Basic Anatomy
69
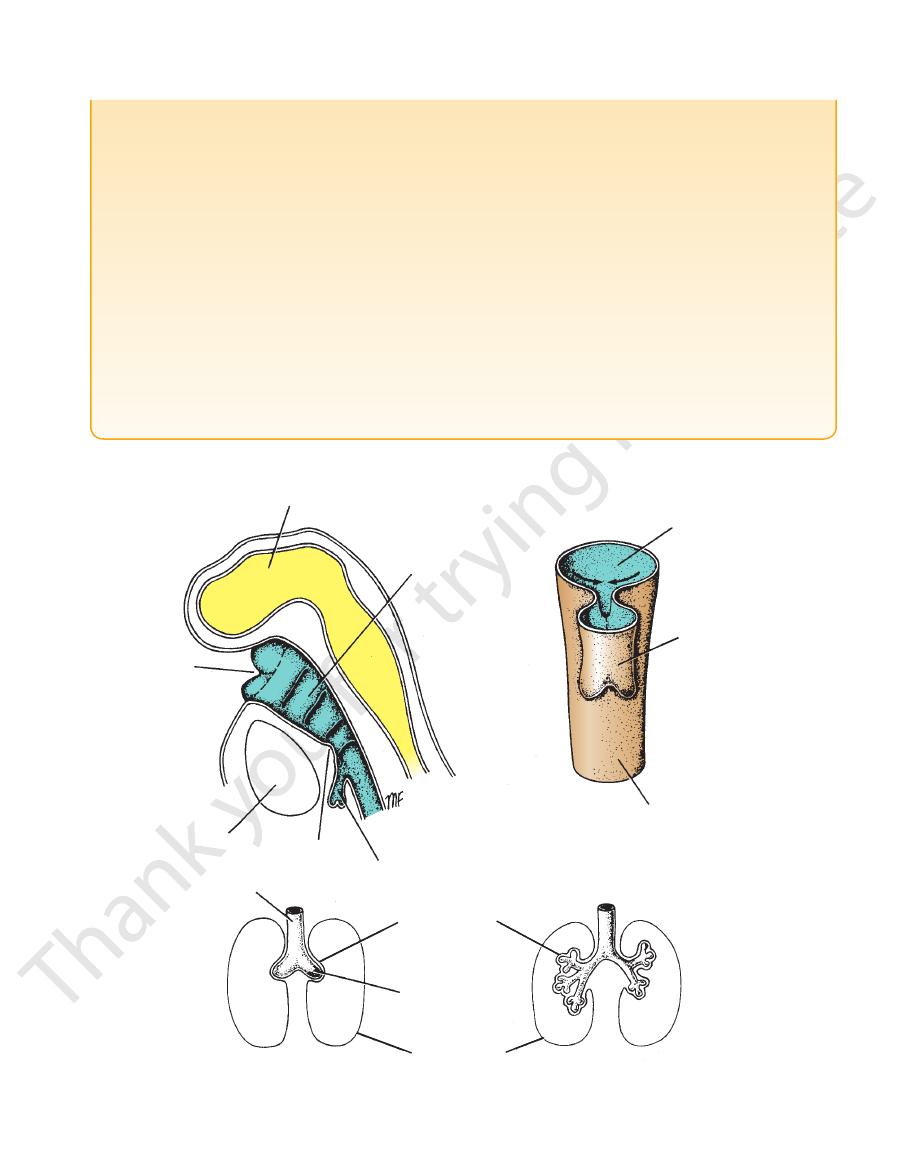
sympathetic trunk
cut rib
cut costal
cartilage
cut costal cartilage
azygos vein
intercostal nerve
right bronchi
pulmonary veins
greater splanchnic
nerve
inferior vena cava
right subclavian vein
right clavicle
right subclavius
muscle
internal thoracic
artery
superior vena cava
ascending aorta
right phrenic
nerve
right atrium
right ventricle
right cupola of
diaphragm
ANTERIOR
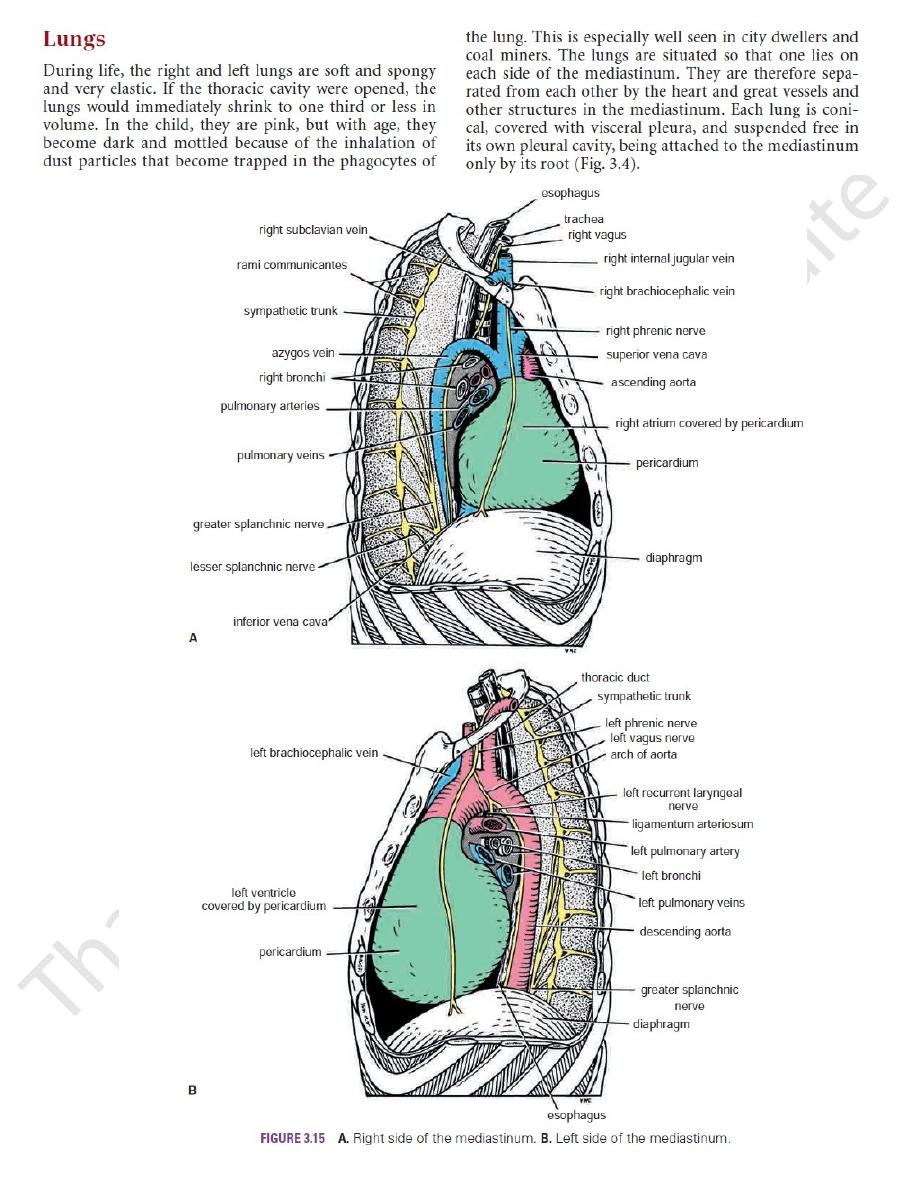
FIGURE 3.16
ed. The
Dissection of the right side of the mediastinum; the right lung and the pericardium have been remov
costal parietal pleura has also been removed.
