented colonies ,motile.
Pathogenesis:
K. pneumoniae
: in 5% of normal persons (in R. T. &
feces). It cause 1% of bacterial pneumonia (extensive
hemorrhagic necrotizing consolidation of the lung),
occasionally cause UTI & bacteremia with focal lesions in
debilitated patients .
K. pneumoniae subsp. Ozaenae
: hospital-acquired
infection (upper R.T.) ,isolated from the nasal mucosa, a
fetid, progressive atrophy of mucous membrans.
K. pneumoniae subsp. rhinoscleroderma
: cause
rhinoscleroma (destructive granulomatous disease of the
nose & pharynx ).
K. granulomatis
(formerly Calymmatobacterium
granulomatis) causes genital ulcerative disease.
E. aerogenes
: free-living in GIT , opportunistic cause
UTIs & sepsis .
S. marcescens
: a common opportunistic pathogen in
hospitalized patients, cause pneumonia, bacteremia &
endocarditis .Can be treated by 3ed–generation of
cephalosporins .
3- Proteus-Morganella-Providencia Group
General characteristics:
• Proteus: non-lactose F.,very active motile (peritrichous
flagella)→swarming on blood agar ,urease +, susceptible
to antimicrobial drugs (penicillins).
• Morganella: non-lactose F., motile, urease + .
• Providencia: lactose F. slowly or not , urease .
Pathogenesis:
Proteus:
UTIs, bacteremia, pneumonia & focal lesions in
debilitated patients .
P. mirabilis
: UTIs & other infections .
P.vulgaris
: nosocomial infection .
The rapid motility of Proteus help to it invasion of the
U.T., & production of urease resulting rapid hydrolysis of
urea with liberation of ammonia (urine become alkaline)&
promoting stone formation.
Diagnosis by Weil-Felix test .
Morganella morganii:
nosocomial pathogen .
Providencia
(P. rettgeri ,P. alcalifaciens ,P.stuartii):
normal intestinal flora ,all cause UTIs & other infections ,
resistant to antimicrobial therapy .
Unit 2: Bacteriology
107
4- Citrobacter:
Lactose F. very slowly or not, motile, cause UTIs.
Diagnostic test for Enteric bacteria
• Specimens: urine, blood, pus, C.S.F., sputum, others.
• Culture: on both blood agar & differential media.
• Serological tests: agglutination with specific antisera .
• Variation in bacterial susceptibility is great, so antibiotic
sensitivity are essential .No single drug is available .
• Sulfonamides, ampicillin, cephalosporins, fluoroquinolons
& aminoglycosides .
Prevention & control
Depends on hand washing , rigorous asepsis , sterilization
of equipments , disinfections , strict precautions in I.V.
therapy & keeping U.T. catheters sterile .
Prophylaxis: using ciprofluxacin or trimethprim-
sulfamethaxzole .
Prevention of traveler`s diarrhea, daily ingestion of
bismuth subsalicylate suspension .
EPEC serotypes controlled by orally vaccines (a virulent
mutant strain ) or injection of killed bacterial suspension
Salmonella-Arizona group
Pathogenic by the oral route, transmitted from animals &
animals products to humans & cause enteritis
(enterocolitis), systemic infection & enteric fever.
