Unit 3: Mycology
137
Lecture 1 - Introduction to mycology
Mycology (myco=fungus, logy=study)
Approximately 80,000 known species, less than 400 species
are medically important and less than 50 Species presently
known to be pathogenic for humans and other animals.
Fungi are eukaryotic organisms that do not contain
chlorophyll but have cell wall.
Fungi initially classified with plant kingdom, and then
fungi have transferred to the kingdom fungi.
Importance of Fungi:
Drug manufacturing (usually their waste products are to
our benefit)
Citric acid
Ethanol (yeast)
Antibiotic griseofulvin, penicillin
Cortisone (Rhizopus)
Immunosuppressive agents (cyclosporine)
Classification in mycology:
Fungi are classified on their ability to reproduce sexually,
asexually or by combination of both.
The first criteria are sexual morphological form; the
second set of criteria is based upon a sexual reproductive
structure
1) Ascomycota
– sexual reproduction in a sack called an
Ascus with the production of ascospores.
2) Basidiomycota
– sexual reproduction in a sack called a
Basidium with the production of basediospores.
3) Zygomycota
– A sexual reproduction by gametes while
sexual reproduction with the formation of Zycospores.
4) Fungi imperfecti
– nonrecognizable form of asexual
reproduction most pathogenic fungi.
Structure
Molds
Yeasts
Molds are aerobic,
filamentous fungi
including (mildews,
rusts & smuts)
Molds tend to grow on
surfaces rather than
throughout substrates.
Unicellular /
nonfilamentous
Yeast are fungi which
are: Typically sepherical
or oval & Faculatively
anaerobic
They are often observed
as powdery coatings on
plant material
The fungal cell has typical eukaryotic features including a
nucleus with a nucleolus, nuclear membrane and linear
chromosomes.
