
630
CHAPTER 11
The Head and Neck
Muscles of the Soft Palate
T A B L E 1 1 . 9
Tenses soft palate
Tensor veli palatini
Muscle
Origin
Insertion
Nerve Supply
Action
Spine of sphenoid,
auditory tube
With muscle of other
side, forms palatine
aponeurosis
Nerve to medial pterygoid
from mandibular nerve
Levator veli palatini
Petrous part of temporal
bone, auditory tube
Palatine aponeurosis
Pharyngeal plexus
Raises soft palate
Palatoglossus
Palatine aponeurosis
Side of tongue
Pharyngeal plexus
Pulls root of tongue
upward and backward,
narrows oropharyngeal
isthmus
Palatopharyngeus
Palatine aponeurosis
Posterior border of
thyroid cartilage
Pharyngeal plexus
Elevates wall of pharynx,
pulls palatopharyngeal
folds medially
Musculus uvulae
Posterior border of hard
palate
Mucous membrane of
uvula
Pharyngeal plexus
Elevates uvula
communication
between nasal
and mouth
cavities
palatal process
of maxilla
superior concha
middle
concha
inferior
concha
tongue
nasal
cavity
palatal process
of maxilla
mouth
cavity
nasal
cavity
mouth
cavity
primary
palate
palatal
processes
of the
maxilla
nasal septum
primary
palate
primary palate
formation of
secondary palate
incisive
foramen
future
hard
palate
soft
palate
uvula
1
A
B
2
1
2
3
3
4
nasal septum
FIGURE 11.82
A.
molar tooth (Fig. 11.72).
the mouth upon a small papilla opposite the upper second
the lateral surface of the masseter. It enters the vestibule of
the anterior border of the gland and passes forward over
The parotid duct emerges from
deep lobes.
superficial
mastoid muscle. The facial nerve divides the gland into
mandible (Fig. 11.85), and in front of the sternocleido
the external auditory meatus, behind the ramus of the
posed mostly of serous acini. It lies in a deep hollow below
The parotid gland is the largest salivary gland and is com
The different stages in the formation
The formation of the palate and the nasal septum (coronal section). B.
of the palate.
The Salivary Glands
Parotid Gland
-
-
and
Basic Anatomy
631
A
B
C
D
E
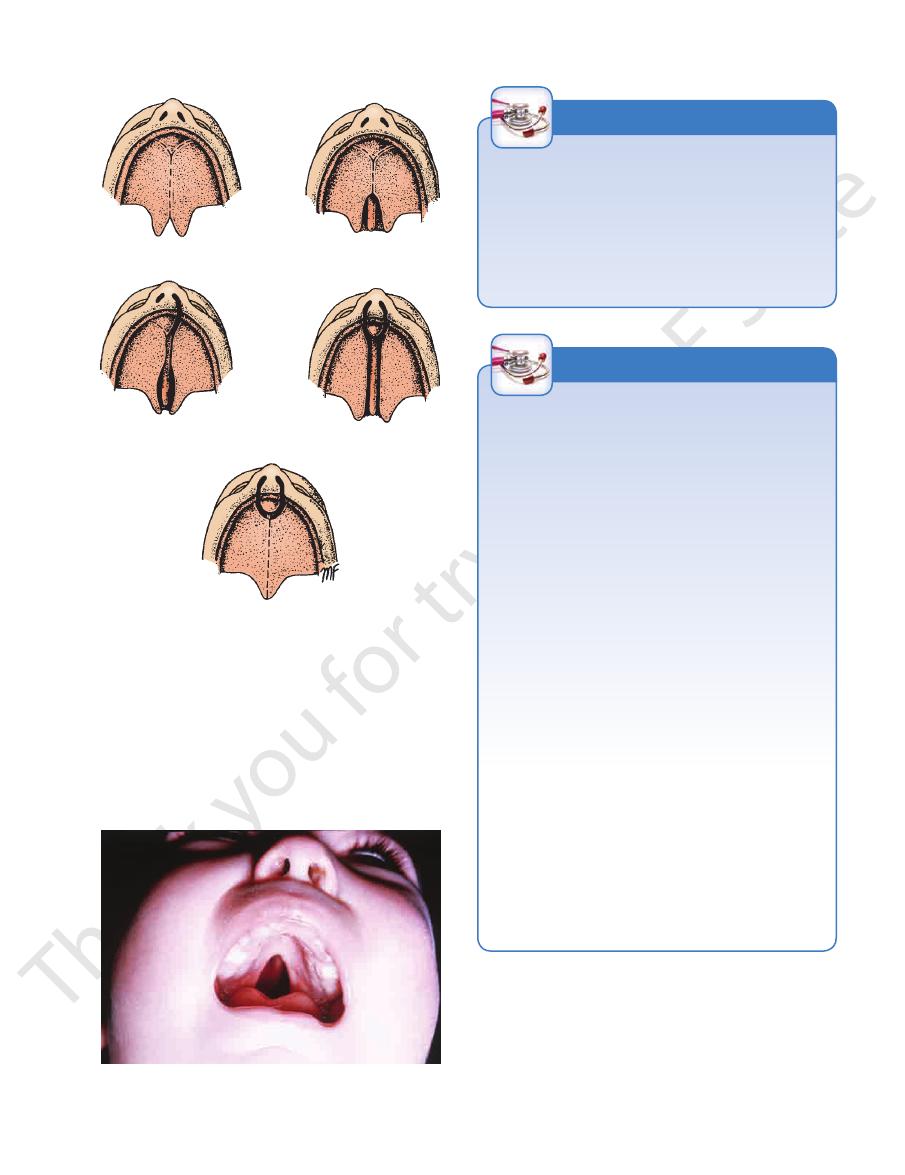
FIGURE 11.83
Different forms of cleft palate: cleft uvula
bilateral cleft lip and jaw
, total bilateral cleft palate and cleft lip
cleft lip
, total unilateral cleft palate and
cleft soft and hard palate
(A),
(B)
(C)
(D), and
(E).