left subclavian
artery
left common
carotid artery
arch of
aorta
pulmonary trunk
right ventricle
apex of heart
sympathetic
trunk
left vagus
nerve
descending
aorta
left auricle
left phrenic
nerve
left cupola of
diaphragm
left ventricle
ANTERIOR
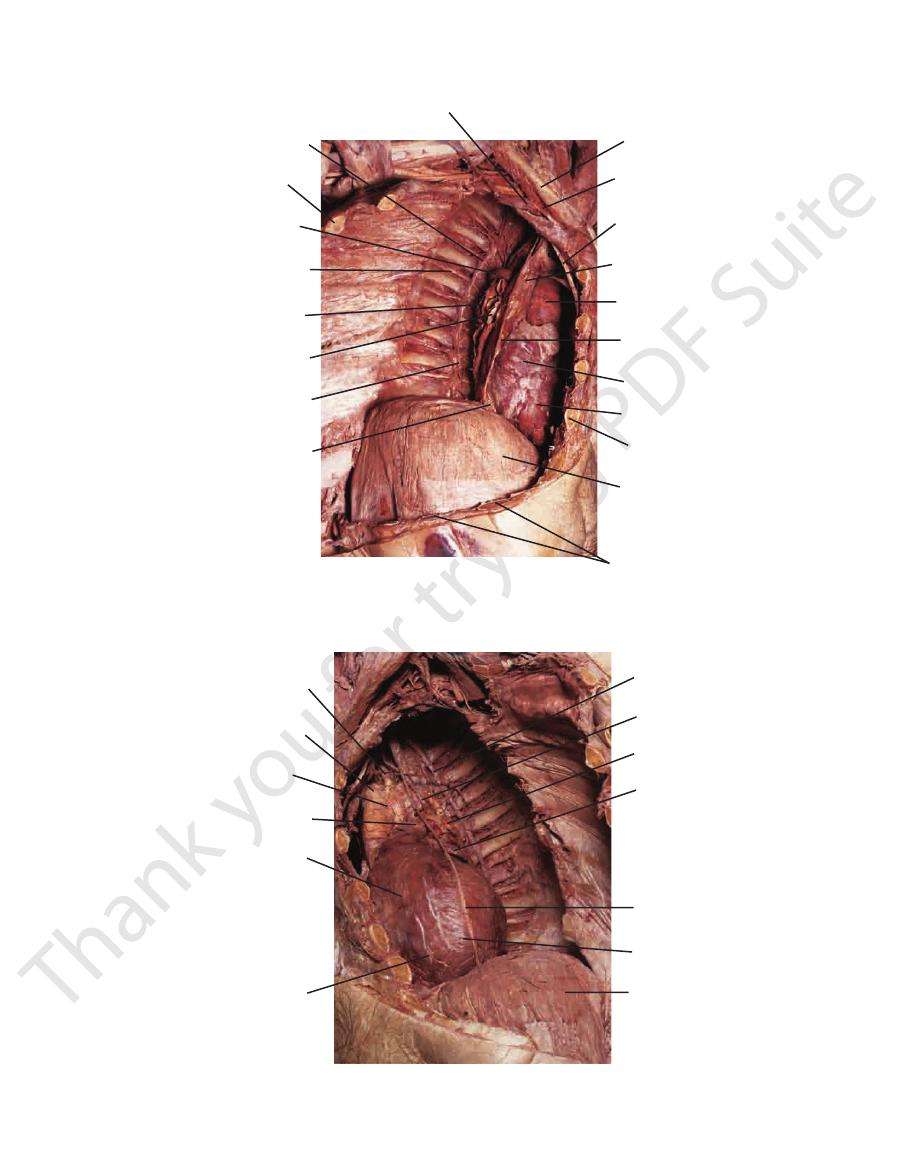
FIGURE 3.17
e been removed. The costal
Dissection of the left side of the mediastinum; the left lung and the pericardium hav
parietal pleura has also been removed.

70
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
respiratory bronchiole
trachea
left principal bronchus
lobar bronchus
segmental bronchus
alveolar duct
alveolar sac
alveolus
terminal bronchiole
FIGURE 3.18
Trachea, bronchi, bronchioles, alveolar ducts, alveolar sacs, and alveoli. Note the path taken by inspired air from
is found. The
cardiac notch
here on the left lung that the
is thin and overlaps the heart; it is
anterior border
The
enter and leave the lung.
root
form the
depression in which the bronchi, vessels, and nerves that
hilum,
3.21). At about the middle of this surface is the
cardium and other mediastinal structures (Figs. 3.20 and
which is molded to the peri
mediastinal surface,
concave
which corresponds to the concave chest wall; and a
face,
costal sur
that sits on the diaphragm; a convex
cave
the neck for about 1 in. (2.5 cm) above the clavicle; a con
which projects upward into
apex,
Each lung has a blunt
the trachea to the alveoli.
