
Basic Anatomy
585
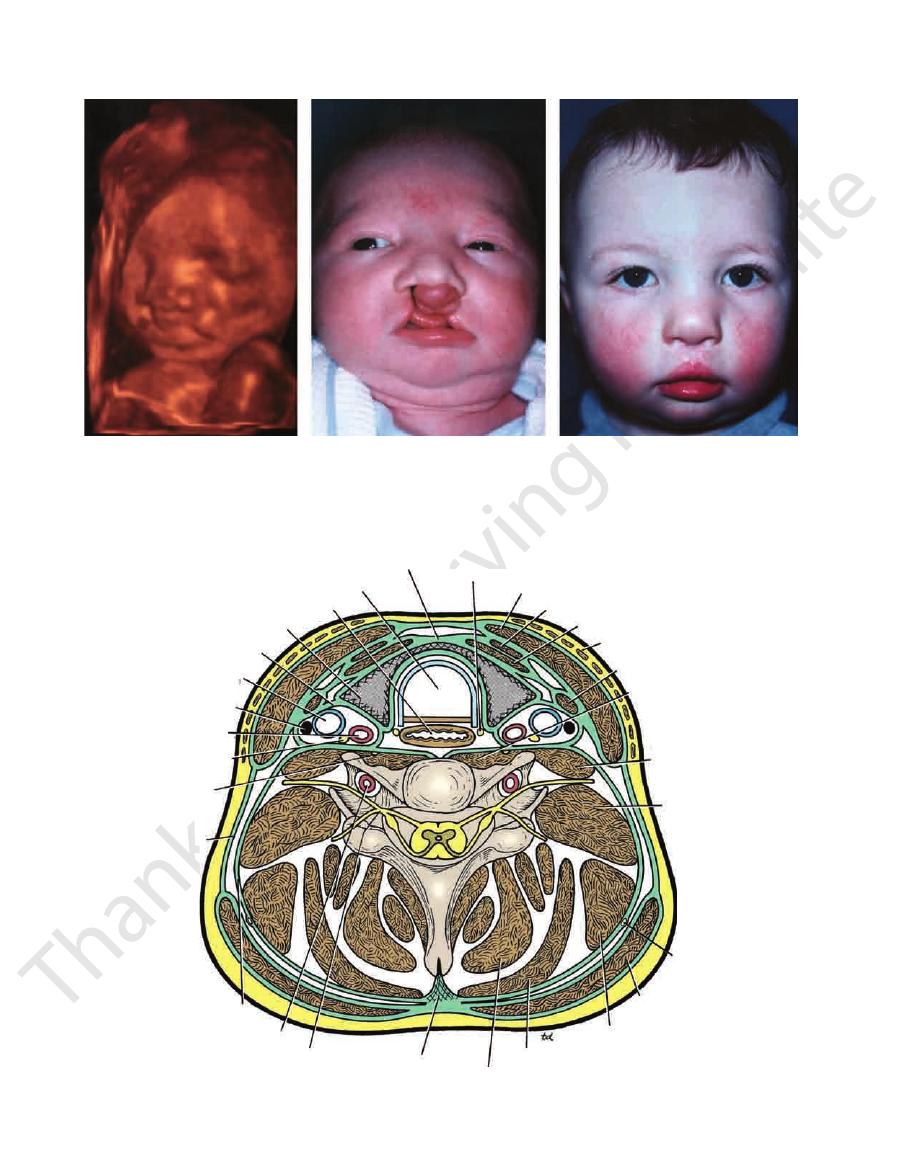
unilateral cleft lip
bilateral cleft lip
median cleft upper lip
median cleft lower lip
oblique facial cleft
FIGURE 11.44
Various forms of cleft lip.
FIGURE 11.45
Unilateral cleft upper lip. (Courtesy of
R. Chase.)
FIGURE 11.46
Bilateral cleft upper lip and palate. (Courtesy
of R. Chase.)
FIGURE 11.47
Right-sided oblique facial cleft and left-sided
cleft upper lip. There also is total bilateral cleft palate.
(Courtesy of R. Chase.)
clinically because an incision along a cleavage line will heal
run almost horizontally around the neck. This is important
The natural lines of cleavage of the skin are constant and
the deep cervical lymph nodes (Fig. 11.49).
carotid arteries, internal jugular veins, the vagus nerve, and
At the sides of these structures are the vertically running
of the alimentary system, the pharynx and the esophagus.
namely, the larynx and the trachea, and behind are parts
tral region of the neck are parts of the respiratory system,
a smaller group of flexor muscles (Fig. 11.49). In the cen
the vertebrae is a mass of extensor muscles and in front is
which is convex forward and supports the skull. Behind
strengthened by the cervical part of the vertebral column,
nal notch and the upper border of the clavicle below. It is
lower margin of the mandible above and the supraster
The neck is the region of the body that lies between the
The Neck
-
-
Skin of the Neck
586
CHAPTER 11
The Head and Neck
A
B
C
FIGURE 11.48
Cleft lip and palate.
351;8:769.)
of age, after synchronous nasolabial repair and palatal closure performed at a second stage. (Courtesy of Dr. J. B. Mulliken.
Shows the same child at 18 months
An infant with bilateral complete cleft lip and palate.
(Courtesy of Dr. B. Benacerraf.)
A three-dimensional ultrasonograph reveals bilateral cleft lip at 22 weeks of gestation.
A.
B.
C.
N Engl J Med
