Unit 2: Bacteriology
110
Lecture 4 – Pseudomonads,
Acinetobacter & Uncommon gram
negative bacteria
Pseudomonads
General characteristics:
Gram negative, motile, aerobic rods, some of which
produce water-soluble pigments. Habitat: soil, water, plant,
and animals. Small No. found in the normal intestinal flora
and on the skin of humans.
Medically important Pseudomonas:
1. Pseudomonas aeruginosa
Widely distributed and is present in moist environments in
hospitals and in the normal intestinal flora.. An important
nosocomial pathogen.
Morphology:
Gram negative rods, motile with polar flagellum, as a
single, pairs and short chains.
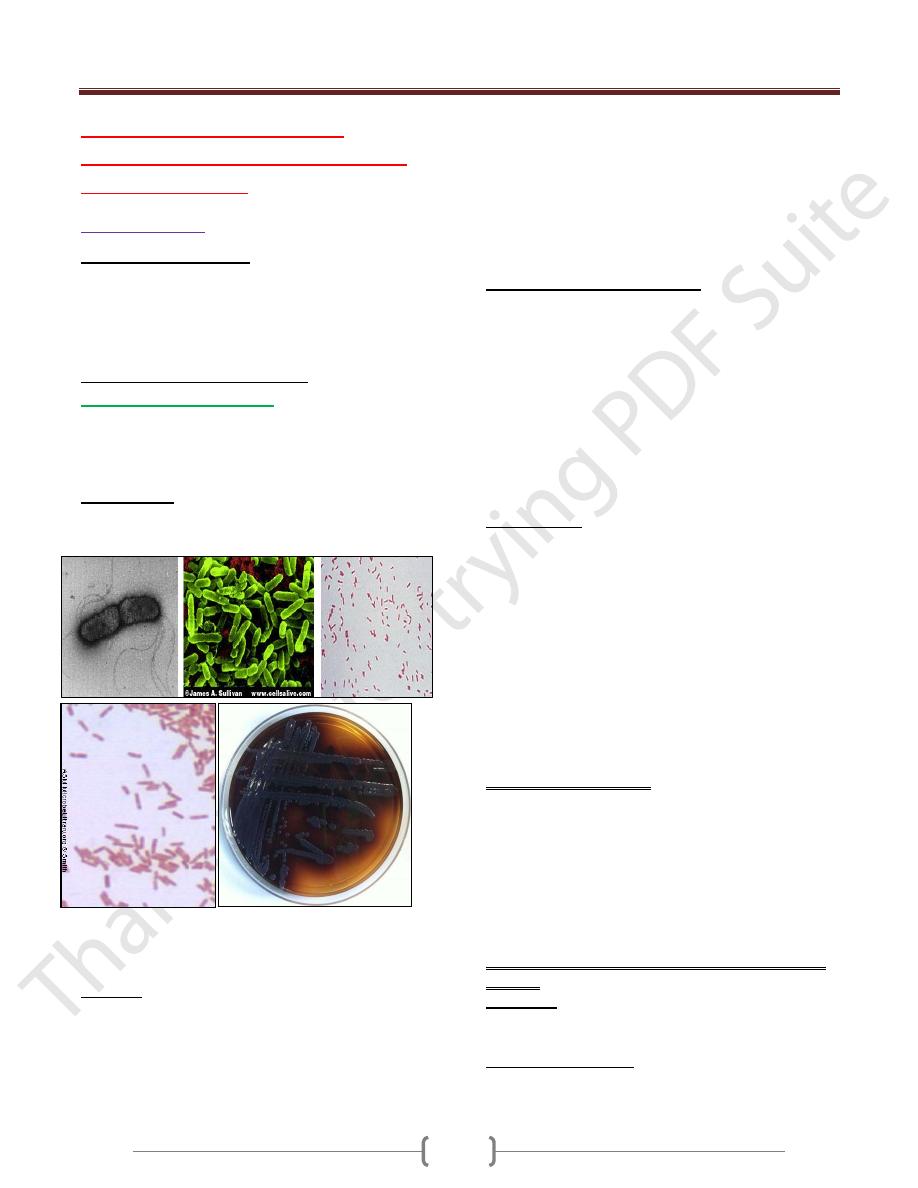
Three looks at Pseudomonas, the head of the Gram-negative
aerobic rods. A. Electron micrograph, negative stain. B.
Scanning electron micrograph. C. Gram stain.