The cytoplasm contains organelles such as mitochondria
and the Golgi apparatus fungal cells, which have a rigid cell
wall external to the cytoplasmic membrane, differ from
mammalian cells. The composition of that wall makes fungi
different from bacteria and plants. Another important
difference from mammalians involves the sterol makeup of
the cytoplasmic membrane. In fungi, the dominant sterol is
ergosterol. In mammalian cells, it is cholesterol.
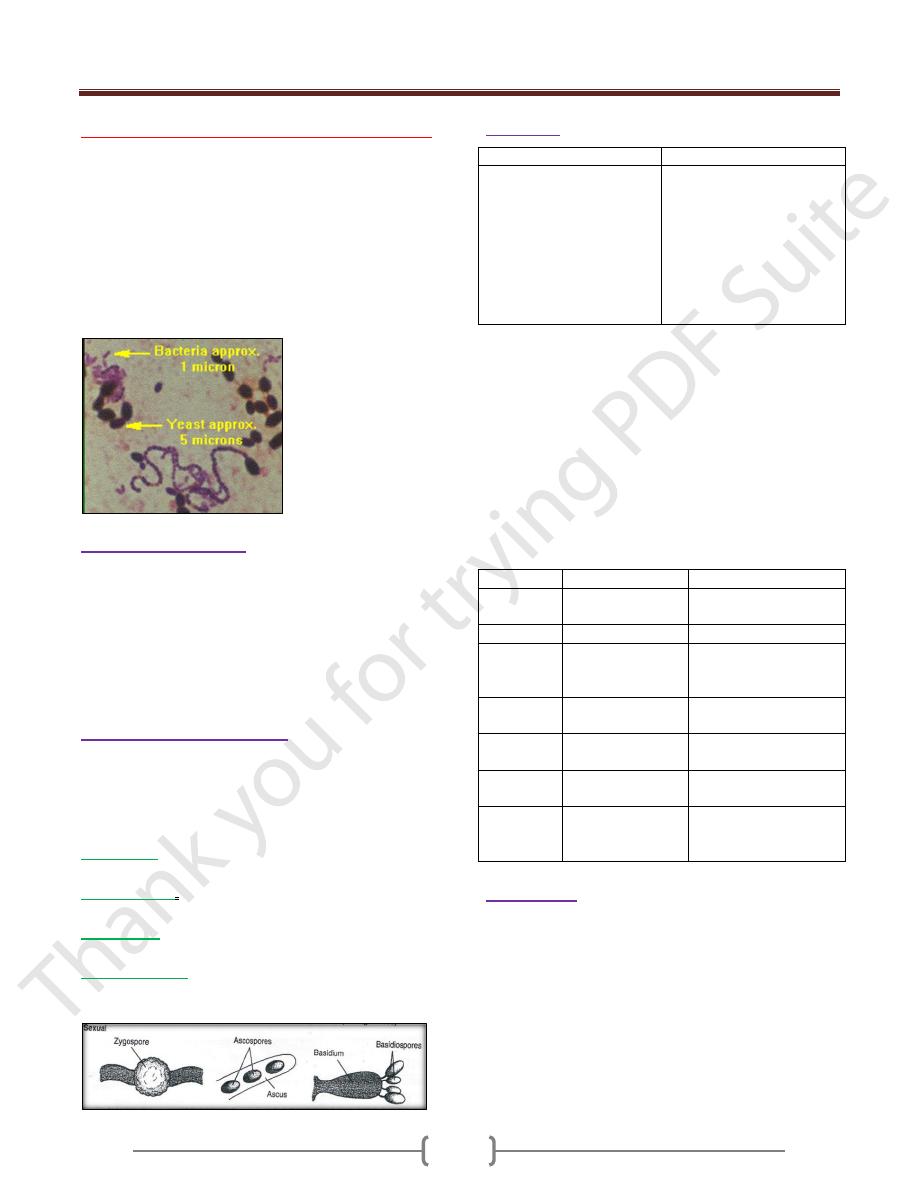
Feature
Fungi
Bacteria
Diameter
Approximately 4
µm (Candida)
Approximately 1µm
(staphylococcus )
Nucleus
Eukaryotic
Prokaryotic
Cytoplasm
Mitochondria and
endoplasmic
reticulum present
Mitochondria and
endoplasmic reticulum
absent
Cell
membrane
Sterol present
sterol absent (except
Mycoplasma)
Cell wall
content
Chitin
peptidoglycan
Spores
Sexual and asexual
reproduction
Endospores for survival,
not for reproduction
Metabolism
Require organic
carbon; no obligate
anaerobes
Many do not require
organic carbon; many
obligate anaerobes
Metabolism
Fungal growth requirements
In contrast to bacteria, fungi tend to grow in places that are:
More acidic
Have higher osmotic pressure
Are lower in moisture
Are lower in nitrogen
Contain coplex carbohydrates
Unit 3: Mycology
138
Reproduction
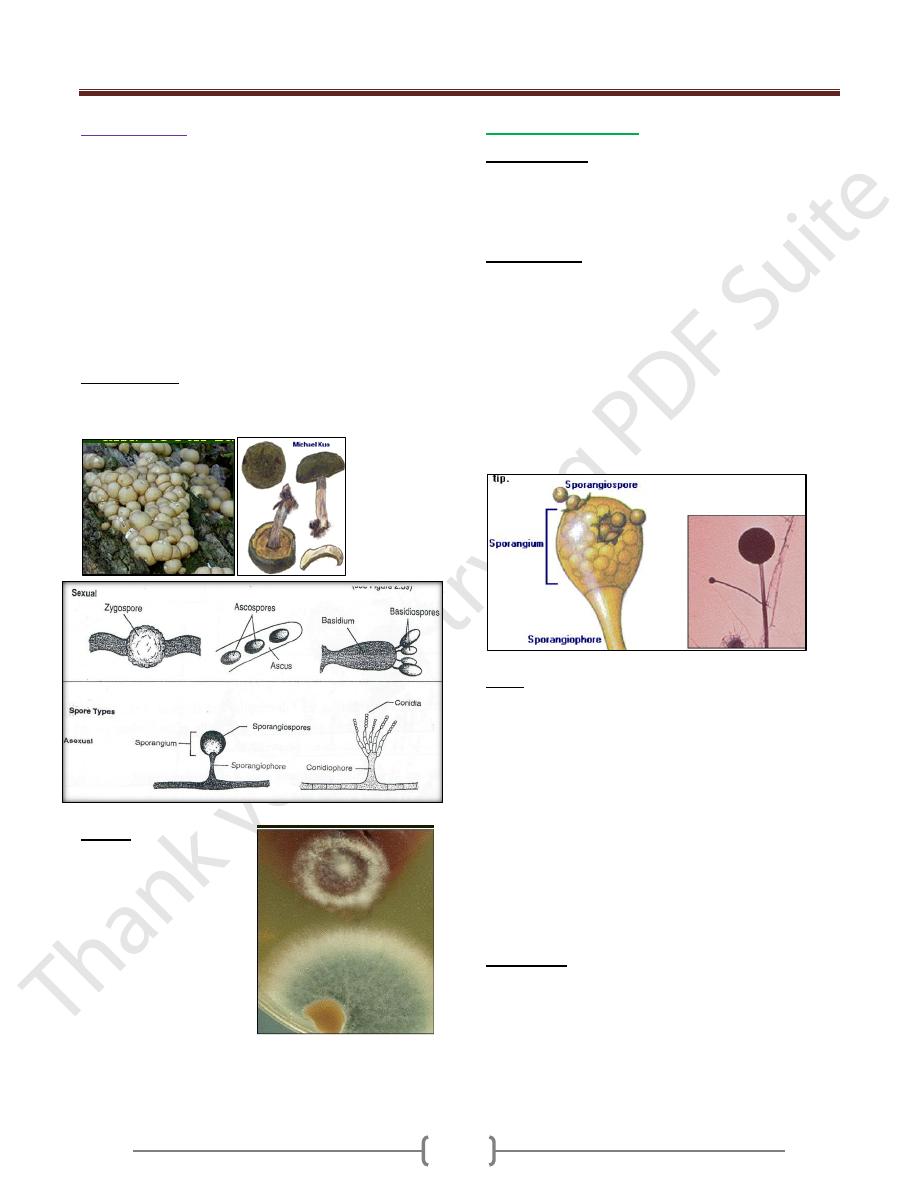
Fungi may reproduce sexually or asexually. Reproductive
elements produced a sexually are termed conidia. Those
produced sexual are termed spores, spores may be either
sexual or a sexual in origin, sexual spores includes
ascospors, Basidiospores or Zygospores. Sexual
reproduction occurs by the fusion of two haploid nuclei
followed by meiotic division of diploid nucleus. Asexual
spores are produced in sac like cell called sporangia and