-
base
-
-
a
posterior border is thick and lies beside the vertebral column.
oblique fissure in the midaxillary line. The middle lobe is
surface at the level of the 4th costal cartilage to meet the
runs horizontally across the costal
horizontal fissure
The
posterior border about 2.5 in. (6.25 cm) below the apex.
ward across the medial and costal surfaces until it cuts the
runs from the inferior border upward and back
fissure
oblique
(Fig. 3.20). The
lower lobes
upper, middle,
by the oblique and horizontal fissures into three lobes: the
The right lung is slightly larger than the left and is divided
Lobes and Fissures
Right Lung
and
-

Basic Anatomy
71
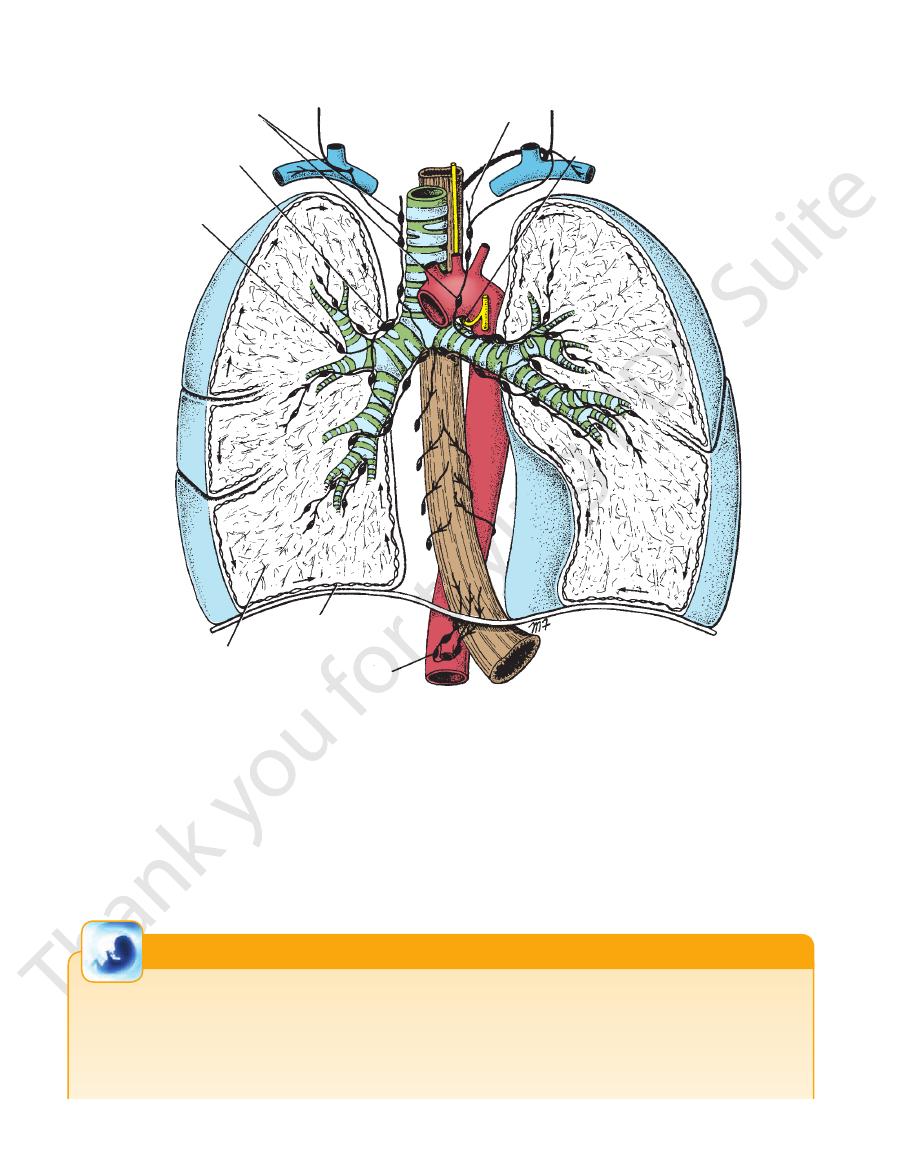
trachea
upper lobe of right lung
right principal
bronchus
upper lobe of left lung
left principal
bronchus
lower lobe
of left lung
lower lobe of right lung
bronchi in middle lobe of right lung
(dissected)
FIGURE 3.19
A plastinized specimen of an adult trachea,
of the trachea than the left main bronchus.
right main bronchus is wider and a more direct continuation
been dissected to reveal the larger bronchi. Note that the
principal bronchi, and lung; some of the lung tissue has
apex
upper lobe
horizontal fissure
middle
lobe
oblique fissure
base
lower
lobe
apex
lower lobe
middle
lobe
upper lobe
FIGURE 3.20
Lateral and medial surfaces of the right lung.
the blood within the surrounding capillaries.
the air in the alveolar lumen through the alveolar wall into
of blood capillaries. Gaseous exchange takes place between
and 3.23). Each alveolus is surrounded by a rich network
of several alveoli opening into a single chamber (Figs. 3.22
The alveolar sacs consist
alveolar sacs.
pouchings called
lead into tubular passages with numerous thin-walled out
which
alveolar ducts,
bronchioles end by branching into
a respiratory bronchiole is about 0.5 mm. The respiratory
The diameter of
respiratory bronchiole.
explains the name
air takes place in the walls of these outpouchings, which
ings from their walls. Gaseous exchange between blood and
(Fig. 3.22), which show delicate outpouch
bronchioles
terminal
The bronchioles then divide and give rise to
circularly arranged smooth muscle fibers.
epithelium. The submucosa possesses a complete layer of
cartilage in their walls and are lined with columnar ciliated
are <1 mm in diameter (Fig. 3.22). Bronchioles possess no
which
bronchioles,
smallest bronchi divide and give rise to
cartilage, which become smaller and fewer in number. The
in the trachea are gradually replaced by irregular plates of
chi become smaller, the U-shaped bars of cartilage found
mental bronchus divides repeatedly (Fig. 3.22). As the bron
On entering a bronchopulmonary segment, each seg
nerve supply.
Each segment has its own lymphatic vessels and autonomic
tive tissue between adjacent bronchopulmonary segments.
the tributaries of the pulmonary veins run in the connec
accompanied by a branch of the pulmonary artery, but
connective tissue (Fig. 3.22). The segmental bronchus is
which is surrounded by
bronchopulmonary segment,
functionally independent unit of a lung lobe called a
Each segmental bronchus passes to a structurally and
(Fig. 3.18).
segmental (tertiary) bronchi
branches called
ary) bronchus, which passes to a lobe of the lung, gives off
tional, and surgical units of the lungs. Each lobar (second
The bronchopulmonary segments are the anatomic, func
horizontal fissure in the left lung.