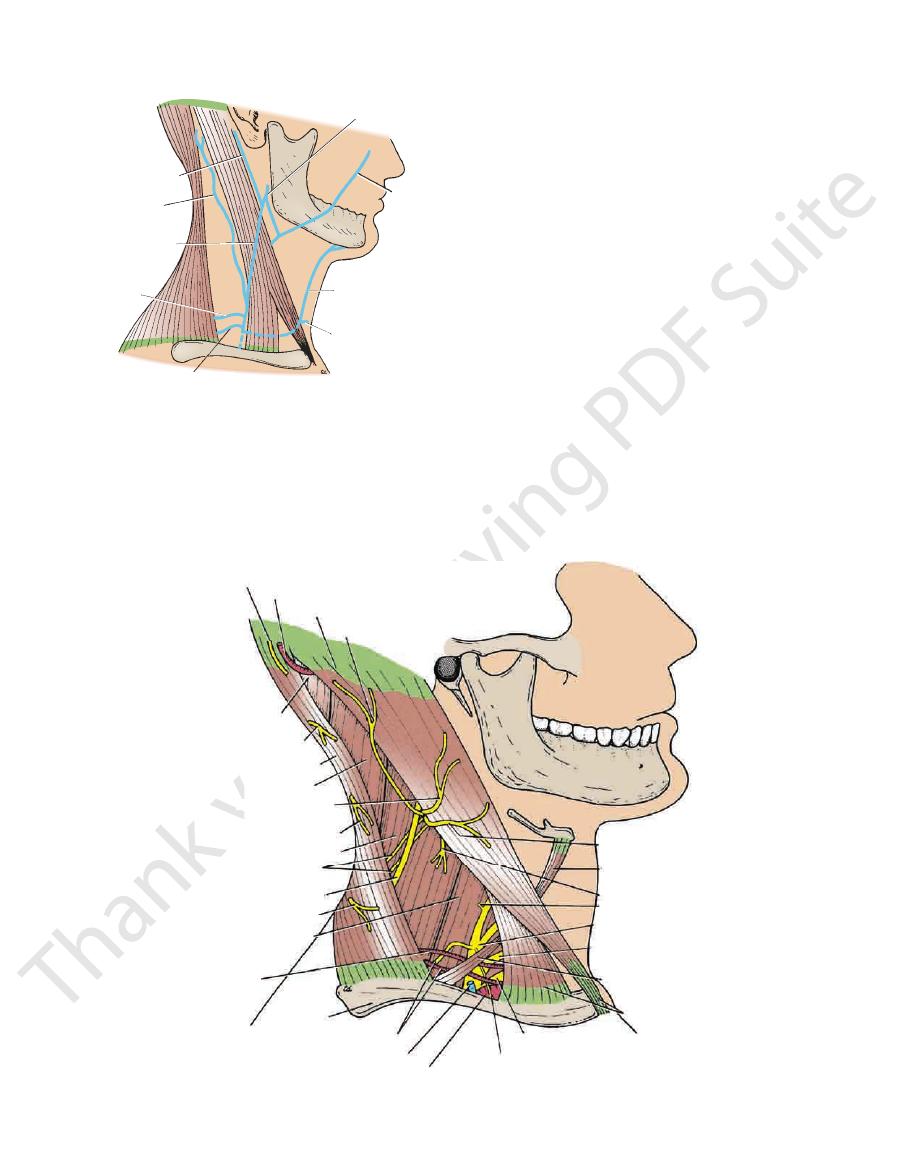
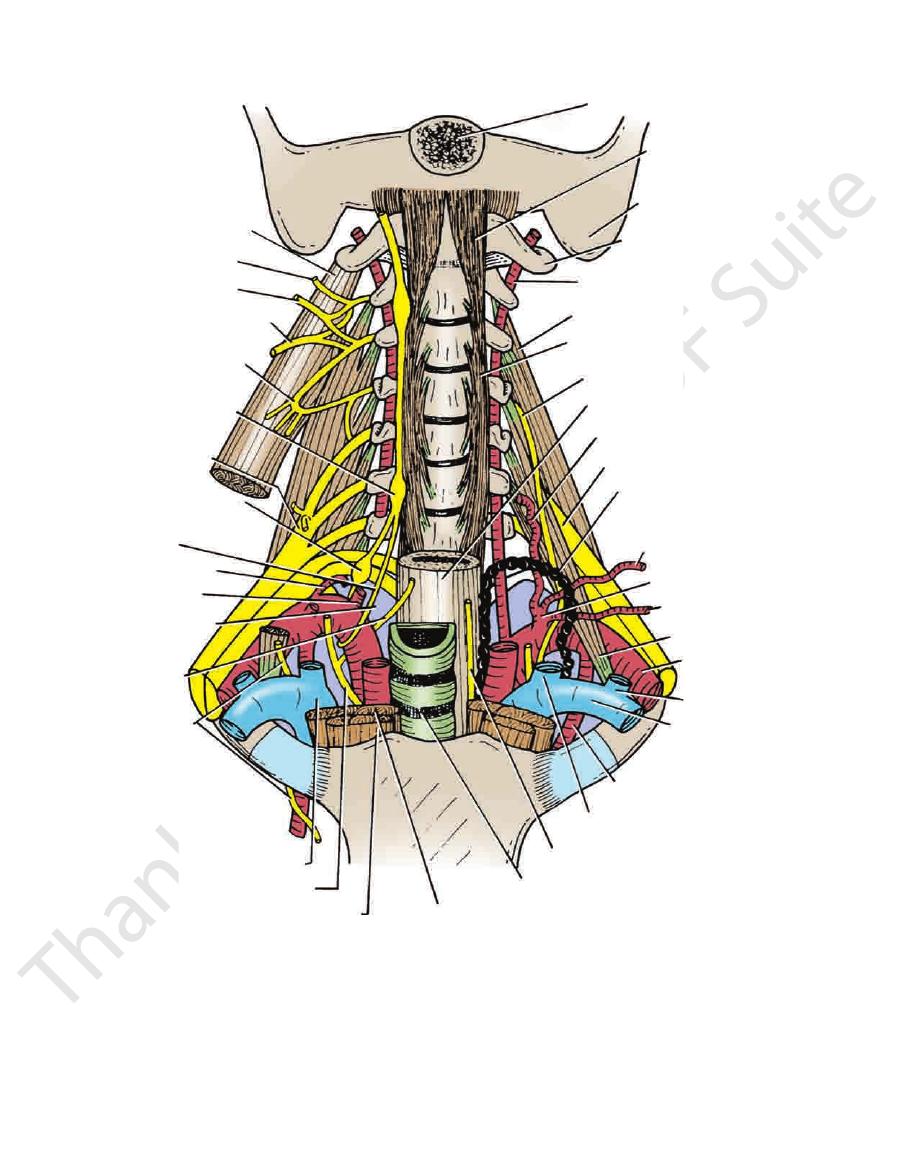
pretracheal fascia
trachea
esophagus
thyroid gland
carotid sheath
internal
jugular vein
deep cervical
lymph node
common
carotid artery
vagus nerve
sympathetic
trunk
investing
layer of
fascia
prevertebral
layer of fascia
vertebral artery
spinal nerve
ligamentum nuchae
semispinalis capitis
splenius capitis
levator scapulae muscle
trapezius
spinal
part of
accessory
nerve
scalenus
medius
muscle
scalenus
anterior
muscle
longus cervicis
muscle
omohyoid muscle
platysma
sternothyroid muscle
sternohyoid muscle
sternocleidomastoid muscle
recurrent laryngeal nerve
C6
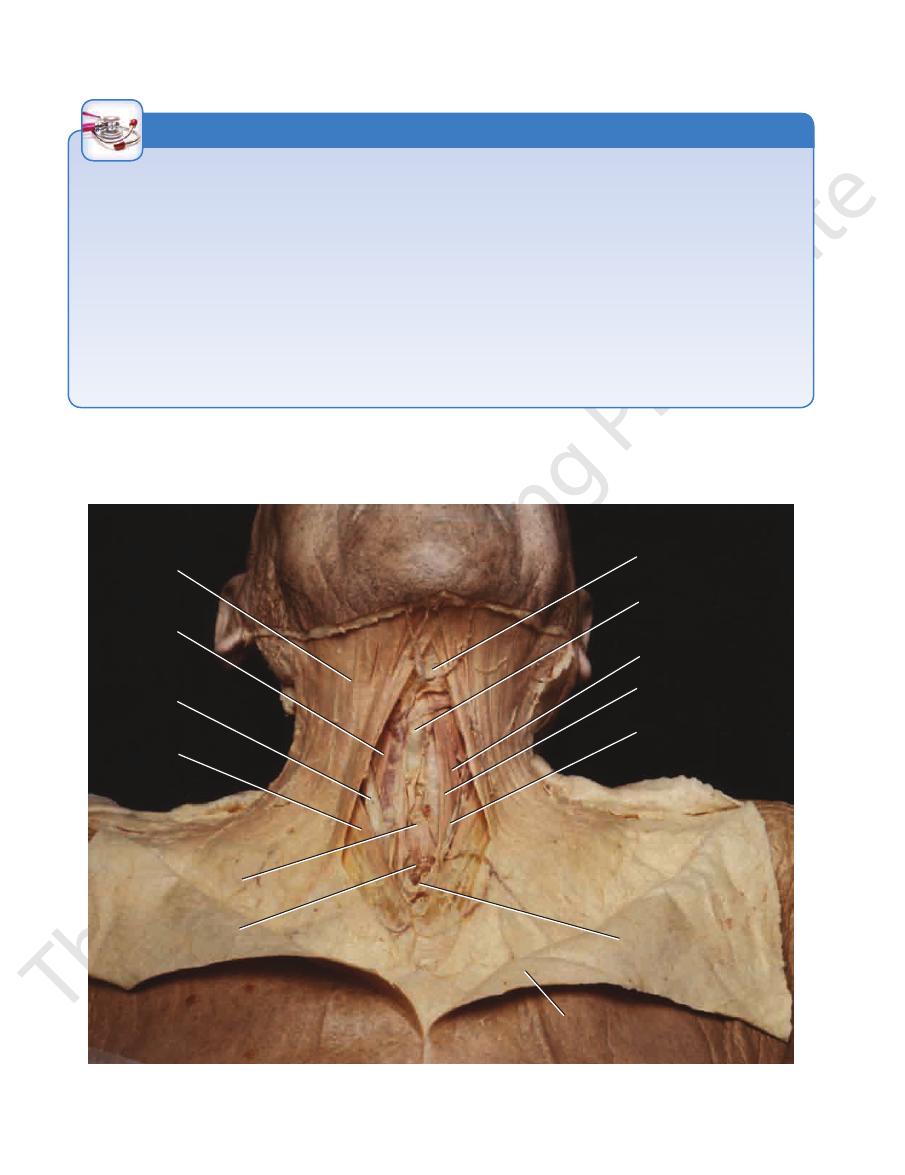
FIGURE 11.49
vical vertebra.
Cross section of the neck at the level of the 6th cer
Basic Anatomy
the posterior border of the sternocleidomastoid muscle
of the cervical plexus. The branches emerge from beneath
by anterior rami of cervical nerves 2 to 4 through branches
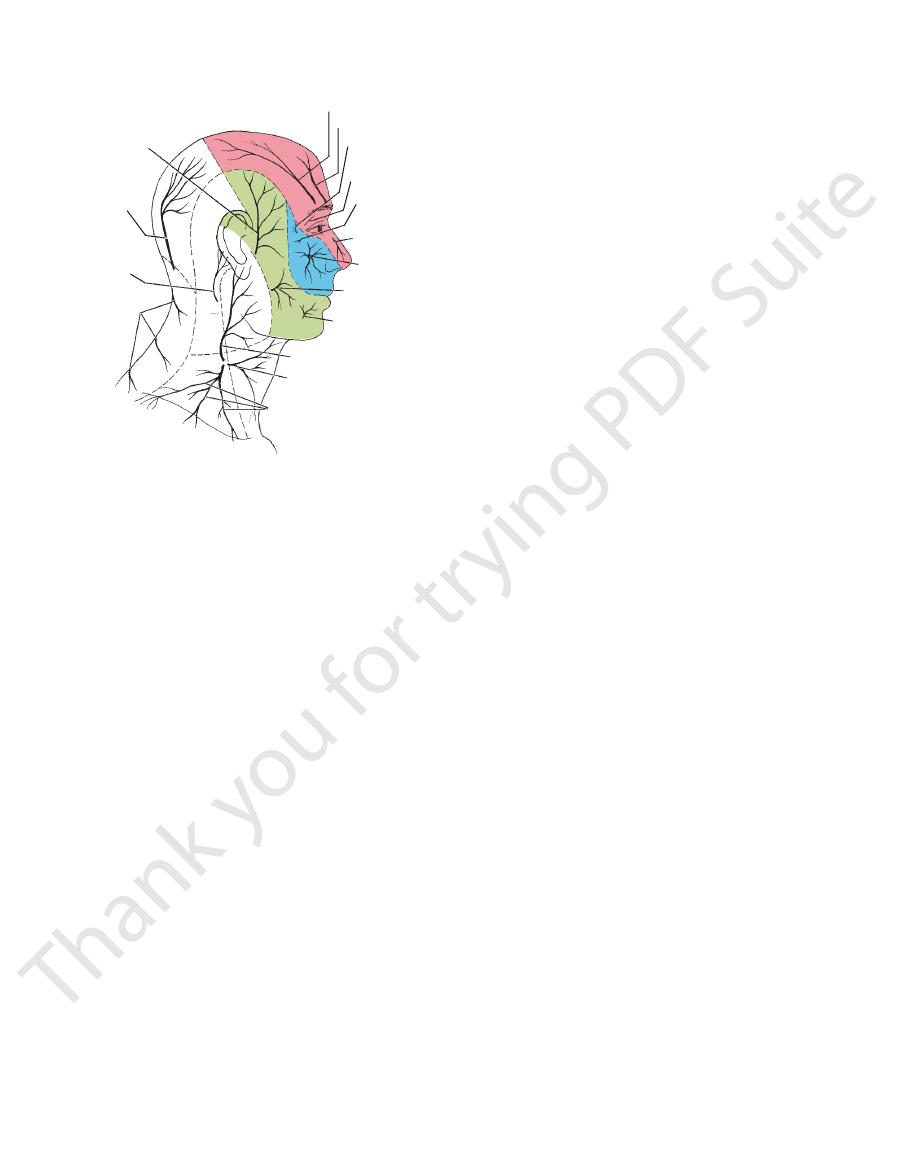
The skin of the front and sides of the neck is supplied
cervical nerve has no cutaneous branch.
of the posterior ramus of the 2nd cervical nerve. The 1st
is a branch
greater occipital nerve
2 to 5 (Fig. 11.50). The
supplied segmentally by posterior rami of cervical nerves
neck and on the back of the scalp as high as the vertex is
The skin overlying the trapezius muscle on the back of the
Cutaneous Nerves
as a wide or heaped-up scar.
as a narrow scar, whereas one that crosses the lines will heal
587
(Fig. 11.50).
sternocleidomastoid muscle. It passes forward across
from behind the middle of the posterior border of the
(C2 and 3) emerges
transverse cutaneous nerve
The
cle (Fig. 11.50).
dible, the parotid gland, and on both surfaces of the auri
branches that supply the skin over the angle of the man
across the sternocleidomastoid muscle and divides into
(C2 and 3) ascends
great auricular nerve
The
the auricle (Fig. 11.50).