FIGURE 11.84
Cleft hard and soft palate. (Courtesy of R.
glion, and the auriculotemporal nerve.
tympanic branch, the lesser petrosal nerve, the otic gan
sopharyngeal nerve. The nerves reach the gland via the
Parasympathetic secretomotor supply arises from the glos
Nerve Supply
Chase.)
-
-
across the masseter about a fingerbreadth below the zygo
Parotid Duct Injury
The parotid duct, which is a comparatively superficial struc-
ture on the face, may be damaged in injuries to the face or
may be inadvertently cut during surgical operations on the
face. The duct is about 2 in. (5 cm) long and passes forward
-
matic arch. It then pierces the buccinator muscle to enter the
mouth opposite the upper second molar tooth.
C L I N I C A L N O T E S
facial skin. By this means, a stimulus intended for saliva
Eventually, these fibers reach the sweat glands in the
out and join the distal end of the great auricular nerve.
secretomotor fibers in the auriculotemporal nerve grow
nerves. During the process of healing, the parasympathetic
by damage to the auriculotemporal and great auricular
on the skin covering the parotid. This condition is caused
gland. When the patient eats, beads of perspiration appear
times develops after penetrating wounds of the parotid
usually highly invasive and quickly involves the facial nerve,
Parotid Salivary Gland and Lesions of the Facial
Nerve
The parotid salivary gland consists essentially of superficial
and deep parts, and the important facial nerve lies in the inter-
val between these parts. A benign parotid neoplasm rarely, if
ever, causes facial palsy. A malignant tumor of the parotid is
causing unilateral facial paralysis.
Parotid Gland Infections
The parotid gland may become acutely inflamed as a result of
retrograde bacterial infection from the mouth via the parotid
duct. The gland may also become infected via the blood-
stream, as in mumps. In both cases, the gland is swollen; it is
painful because the fascial capsule derived from the invest-
ing layer of deep cervical fascia is strong and limits the swell-
ing of the gland. The swollen glenoid process, which extends
medially behind the temporomandibular joint, is responsible
for the pain experienced in acute parotitis when eating.
Frey’s Syndrome
Frey’s syndrome is an interesting complication that some-
production produces sweat secretion instead.