called sporangiospores. Asexual reproduction results from
division of nuclei by mitosis. Fungi that do not form
sexual spores called Fungi imperfecti.
Basidiomycetes
Basidiospore. Examples: boletes, puffballs, smuts,
stinkhorns & tooth fungi
.
Culture
In vitro, culture at room
temperature with low pH
& minimal nutrients,
supports the growth of
environmental (mycelial)
phase. Incubation at body
temperature with media
supplemented with blood
& amino acids supports
the growth of the body
(yeast) phase of dimorphic fungi.
Yeast & other filamentous fungi may grow in either
condition
Asexual reproduction
Conidial fungus
Reproduces by means of asexual spores called conidia
Conidia vary greatly in shape, size & color
Most of the common household molds & mildews are
conidial fungi
Asexual spores
Conidiaspore
o Multiple (chains) or single spores formed at the end of
an aerial hypha
o Not enclosed within a sac
o Aspergillus spp.
o Penicillium spp.
Sporangiospores (sporulation)
o Hundreds formed within a sac (sporangium) at the end
of an aerial hypha (hyphal tip)
o Rhizopus spp.
Entry
Fungi infect the body through several portals of entry.
The first exposure to fungi that most humans experience
occurs during birth, when Candida albicans encounter
while passing through the vaginal canal. During this
process the fungus colonizes the buccal cavity and
portions of upper and lower gastrointestinal tract of
newborn and maintains a lifelong as a commensal. Other
fungi, malassezia furfur is common in areas of skin in
sebaceous glands. The mechanism of disease with these
two fungi is called endogenous both M. furfur and C.
albicans are considered part of normal flora. Other fungi
that have implicated in human diseases come from
exognous sources, where exist as saprophytes.