eral part of the occipital region and the medial surface of
sternocleidomastoid muscle to supply the skin over the lat
sory nerve and ascends along the posterior border of the
(C2) hooks around the acces
lesser occipital nerve
The
-
-
-
-
that muscle and divides into branches that
supply
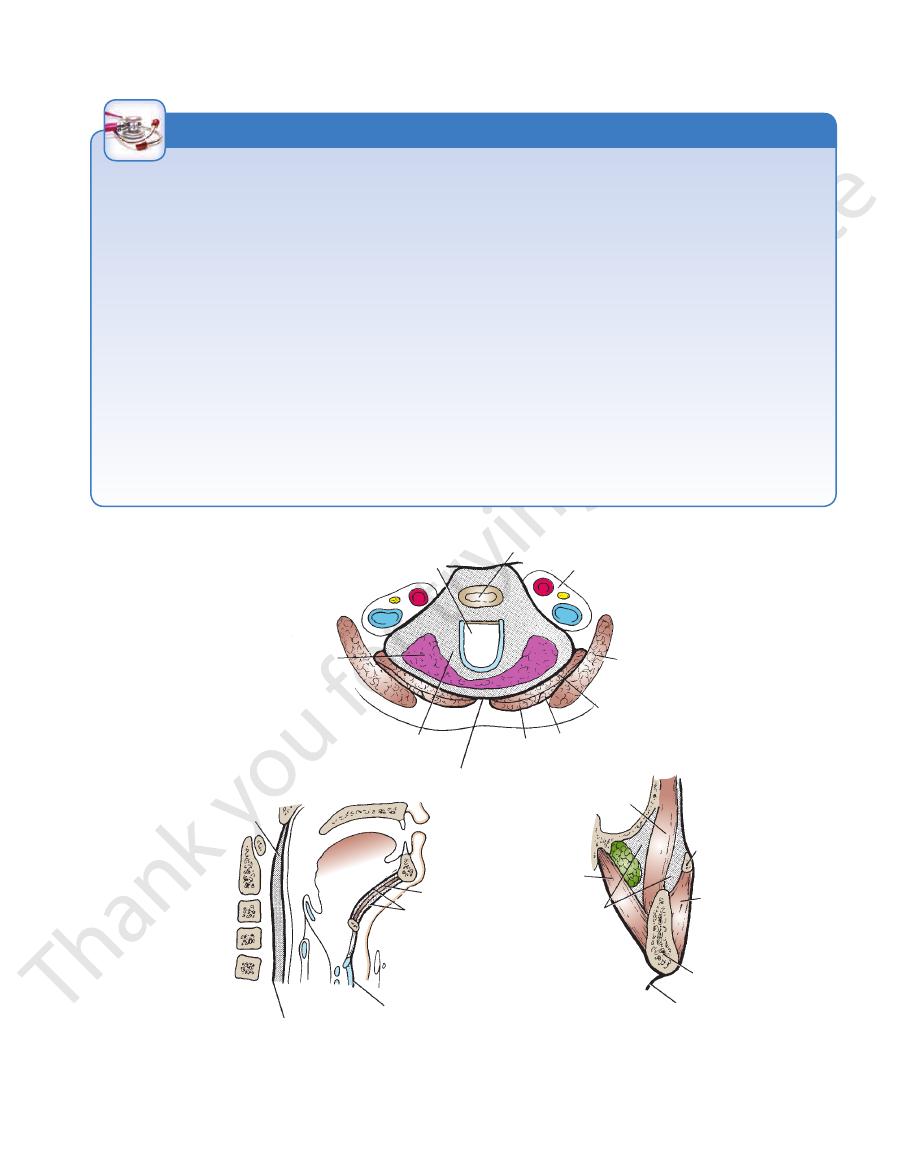
greater
occipital
nerve
(C2)
lesser
occipital
nerve
posterior
rami of
C3, 4,
and 5
supraclavicular nerves
(C3 and 4)
transverse cutaneous nerve
of neck (C2 and 3)
great auricular nerve
(C2 and 3)
mental nerve
buccal nerve
infraorbital nerve
external nasal
nerve
zygomaticofacial
nerve
lacrimal nerve
supratrochlear nerve
zygomaticotemporal
nerve
supraorbital nerve
V2
V3
auriculotemporal
nerve
V1
FIGURE 11.50
Sensory nerve supply to skin of the head
neck, from the body of the mandible to the sternum
the skin on the anterior and lateral surfaces of the
branches of the trigeminal nerve.
supplied by the great auricular nerve (C2 and 3) and not by
and neck. Note that the skin over the angle of the jaw is
(Fig. 11.50).
Anterior jugular vein
Suprascapular vein
Transverse cervical vein
external jugular vein about halfway along its course
the posterior part of the scalp and neck and joins the
Posterior external jugular vein, a small vein that drains
Posterior division of the retromandibular vein
Posterior auricular vein
tributaries:
The external jugular vein (Fig. 11.52) has the following
Tributaries
dle of the clavicle.
course extends from the angle of the mandible to the mid
vian vein (Fig. 11.53). It varies considerably in size, and its
triangle, pierces the deep fascia and drains into the subcla
mastoid muscle and, just above the clavicle in the posterior
(Fig. 11.52). It descends obliquely across the sternocleido
with the posterior division of the retromandibular vein
the mandible by the union of the posterior auricular vein
The external jugular vein begins just behind the angle of
External Jugular Vein
Superficial Veins
the superficial fascia. It is described in Table 11.5, page
but clinically important muscular sheet embedded in
The platysma muscle (Figs. 11.38 and 11.51) is a thin
nodes.
tion, the superficial veins, and the superficial lymph
the cutaneous nerves referred to in the previous sec
encloses the platysma muscle. Also embedded in it are
The superficial fascia of the neck forms a thin layer that
spine of the scapula.
the posterior aspect of the shoulder as far down as the
upper half of the deltoid muscle; this nerve also supplies
clavicle and supplies the skin over the shoulder and the
crosses the lateral end of the
eral supraclavicular nerve
clavicle and supplies the skin of the chest wall. The
crosses the middle of the
mediate supraclavicular nerve
inter
supplies the skin as far as the median plane. The
crosses the medial end of the clavicle and
vicular nerve
medial supracla
level of the second rib (Fig. 11.50). The
onto the chest wall and shoulder region, down to the
muscle and descend across the side of the neck. They pass
beneath the posterior border of the sternocleidomastoid
(C3 and 4) emerge from
supraclavicular nerves
The
-
-
lat-
Superficial Fascia
-
Platysma
589.
-
-
-
■
■
■
■
■
■
■
■
■
■
■
■
588
CHAPTER 11
The Head and Neck
Visibility of the External Jugular Vein
the cricoid cartilage and the clavicle. The passage of the catheter
The vein is catheterized about halfway between the level of
one third of the way up the neck. As the patient sits up, the blood
even when they are asked to hold their breath, which impedes the
sue of men. In obese individuals, the vein may be difficult to identify
The external jugular vein is less obvious in children and women
because their subcutaneous tissue tends to be thicker than the tis-
venous return to the right side of the heart and distends the vein.
The superficial veins of the neck tend to be enlarged and
often tortuous in professional singers because of prolonged
periods of raised intrathoracic pressure.
The External Jugular Vein as a Venous Manometer
The external jugular vein serves as a useful venous manometer.
Normally, when the patient is lying at a horizontal angle of 30°,
the level of the blood in the external jugular veins reaches about
level falls until it is no longer visible behind the clavicle.
External Jugular Vein Catheterization
The external jugular vein can be used for catheterization, but the
presence of valves or tortuosity may make the passage of the
catheter difficult. Because the right external jugular vein is in the
most direct line with the superior vena cava, it is the one most
commonly used (Fig. 11.54).
should be performed during inspiration when the valves are open.
C L I N I C A L N O T E S
platysma
hyoid bone
thyroid cartilage
anterior belly
of the omohyoid
sternohyoid
anterior jugular
vein
jugular arch
reflected skin
common
carotid
artery
internal
jugular
vein
sternocleido-
mastoid
isthmus of
thyroid gland
trachea
FIGURE 11.51
sma muscles and the lower ends of the
Dissection of the anterior aspect of the neck showing the platy
sternocleidomastoid muscles on both sides. The skin has been reflected downward.
Basic Anatomy
589
Muscles of the Neck
T A B L E 1 1 . 5
Two muscles acting
Muscle
Origin
Insertion
Nerve Supply
Action
Platysma
Deep fascia over
pectoralis major and
deltoid
Body of mandible and angle
of mouth
Facial nerve cervical
branch
Depresses mandible and
angle of mouth
Sternocleidomastoid
Manubrium sterni and
medial third of clavicle
Mastoid process of
temporal bone and
occipital bone
Spinal part of
accessory nerve
and C2 and 3
together extend head
and flex neck; one
muscle rotates head to
opposite side
Digastric
Posterior belly
Mastoid process of
temporal bone
Intermediate tendon is held
to hyoid by fascial sling
Facial nerve
Depresses mandible or
elevates hyoid bone
Anterior belly
Body of mandible
Nerve to mylohyoid
Stylohyoid
Styloid process
Body of hyoid bone
Facial nerve
Elevates hyoid bone
Mylohyoid
Mylohyoid line of body of
mandible
Body of hyoid bone and
fibrous raphe
Inferior alveolar
nerve
Elevates floor of mouth
and hyoid bone or
depresses mandible
Geniohyoid
Inferior mental spine of
mandible
Body of hyoid bone
1st cervical nerve
Elevates hyoid bone or
depresses mandible
Sternohyoid
Manubrium sterni and
clavicle
Body of hyoid bone
Ansa cervicalis; C1,
2, and 3
Depresses hyoid bone
Sternothyroid
Manubrium sterni
Oblique line on lamina of
thyroid cartilage
Ansa cervicalis; C1,
2, and 3
Depresses larynx
Thyrohyoid
Oblique line on lamina of
thyroid cartilage
Lower border of body of
hyoid bone
1st cervical nerve
Depresses hyoid bone or
elevates larynx
Omohyoid
Inferior belly
Upper margin of scapula
and suprascapular
ligament
Intermediate tendon is held
to clavicle and first rib by
fascial sling
Ansa cervicalis; C1,
2, and 3
Depresses hyoid bone
Superior belly
Lower border of body of
hyoid bone
Transverse processes
Transverse processes
Transverse processes of
Scalenus anterior
3rd, 4th, 5th, and 6th
cervical vertebrae
1st rib
C4, 5, and 6
Elevates 1st rib; laterally
flexes and rotates
cervical part of
vertebral column
Scalenus medius
of upper six cervical
vertebrae
1st rib
Anterior rami of
cervical nerves
Elevates 1st rib; laterally
flexes and rotates
cervical part of
vertebral column
Scalenus posterior
of lower cervical
vertebrae
2nd rib
Anterior rami of
cervical nerves
Elevates 2nd rib; laterally
flexes and rotates
cervical part of
vertebral column
590
CHAPTER 11
oid ligament and to the thyroid cartilage by the thyrohyoid
cornua (Fig. 11.32). It is attached to the skull by the stylohy
shaped and consists of a body and two greater and two lesser
not articulate with any other bones. The hyoid bone is U
of the neck below the mandible and abides the larynx. It does
The hyoid bone is a mobile single bone found in the midline
page 686.