C L I N I C A L N O T E S
Submandibular Gland
of the mouth on the side of the tongue. The submandibular
deep part of the gland lies beneath the mucous membrane
superficial and deep parts by the mylohyoid muscle. The
body of the mandible (Fig. 11.86) and is divided into
and mucous acini. It lies beneath the lower border of the
The submandibular gland consists of a mixture of serous
632
CHAPTER 11
The Head and Neck
superficial
temporal vein
posterior
auricular vein
external jugular vein
angle of mandible
sternocleidomastoid
masseter
buccinator
orbicularis oris
parotid duct
accessory part of
parotid gland
zygomatic arch
temporalis
superior constrictor of pharynx
carotid sheath
internal jugular vein
glossopharyngeal nerve
accessory nerve
hypoglossal nerve
stylopharyngeus
styloid process
stylohyoid
posterior auricular artery
posterior belly
of digastric
mastoid process
skin
facial nerve
sternocleidomastoid
parotid lymph nodes
great auricular nerve
superficial part of parotid gland
deep part of parotid gland
masseter
ramus of mandible
formation of
retromandibular vein
medial pterygoid
division of external
carotid artery
stylomandibular ligament
fibrous capsule
fascial capsule
auriculotemporal nerve
styloglossus
internal carotid artery
vagus nerve
A
B
parotid gland
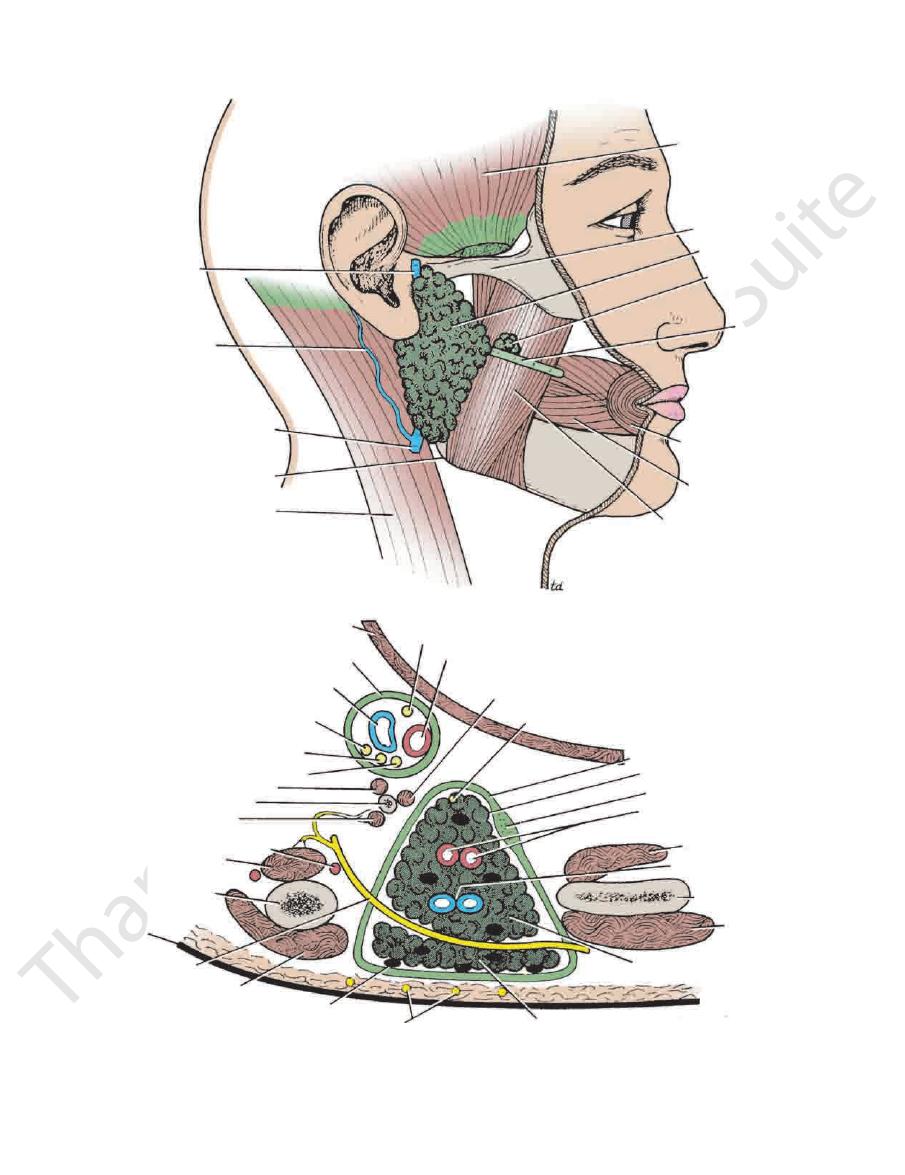
FIGURE 11.85
Parotid gland and its relations.
Horizontal
Lateral surface of the gland and the course of the parotid duct.
A.
B.
section of the parotid gland.

Basic Anatomy
633
super ficial part of submandibular gland
super ficial part of submandibular gland
deep part of submandibular gland
tongue
submandibular duct
opening of submandibular duct
central incisor tooth
sublingual gland
mylohyoid
body of mandible
anterior belly of digastric
hyoid bone
fibrous band
posterior belly of digastric
stylohyoid
mouth cavity
styloglossus
vestibule
buccinator
inferior alveolar nerve
muscles of tongue
fibrous septum
genioglossus
geniohyoid
mylohyoid
anterior belly of digastric
submandibular duct
sublingual gland
A
B
C
mylohyoid
deep part of submandibular gland
FIGURE 11.86
A.
gland.
ganglion. The postganglionic fibers pass directly to the
nerve via the chorda tympani, and the submandibular
Parasympathetic secretomotor supply is from the facial
Nerve Supply
(Fig. 11.72).
which is situated at the side of the frenulum of the tongue
of the mouth. It opens into the mouth on a small papilla,
gland and runs forward beneath the mucous membrane
duct emerges from the anterior end of the deep part of the
the ducts of the submandibular salivary glands.
