Unit 2: Bacteriology
123
Lecture 10+11 - zoonotic gram
negative rods
Zoonoses: are human diseases caused by organisms that
are acquired from animals (animal sources). There are
bacteria, viral, fungal & parasitic zoonoses. Some
zoonotic organisms are acquired directly from the animal
reservoir, others transmitted by vectors (mosquitoes, fleas
or ticks). There are 4 medically important G- rods (have
animal reservoirs):
Yersinia, Pasteurella , Francisella & Brucella species.
(YERSINIA, FRANCISELLA, & PASTEURELLA)
They are short; pleomorphic G- rods can exhibit bipolar
staining.
Yersinia
Y.pestis, Y. enterocolitica, & Y. pseudotuberculosis
Y.pestis:
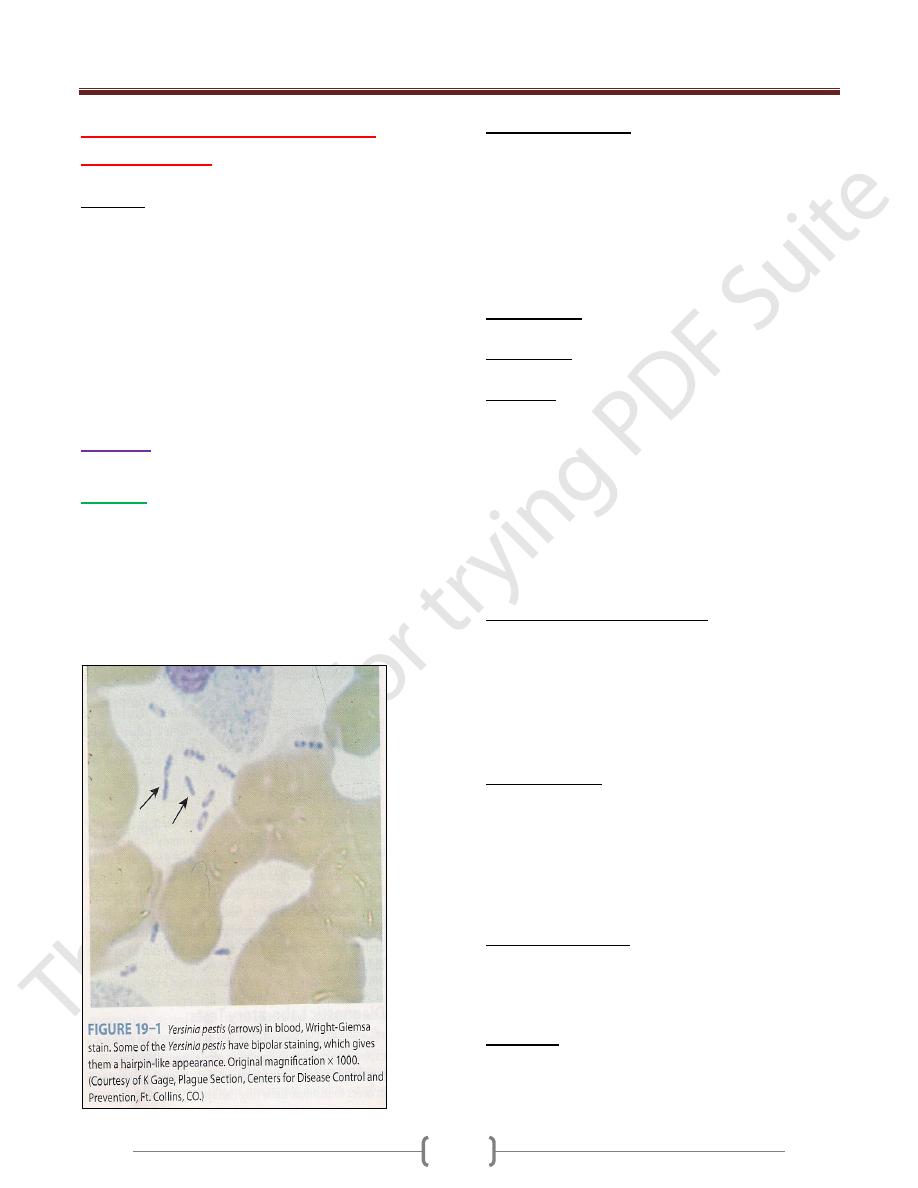
Short, pleomorphic G- rods, motile (like safety pin)
Bipolar staining by methylene blue & carbol fuchsin.