The cervical part of the vertebral column is described on
Cervical Vertebrae
deep cervical lymph nodes.
and mastoid lymph nodes (see page 604) and drain into the
(Fig. 11.40). They receive lymph vessels from the occipital
jugular vein superficial to the sternocleidomastoid muscle
The superficial cervical lymph nodes lie along the external
Superficial Lymph Nodes
drain into the external jugular vein.
ally and passes deep to the sternocleidomastoid muscle to
. The vein then turns sharply later
jugular arch
called the
the veins of the two sides are united by a transverse trunk
The Head and Neck
-
Bones of the Neck
Hyoid Bone
-
posterior auricular
vein
posterior external
jugular vein
external jugular vein
transverse
cervical vein
suprascapular vein
jugular arch
anterior jugular
vein
facial
vein
retromandibular vein
FIGURE 11.52
Major superficial veins of the face and neck.
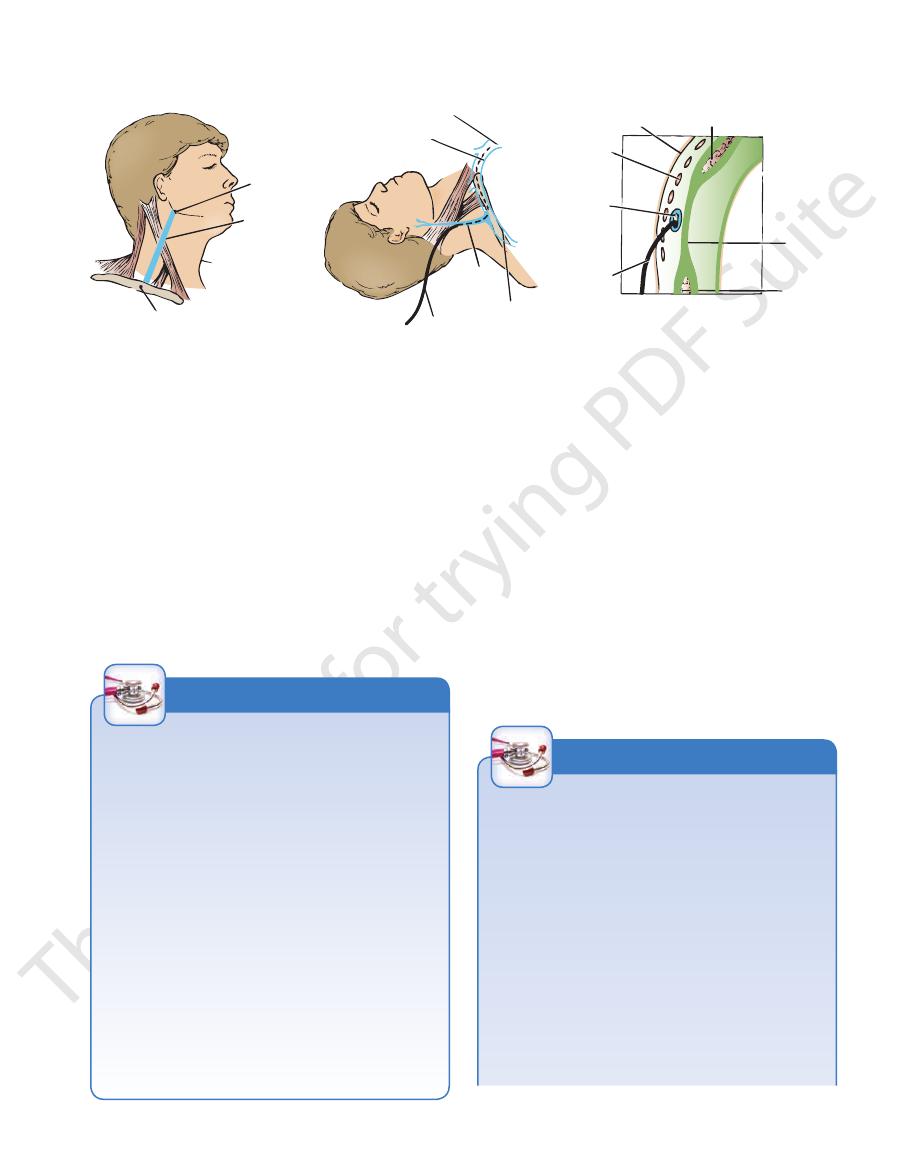
greater occipital nerve
occipital artery
sternocleidomastoid
lesser occipital nerve
semispinalis capitis
posterior ramus C3
trapezius
splenius capitis
great auricular nerve
posterior ramus C4
levator scapulae
C3 and C4
spinal part of accessory nerve
posterior ramus C5
scalenus medius
superficial cervical artery
clavicle
suprascapular nerve and artery
external jugular vein
third part of subclavian artery
nerve to subclavius
lower trunk of brachial plexus
sternocleidomastoid
inferior belly of omohyoid
middle trunk of brachial plexus
upper trunk of brachial plexus
dorsal scapular nerve
supraclavicular nerves
superior belly of omohyoid
transverse cutaneous nerve
FIGURE 11.53
Posterior triangle of the neck.
neck close to the midline. Just above the suprasternal notch,
union of several small veins (Fig. 11.52). It runs down the
The anterior jugular vein begins just below the chin, by the
Anterior Jugular Vein
Basic Anatomy
591
angle of
mandible
external
jugular
vein
midpoint of clavicle
skin
platysma
external
jugular
vein
catheter
trapezius
investing
layer of
deep
cervical
fascia
sternocleidomastoid
muscle
superior vena cava
right brachiocephalic vein
right subclavian
vein
external
jugular
vein
catheter
A
B
C
FIGURE 11.54
Catheterization of the right external jugular vein.
membrane. The hyoid bone forms a base for the tongue and
of the external jugular vein as it crosses the posterior triangle of the neck.
Cross section of the neck showing the relationships
how the external jugular vein joins the subclavian vein at a right angle.
Surface marking of the vein.
A.
B. Site of catheterization. Note
C.
is suspended in position by muscles that
t it to the
connec
muscles are also described in Table 11.5.
infrahyoid muscles and the anterior and lateral vertebral
and 11.51) are described in Table 11.5. The suprahyoid and
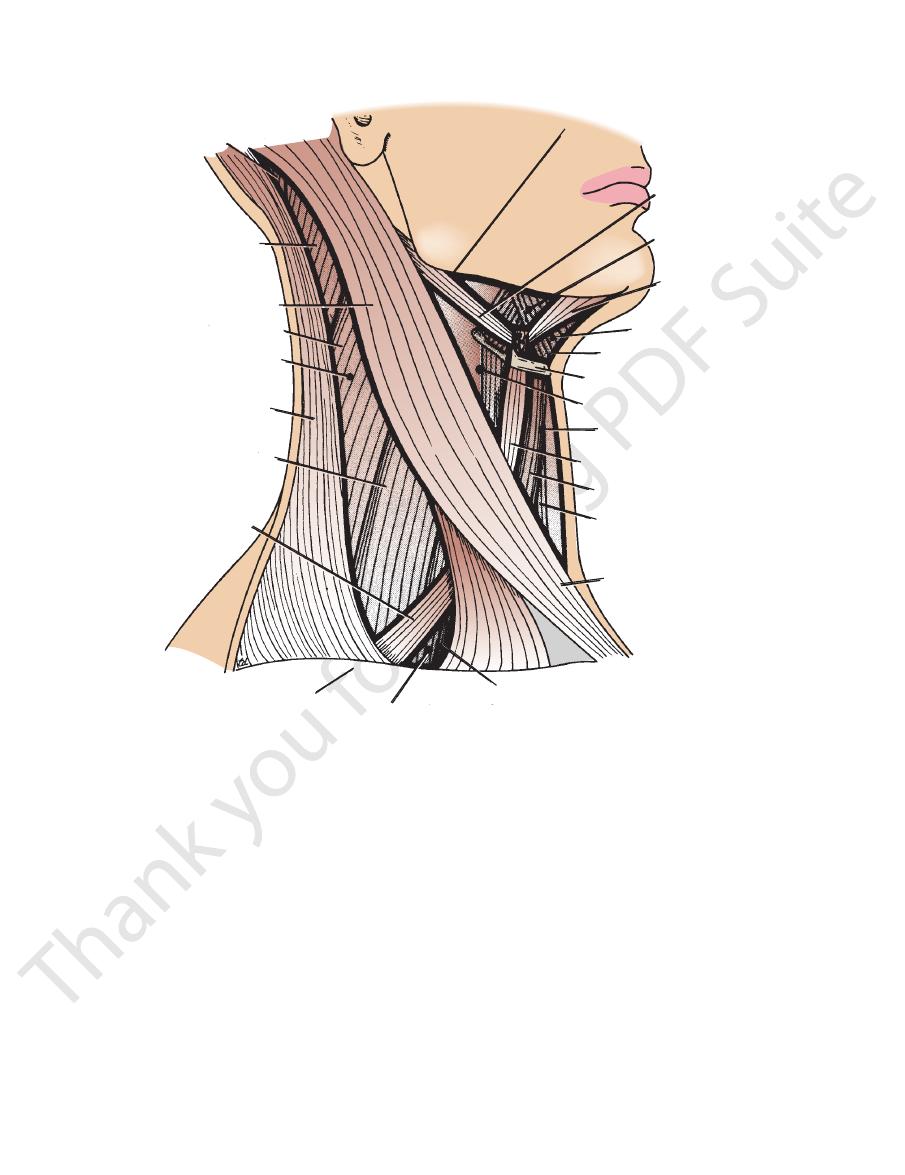
The superficial muscles of the side of the neck (Figs. 11.38
shown in Figure 11.32.
The important muscles attached to the hyoid bone are
thyroid cartilage, to the sternum, and to the scapula.
mandible, to the styloid process of the temporal bone, to the
Muscles of the Neck
fully sutured, since the tone of the platysma can pull on the
In lacerations or surgical incisions in the neck, it is very impor
firmly. The muscle extends from the body of the mandible
Clinical Identification of the Platysma
The platysma can be seen as a thin sheet of muscle just
beneath the skin by having the patient clench his or her jaws
downward over the clavicle onto the anterior chest wall.