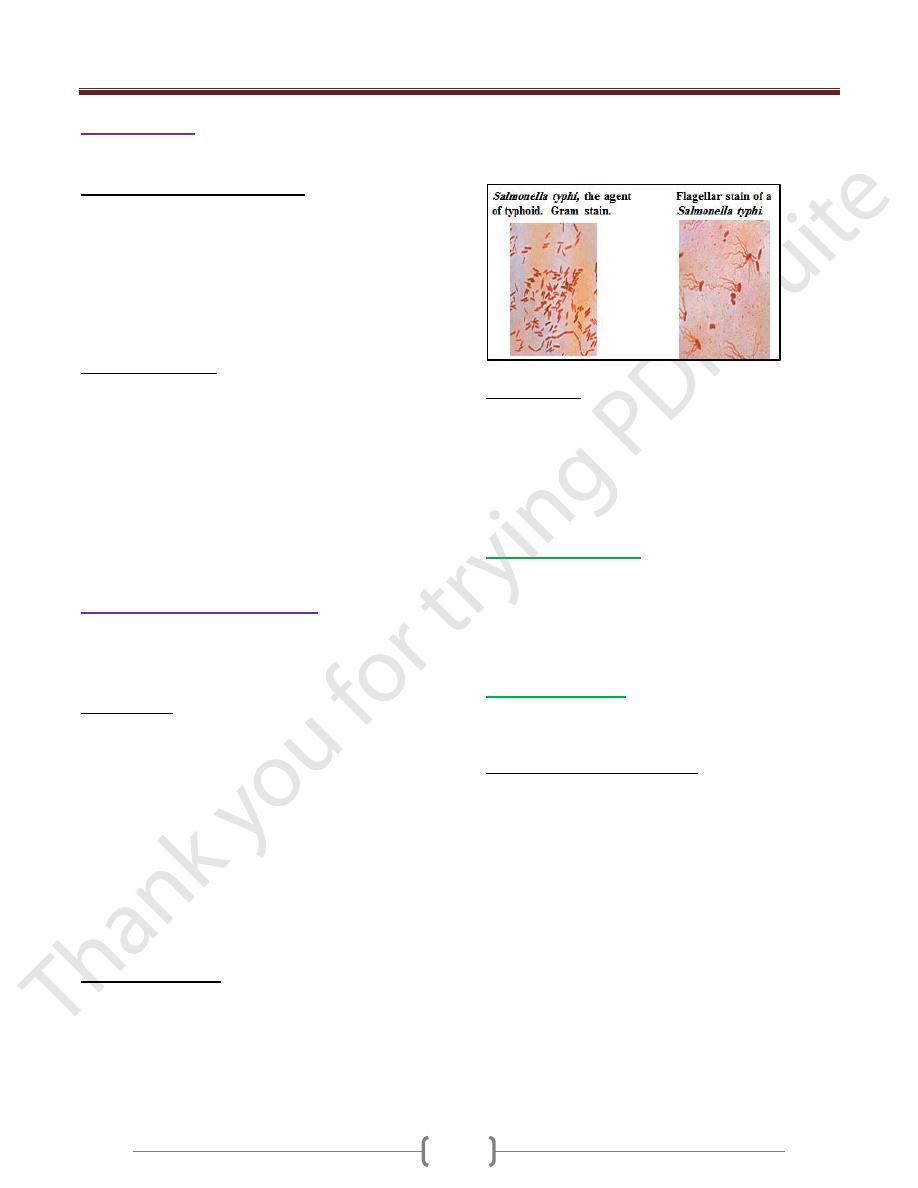
Morphology:
• Vary in length, motile with peritrichous flagellae. They
survive freezing in water for long periods & resistant to
certain chemicals (brilliant green, Na-tetrathionate & Na-
deoxycholate) that inhibit other enteric bacteria, so such
compounds useful for isolation salmonellae from feces.
• Aerobic or facultative anaerobic, grow in pH (6-8) & 15-
41 C° → produce large, smooth & circular colonies (2-3
mm in diameter).
• On MacConkey’s & deoxycholate-citrate agars → Pale
colonies (non-lactose fermented). Ferment glucose,
mannitol, mannose (with acid & with or without gas);
produce H
2
S (Black precipitate on TSI agar).
Antigenic Structure
1) H (flagellar) Ag: heat-labile protein & highly antigenic.
2) O (somatic) Ag: heat-stable polysaccharide (integral part
of LPS).
3) Vi (capsular or surface) Ag: heat-labile, related to virulence
Variation may occurs by lose H Ag (become non-motile),
lose of O Ag (change from smooth to rough colony form)
& lose of Vi Ag partially or completely.
