Basic Anatomy
by dividing into right and left principal (main)
carina
line of the neck. In the thorax, the trachea ends below at
level of the 6th cervical vertebra. It descends in the mid
the larynx at the lower border of the cricoid cartilage at the
tube (Fig. 3.9). It begins in the neck as a continuation of
The trachea is a mobile cartilaginous and membranous
Trachea
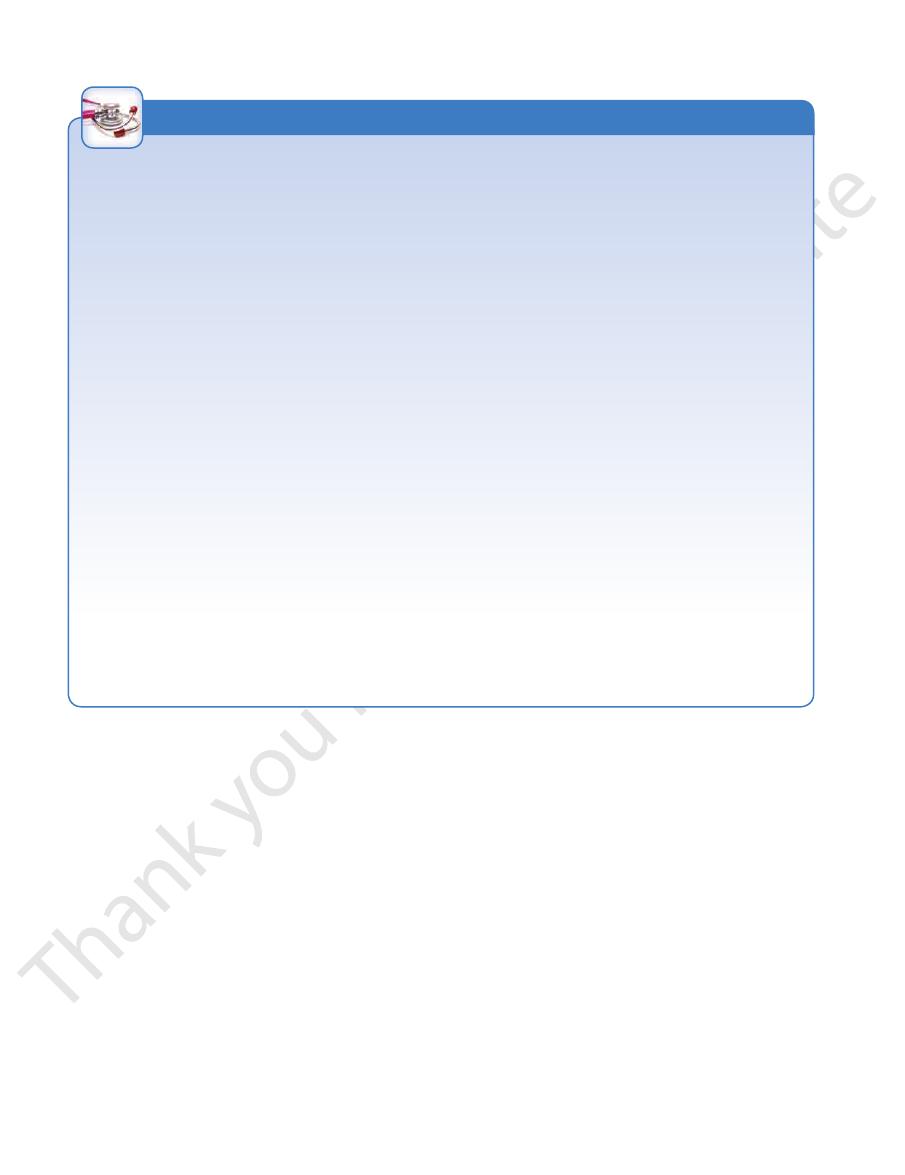
monary plexus (Fig. 3.7).