Platysma Tone and Neck Incisions
-
tant that the subcutaneous layer with the platysma be care-
scar tissue, resulting in broad, unsightly scars.
Platysma Innervation, Mouth Distortion, and Neck
Incisions
The platysma muscle is innervated by the cervical branch of
the facial nerve. This nerve emerges from the lower end of
the parotid gland and travels forward to the platysma; it then
sometimes crosses the lower border of the mandible to supply
the depressor anguli oris muscle (see page XXX). Skin lacera-
tions over the mandible or upper part of the neck may distort
the shape of the mouth.
C L I N I C A L N O T E S
Key Neck Muscles
sternocleidomastoid muscle are summarized in Table 11.5.
plexus. The origin, insertion, nerve supply, and action of the
nerves, the phrenic nerve, and the upper part of the brachial
of the posterior border is related to the cervical plexus of
sma muscle, and the external jugular vein. The deep surface
The muscle is covered superficially by skin, fascia, the platy
deep cervical lymph nodes; it also overlaps the thyroid gland.
covers the carotid arteries, the internal jugular vein, and the
rior and posterior triangles (Fig. 11.56). The anterior border
mastoid process of the skull. It divides the neck into ante
the side of the neck from the sternoclavicular joint to the
and 11.55) contracts, it appears as an oblique band crossing
When the sternocleidomastoid muscle (Figs. 11.51, 11.53,
Sternocleidomastoid Muscle
-
-
Sternocleidomastoid Muscle and Protection from
and the greater part of the sternocleidomastoid muscles have
with the head and neck fully extended, some individuals have
The sternocleidomastoid, a strong, thick muscle crossing the
Trauma
side of the neck, protects the underlying soft structures from
blunt trauma. Suicide attempts by cutting one’s throat often
fail because the individual first extends the neck before mak-
ing several horizontal cuts with a knife. Extension of the cer-
vical part of the vertebral column and extension of the head
at the atlantooccipital joint cause the carotid sheath with its
contained large blood vessels to slide posteriorly beneath the
sternocleidomastoid muscle. To achieve the desired result
to make several attempts and only succeed when the larynx
been severed. The common sites for the wounds are immedi-
ately above and below the hyoid bone.
C L I N I C A L N O T E S
(continued)
592
CHAPTER 11
The Head and Neck
Congenital Torticollis
medial border is related to the thoracic duct.
the sympathetic trunk (Fig. 11.57). On the left side, the
Related to the vertebral artery and vein and
Medially:
scalenus anterior muscle.
(Fig. 11.57). The scalenus medius muscle lies behind the
chial plexus, and the second part of the subclavian artery
Related to the pleura, the origin of the bra
Posteriorly:
muscle.
of deep cervical fascia bind the phrenic nerve to the
and suprascapular arteries and the prevertebral layer
cal lymph nodes (Fig. 11.49). The transverse cervical
nerve, the internal jugular vein, and the deep cervi
Related to the carotid arteries, the vagus
Anteriorly:
Important Relations
to the 1st rib.
and it descends almost vertically from the vertebral column
standing the root of the neck (Fig. 11.57). It is deeply placed
The scalenus anterior muscle is a key muscle in under
Scalenus Anterior Muscle
upward to the opposite side. If left untreated, asymmetrical
cess is thus pulled down toward the sternoclavicular joint of
Most cases of congenital torticollis are a result of excessive
stretching of the sternocleidomastoid muscle during a dif-
ficult labor. Hemorrhage occurs into the muscle and may be
detected as a small, rounded “tumor” during the early weeks
after birth. Later, this becomes invaded by fibrous tissue,
which contracts and shortens the muscle. The mastoid pro-
the same side, the cervical spine is flexed, and the face looks
growth changes occur in the face, and the cervical vertebrae
may become wedge shaped.
Spasmodic Torticollis
Spasmodic torticollis, which results from repeated chronic
contractions of the sternocleidomastoid and trapezius mus-
cles, is usually psychogenic in origin. Section of the spinal part
of the accessory nerve may be necessary in severe cases.
-
■
■
-
■
■
-
■
■
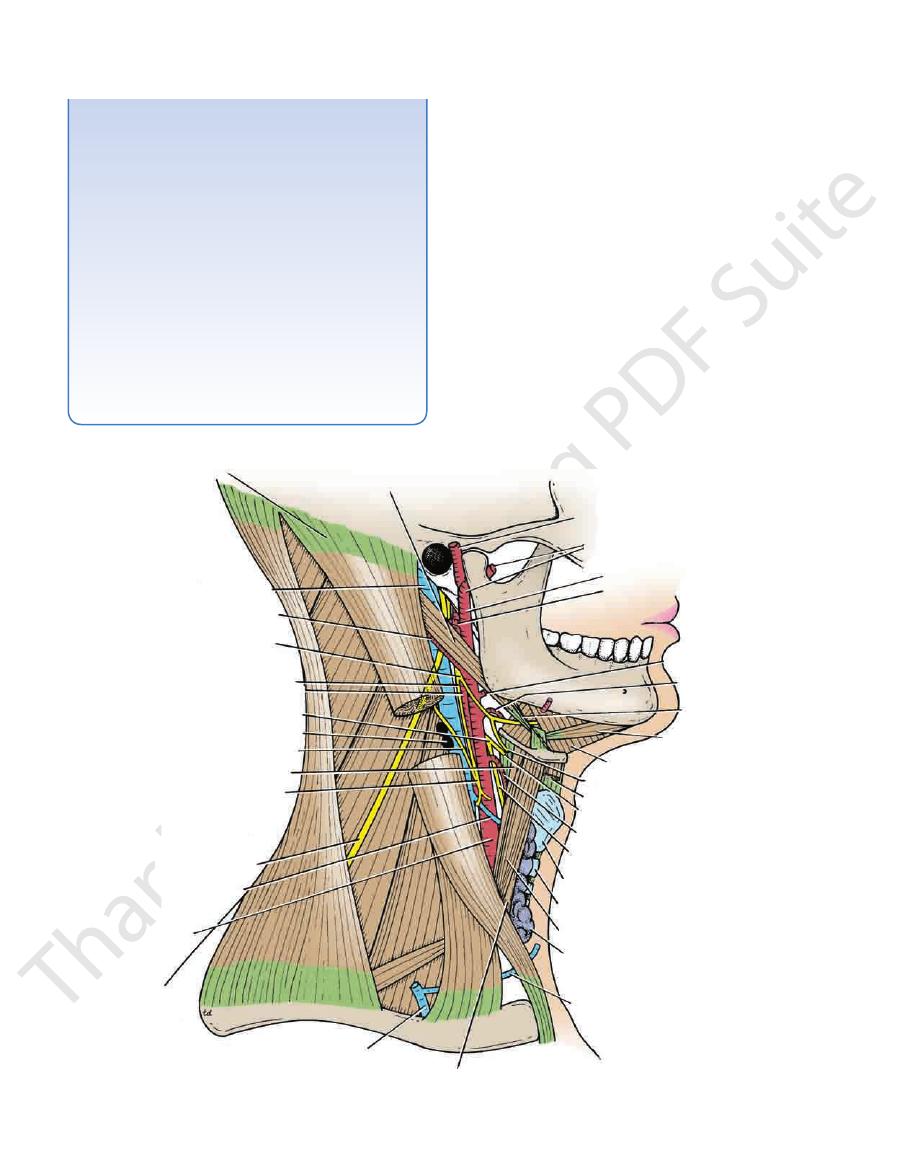
sternocleidomastoid
internal jugular vein
occipital artery
hypoglossal nerve
descending branch
of hypoglossal nerve
internal carotid artery
superior laryngeal nerve
deep cervical lymph nodes
descending cervical nerve
thyrohyoid
ansa cervicalis
spinal part of
accessory nerve
common
carotid
artery
external jugular vein
sternothyroid
anterior jugular vein
isthmus of thyroid gland
superior belly of omohyoid
cricoid cartilage
thyroid cartilage
external laryngeal nerve
superior thyroid artery
internal laryngeal nerve
sternohyoid
nerve to thyrohyoid
mylohyoid
anterior belly
of digastric
stylohyoid
lingual
artery
facial artery
posterior auricular
artery
external carotid artery
maxillary artery
superficial temporal artery
posterior belly of digastric
superior thyroid
vein
FIGURE 11.55
Anterior triangle of the neck.
Basic Anatomy
593
submental triangle
lower margin of body of mandible
of digastric
posterior belly
digastric triangle
of digastric
anterior belly
carotid triangle
muscular triangle
superior belly of omoh
sternoh
sternothyroid
sternocleidomastoid
sternal head of
scalenus anterior
(supraclavicular triangle)
posterior triangle
clavicle
omohyoid
inferior belly of
(occipital triangle)
posterior triangle
levator scapulae
sternocleidomastoid
semispinalis capitis
splenius capitis
trapezius
scalenus medius
yoid
yoid
hyoid bone
mylohyoid
FIGURE 11.56
Muscular triangles of the neck.
agus and in front of the prevertebral muscles and the
tum across the neck behind the pharynx and the esoph
The prevertebral layer is a thick layer that passes like a sep
Prevertebral Layer
and encloses the infrahyoid muscles.
roid and the parathyroid glands, forming a sheath for them,
to the laryngeal cartilages (Fig. 11.49). It surrounds the thy
The pretracheal layer is a thin layer that is attached above
Pretracheal Layer
muscles (Fig. 11.49).
splits to enclose the trapezius and the sternocleidomastoid
The investing layer is a thick layer that encircles the neck. It
Investing Layer
It is also condensed to form the carotid sheath (Fig. 11.49).
prevertebral layer.
pretracheal layer,
ing layer,
invest
densed to form well-defined, fibrous sheets called the
the viscera of the neck (Fig. 11.49). In certain areas, it is con
The deep cervical fascia supports the muscles, the vessels, and
nus anterior muscle are summarized in Table 11.5.