Classification
• 4 serotypes(group1)causes enteric fever (primarily
infective for humans):
Salmonella Paratyphi A(serogroup A)
S. Paratyphi B (serogroup B)
S. Typhi and S. Enteritidis (serogroup D)
S. Choleraesuis (serogroup C
1
)
•
Currently, the genus Salmonella is devided into 2 species:
1. S.entterica (5 subsp.):
1.= = subsp.enterica (subsp.I)
2.= = subsp.salamae (subsp.II)
3.= = subsp.arizonae (subsp.IIIa),and
subsp.diarizonae (subsp.IIIb)
4.= = subsp.houtenae (subsp.IV)
5.= = subsp.indica (subsp.VI)
2. S.bongori (subsp.V)
Most human illness is caused by subsp.I strains, rarely by
IIIa, IIIb, & others, which found in cold-blooded animals.
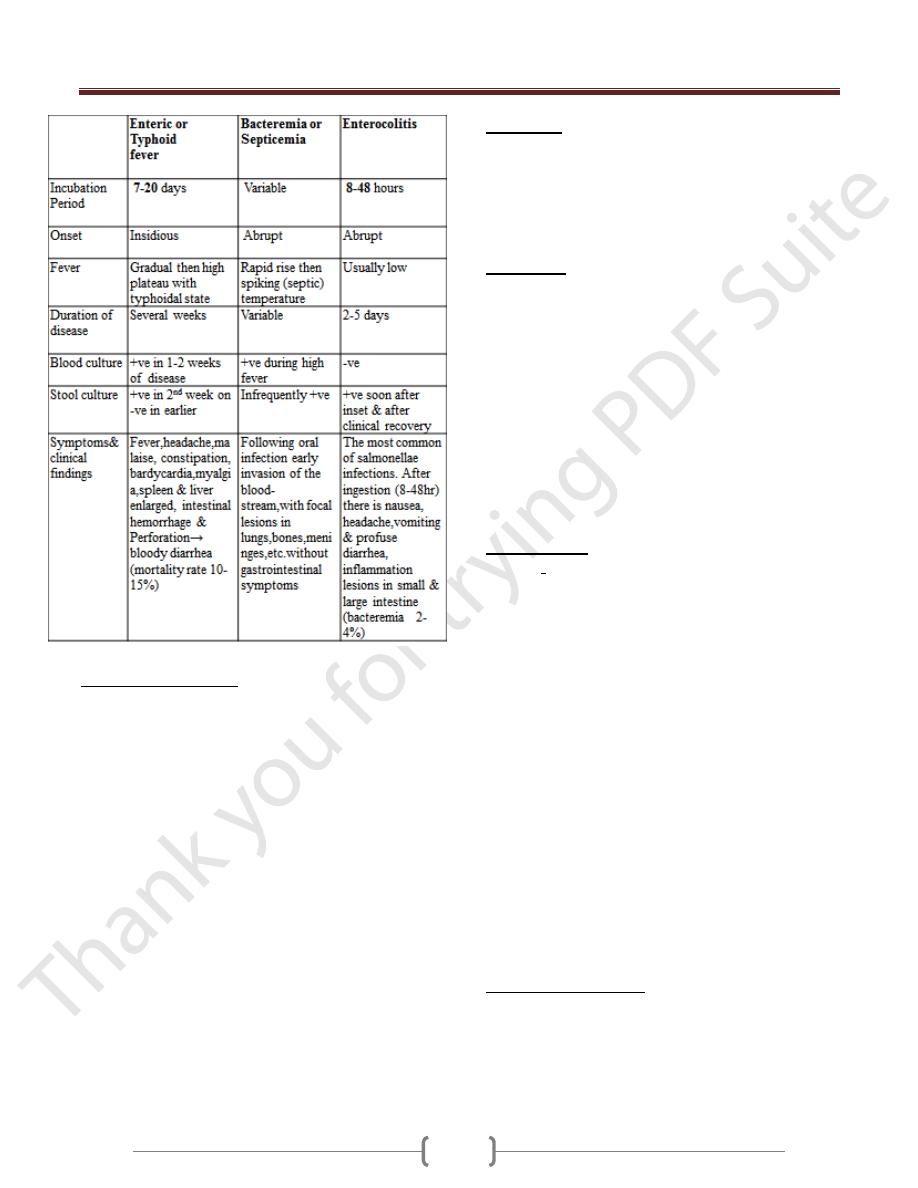
Pathogenesis & Clinical Findings
The majorities of salmonellae are pathogenic in animals
(poultry, pigs, rodents, cattle & others)- → the reservoir for
human infection. The bacteria enter via the oral route by
contaminated food or drink → produce 3 main types of
diseases (enteric or typhoid fever, bacteremia or septicemia
or systemic infection & enteritis or enterocolitis).