(Fig. 3.21). There is no
lower lobes
and
upper
lobes: the
The left lung is divided by a similar oblique fissure into two
Left Lung
oblique fissures.
thus a small triangular lobe bounded by the horizontal and
Bronchopulmonary Segments
-
-
-
-
-
-
-
apex
apex
upper lobe
lower lobe
base
oblique
fissure
lower lobe
upper lobe
FIGURE 3.21
Lateral and medial surfaces of the left lung.

72
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
autonomic nerves
lymphatic vessel
pulmonary vein
terminal bronchiole
respiratory
bonchiole
alveolar sac
bronchopulmonary segment
segmental bronchus
alveolus
lung lobule
pulmonary artery
pulmonary vein in
intersegmental
connective tissue
FIGURE 3.22
A bronchopulmonary segment and a lung lobule. Note that the pulmonary veins lie within the connective tissue
The main characteristics of a bronchopulmonary
septa that separate adjacent segments.
segment may be summarized as follows:
3.15, 3.16, and 3.17).
pleura to the visceral pleura covering the lungs (Figs. 3.5,
sheath of pleura, which joins the mediastinal parietal
vessels, and nerves. The root is surrounded by a tubular
chi, pulmonary artery and veins, lymph vessels, bronchial
entering or leaving the lung. It is made up of the bron
is formed of structures that are
root of the lung
The
pulmonary medicine or surgery.
to memorize the details unless one intends to specialize in
nary segments is of clinical importance, it is unnecessary
Although the general arrangement of the bronchopulmo
basal, lateral basal, posterior basal
Superior (apical), medial basal, anterior
Inferior lobe:
gular, inferior lingular
Apical, posterior, anterior, superior lin
Superior lobe:
Left lung
basal, lateral basal, posterior basal
Superior (apical), medial basal, anterior
Inferior lobe:
Lateral, medial
Middle lobe:
Apical, posterior, anterior
Superior lobe:
Right lung
3.25) are as follows:
The main bronchopulmonary segments (Figs. 3.24 and
removed surgically.
Because it is a structural unit, a diseased segment can be
adjacent bronchopulmonary segments.
The segmental vein lies in the connective tissue between
vessels, and autonomic nerves.
It has a segmental bronchus, a segmental artery, lymph
It is surrounded by connective tissue.
root.
It is pyramid shaped, with its apex toward the lung
It is a subdivision of a lung lobe.
■
■
■
■
■
■
■
■
■
■
■
■
■
■
■
■
-
-
-
Basic Anatomy
73
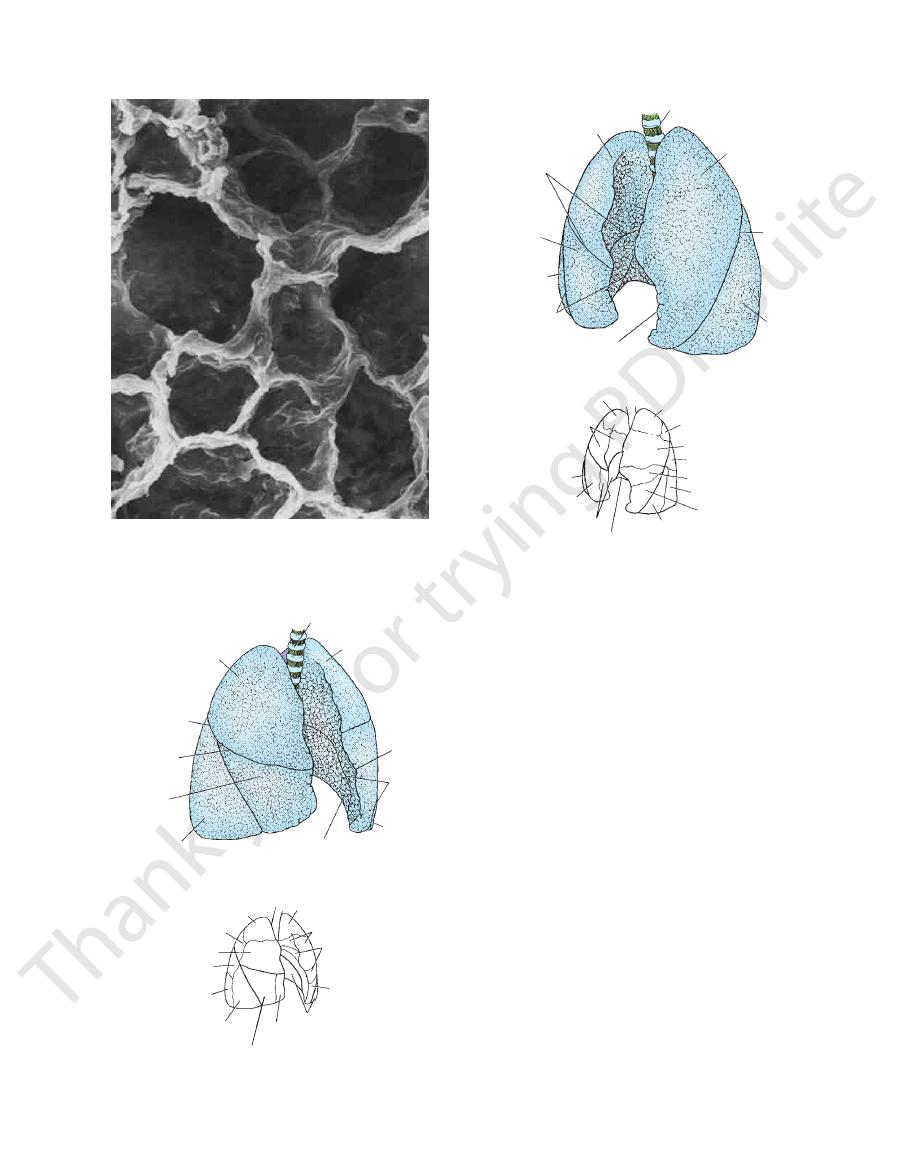
FIGURE 3.23
Scanning electron micrograph of the lung
tesy of Dr. M. Koering.)
sions, or alcoves, along the walls of the alveolar sac. (Cour
showing numerous alveolar sacs. The alveoli are the depres-
-
upper lobe of
right lung
oblique
fissure
horizontal
fissure
middle lobe
of right lung
lower lobe
of right lung
lower lobe
of left lung
lower lobe
of left lung
oblique
fissure
cardiac
notch
upper lobe
of left lung
trachea
lateral
division
of middle
medial
division
of middle
anterior basal
inferior division
of lingular
superior division
of lingular
anterior
apical
apical
posterior
anterior
apical lower
lateral basal
anterior basal
B
A
FIGURE 3.24
Lungs viewed from the right.