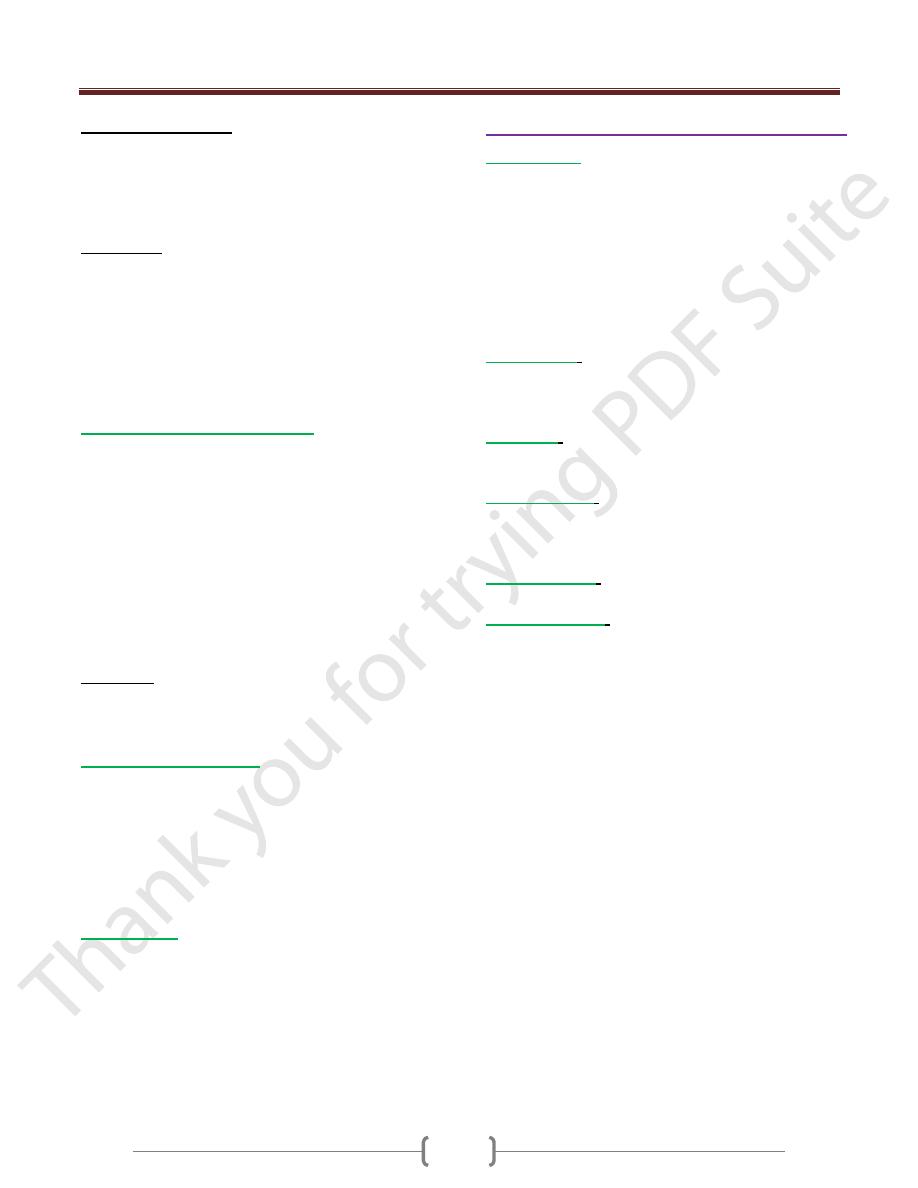
Culture:
Grows on many types of media, obligate aerobe, sometimes
producing a sweet or grape-like odor. Some strains
hemolysis blood.
It forms smooth round colonies with:
a fluorescent greenish pigment (Pyoverdin)
or non-fluorescent bluish pigment (Pyocyanin) or dark
red pigment (Pyomelanin).
Grows well at 37-42 C
˚,
42 C˚
helps in differentiation
P.aeroginosa from other spp., oxidase + , catalase + , dose
not ferment carbohydrates, but many strains oxidize
glucose, dose not ferment lactose → pale colonies on
MacConkey’s agar.
Antigenic Structure & Toxins:
1) Pili (attachment to host epithelial cells).
2) Polysaccharide capsule (mucoid colonies in culture from
patients with cystic fibrosis).
3) LPS (endotoxin).
4) Pyocin (bacteriocin).
5) Extracellular enzymes (elastases, proteases, and 2 type of
hemolysins: a heat-labile phospholipase C and a heat-staple
glycolipid).
6) Exotoxin A (causes tissue necrosis by blokes protein
synthesis).