The origin, insertion, nerve supply, and action of the scale
part of the subclavian artery (Fig. 11.57).
cal plexus, the roots of the brachial plexus, and the third
Related to the emerging branches of the cervi
Laterally:
■
■
-
-
Deep Cervical Fascia
-
-
the
and the
-
-
-
vertebral column (Fig. 11.49). It forms the fascial floor of
bral, the pretracheal, and the investing layers of the deep
The carotid sheath is a local condensation of the preverte
Carotid Sheath
(see page 596).
axillary sheath
rib into the axilla to form the important
the posterior triangle, and it extends laterally over the first
-
594
CHAPTER 11
The Head and Neck
levator scapulae
lesser occipital nerve
great auricular nerve
transverse cutaneous nerve
supraclavicular nerves
middle cervical
sympathetic ganglion
upper trunk of
brachial plexus
inferior cervical
sympathetic ganglion
ansa subclavia
costocervical trunk
vertebral artery
cervical pleura
right recurrent
laryngeal nerve
phrenic nerve
right brachiocephalic vein
vagus
sternohyoid
sternothyroid
trachea
left recurrent laryngeal nerve
internal jugular vein
internal thoracic artery
subclavian vein
external jugular vein
third part of
subclavian artery
scalenus anterior
suprascapular artery
thyrocervical trunk
superficial cervical artery
thoracic duct
upper trunk of brachial plexus
inferior thyroid artery
esophagus
phrenic nerve
longus cervicis
scalenus medius
vertebral artery
transverse process of atlas
mastoid process
longus capitis
basilar part of occipital bone
2
3
4
5
6
7
FIGURE 11.57
Prevertebral region and the root of the neck.
Basic Anatomy
595
Clinical Significance of the Deep Fascia of the Neck
abscess but must not forget the existence of the deeply placed
Later, this becomes eroded at one point, and the pus passes into
ward and upward. Further spread downward may involve the
most commonly involve the lower molar teeth.
Dental infections
and the tough fascia can determine the direction of spread of
esophagus can spread among the fascial planes and spaces,
ically important. Among the more important spaces are the vis
As previously described, the deep fascia in certain areas forms
distinct sheets called the investing, pretracheal, and preverte-
bral layers. These fascial layers are easily recognizable to the
surgeon at operation.
Fascial Spaces
Between the more dense layers of deep fascia in the neck is
loose connective tissue that forms potential spaces that are clin-
-
ceral, retropharyngeal, submandibular, and masticatory spaces
(Fig. 11.58).
The deep fascia and the fascial spaces are important
because organisms originating in the mouth, teeth, pharynx, and
infection and the path taken by pus. It is possible for blood, pus,
or air in the retropharyngeal space to spread downward into the
superior mediastinum of the thorax.
Acute Infections of the Fascial Spaces of the Neck
The infection spreads medially from the mandible into the sub-
mandibular and masticatory spaces and pushes the tongue for-
visceral space and lead to edema of the vocal cords and airway
obstruction.
Ludwig’s angina is an acute infection of the submandibular
fascial space and is commonly secondary to dental infection.
Chronic Infection of the Fascial Spaces of the Neck
Tuberculous infection of the deep cervical lymph nodes can
result in liquefaction and destruction of one or more of the nodes.
The pus is at first limited by the investing layer of the deep fascia.
the less restricted superficial fascia. A dumbbell or collar-stud
abscess is now present. The clinician is aware of the superficial
abscess.
C L I N I C A L N O T E S
trachea
thyroid gland
visceral space
pretracheal layer of
deep cervical fascia
sternohyoid
muscle
superior belly of omohyoid muscle
sternothyroid
sternocleidomastoid
muscle
carotid sheath
esophagus
retropharyngeal space
prevertebral layer of
deep cervical fascia
pretracheal layer
of deep cervical fascia
submandibular
space
mylohyoid muscle
medial
pterygoid
muscle
masticatory
space
investing layer of
deep cervical fascia
mandible
masseter muscle
zygomatic arch
A
B
C
temporalis
FIGURE 11.58
A.
the masticatory space.
Vertical section of the body of the mandible close to the angle showing
of the retropharyngeal and submandibular spaces.
Sagittal section of the neck showing the positions
Cross section of the neck showing the visceral space. B.
C.
596
CHAPTER 11
(Figs. 11.55 and 11.60).
divides into the external and internal carotid arteries
to the upper border of the thyroid cartilage. Here, it
nocleidomastoid muscle, from the sternoclavicular joint
the neck under cover of the anterior border of the ster
95). The common carotid artery runs upward through
arch of the aorta in the superior mediastinum (see page
(Figs. 11.57 and 11.59). The left artery arises from the
ocephalic artery behind the right sternoclavicular joint
The right common carotid artery arises from the brachi
Common Carotid Artery
and lateral vertebral muscles are described in Table 11.5.
The suprahyoid and infrahyoid muscles and the anterior
below (Fig. 11.56).
supraclavicular triangle
and a small
above
occipital triangle
into a large
of the omohyoid muscle
inferior belly
angle of the neck is further subdivided by the
and inferiorly by the clavicle (Fig. 11.56). The posterior tri
zius muscle, anteriorly by the sternocleidomastoid muscle,
The posterior triangle is bounded posteriorly by the trape
Posterior Triangle
(Fig. 11.56).
muscular triangle
submental triangle,
the
digastric triangle,
carotid triangle,
divided into the
and anteriorly by the midline (Fig. 11.56). It is further sub
mandible, posteriorly by the sternocleidomastoid muscle,
The anterior triangle is bounded above by the body of the
Anterior Triangle
anterior and the posterior triangles (Fig. 11.56).
The sternocleidomastoid muscle divides the neck into the
Muscular Triangles of the Neck
(Fig. 11.80).
to the superior constrictor and the buccinator muscles
the mylohyoid line of the mandible. It gives attachment
cess of the medial pterygoid plate to the posterior end of
Connects the hamular pro
Pterygomandibular ligament:
sphenoid bone to the lingula of the mandible (Fig. 11.33)
Connects the spine of the
Sphenomandibular ligament:
to the angle of the mandible (Fig. 11.33)
Connects the styloid process
Stylomandibular ligament:
lesser cornu of the hyoid bone (Fig. 11.80)
Connects the styloid process to the
Stylohyoid ligament:
Cervical Ligaments
axillary sheath.
extends into the axilla and is called the
muscles, they carry with them a sheath of the fascia, which
val between the scalenus anterior and the scalenus medius
clavian artery and the brachial plexus emerge in the inter
muscles lie at first deep to the prevertebral fascia. As the sub
interval between the scalenus anterior and scalenus medius
All the anterior rami of the cervical nerves that emerge in the
deep cervical lymph nodes (Fig. 11.49).
arteries, the internal jugular vein, the vagus nerve, and the
fascia that surround the common and internal carotid
The Head and Neck
Axillary Sheath
-
-
-
-
the
and the
-
-
Arteries of the Head and Neck
-
-
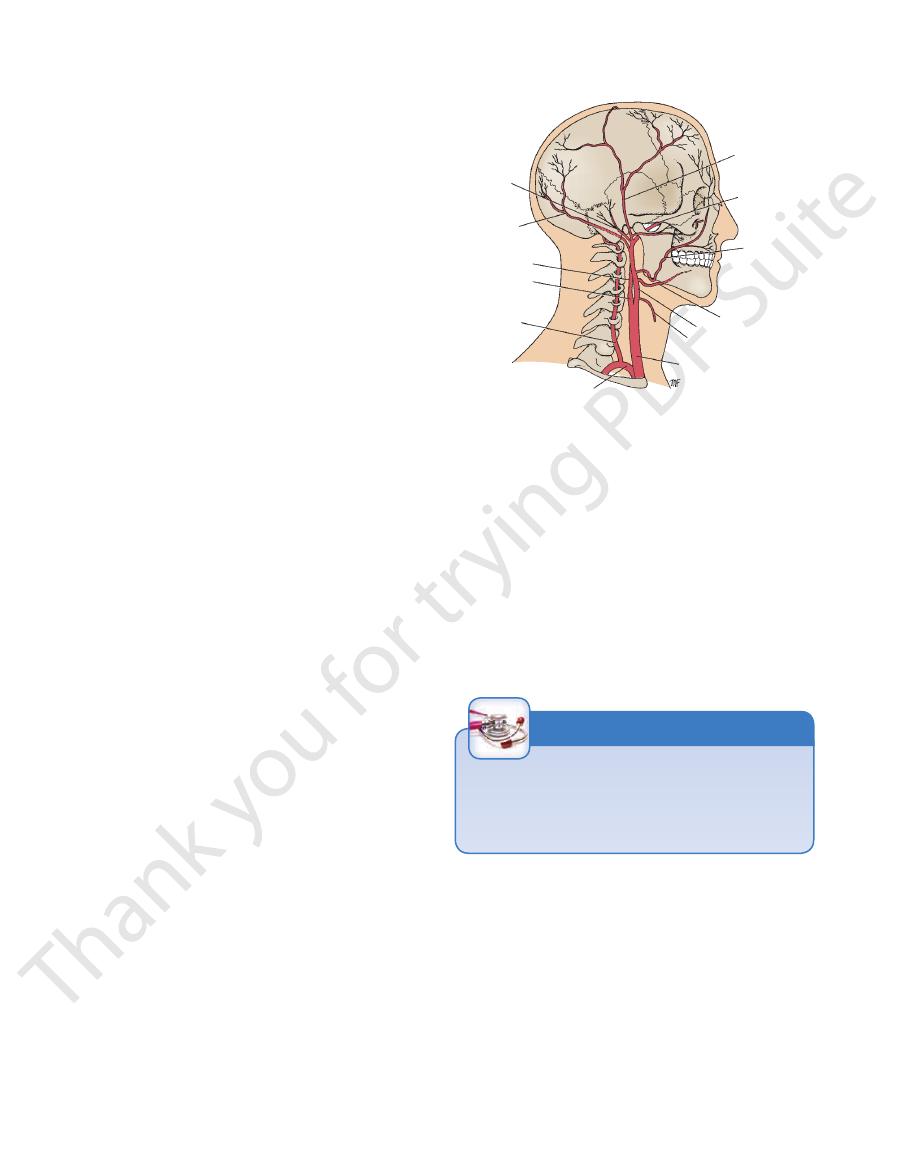
posterior
auricular
artery
occipital artery
internal
carotid artery
carotid sinus
vertebral
artery
subclavian artery
common carotid artery
superior thyroid artery
lingual artery
facial
artery
maxillary
artery
superficial
temporal
artery
external carotid artery
y
FIGURE 11.59
Main arteries of the head and neck. Note that
the heart rate and vasodilatation of the arterioles.
tor mechanism: A rise in blood pressure causes a slowing of
geal nerve. The carotid sinus serves as a reflex pressorecep
numerous nerve endings derived from the glossopharyn
elsewhere, but the adventitia is relatively thick and contains
(Fig. 11.60). The tunica media of the sinus is thinner than
carotid sinus
artery shows a localized dilatation, called the
carotid artery or the beginning of the internal carotid
At its point of division, the terminal part of the common
Carotid Sinus
artery—are not shown.
and the internal thoracic artery—branches of the subclavian
for clarity the thyrocervical trunk, the costocervical trunk,
-
-
rate, a fall in blood pressure, and cerebral ischemia with fainting.