Causes plague.
Grow as a facultative anaerobic on media containing
blood or tissue fluids, freshly isolates possess capsule,
incubation at 37C˚ → gray viscous colonies, catalase+,
oxidase -
Antigenic Structure:
LPS (endotoxin activity).
Envelope contains protein = fraction 1 (antiphagocytic).
V & W antigens (proteins encoded by plasmid, lack of
this plasmid → avirulent strain used as vaccine).
Exotoxin (1μg is lethal in mice).
Pesticin= bacteriocin.
Note: There is a cross-reaction between Y.pestis &other yersiniae
Pathogenesis:
2 types of plague: Pneumonic p. & Bubonic p.
Pneumonic p.: results from inhalation of droplets or septic
emboli (contains the bacteria) that reach the lungs.
Bubonic p.:Y.pestis found in bacteremic rodent, blood
meal of flea ingests the bacteria which cause blood clots
in stomach (by bacterial coagulase), the bacteria trapped
in fibrin & proliferate → mass of bacteria block of
flea΄s intestinal tract → regurgitate the bacteria into next
animal or bites a human (the flea become hungrier &
loses its natural host, rodents).
The flea bite a human, inoculated bacteria → spread to
regional lymph nodes → swollen & tender (groin &
axillae) → buboes (bubonic p.).
Clinical Findings of bubonic p.:
Incubation period 2-7 days, high fever,
lymphoadenopathy, vomiting & diarrhea may develop.
DIC (hypotension, renal & cardiac failure),signs of
meningitis may appear.
Endotoxin-related symptoms (DIC & cutaneous
hemorrhages) → black death.
Diagnostic Lab.:
Specimens: blood, sputum, lymph aspirate & csf.
1) Smear: Giemsa’s stain or Wayson΄s stain.
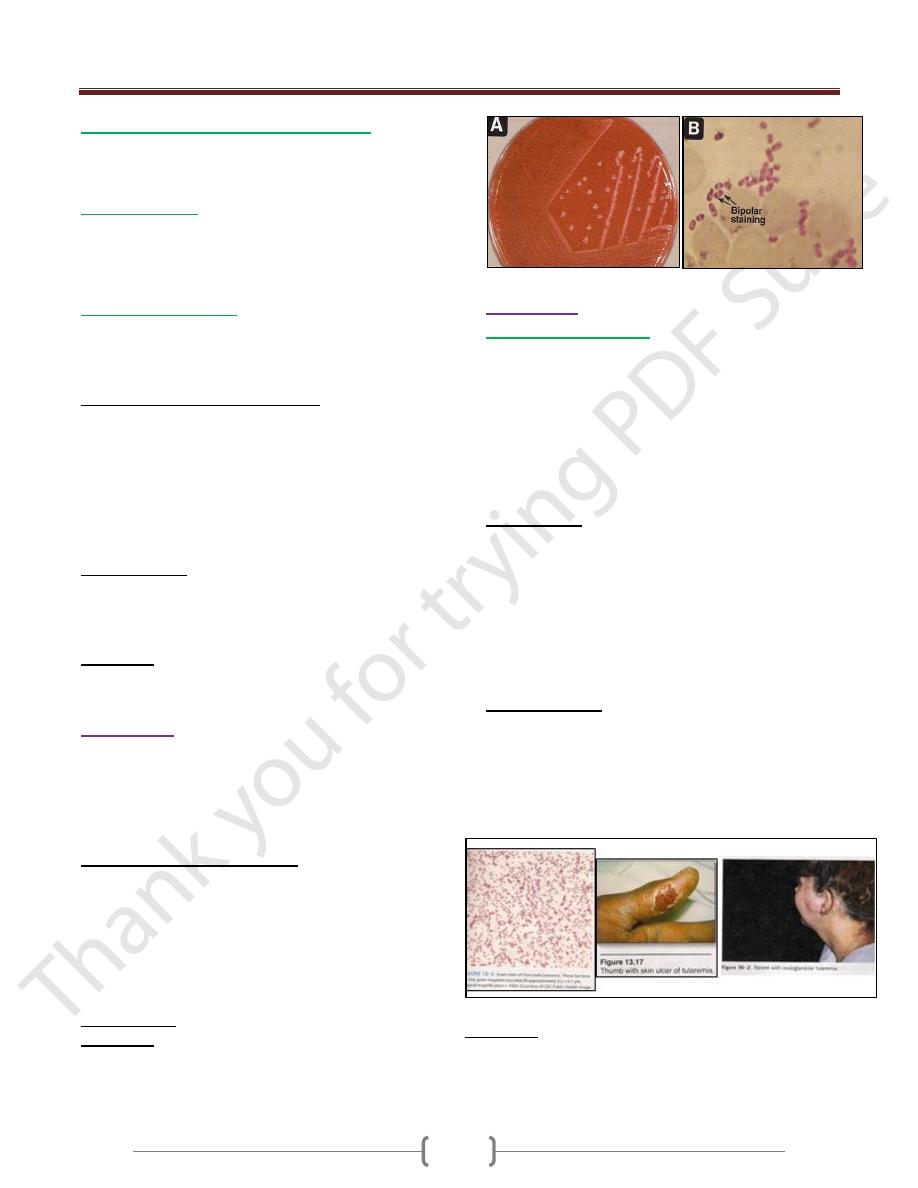
2) Culture: blood agar (is best confirmed by
immunofluorescence).
Serum Ab. Titer ≥ 1:16 is presumptive evidence of
Y.pestis infection.
Control & prevention:
1. Control of flea by insecticide.