Bronchopulmonary segments.
Lobes.
A.
B.
upper lobe
of right lung
horizontal
fissure
middle lobe
of right lung
lower lobe
of right lung
oblique
fissure
cardiac
notch
lower lobe
of left lung
oblique
fissure
upper lobe
of left lung
trachea
apical
medial division
of middle
posterior
basal
anterior
basal
inferior division of lingular
lateral basal
superior division of lingular
apical lower
anterior
posterior
apical
A
B
lateral division
of middle
anterior
anterior
basal
FIGURE 3.25
Lungs viewed from the left.
bronchomediastinal lymph trunks.
then into the
and
tracheobronchial nodes
the hilum and drains into the
in the hilum of the lung. All the lymph from the lung leaves
stance; the lymph then enters the bronchopulmonary nodes
located within the lung sub
pulmonary nodes
ing through
and pulmonary vessels toward the hilum of the lung, pass
travels along the bronchi
deep plexus
The
monary nodes.
bronchopul
the hilum, where the lymph vessels enter the
ceral pleura and drains over the surface of the lung toward
lies beneath the vis
superficial (subpleural) plexus
The
uses (Fig. 3.26); they are not present in the alveolar walls.
The lymph vessels originate in superficial and deep plex
Lymph Drainage of the Lungs
into the left atrium of the heart.
pulmonary veins leave each lung root (Fig. 3.15) to empty
mental connective tissue septa to the lung root. Two
taries of the pulmonary veins, which follow the interseg
blood leaving the alveolar capillaries drains into the tribu
nal branches of the pulmonary arteries. The oxygenated
The alveoli receive deoxygenated blood from the termi
veins) drain into the azygos and hemiazygos veins.
bronchial veins (which communicate with the pulmonary
arteries, which are branches of the descending aorta. The
ceral pleura receive their blood supply from the bronchial
The bronchi, the connective tissue of the lung, and the vis
chopulmonary segments.
Lobes.
A.
B. Bron-
Blood Supply of the Lungs
-
-
-
-
-
-
-
-
-
74
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
tracheobronchial nodes
bronchopulmonary nodes
pulmonary nodes
deep lymphatic plexus
superficial lymphatic plexus
celiac nodes
left recurrent laryngeal nerve
bronchomediastinal trunk
FIGURE 3.26
Lymph drainage of the lung and lower end of the esophagus.
and decrease of the capacity of the thoracic cavity. The rate
ration—which are accomplished by the alternate increase
Respiration consists of two phases—inspiration and expi
parasympathetic nerves.
pass to the central nervous system in both sympathetic and
membrane and from stretch receptors in the alveolar walls
Afferent impulses derived from the bronchial mucous
increased glandular secretion.
fibers produce bronchoconstriction, vasodilatation, and
tion and vasoconstriction. The parasympathetic efferent
The sympathetic efferent fibers produce bronchodilata
receives parasympathetic fibers from the vagus nerve.
is formed from branches of the sympathetic trunk and
of efferent and afferent autonomic nerve fibers. The plexus
composed
pulmonary plexus
At the root of each lung is a
Nerve Supply of the Lungs
-
The Mechanics of Respiration
-
Development of the Lungs and Pleura
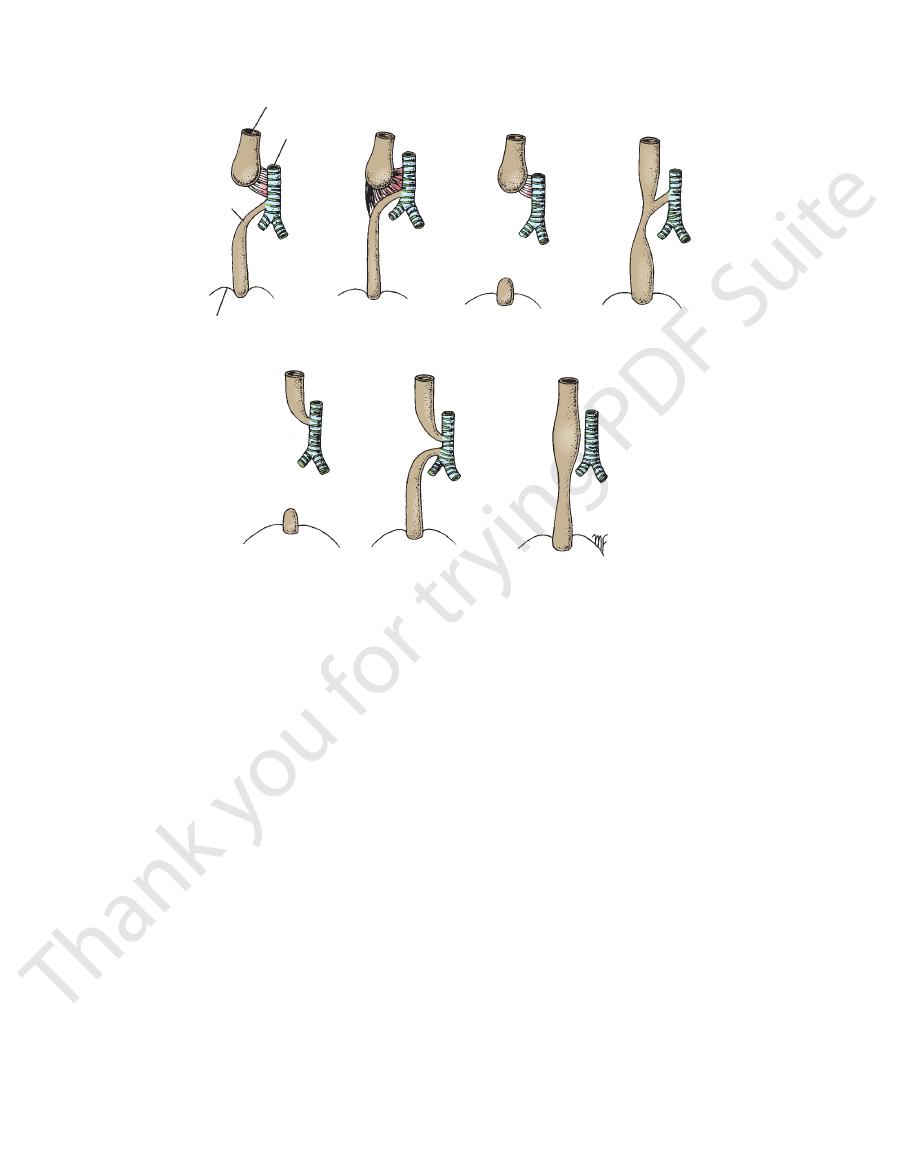
the permanent opening into the larynx. The laryngotracheal tube
and the epithelium of the alveoli develop from this groove. The
A longitudinal groove develops in the entodermal lining of the
floor of the pharynx. This groove is known as the laryngotra-
cheal groove. The lining of the larynx, trachea, and bronchi
margins of the groove fuse and form the laryngotracheal tube
(Fig. 3.27). The fusion process starts distally so that the lumen
becomes separated from the developing esophagus. Just behind
the developing tongue, a small opening persists that will become
grows caudally into the splanchnic mesoderm and will eventually
lie anterior to the esophagus. The tube divides distally into the
(continued)
E M B R Y O L O G I C N O T E S
Basic Anatomy
75
right and left
ferent types of atresia, with and without fistula, are shown in
formed from somatic mesoderm. By the seventh month, the
derived
visceral pleura
Each lung will receive a covering of
ects into the pleural part of the embryonic coelom (Fig. 3.27). The
surrounding the tube, and the upper part of the tube becomes
lung buds. Cartilage develops in the mesenchyme
the larynx, whereas the lower part becomes the trachea.