touch. It receives an autonomic nerve supply from the pul
but is insensitive to common sensations such as pain and
The visceral pleura covering the lungs is sensitive to stretch
63
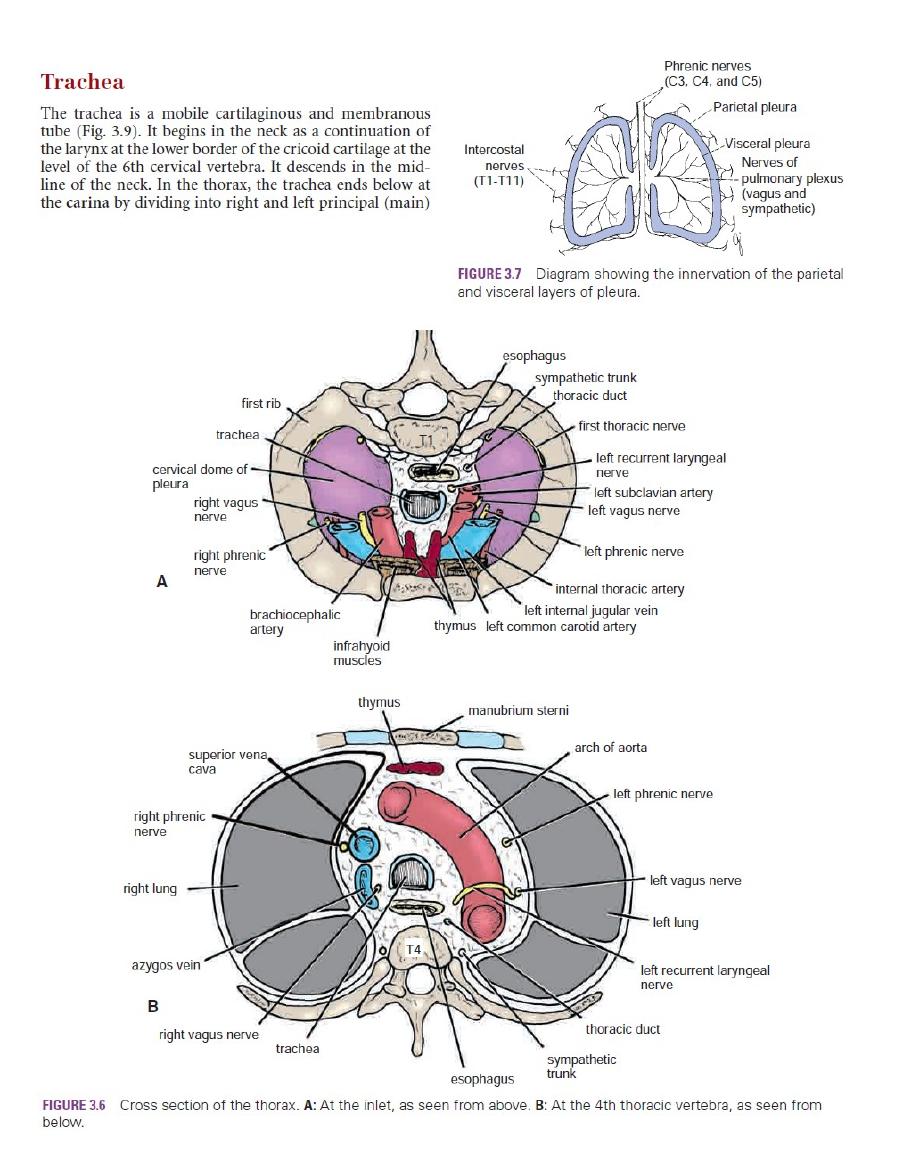
-
-
the
nerve
first rib
trachea
cervical dome of
pleura
right vagus
right phrenic
nerve
brachiocephalic
artery
infrahyoid
muscles
thymus left common carotid artery
left internal jugular vein
internal thoracic artery
left phrenic nerve
left vagus nerve
left subclavian artery
left recurrent laryngeal
nerve
first thoracic nerve
thoracic duct
sympathetic trunk
esophagus
T1
superior vena
cava
right phrenic
nerve
right lung
azygos vein
right vagus nerve
trachea
esophagus
sympathetic
trunk
thoracic duct
left recurrent laryngeal
nerve
left lung
left vagus nerve
left phrenic nerve
arch of aorta
manubrium sterni
thymus
T4
A
B
FIGURE 3.6
Cross section of the thorax.
below.