Pathogenesis:
It is pathogenic only when there is abnormal host defenses
(mucous membranes & skin are disrupted by direct damage,
I.V. or urinary catheters are used or neutropenia as in
cancer therapy).The bacterium attaches & colonizes the
mucous membrane, invades locally and produces systemic
disease. These processes are promoted by the pili, enzymes,
& toxins described above.
LPS (endotoxin) causing fever, shock, oliguria,
leukocytosis, leukopenia & DIC & adult respiratory distress
syndrome. Pseudomonas are resistance to many
antimicrobial agents→ important when the normal flora are
suppressed.
aeruginosa infections are:
1) Wounds & burns infection (with blue green pus).
2) Meningitis (contamination due to lumbar puncture).
3) UTIs (by catheters).
4) RTIs (by respirators).
5) Otitis externa (in swimmers) & malignant otitis externa (in
diabetic patients).
6) Eye infection (after injury or surgical procedures).
7) Fatal sepsis (in infants or debilitated persons).
The symptoms are nonspecific & related to the organ
involved
Veroglobin: a breakdown product of hemoglobin, a
fluorescence pigment can be detected in wounds and burns
or urine.
Ecthyma gangrenosum: a hemorrhagic necrosis lesion of
skin occurs in sepsis due to P. aeruginosa are surrounds by
erythema without pus.
Unit 2: Bacteriology
111
Diagnostic Lab. Test:
Specimens: skin lesions, pus, urine, blood, c.s.f., sputum &
other materials.
Culture: the specific test for diagnosis of P. aeruginosa
infections.
Treatment:
Should not be treated with single-drug, because success rate
is low and the bacteria can rapidly develop resistance when
single drugs are used.
penicillin combination with aminoglycosides.
others: aztreonam, imipenem, ciprofloxacin, newer
cephalosporines
2. Burkholderia pseudomallei:
Causes melioidosis, an endemic glanders-like disease of
animals and humans, as acute, subacute, or chronic
infection. A localized suppurative infection can occur at the
inoculation site such as break in the skin, this may lead to
acute septicemic infection with involvement of many
organs.
The most commons of melioidosis is pulmonary infection
(pneumonitis).
May develop chronic suppurative infection with abscesses
in skin, brain, lung, myocardium, liver, bone and other
sites.
Treatment: Susceptible to tetracycline, sulfonamides,
chloramphenicol, amoxicillin & 3ed. Generation
cephalosporines.
3. Burkholderia mallei:
Cause glanders, a disease of horses and donkeys
transmissible to humans, may be fatal. Begins as ulcer of
the skin or mucous membranes followed by lymphangitis
(lymphatic thickening with nodules), & sepsis.
Inhalation of organisms may lead to primary pneumonia,
can be treated with tetracyclines plus aminoglycosides.
4. B.cepacia:
slow growth (may take 3 days for colonies are visible),
multidrug-resistant, causes necrotizing pneumonia and
bacteremia in patients with cystic fibrosis. In hospitals, it
has been isolated from a variety of water and environmental
sources from which it can be transmitted to patients and
from one cystic fibrosis patients to another by close contact.
Acinetobacter & Uncommon gram -ve bacteria
Acinetobacter:
coccobacillary or coccal (diplococci forms,
resemble neisseriae in smears, also recovered from female
genital tract has been mistaken for N.gonorhoeae and
recovered from meningitidis and sepsis has been mistaken
for N.meningitidis). Commensal but causes nosocomial
infections & as opportunistic pathogen & cause sepsis
(isolated from blood, sputum, skin, pleural fluid & urine).
-Resistant to antimicrobial agents. Therapy: difficult, but
responded to gentamicin, amikacin, tobramicin & newer
penicillins or cephalosporines.
Actinobacillus
: causes sever periodontal disease in
adolescents, endocarditis, abscesses, osteomyelitis and
others. Treatable with tetracycline or chloramphenicol and
penicillin G, ampicilline or erythromycin.
Alcaligenes
: as normal human flora, isolated from
respirators, nebulizers & renal dialysis systems & from
urine, blood, c.s.f., wounds & abscesses.
Capnocytophaga
: as oral human flora, causes bacteremia
and sever systemic disease in immunocompromised
patients and assotiated with wound infections from dog or
cat bites or scratches.
Cardiobacterium
: normal flora of upper R. T. & bowel
causes endocarditis.
Chromobacterium
: found in subtropical climates in soil &
water. Infects humans through breaks in the skin or via the
gut, cause abscesses, diarrhea, sepsis (many deaths).