Each lung bud consists of an entodermal tube surrounded
by splanchnic mesoderm; from this, all the tissues of the corre-
sponding lung are derived. Each bud grows laterally and proj-
lung bud divides into three lobes and then into two, correspond-
ing to the number of main bronchi and lobes found in the fully
developed lung. Each main bronchus then divides repeatedly in
a dichotomous manner, until eventually the terminal bronchioles
and alveoli are formed. The division of the terminal bronchioles,
with the formation of additional bronchioles and alveoli, contin-
ues for some time after birth.
from the splanchnic mesoderm. The parietal pleura will be
capillary loops connected with the pulmonary circulation have
become sufficiently well developed to support life, should pre-
mature birth take place. With the onset of respiration at birth, the
lungs expand and the alveoli become dilated. However, it is only
after 3 or 4 days of postnatal life that the alveoli in the periphery
of each lung become fully expanded.
Congenital Anomalies
Esophageal Atresia and Tracheoesophageal Fistula
If the margins of the laryngotracheal groove fail to fuse ade-
quately, an abnormal opening may be left between the laryn-
gotracheal tube and the esophagus. If the tracheoesophageal
septum formed by the fusion of the margins of the laryngo-
tracheal groove should be deviated posteriorly, the lumen of
the esophagus would be much reduced in diameter. The dif-
Figure 3.28. Obstruction of the esophagus prevents the child from
early diagnosis, it is often possible to correct this serious anom
larynx and trachea, which usually results in pneumonia. With
swallowing saliva and milk, and this leads to aspiration into the
-
aly surgically.
brain
pharynx
mouth
pericardial cavity
copula
laryngotracheal tube
pharynx
laryngotracheal tube
esophagus
trachea
visceral pleura
lung bud
parietal pleura
A
B
C
D
FIGURE 3.27
The development of the lungs.
The lung buds divide to form the main bronchi.
The lung buds invaginate the wall of the intraembryonic
the laryngotracheal groove fuse to form the laryngotracheal tube.
The margins of
The laryngotracheal groove and tube have been formed.
A.
B.
C.
coelom. D.
76
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
esophagus
trachea
fistula
diaphragm
A
B
C
D
E
F
G
FIGURE 3.28
Different types of esophageal atresia and tracheoesophageal fistula.
nal viscera and the tone of the muscles of the anterior
the effect of the descent of the diaphragm on the abdomi
An additional factor that must not be overlooked is
(Fig. 3.10).
the other ribs to it by contracting the intercostal muscles
this can be accomplished by fixing the 1st rib and raising
thoracic cavity will be increased. As described previously,
raised (like bucket handles), the transverse diameter of the
dles (see Fig. 3.29). It therefore follows that if the ribs are
as forward around the chest wall, they resemble bucket han
vertebral column. Because the ribs curve downward as well
the sternum via their costal cartilages and behind with the
The ribs articulate in front with
Transverse Diameter
the first rib.
means, all the ribs are drawn together and raised toward
contracting the intercostal muscles (Fig. 3.10). By this
by the contraction of the scaleni muscles of the neck and
(Fig. 3.29). This can be brought about by fixing the 1st rib
the lower end of the sternum would be thrust forward
diameter of the thoracic cavity would be increased and
ribs were raised at their sternal ends, the anteroposterior
If the downward-sloping
Anteroposterior Diameter
diaphragm is lowered (Fig. 3.29).
contracts, the domes become flattened and the level of the
is formed by the mobile diaphragm. When the diaphragm
suprapleural membrane and is fixed. Conversely, the floor
raised and the floor lowered. The roof is formed by the
Theoretically, the roof could be
Vertical Diameter
and how they may be increased (Fig. 3.29).
Consider now the three diameters of the thoracic cavity
sure entering the box through the tube.
diameters, and this results in air under atmospheric pres
capacity of the box can be increased by elongating all its
(Fig. 3.29). The
trachea
at the top, which is a tube called the
Compare the thoracic cavity to a box with a single entrance
Inspiration
patients and is faster in children and slower in the elderly.
varies between 16 and 20 per minute in normal resting
cases, the lower esophageal segment communicates with the trachea, and types A and B occur more commonly.
Narrowing of the esophagus without a fistula. In most
Separate esophagotracheal and tracheoesophageal fistulas.
An esophagotracheal fistula; the esophagus is not connected with the distal end, which is rudimentary.
A tracheoesophageal fistula with narrowing of
Complete blockage of the esophagus; the distal end is rudimentary.
Similar to type A, but the two parts of the esophagus are joined together by fibrous tis
with a tracheoesophageal fistula.
Complete blockage of the esophagus
A.
B.
-
sue. C.
D.
the esophagus. E.
F.
G.