Coronal section (anterior to B) through the sublingual salivary glands and
deep parts of the submandibular salivary glands.
lateral view
Submandibular and sublingual salivary glands (
). B. Coronal section through the superficial and
C.
Submandibular Salivary Gland: Calculus Formation
the condition. Examination of the floor of the mouth will reveal
is reduced in size or absent between meals, is diagnostic of
the mandible, which is greatest before or during a meal and
glands. The presence of a tense swelling below the body of
culus formation. This condition is rare in the other salivary
The submandibular salivary gland is a common site of cal-
C L I N I C A L N O T E S
(continued)

634
CHAPTER 11
The Head and Neck
Sublingual Gland
glion. Postganglionic fibers pass directly to the gland.
nerve via the chorda tympani, and the submandibular gan
Parasympathetic secretomotor supply is from the facial
Nerve Supply
summit of the sublingual fold (Fig. 11.72).
(8 to 20 in number) open into the mouth on the
gual ducts
sublin
mucous acini, with the latter predominating. The
frenulum of the tongue (Fig. 11.86). It has both serous and
(sublingual fold) of the floor of the mouth, close to the
The sublingual gland lies beneath the mucous membrane
-
-
nasal part
of pharynx
oral part of
pharynx
laryngeal part of
pharynx
FIGURE 11.87
Sagittal section through the nose, mouth,
(Fig. 11.89).
tubal elevation
ridge of which is called the
the elevated
auditory tube,
lateral wall is the opening of the
the soft palate and the posterior pharyngeal wall. On the
The pharyngeal isthmus is the opening in the floor between
(Fig. 11.89).
pharyngeal tonsil
lymphoid tissue called the
(Fig. 11.87). In the submucosa of the roof is a collection of
This lies above the soft palate and behind the nasal cavities
the oral pharynx, and the laryngeal pharynx.
The pharynx is divided into three parts: the nasal pharynx,
Table 11.10.
and actions of the pharyngeal muscles are summarized in
The details of the origins, insertions, nerve supply,
sphincteric part, the cricopharyngeus.
propulsive part of the inferior constrictor and the lower
area on the posterior pharyngeal wall between the upper
Killian’s dehiscence
pharynx and act as a sphincter.
horizontally around the lowest and narrowest part of the
(Fig. 11.88). The fibers of the cricopharyngeus pass
muscle
cricopharyngeus
from the cricoid cartilage, is called the
The lower part of the inferior constrictor, which arises
outside the lower part of the middle constrictor (Fig. 11.88).
of the superior constrictor and the inferior constrictor lies
the middle constrictor lies on the outside of the lower part
The three constrictor muscles overlap each other so that
of the occipital bone of the skull down to the esophagus.
extends from the pharyngeal tubercle on the basilar part
yngeal wall to be inserted into a fibrous band or raphe that
The three constrictor muscles extend around the phar
direction.
whose fibers run in a somewhat longitudinal
geus muscles,
salpingopharyn
stylopharyngeus
direction, and the
pharynx, and larynx to show the subdivisions of the pharynx.
and
-
-
is the
Interior of the Pharynx
Nasal Pharynx
Sublingual Salivary Gland and Cyst Formation
The sublingual salivary gland, which lies beneath the sub-
lingual fold of the floor of the mouth, opens into the mouth
by numerous small ducts. Blockage of one of these ducts is
believed to be the cause of cysts under the tongue.
C L I N I C A L N O T E S
absence of ejection of saliva from the orifice of the duct of the
superior, middle, and inferior constrictor muscles
The muscles in the wall of the pharynx consist of the
brane is also continuous with that of the tympanic cavity.
larynx. By means of the auditory tube, the mucous mem
(choanae), the opening into the mouth, and the inlet of the
Here, it is replaced by the posterior openings into the nose
musculomembranous wall, which is deficient anteriorly.
gus opposite the 6th cervical vertebra. The pharynx has a
lower, narrow end becoming continuous with the esopha
shaped, its upper, wider end lying under the skull and its
The pharynx is funnel
laryngeal parts.
nasal, oral,
mouth, and the larynx (Fig. 11.87) and may be divided into
The pharynx is situated behind the nasal cavities, the
a result of a pathologic condition of the scalp, face, maxillary
affected gland. Frequently, the stone can be palpated in the
duct, which lies below the mucous membrane of the floor of
the mouth.
Enlargement of the Submandibular Lymph Nodes
and Swelling of the Submandibular Salivary Gland
The submandibular lymph nodes are commonly enlarged as
sinus, or mouth cavity. One of the most common causes of
painful enlargement of these nodes is acute infection of the
teeth. Enlargement of these nodes should not be confused
with pathologic swelling of the submandibular salivary gland.
The Pharynx
and
-
-
Muscles of the Pharynx
(Fig.
fibers run in a somewhat circular
11.80A), whose