both carotid sinuses can cause excessive slowing of the heart
In cases of carotid sinus hypersensitivity, pressure on one or
Carotid Sinus Hypersensitivity
C L I N I C A L N O T E S
Carotid Body
vagus nerve (Fig. 11.49).
course and is closely related to the internal jugular vein and
tive tissue sheath, called the carotid sheath, throughout its
The common carotid artery is embedded in a connec
tory movements.
blood pressure and heart rate and an increase in respira
in the blood. Such a stimulus reflexly produces a rise in
tive to excess carbon dioxide and reduced oxygen tension
nerve. The carotid body is a chemoreceptor, being sensi
(Fig. 11.60). It is innervated by the glossopharyngeal
to the point of bifurcation of the common carotid artery
The carotid body is a small structure that lies posterior
-
-
-
Basic Anatomy
597
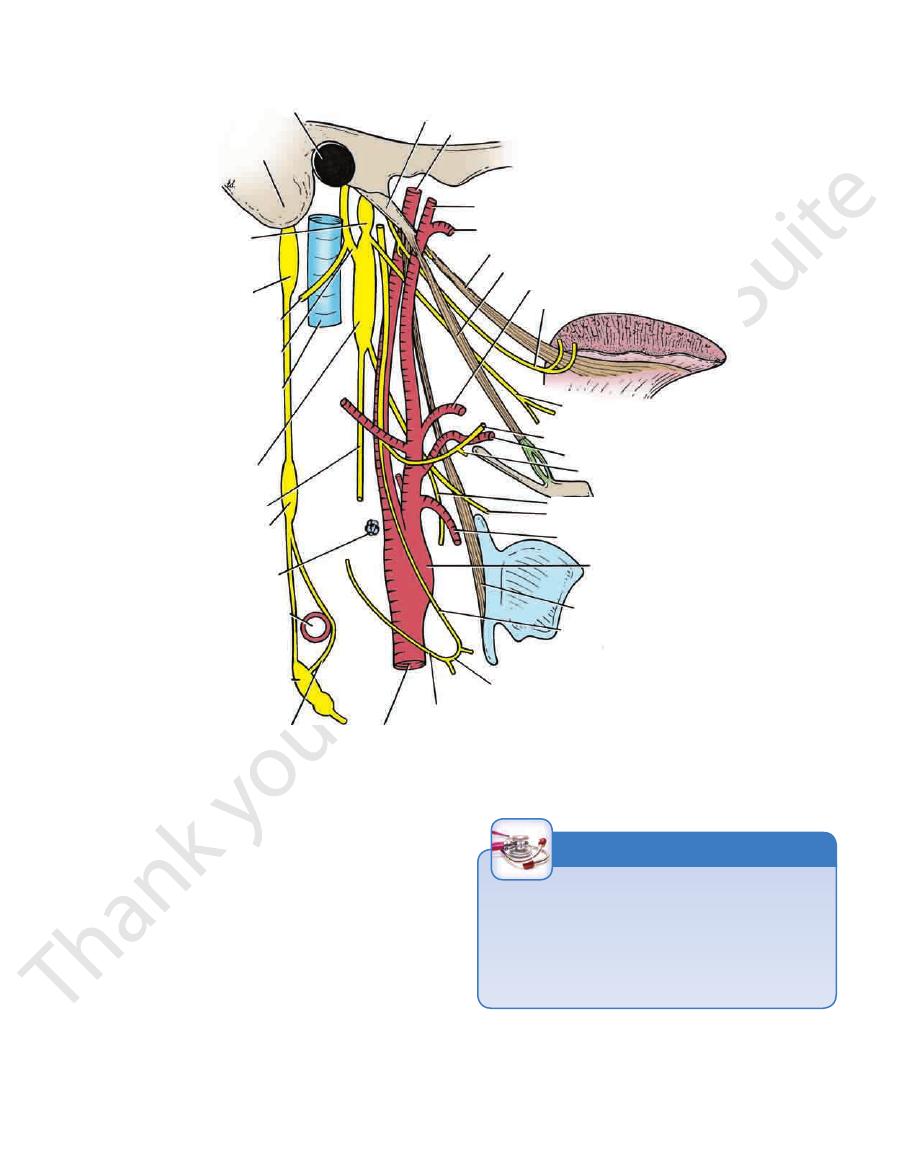
cervical
external auditory meatus
mastoid process
superior
ganglion
of vagus
superior
sympathetic
ganglion
spinal part of
accessory nerve
cranial part of
accessory nerve
internal jugular
vein
inferior
ganglion
of vagus
vagus nerve
middle cervical
ganglion
carotid body
subclavian artery
stellate ganglion
ansa subclavia
common carotid artery
descending cervical nerve (C2 and 3)
ansa cervicalis
descending branch of
hypoglossal nerve (C1)
stylopharyngeus
carotid sinus
superior thyroid artery
internal laryngeal nerve
external laryngeal nerve
nerve to thyrohyoid
lingual artery
hypoglossal nerve
pharyngeal branch of vagus nerve
glossopharyngeal nerve
facial artery
stylohyoid
styloglossus
maxillary artery
superficial temporal artery
internal carotid artery
styloid process
FIGURE 11.60
Styloid muscles, vessels, and nerves of the neck.
artery gives off no branches.
Apart from the two terminal branches, the common carotid
Branches of the Common Carotid Artery
ally, the vagus nerve (Fig. 11.49).
The internal jugular vein and, posterolater
Laterally:
roid gland also lies medially.
trachea and esophagus (Fig. 11.49). The lobe of the thy
The larynx and pharynx and, below these, the
Medially:
neck are the vertebral vessels.
sympathetic trunk (Fig. 11.57). In the lower part of the
cervical vertebrae, the prevertebral muscles, and the
The transverse processes of the lower four
Posteriorly:
superior belly of the omohyoid (Fig. 11.55)
mastoid, the sternohyoid, the sternothyroid, and the
The skin, the fascia, the sternocleido
Anterolaterally:
Relations of the Common Carotid Artery
■
■
-
■
■
■
■
-
■
■
-
Taking the Carotid Pulse
The bifurcation of the common carotid artery into the inter-
nal and external carotid arteries can be easily palpated just
beneath the anterior border of the sternocleidomastoid mus-
cle at the level of the superior border of the thyroid cartilage.
This is a convenient site to take the carotid pulse.
C L I N I C A L N O T E S
External Carotid Artery
tures in the neck, face, and scalp; it also supplies the tongue
of the common carotid artery (Fig. 11.59). It supplies struc
The external carotid artery is one of the terminal branches
-
598
CHAPTER 11
The internal carotid artery leaves the neck by passing into
gland (Figs. 11.60 and 11.85B).
lies superficially; it then passes deep to the parotid salivary
with the internal jugular vein and vagus nerve. At first it
artery ascends in the neck embedded in the carotid sheath
the brain, the eye, the forehead, and part of the nose. The
the thyroid cartilage (Figs. 11.55 and 11.59). It supplies
common carotid artery at the level of the upper border of
The internal carotid artery begins at the bifurcation of the
Internal Carotid Artery
nal carotid artery are shown in Figure 11.59.
The origin and distribution of the branches of the exter
where it is prone to damage after a blow to the head.
skull and the thin anteroinferior angle of the parietal bone,
upper part of the greater wing of the sphenoid bone of the
Accompanied by its vein, it grooves (or tunnels) through the
it lies close to the motor area of the cerebral cortex of the brain.
11.20 and 11.131). The anterior branch is important because
skull and divides into anterior and posterior branches (Figs.
foramen spinosum (Fig. 11.66). It runs laterally within the
The middle meningeal artery enters the skull through the
Middle Meningeal Artery
inside the skull.
cles of mastication, the nose, the palate, and the meninges
Branches supply the upper and the lower jaws, the mus
Branches of the Maxillary Artery
of the skull.
mandible (Fig. 11.59) and enters the pterygopalatine fossa
The maxillary artery runs forward medial to the neck of the
Maxillary Artery
nerve, and it supplies the scalp.
(Fig. 11.59). It is accompanied by the auriculotemporal
arch, where it may be palpated just in front of the auricle
The superficial temporal artery ascends over the zygomatic
Superficial Temporal Artery
scalp (Fig. 11.59).
The posterior auricular artery supplies the auricle and the
Posterior Auricular Artery
The artery supplies the back of the scalp (Fig. 11.59).
Occipital Artery
the face.
mandibular salivary gland, and the muscles and the skin of
supply the tonsil, the sub
Branches of the facial artery
terminates at the medial angle of the eye (Figs. 11.55 and
then ascends around the lateral margin of the mouth and
to the anterior border of the masseter muscle. The artery
border of the mandible. It then ascends over the face close
lar salivary gland and emerges and bends around the lower
the pharynx and the tonsil. It lies deep to the submandibu
The facial artery loops upward close to the outer surface of
Facial Artery
the tongue (Figs. 11.55 and 11.60).
The lingual artery loops upward and forward and supplies
Lingual Artery
plies the pharyngeal wall.
The ascending pharyngeal artery ascends along and sup
Ascending Pharyngeal Artery
plies the cricothyroid muscle.
accompanied by the external laryngeal nerve, which sup
pole of the thyroid gland (Figs. 11.55 and 11.60). It is
The superior thyroid artery curves downward to the upper
Superior Thyroid Artery
Maxillary artery
Superficial temporal artery
Posterior auricular artery
Occipital artery
Facial artery
Lingual artery
Ascending pharyngeal artery
Superior thyroid artery
Branches of the External Carotid Artery
gland, see Figure 11.85B.
For the relations of the external carotid artery in the parotid
arteries (Fig. 11.60).
vagus pass between the external and internal carotid
sopharyngeal nerve, and the pharyngeal branch of the
carotid artery. The stylopharyngeus muscle, the glos
The wall of the pharynx and the internal
Medially:
artery and then posterior to it.
11.85). The internal jugular vein first lies lateral to the
the parotid gland, it is crossed by the facial nerve (Fig.
digastric muscle, and the stylohyoid muscles. Within
hypoglossal nerve (Fig. 11.55), the posterior belly of the
being covered by skin and fascia. It is crossed by the
Above this level, the artery is comparatively superficial,
ning by the anterior border of the sternocleidomastoid.