Quiet Inspiration
-
-
-
abdominal wall. As the diaphragm descends on inspiration,
the diaphragm will now have its central tendon supported
further diaphragmatic descent. On further contraction,
other upper abdominal viscera act as a platform that resists
further abdominal relaxation is possible, and the liver and
nal wall musculature. However, a point is reached when no
accommodated by the reciprocal relaxation of the abdomi
intra-abdominal pressure rises. This rise in pressure is
-

Basic Anatomy
77
expanding thoracic cavity
bucket handle action
lateral expansion
descent of diaphragm
anteroposterior expansion
expanding box
FIGURE 3.29
The different ways in which the capacity of the
supported by grasping a chair back or table, the sternal
lis minor to pull up the ribs. If the upper limbs can be
muscles, enabling the serratus anterior and the pectora
are fixed by the trapezius, levator scapulae, and rhomboid
already engaged becomes more violent, and the scapulae
toid. In respiratory distress, the action of all the muscles
scalenus anterior and medius and the sternocleidomas
can raise the ribs is brought into action, including the
capacity of the thoracic cavity occurs. Every muscle that
In deep forced inspiration, a maximum increase in the
Forced Inspiration
serratus posterior superior muscles.
muscles
levatores costarum
assist in elevating the ribs, namely, the
less important muscles also contract on inspiration and
Apart from the diaphragm and the intercostals, other
intercostal muscles in raising the lower ribs (Fig. 3.10).
from below, and its shortening muscle fibers will assist the
thoracic cavity is increased during inspiration.
and the
-
-
origin of the
oralis major muscles can also assist the
pect
abdominal form.
racic and abdominal forms of respiration, but mainly the
The male uses both the tho
thoracic type of respiration.
the diaphragm on inspiration. This is referred to as the
the movements of the ribs rather than on the descent of
piratory movements. The female tends to rely mainly on
In the adult, a sexual difference exists in the type of res
oblique, and the adult form of respiration is established.
After the second year of life, the ribs become more
abdominal type of respiration.
is easily seen, respiration at this age is referred to as the
outward excursion of the anterior abdominal wall, which
tion. Because this is accompanied by a marked inward and
diaphragm to increase their thoracic capacity on inspira
tal. Thus, babies have to rely mainly on the descent of the
In babies and young children, the ribs are nearly horizon
Types of Respiration
a higher level.
size. The lower margins of the lungs shrink and rise to
and the costodiaphragmatic recess becomes reduced in
matic and costal parietal pleura come into apposition,
ment of the diaphragm, increasing areas of the diaphrag
lungs become reduced in size. With the upward move
contract. The elastic tissue of the lungs recoils, and the
the bifurcation of the trachea. The bronchi shorten and
In expiration, the roots of the lungs ascend along with
minor role.
inferior and the latissimus dorsi muscles may also play a
the lowered 12th rib (Fig. 3.10). The serratus posterior
may contract, pull the ribs together, and depress them to
under these circumstances some of the intercostal muscles
tracts and pulls down the 12th rib. It is conceivable that
rior abdominal wall. The quadratus lumborum also con
the forcible contraction of the musculature of the ante
Forced expiration is an active process brought about by
Forced Expiration
ing down the lower ribs.
play a minor role in pull
ratus posterior inferior muscles
ser
wall, which forces the relaxing diaphragm upward. The
increase in tone of the muscles of the anterior abdominal
tion of the intercostal muscles and diaphragm, and an
brought about by the elastic recoil of the lungs, the relaxa
Quiet expiration is largely a passive phenomenon and is
Expiration
lower level.
the expanding sharp lower edges of the lungs descend to a
costodiaphragmatic recess of the pleural cavity opens, and
nective tissue are stretched. As the diaphragm descends, the
the lungs, the elastic tissue in the bronchial walls and con
increased capacity of the thoracic cavity. With expansion of
sure on the outer surface of the lungs brought about by the
upper part of the respiratory tract and the negative pres
of the positive atmospheric pressure exerted through the
circulation. Air is drawn into the bronchial tree as the result
alveolar capillaries dilate, thus assisting the pulmonary
as two vertebrae. The bronchi elongate and dilate and the
the bifurcation of the trachea may be lowered by as much
In inspiration, the root of the lung descends and the level of
process.
Lung Changes on Inspiration
-
-
Quiet Expiration
-
-
-
-
-
Lung Changes on Expiration
-
-
-
-
-
-
78
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
Physical Examination of the Lungs
is often quickly followed by infection. To aid in the normal drain
Excessive accumulation of bronchial secretions in a lobe or seg
and
Many diseases of the lungs, such as
ther impeded by the presence of excess mucus, which the patient
racic cage becomes permanently enlarged, forming the so-called
ficulty in expiring, although inspiration is accomplished normally.
tion, usually causing the asthmatic patient to experience great dif
spasm of the smooth muscle in the wall of the bronchioles. This
One of the problems associated with bronchial asthma is the
the lower deep cervical nodes just above the level of the clavicle.
the bronchomediastinal trunks may result in early involvement in
nerves, leading to hoarseness of the voice. Lymphatic spread via
bronchomediastinal nodes and may involve the recurrent laryngeal
lung. The neoplasm rapidly spreads to the tracheobronchial and
larger bronchi and is therefore situated close to the hilum of the
commences in most patients in the mucous membrane lining the
deaths in men and is becoming increasingly common in women. It
Bronchogenic carcinoma accounts for about one third of all cancer
benign neoplasm may require surgical removal. If it is restricted
costal cartilages are sufficiently elastic to permit considerable
retractors that allow the ribs to be widely separated are used. The
taken through an intercostal space (see page 46). Special rib
shoulder because the skin of this region is supplied by the supra
nerve endings, so that pain in the chest is always the result of
visceral pleura until it reaches the lung root. It then passes into the
the lung connective tissue. From there, the air moves under the
pneumothorax and collapse of the lung. It can also find its way into
the lung, and air can escape into the pleural cavity, causing a
cage, a splinter from a fractured rib can nevertheless penetrate
Although the lungs are well protected by the bony thoracic
For physical examination of the patient, it is helpful to remember
that the upper lobes of the lungs are most easily examined from
the front of the chest and the lower lobes from the back. In the
axillae, areas of all lobes can be examined.
Trauma to the Lungs
A physician must always remember that the apex of the lung
projects up into the neck (1 in. [2.5 cm] above the clavicle) and
can be damaged by stab or bullet wounds in this area.
mediastinum and up to the neck. Here, it may distend the subcu-
taneous tissue, a condition known as subcutaneous emphysema.
The changes in the position of the thoracic and upper abdom-
inal viscera and the level of the diaphragm during different
phases of respiration relative to the chest wall are of consider-
able clinical importance. A penetrating wound in the lower part
of the chest may or may not damage abdominal viscera, depend-
ing on the phase of respiration at the time of injury.