2. Control of spreading of rodents.
3. Vaccine (formalin-killed bacteria).
Treatment:
Streptomycin (drug of choice), tetracycline (alternative or
give in combination with streptomycin).
Unit 2: Bacteriology
124
Y.enterocolitica & Y.pseudotuberculosis:
G-rods, urease +, grow best & motile at 25Cº but non-
motile at 37Cº. They are found in the intestinal tract of
animals.Both of them cause bacterimia.
Y.enterocolitica:
isolated from rodents & domestic animals (sheep, cattle,
swine, dogs & cats). Transmitted to humans by
contamination of food, drinks & fomites. Produce a heat-
stable enterotoxin.
Y.pseudotuberculosis:
Found in farm animals & birds which excreted in feces,
human infection → ingestion of materials contaminated
from animals feces.
Pathogenesis & Clinical Findings:
Incubation period = 5-10 days →yersiniae multiply in gut
mucosa of ileum →inflammation & ulceration
→leukocytes appear in feces, the infection extend to
mesenteric lymph nodes → blood (bacteremia).
Fever, diarrhea (watery or bloody because of invasion or
enterotoxin?), abdominal pain the right lower quadrant
suggesting appendicitis.
Diagnostic Lab.:
Specimens: stool & blood for culture.
Serology: agglutination test (cross-reaction with vibrios,
salmonellae & brucellae).
Treatment: Aminoglycosides, Chloramphenicol,
Ttimethoprime-sulfamethoxazole, & Piperacillin.
Pasteurella
Non-motile, G- coccobacilli with bipolar appearance on
stained smears, aerobic or facultative anaerobes, oxidase
+, catalase + & encapsulated bacteria.
The important species is
P.multocida.
Pathogenesis & Clinical Findings:
Part of the normal flora in the mouth of many animals
(domestic animals, cats & dogs), transmitted by biting,
capsule is a virulence factor & endotoxin is present in the
cell wall. No exotoxins.