At the 4th thoracic vertebra, as seen from
At the inlet, as seen from above.
A:
B:
Phrenic nerves
(C3, C4, and C5)
Intercostal
nerves
(T1-T11)
Parietal pleura
Visceral pleura
Nerves of
pulmonary plexus
(vagus and
sympathetic)
FIGURE 3.7
Diagram showing the innervation of the parietal
and visceral layers of pleura.
64
CHAPTER 3
muscle.
laryngeal nerves. Sympathetic nerves supply the trachealis
The sensory nerve supply is from the vagi and the recurrent
Nerve Supply of the Trachea
lymph nodes and the deep cervical nodes.
The lymph drains into the pretracheal and paratracheal
Lymph Drainage of the Trachea
ies and the lower third is supplied by the bronchial arteries.
The upper two thirds are supplied by the inferior thyroid arter
Blood Supply of the Trachea
left phrenic nerves, and the pleura (Figs. 3.6, 3.15B,
carotid and left subclavian arteries, the left vagus and
The arch of the aorta, the left common
Left side:
the pleura (Figs. 3.6, 3.15A, and 3.16)
The azygos vein, the right vagus nerve, and
Right side:
The Thorax: Part II—The Thoracic Cavity
■
■
■
■
and 3.17)
-
Pleural Fluid
bleeding from blood vessels in the chest wall, from vessels in the
In hemopneumothorax, blood enters the pleural cavity. It can
deflected mediastinum. This dangerous condition is called a
on the injured side and the opposite lung is compressed by the
toward the opposite side. In this situation, a collapsed lung is
builds up on the wounded side and pushes the mediastinum
through the wound. In these circumstances, the air pressure
form a valve so that air enters on inspiration but cannot exit
the clothing and the layers of the thoracic wall combine to
pressure being sucked into the pleural cavity. Sometimes
patient inspires, it is possible to hear air under atmospheric
Each time the
pleura so that the pleural cavity is open to the outside air.
Stab wounds of the thoracic wall may pierce the parietal
wall (pneumothorax). In the old treatment of tuberculosis, air was
As the result of disease or injury (stab or gunshot wounds), air
the surfaces to be roughened. This roughening produces fric
surfaces becoming coated with inflammatory exudate, causing
), results in the pleural
inflammation of the lung (e.g.,
decreased breath sounds and dullness on percussion over the
decreased lung expansion on the side of the effusion, with
cient to enable its clinical detection. The clinical signs include
The presence of 300 mL
nancy, congestive heart disease) or impairs the drainage of the
increases the production of the fluid (e.g., inflammation, malig
into the capillaries of the visceral pleura. Any condition that
(pulmonary circulation), the pleural fluid is normally absorbed
the parietal pleura than in the capillaries of the visceral pleura
Since the hydrostatic pressures are greater in the capillaries of
of the fluid results from hydrostatic and osmotic pressures.
parietal pleurae during respiratory movements. The formation
which lubricates the apposing surfaces of the visceral and
The pleural space normally contains 5 to 10 mL of clear fluid,
-
fluid (e.g., collapsed lung) results in the abnormal accumula-
tion of fluid, called a pleural effusion.
of fluid in the costodiaphragmatic recess in an adult is suffi-
effusion (Fig. 3.8).
Pleurisy
Inflammation of the pleura (pleuritis or pleurisy), secondary to
pneumonia
-
tion, and a pleural rub can be heard with the stethoscope on
inspiration and expiration. Often, the exudate becomes invaded
by fibroblasts, which lay down collagen and bind the visceral
pleura to the parietal pleura, forming pleural adhesions.
Pneumothorax, Empyema, and Pleural Effusion
can enter the pleural cavity from the lungs or through the chest
purposely injected into the pleural cavity to collapse and rest the
lung. This was known as artificial pneumothorax. A spontane-
ous pneumothorax is a condition in which air enters the pleural
cavity suddenly without its cause being immediately apparent.
After investigation, it is usually found that air has entered from a
diseased lung and a bulla (bleb) has ruptured.