In typhoid fever: ingested S.Typhi reach the small
intestine →------ enter the lymphatics & bloodstream, the
blood carries them to many organs including the intestine
→------ bacteria multiply in intestinal lymphoid tissue &
excreted in stools. The lesions are hyperplasia & necrosis
of lymphoid tissues (e.g., Peyer’s patches), hepatitis, focal
necrosis of liver & inflammation of the gall bladder,
periosteum, lungs & other organs.
Unit 2: Bacteriology
108
Diagnostic Lab. Tests:
• Specimens: blood & stool (urine rare).
• Culture:
1) Differential media (MacConkey’s, EMB, Deoxycholate,
Bismuth sulfite agar).
2) Selective media (SS, XLD, Hektoen enteric agar).
3) Enrichment media usually for stool (Selenite F broth or
tetrathionate broth, incubation (1-2days) →- plated on
differential & selective media.
4) Biochemical reaction patterns (TSI agar→------ black
precipitate).
• Serological tests:
1) Agglutination test: serotyping for unknown culture +
commercial kit, known sera (anti-O Ags for serogroups
salmonellae A, B, C
1
, C
2
, D & E).
2) Widal test (tube dilution agglutination): determination of
antibody titer in patient serum. The result as following:
a) High titer O (≥ 1:160)- → Active infection.
b) High titer H (≥ 1:160)- → Passive infection or past
immunization.
c) High titer Vi (in some carriers).
Immunity:
• Secretory IgA may prevent attachment of salmonellae to
intestinal epithelium.
• Circulating Abs to O & Vi are related to resistance of
infection →-relapses may occur in 2-3 weeks after recovery
in spite of Abs-→ reinfection milder than the 1
st
infection.
Treatment:
• Enteric fever & bacteremia require antimicrobial therapy
but enterocolitis do not, because the clinical symptoms &
excretion of the salmonellae may be prolonged by
antimicrobial therapy.
• In severe diarrhea, replacement of fluids & electrolytes is
essential.
• Therapy: Ampicillin, trimethoprim-sulfomethaxzole or
3ed-generation cephalosporine. In most carriers, the
organisms persist in the gall bladder (if gallstones are
present) &in the biliary tract. Chronic carriers cured by
ampicillin, but in most cases cholecystectomy must be +
drug treatment.
Epidemiology:
• Carriers: After manifest or subclinical infection, some
individuals continue to harbor salmonellae in their tissues
for variable length of time (convalescent carriers or
healthy permanent carriers). 3% of survivors of typhoid
become permanent carriers, harboring the organisms in
the gallbladder, biliary tract, or rarely, the intestine or
urinary tract.
• The feces of persons who have unsuspected subclinical
disease or carriers are a more important source, So food
handlers are shedding organisms. The contamination of
the following sources is important:
1) Water.
2) Milk & other dairy products (ice cream, cheese & custard
3) Shellfish.
4) Dried or frozen eggs.
5) Meat & meat products (poultry) or contaminated with
feces by rodents or humans.
6) Recreational drugs (Marijuana).
7) Household pest (dogs, cats, turtles, etc.).