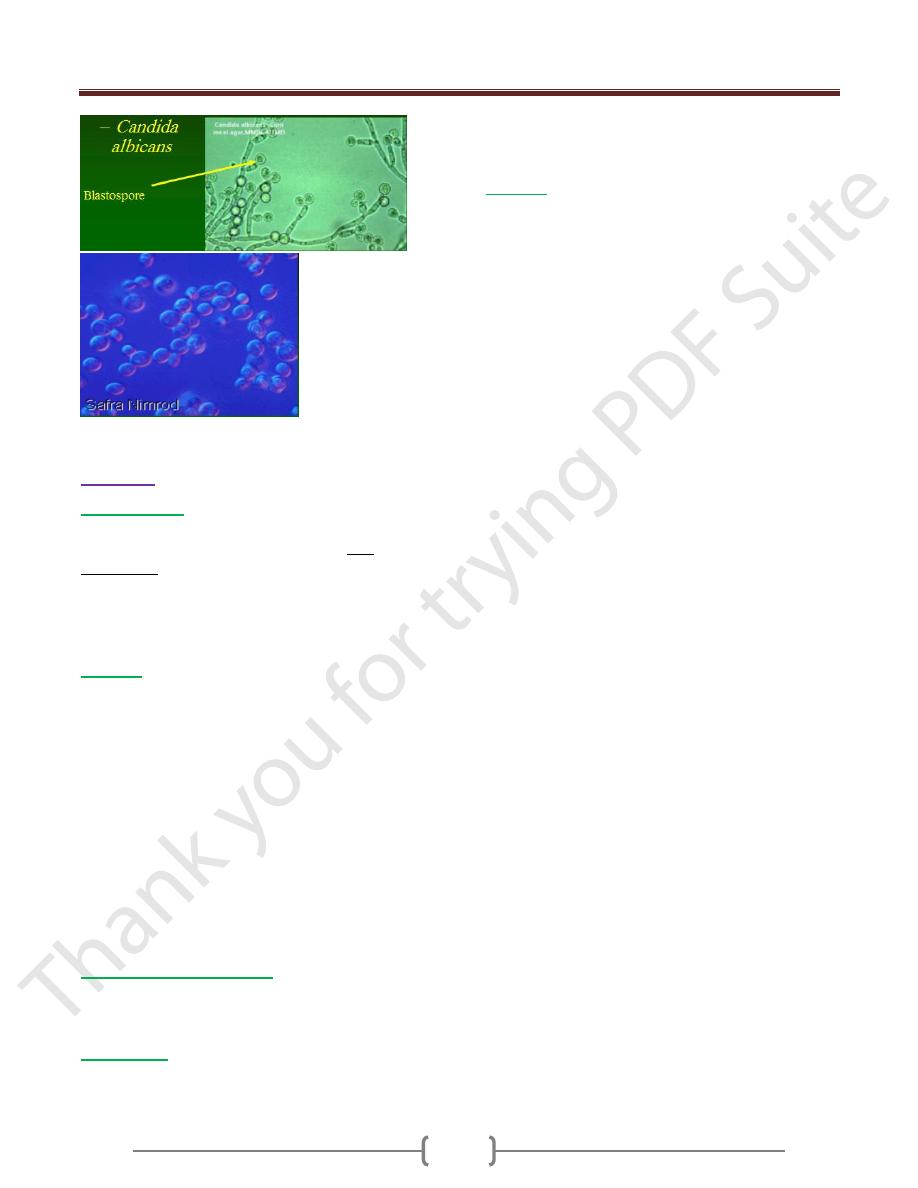
Blastospores:
Another type of conidiophore
A bud coming off the parent cell
Candida albicans
Unit 3: Mycology
139
Diagnosis
Skin scrapings
Suspected to contain dermatophytes or pus from lesion
can be mounted in 10-20 % KOH on a slide (wet
preparation) to dissolve tissue materials leaving the
fungus intact or stained with special fungal stains and
examined directly under the microscope.
Skin test is used be popular as a diagnostic tool, but this is
now discouraged.
Serology
May be helpful when it is applied to a specific, these tests
for the presence of antibodies in the patient’s serum or
CSF which are useful in diagnosing systemic mycosis.
The most common serological test for fungi based on
double immunodiffusion, complement fixation. The
complement fixation test is most frequently used in
suspected cases of Coccidioidomycosis, Histoplasmosis .
If Cryptococcal meningitis, the presence of the
polysaccharide capsular antigen of C.neoformas in CSF
can be detected by Latex Agglutination text.
Direct fluorescence microscopy may be used for fungal
identification, calcofluor white is a fluorescent dye that
binds to fungal wall and useful for identification of fungi
in tissue specimen or cultures.
Biopsy and histopathology:
A biopsy may be very useful for the identification of
tissue invading fungi. Gomori methenamine silver, H&E
stain or Geimsa stains can used.
DNA probe:
This test is rapid (2 hours) and species – specific. Can
identify colonies growing in culture at earlier stage of
growing than can based on visual detection of colonies
DNA probe are available for Coccidioidomycosis,
blastomycosis, Histoplasmosis and cryptococcosis
Culture:
A definite diagnosis requires a culture. Pathogenic fungi
are usually grown on Sabouraud dextrose agar it has a
slightly acidic pH (5.6).
Cycloheximide, penicillin or other inhibitory substances
are often added to prevent bacterial overgrowth. Two
cultures are inoculated and incubated at 25 degree C and
37 degree C to reveal dimorphism, the cultures examined
macroscopically and microscopically, the appearance of
the mycelium and the nature of a sexual spore are
sufficient for identify of the organism.
.