Rapid onset of cellulitis at the site of cat bite. After cat
bites osteomyelitis developed (because cats teeth sharp
pointed implant bacteria under the periosteum).
Diagnosis Lab.: Culture the sample from wound site.
Treatment: Penicillin G.
Francisella
Francisella tularensis
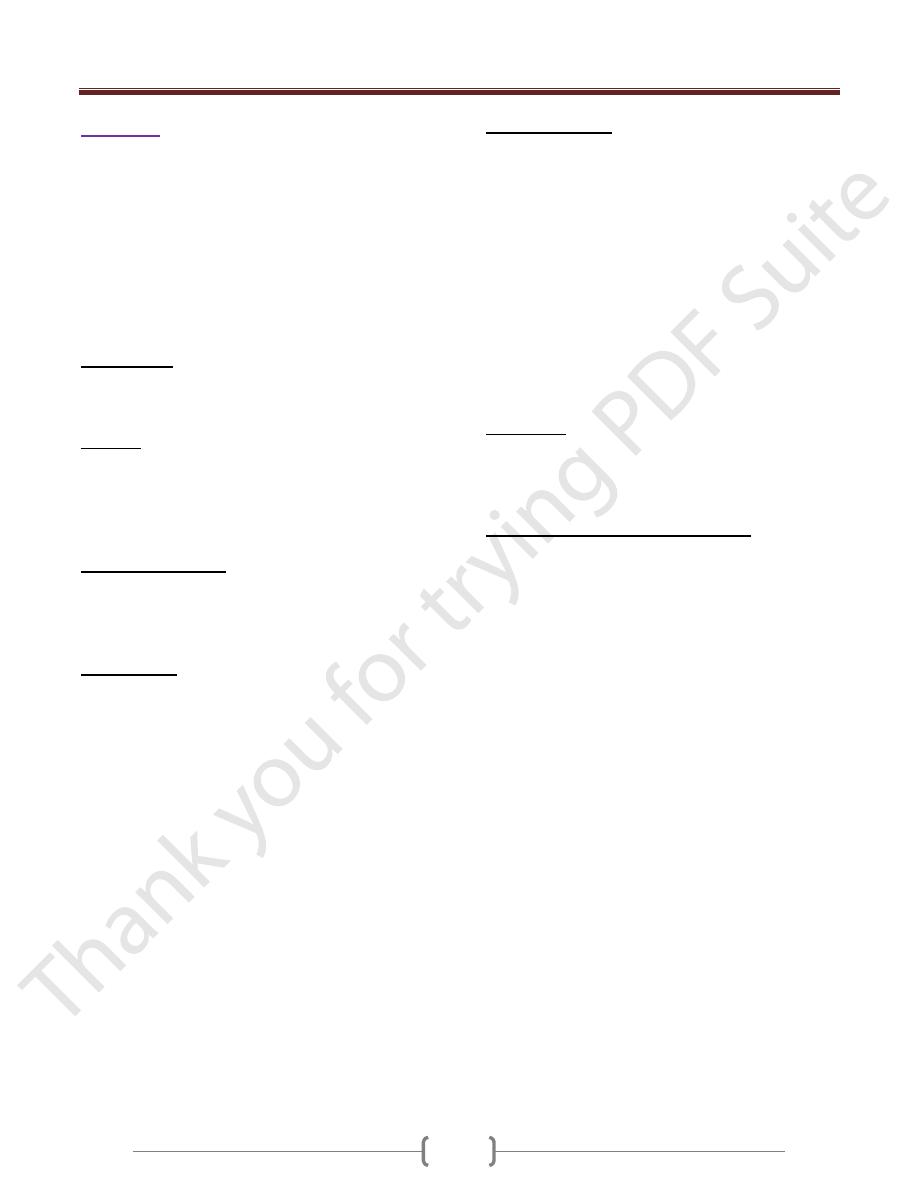
Small, G- pleomorphic rods, causes tularemia, transmitted
to humans by:
1) Biting arthropods (ticks).