Pain and Lung Disease
Lung tissue and the visceral pleura are devoid of pain-sensitive
conditions affecting the surrounding structures. In tuberculosis
or pneumonia, for example, pain may never be experienced.
Once lung disease crosses the visceral pleura and the pleural
cavity to involve the parietal pleura, pain becomes a prominent
feature. Lobar pneumonia with pleurisy, for example, produces a
severe tearing pain, accentuated by inspiring deeply or cough-
ing. Because the lower part of the costal parietal pleura receives
its sensory innervation from the lower five intercostal nerves,
which also innervate the skin of the anterior abdominal wall,
pleurisy in this area commonly produces pain that is referred to
the abdomen. This has sometimes resulted in a mistaken diagno-
sis of an acute abdominal lesion.
In a similar manner, pleurisy of the central part of the dia-
phragmatic pleura, which receives sensory innervation from the
phrenic nerve (C3, 4, and 5), can lead to referred pain over the
-
clavicular nerves (C3 and 4).
Surgical Access to the Lungs
Surgical access to the lung or mediastinum is commonly under-
bending. Good exposure of the lungs is obtained by this method.
Segmental Resection of the Lung
A localized chronic lesion such as that of tuberculosis or a
to a bronchopulmonary segment, it is possible carefully to dis-
sect out a particular segment and remove it, leaving the sur-
rounding lung intact. Segmental resection requires that the
radiologist and thoracic surgeon have a sound knowledge of the
bronchopulmonary segments and that they cooperate fully to
localize the lesion accurately before operation.
Bronchogenic Carcinoma
Hematogenous spread to bones and the brain commonly occurs.
Conditions That Decrease Respiratory Efficiency
Constriction of the Bronchi (Bronchial Asthma)
particularly reduces the diameter of the bronchioles during expira-
-
The lungs consequently become greatly distended and the tho-
barrel chest. In addition, the air flow through the bronchioles is fur-
is unable to clear because an effective cough cannot be produced.
Loss of Lung Elasticity
emphysema
pulmonary
fibrosis, destroy the elasticity of the lungs, and thus the lungs are
unable to recoil adequately, causing incomplete expiration. The
respiratory muscles in these patients have to assist in expiration,
which no longer is a passive phenomenon.
Loss of Lung Distensibility
Diseases such as silicosis, asbestosis, cancer, and pneumonia
interfere with the process of expanding the lung in inspiration.
A decrease in the compliance of the lungs and the chest wall
then occurs, and a greater effort has to be undertaken by the
inspiratory muscles to inflate the lungs.
Postural Drainage
-
ment of a lung can seriously interfere with the normal flow of air
into the alveoli. Furthermore, the stagnation of such secretions
-
age of a bronchial segment, a physiotherapist often alters the
position of the patient so that gravity assists in the process of
drainage. Sound knowledge of the bronchial tree is necessary to
determine the optimum position of the patient for good postural
drainage.
C L I N I C A L N O T E S

Basic Anatomy
that closely covers the heart (Fig. 3.32).
continuous with the visceral layer of serous pericardium
reflected around the roots of the great vessels to become
lines the fibrous pericardium and is
parietal layer
The
(Fig. 3.31).
coats the heart. It is divided into parietal and visceral layers
The serous pericardium lines the fibrous pericardium and
nopericardial ligaments.
ster
pericardium is attached in front to the sternum by the
cavae, and the pulmonary veins (Fig. 3.32). The fibrous
the pulmonary trunk, the superior and inferior venae
vessels passing through it (Fig. 3.31)—namely, the aorta,
diaphragm. It fuses with the outer coats of the great blood
sac. It is firmly attached below to the central tendon of the
The fibrous pericardium is the strong fibrous part of the
vertebrae.
costal cartilages and anterior to the 5th to the 8th thoracic
terior to the body of the sternum and the 2nd to the 6th
middle mediastinum (Figs. 3.2, 3.30, 3.31, and 3.32), pos
of the heart can contract. The pericardium lies within the
serve as a lubricated container in which the different parts
restrict excessive movements of the heart as a whole and to
heart and the roots of the great vessels. Its function is to
The pericardium is a fibroserous sac that encloses the
79
Pericardium
-
Fibrous Pericardium
-
Serous Pericardium
right common
carotid artery
right subclavian
artery and vein
brachiocephalic
artery
right brachiocephalic
vein
superior vena
cava
right lung
pericardium
diaphragm
left lung
left
brachiocephalic
vein
left subclavian
artery and vein
left common carotid artery
esophagus
trachea
FIGURE 3.30
The pericardium and the lungs exposed from
in front.
parietal layer of
serous pericardium
visceral layer of serous
pericardium (epicardium)
fibrous pericardium
large blood vessel
heart
pericardial cavity
FIGURE 3.31
Different layers of the pericardium.
apex, which is directed downward, forward, and to the left.
phragmatic (inferior), and a base (posterior). It also has an
The heart has three surfaces: sternocostal (anterior), dia
pericardium.
the great blood vessels but otherwise lies free within the
astinum (Figs. 3.33 and 3.34). It is connected at its base to
amid shaped and lies within the pericardium in the medi
The heart is a hollow muscular organ that is somewhat pyr
branches of the sympathetic trunks and the vagus nerves.
ceral layer of the serous pericardium is innervated by
pericardium are supplied by the phrenic nerves. The vis
The fibrous pericardium and the parietal layer of the serous
page 91). They have no clinical significance.
sequence of the way the heart bends during development
(see
large veins (Fig. 3.32). The pericardial sinuses form as a con
the aorta and pulmonary trunk and the reflection around the
that lies between the reflection of serous pericardium around
which is a short passage
transverse sinus,
of the heart is the
(Fig. 3.32). Also on the posterior surface
oblique sinus
serous pericardium around the large veins forms a recess called
On the posterior surface of the heart, the reflection of the
which acts as a lubricant to facilitate movements of the heart.
pericardial fluid,
amount of tissue fluid (about 50 mL), the
(Fig. 3.31). Normally, the cavity contains a small
cavity
pericardial
parietal and visceral layers is referred to as the
The slitlike space between the
epicardium.
often called the
is closely applied to the heart and is
visceral layer
The
Pericardial Sinuses
the
-
Nerve Supply of the Pericardium
-
Heart
-
-
Surfaces of the Heart
-