The artery is overlapped at its begin
Anterolaterally:
Relations of the External Carotid Artery
the stylohyoid (Fig. 11.55).
to it. It is crossed by the posterior belly of the digastric and
but as it ascends in the neck, it passes backward and lateral
be felt. At first, it lies medial to the internal carotid artery,
of the sternocleidomastoid muscle, where its pulsations can
Close to its origin, the artery emerges from undercover
arteries.
ble by dividing into the superficial temporal and maxillary
stance of the parotid gland behind the neck of the mandi
border of the thyroid cartilage and terminates in the sub
and the maxilla. The artery begins at the level of the upper
The Head and Neck
-
-
■
■
-
■
■
-
■
■
■
■
■
■
■
■
■
■
■
■
■
■
■
■
-
-
-
11.59).
-
-
-
sphenoid bone. The internal carotid artery then inclines
upward again medial to the anterior clinoid process of the
cating with it). The artery then leaves the sinus and passes
ward in the cavernous venous sinus (without communi
part of the temporal bone. It then passes upward and for
the cranial cavity through the carotid canal in the petrous
-
-
backward, lateral to the optic chiasma, and
es by
terminat
dividing into the anterior and the middle cerebral arteries.

Basic Anatomy
The internal jugular vein and the vagus nerve
Laterally:
geal nerve
The pharyngeal wall and the superior laryn
Medially:
the upper three cervical vertebrae
longus capitis muscle, and the transverse processes of
The sympathetic trunk (Fig. 11.60), the
Posteriorly:
artery (Figs. 11.60 and 11.85B).
the vagus, the parotid gland, and the external carotid
the glossopharyngeal nerve, the pharyngeal branch of
lie the stylohyoid muscle, the stylopharyngeus muscle,
Above the digastric
the hypoglossal nerve (Fig. 11.55).
cia, the anterior border of the sternocleidomastoid, and
lie the skin, the fas
Anterolaterally: Below the digastric
Relations of the Internal Carotid Artery in the Neck
599
■
■
-
■
■
■
■
-
■
■
neck can cause visual impairment or blindness in the eye
Extensive arteriosclerosis of the internal carotid artery in the
Arteriosclerosis of the Internal Carotid Artery
on the side of the lesion because of insufficient blood flow
through the retinal artery. Motor paralysis and sensory loss
may also occur on the opposite side of the body because of
insufficient blood flow through the middle cerebral artery.
C L I N I C A L N O T E S
Branches of the Internal Carotid Artery
off the vertebral artery, the thyrocervical trunk, and the
the scalenus anterior muscle (Fig. 11.57). This part gives
the origin of the subclavian artery to the medial border of
The first part of the subclavian artery extends from
First Part of the Subclavian Artery
artery on each side and divides it into three parts.
The scalenus anterior muscle passes anterior to the
clavian artery (Fig. 11.57).
arches laterally in a manner similar to that of the right sub
in the thorax. It ascends to the root of the neck and then
The left subclavian artery arises from the arch of the aorta
Left Subclavian Artery
the outer border of the 1st rib, it becomes the axillary artery.
and between the scalenus anterior and medius muscles. At
and 11.59). It arches upward and laterally over the pleura
artery, behind the right sternoclavicular joint (Figs. 11.57
The right subclavian artery arises from the brachiocephalic
Right Subclavian Artery
Subclavian Arteries
arise from the circle and supply the brain.
that contribute to the circle. Cortical and central branches
the junction of the two vertebral arteries) are all arteries
communicating, posterior cerebral, and basilar (formed by
ies and the two vertebral arteries (Fig. 11.15). The anterior
sis between the branches of the two internal carotid arter
543) at the base of the brain. It is formed by the anastomo
The circle of Willis lies in the subarachnoid space (see page
Circle of Willis
the internal capsule of the brain.
tral branches that supply central masses of gray matter and
the cerebral cortex except the leg area. It also gives off cen
middle cerebral artery thus supplies all the motor area of
which are supplied by the posterior cerebral artery). The
pole and inferolateral surface of the hemisphere (both of
supplied by the anterior cerebral artery) and the occipital
the narrow strip along the superolateral margin (which is
the entire lateral surface of the cerebral hemisphere except
ally in the lateral cerebral sulcus of the brain. It supplies
of the internal carotid artery (Fig. 11.15), and it runs later
The middle cerebral artery is the largest terminal branch
Middle Cerebral Artery
communicating artery.
anterior
joined to the artery of the opposite side by the
the superolateral surfaces of the cerebral hemisphere. It is
the corpus callosum of the brain to supply the medial and
between the cerebral hemispheres and then winds around
internal carotid artery (Fig. 11.15). It passes forward
The anterior cerebral artery is a terminal branch of the
Anterior Cerebral Artery
the posterior cerebral artery (Fig. 11.15).
The posterior communicating artery runs backward to join
Posterior Communicating Artery
artery is an end artery and the only blood supply to the retina.
optic nerve and runs forward to enter the eyeball. The central
it gives off the central artery of the retina, which enters the
forward into the orbital cavity through the optic canal, and
as it emerges from the cavernous sinus (Fig. 11.20). It passes
The ophthalmic artery arises from the internal carotid artery
Ophthalmic Artery
branches, however, are given off in the skull.
There are no branches in the neck. Many important
-
-
-
-
-
internal thoracic artery.
spinal, posterior inferior cerebellar, medullary arteries
Meningeal, anterior and posterior
Branches in the skull:
Spinal and muscular arteries
Branches in the neck:
surfaces of the occipital lobe.
ral lobe and the visual cortex on the lateral and the medial
cal branches supply the inferolateral surfaces of the tempo
curves laterally and backward around the midbrain. Corti
(Fig. 11.15)
posterior cerebral artery
On each side, the
into the two posterior cerebral arteries.
pons, the cerebellum, and the internal ear. It finally divides
the anterior surface of the pons. It gives off branches to the
(Fig. 11.15) ascends in a groove on
basilar artery
The
sel of the opposite side to form the basilar artery.
at the level of the lower border of the pons, it joins the ves
the anterior surface of the medulla oblongata of the brain
through the foramen magnum into the skull. On reaching
ally above the posterior arch of the atlas and then ascends
upper six cervical vertebrae (Fig. 11.57). It passes medi
through the foramina in the transverse processes of the
ascends in the neck
vertebral artery
The
Branches
-
-
-
-
600
CHAPTER 11
this part.
vical arteries, the suprascapular arteries, or both arise from
has no branches. Occasionally, however, the superficial cer
The third part of the subclavian artery usually
Branches
the brachial plexus.
in the root of the neck, it is closely related to the nerves of
der of the 1st rib, where it becomes the axillary artery. Here,
across the posterior triangle of the neck to the lateral bor
lateral border of the scalenus anterior muscle (Fig. 11.57)
The third part of the subclavian artery extends from the
Third Part of the Subclavian Artery
deep muscles of the neck.
which supplies the
deep cervical artery,
spaces, and the
which supplies the 1st and the 2nd intercostal
tal artery,
superior intercos
dome of the pleura and divides into the
runs backward over the
costocervical trunk
The
Branches
scalenus anterior muscle (Fig. 11.57).
The second part of the subclavian artery lies behind the
Second Part of the Subclavian Artery
the superior epigastric and the musculophrenic arteries.
to the sternum; in the 6th intercostal space, it divides into
(Fig. 11.57). It descends vertically one fingerbreadth lateral
behind the 1st costal cartilage and in front of the pleura
descends into the thorax
internal thoracic artery
The
back of the scapula (Fig. 11.57).
chial plexus and follows the suprascapular nerve onto the
runs laterally over the bra
suprascapular artery
The
crosses the brachial plexus (Fig. 11.57).
is a small branch that
superficial cervical artery
The
inferior parathyroid glands.
recurrent laryngeal nerve. It supplies the thyroid and the
face of the thyroid gland, where it is closely related to the
ascends to the posterior sur
inferior thyroid artery
The
terminal branches (Fig. 11.57).
is a short trunk that gives off three
thyrocervical trunk
The
The Head and Neck
-
-
-
-
-
pressure is of great help, and the artery is compressed against
the subclavian artery. The use of a blunt object to exert the
strong pressure downward and backward on the third part of
remember that the hemorrhage can be stopped by exerting
In severe traumatic accidents to the upper limb involving lac
Palpation and Compression of the Subclavian
Artery in Patients with Upper Limb Hemorrhage
-
eration of the brachial or axillary arteries, it is important to
the upper surface of the 1st rib.
C L I N I C A L N O T E S
Veins of the Head and Neck
external jugular vein.
branch, which joins the posterior auricular vein to form the
anterior branch, which joins the facial vein, and a posterior
On leaving the parotid salivary gland, it divides into an
superficial temporal and the maxillary veins (Fig. 11.39).
The retromandibular vein is formed by the union of the
Retromandibular Vein
retromandibular vein.
illary vein joins the superficial temporal vein to form the
from the pterygoid venous plexus (Fig. 11.39). The max
The maxillary vein is formed in the infratemporal fossa
Maxillary Vein
retromandibular vein.
salivary gland, where it joins the maxillary vein to form the
and the auriculotemporal nerve and then enters the parotid
scalp (Fig. 11.39). It follows the superficial temporal artery
The superficial temporal vein is formed on the side of the
Superficial Temporal Vein
drains into the internal jugular vein.
by the anterior division of the retromandibular vein, and
side of the mouth. It then crosses the mandible, is joined
the face with the facial artery and passes around the lateral
with the cavernous sinus. The facial vein descends down
(Fig. 11.39). It is connected through the ophthalmic veins
supratrochlear veins
the union of the supraorbital and
The facial vein is formed at the medial angle of the eye by
Facial Vein
Veins of the Face and the Neck
spread of infection).
to the venous sinuses (and are an important route for the
skull bones (Fig. 11.9). They connect the veins of the scalp
The emissary veins are valveless veins that pass through the
Emissary Veins
vault of the skull (Fig. 11.9).
The diploic veins occupy channels within the bones of the
Diploic Veins
are described on page 544.
and inferior petrosal sinuses (Fig. 11.9). All these sinuses
the occipital sinus, the cavernous sinuses, and the superior
straight sinus, the transverse sinuses, the sigmoid sinuses,
include the superior and inferior sagittal sinuses, the
bones, the orbit, and the internal ear. The venous sinuses
no valves. They receive tributaries from the brain, the skull
page 544). They have thick, fibrous walls, but they possess
the meningeal layer of the dura mater (Fig. 11.37A; see also
The venous sinuses are situated between the periosteal and
Venous Sinuses
neighboring venous sinuses.
and the veins of the brainstem, all of which drain into the
They consist of the cerebral veins, the cerebellar veins,
The veins of the brain are thin walled and have no valves.
Veins of the Brain
The veins of the scalp, face, and neck
emissary veins
The veins of the brain, venous sinuses, diploic veins, and
The veins of the head and neck may be divided into
■
■
■
■
-