8) Animal dyes (carmine) used in drugs, food & cosmetics.
Prevention & Control:
1) Sanitary measures must be taken to prevent contamination
of food & water.
2) Infected poultry, meats & eggs must be thoroughly
cooked
3) Carriers must not be allowed to work as food handlers.
4) Strict hygienic precautions.
Unit 2: Bacteriology
109
5) Vaccination:
a) 2 injections of acetone-killed S. Typhi followed by a
booster injection some months later→------ partial
resistance.
b) Oral administration of a live avirulent mutant S.Typhi
strain.
Shigellae (shigella)
Natural habitat is the intestinal tract of humans and
primates, causes bacillary dysentery.
Morphology & identification:
• Slender G-ve rods, coccobacillary in young culture,
facultative anaerobes, non-motile.
• Convex, circular, transparent colonies, non-lactose
F.(except S.sonnei), mannitol fermenters(except S.
dysenteriae).
• Antigenic structure: somatic O-Ag (LPS), more than 40
serotypes (share with other enteric bacilli).
•
Classification: on biochemical & antigenic structure,
pathogenic spp. are:
S.dysenteriae, S.flexneri, S.boydii,
S.sonnei.
Pathogenesis:
The infective dose is 10
3
organisms(10
5
-10
8
for
salmonellae & vibrios), it is limited to the GIT, invasion
of the mucosal epithelial cells by inducing phagocytosis,
escape from the phagocytic vacuole, multiplication &
spread within the cytoplasm then passage to adjacent
cells. Bloodstream invasion is rare. Microabscesses
formation in the wall of the large intestine & terminal
ileum lead to necrosis, superficial ulceration, bleeding, &
formation of pseudomembrane (consists of fibrin,
leucocytes, cell debris, a necrotic mucous membrane, &
bacteria). Granulation tissue fills the ulcers and scar
tissue forms. Blood & pus found in stools.
Toxins:
1) Endotoxin: Causes irritation of the bowel wall.
2) Shiga toxin (exotoxin): produced by S.dysenteriae type
1(Shiga bacillus) heat-labile, antigenic protein acting as
verotoxin of E.coli → inhibit sugars & amino acids
absorption in the small intestine & acting as neurotoxin →
----- CNS reactions, meningismus & comma → -----
severity & fatal infection of S.dysenteriae .
Clinical Findings:
After short incubation period (1-2 days)→ sudden
abdominal pain, fever & watery diarrhea. When infection
involves the ileum & colon → the No. of stools increases
(less liquid but contain mucus & blood).
In children & elderly, loss of water & electrolytes-→
dehydration, acidosis & death.
More than 50% of adult cases, fever & diarrhea subside
spontaneously in 2-5days, few patients-→chronic
intestinal carrier & recurrent of diseases.
Diagnostic Lab. Test:
Specimens: Fresh stool, mucus flecks & rectal swabs→
smear & culture.
Smear: Direct microscopic exam. Of stool-→ large No.
of leukocytes & RBC’s.
Culture: Using differential media (MacConkey’s agar,
EMB agar) & selective media (SS agar, Hektoen enteric
agar).
• Serology: Normal persons have Abs against Shigella spp.
→ not used for diagnosis.
Immunity:
Serum IgM (anti-O shigellae Ags) → not protect against
shigellae infection.
Treatment:
• Multiple drug resistance can be transmitted by R-factor so
resistant infections are wide spread.
• Ciprofloxacin, Ampicillin, Tetracycline, Trim.-
sulfamethasone & Chloramphenicol.
Epidemiology:
S. dysenteriae spread widely.
-Shigellae infections occur in children under 10 years,
transmitted from person-person by food, fingers, feces &
flies.
Prevention & Control:
Eliminating shigellae from reservoirs by:
1) Sanitary control of water, foods & milk; sewage disposal
&fly control.
2) Isolation of patients & disinfecting of excreta.
3) Detection of subclinical cases & carriers especially food
handlers.
Antibiotic treatment of infected individuals.