2) Direct contact with infected animal tissue (rabbits &
deer).
3) Inhalation of aerosols.
4) Ingestion of contaminated food or water.
Pathogenesis:
Bacteria on skin abrasions (2-6 days) → an inflammatory
& ulcerating papule develops regional lymph nodes
enlargement.
Inhalation → peribronchial inflammation & pneumonitis.
Droplet or infected finger touches eye (conjunctiva) →
oculograndular tularemia.
Fever, malaise, headache & pain in the regional lymph nodes.
Diagnostic Lab.:
Specimens: Blood.
Agglutination test: titer 1:160 is highly suggestive if the
history or physical findings are compatible with the
diagnosis (cross-reaction with brucellae).
Culture: glucose blood agar or glucose cystine blood agar.
Treatment: Streptomycin or gentamicin for 10 days.
Unit 2: Bacteriology
125
Brucellae
They are cause brucellosis (undulant fever & Maltafever)
is characterized by an acute bacteremic phase then a
chronic stage may extend over many years & involve
many tissues.
4 species (infected humans):
1) Brucella melitensis (goats & sheep)
2) B. abortus (cattle)
3) B. suis (pigs)
4) B. canis (dogs)
Morphology:
G-, short coccobacillary, aerobic, non-capsulated, non-
spore forming & non-motile.
Culture:
Small convex, smooth colonies.
B. abortus requires 5-10 % CO
2
.Brucellae are oxidase,
catalase & urease positive, produce H
2
S & moderately
sensitive to heat & acid (in milk killed by pasteurization).
Antigenic Structure:
LPS: 2 antigens A & M (present in different proportions
in 4 species).
L antigen (resembles of Vi Ag of salmonellae).
Pathogenesis:
Obligate intracellular parasite transmitted from animal to
human (zoonoses).
The common routes of infection in human:
1) Intestinal tract (ingestion of infected & unpasteurized
milk, & cheese).
2) Mucous membrane by droplets.
3) Skin (contact with infected tissues of animals).
After infection, brucellae → lymph duct or channels &
lymph nodes → thoracic duct & bloodstream →
parenchymatous organs → granulomatous tissues
(abscess) in lymphatic tissue, liver, spleen, bone marrow
& other parts of reticuloendothelial systems.
The disease has 2 phases: acute bacteremic phase &
chronic phase.
Placentas & fatal membranes of cattle, swine, sheep &
goats contain erythritol (growth factor for brucellae). The
proliferation of brucellae in pregnant animals →
placentitis & abortion. No erythritol in human (no
abortion)
B. melitensis infections more sever & prolonged than B.
abortus infections which are more self-limited.
Clinical Findings:
After incubation period (1-6 weeks), insidious onset with
malaise, fever (rises in the afternoon & fall during the
night with drenching sweat), weakness, aches & sweats.
There may be gastrointestinal & nervous symptoms,
lymph nodes enlarge & the spleen becomes palpable,
hepatitis may be with jaundice → these generalized
symptoms subside in weeks or months but localized
lesions & symptoms may continue.
Chronic stage may develop (weakness, aches, pains, low-
grade fever, nervousness & other nonspecific with
psychoneurotic symptoms). The diagnosis of this stage is
difficult unless local lesions are present (brucellae cannot be
isolated from the patient but agglutinin titer may be high)
Treatment:
Brucellae susceptible to tetracyclines & ampicillin for few
days or prolonged for best results & combined treatment
(tetracycline + streptomycin or gentamicin).
Epidemiology, Prevention & Control:
Brucellae are zoonotic pathogens, so the infection is more
frequent in men because of occupational contact (farmers,
veterinarians, slaughterhouse workers). The majority of
infections remain asymptomatic (latent).
Eradication of brucellosis in cattle (immunization) &
examined by agglutination test. Active immunization of
humans with avirulent live strain 19.
Control by:
1) Limitation of spread & possible eradication of animals
infection.
2) Pasteurization of milk & milk products.
3) Reduction of occupational hazards wherever possible.