This condition is called open pneumothorax.
tension pneumothorax.
Air in the pleural cavity associated with serous fluid is known
as hydropneumothorax, associated with pus as pyopneumo-
thorax, and associated with blood as hemopneumothorax.
A collection of pus (without air) in the pleural cavity is called an
empyema. The presence of serous fluid in the pleural cavity is
referred to as a pleural effusion (Fig. 3.9). Fluid (serous, blood, or
pus) can be drained from the pleural cavity through a wide-bore
needle, as described on page 45.
be caused by stab or bullet wounds to the chest wall, resulting in
chest cavity, or from a lacerated lung.
C L I N I C A L N O T E S
bronchi at the level of the sternal angle (opposite the disc
geal nerve (Fig. 3.6A)
The esophagus and the left recurrent laryn
Posteriorly:
(Figs. 3.6A, 3.9, and 3.30)
left common carotid arteries, and the arch of the aorta
cephalic vein, the origins of the brachiocephalic and
The sternum, the thymus, the left brachio
Anteriorly:
num of the thorax are as follows:
The relations of the trachea in the superior mediasti
page 651.
The relations of the trachea in the neck are described on
trachealis muscle.
ends of the cartilage are connected by smooth muscle, the
of hyaline cartilage embedded in its wall. The posterior free
tube is kept patent by the presence of U-shaped bars (rings)
and 1 in. (2.5 cm) in diameter (Fig. 3.9). The fibroelastic
In adults, the trachea is about 4 1/2 in. (11.25 cm) long
6th thoracic vertebra.
and during deep inspiration may be lowered as far as the
ration, the bifurcation rises by about one vertebral level,
between the 4th and 5th thoracic vertebrae). During expi-
-
■
■
-
■
■
-
Basic Anatomy
65
esophagus
trachea
brachiocephalic
artery
arch of aorta
right principal
bronchus
descending aorta
stomach
esophagus
left principal
bronchus
left common
carotid artery
left subclavian
artery
left recurrent
laryngeal nerve
thoracic duct
lumen of right principal bronchus
right principal bronchus
left principal bronchus
carina
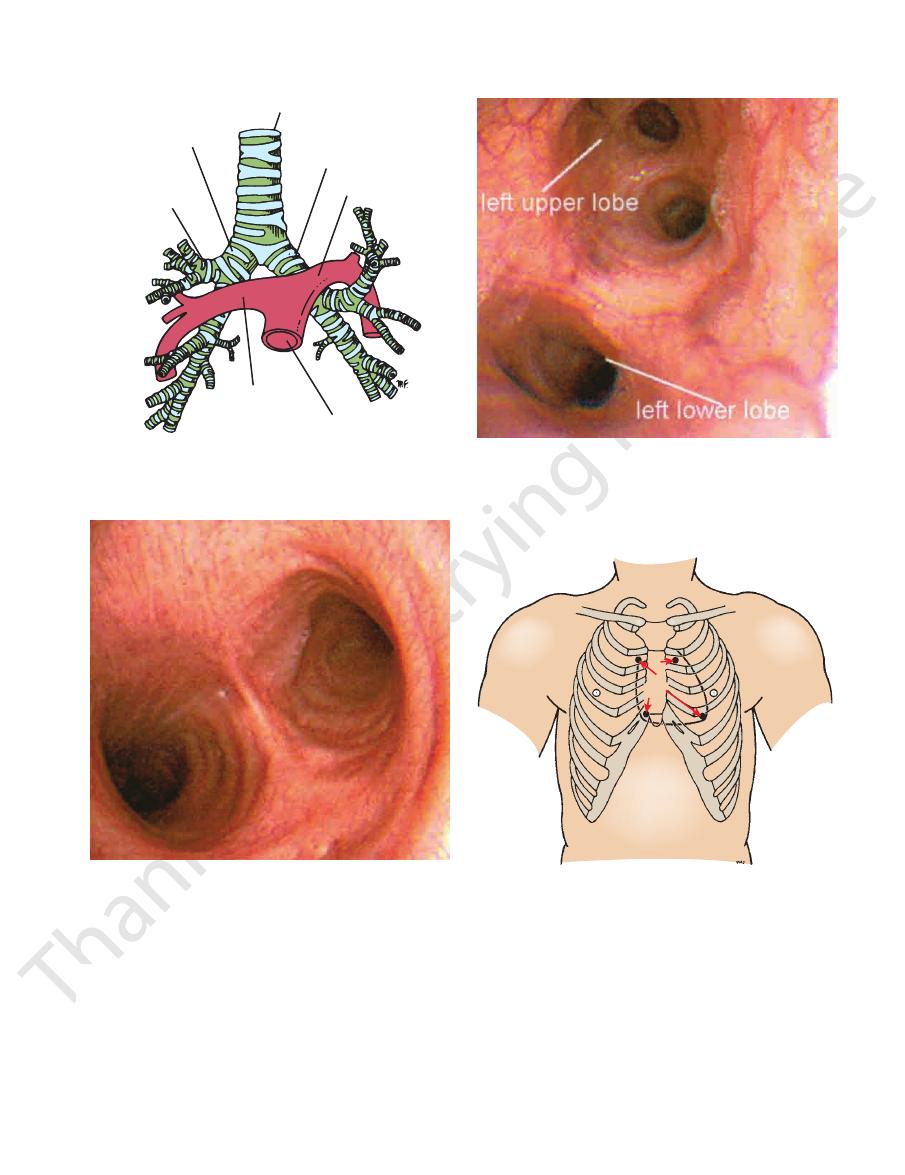
FIGURE 3.9
Thoracic part of the trachea. Note that the right
viewed from above is also shown.
ation of the trachea than the left. Bifurcation of the trachea
principal bronchus is wider and has a more direct continu-
trachea
displaced to left
pleural effusion
serous
fluid
absent breath
sounds
collapsed
right lung
diminished breath
sounds
FIGURE 3.8
Case of right-sided pleural effusion. The
inferior lobar bronchus.
superior
the left lung, the principal bronchus divides into a
On entering the hilum of
in front of the esophagus.
(5 cm) long. It passes to the left below the arch of the aorta
and more horizontal than the right and is about 2 in.
The left principal (main) bronchus is narrower, longer,
inferior lobar bronchus
middle
it divides into a
On entering the hilum,
superior lobar bronchus.
off the
the hilum of the right lung, the principal bronchus gives
and 3.19) and is about 1 in. (2.5 cm) long. Before entering
shorter, and more vertical than the left (Figs. 3.9, 3.18,
The right principal (main) bronchus (Fig. 3.11) is wider,
walls of the sacs as diverticula (see page 71).
ducts that enter the alveolar sacs. The alveoli arise from the
Each respiratory bronchiole divides into 2 to 11 alveolar
that terminate in one or more respiratory bronchioles.
mously, giving rise to several million terminal bronchioles
(Figs. 3.9, 3.18, and 3.19). The bronchi divide dichoto
right and left principal (primary or main) bronchi
The trachea bifurcates behind the arch of the aorta into
and absent breath sounds over fluid in the pleural cavity.
reveal only faint breath sounds over the compressed lung
pressed, and the bronchi are narrowed. Auscultation would
mediastinum is displaced to the left, the right lung is com-
The Bronchi
the
-
Principal Bronchi
and an
.
and
and an
Compression of the Trachea
lateral or bilateral enlargement of the thyroid gland can cause
The trachea is a membranous tube kept patent under normal
conditions by U-shaped bars of cartilage. In the neck, a uni-
gross displacement or compression of the trachea. A dilatation
of the aortic arch (aneurysm) can compress the trachea. With
each cardiac systole, the pulsating aneurysm may tug at the tra-
chea and left bronchus, a clinical sign that can be felt by palpat-
ing the trachea in the suprasternal notch.
C L I N I C A L N O T E S
(continued)
66
CHAPTER 3
The Thorax: Part II—The Thoracic Cavity
Tracheitis or Bronchitis
immediate relief to prevent asphyxiation. A method commonly used
membrane of the larynx secondary to infection or trauma may require
Lodgment of a foreign body in the larynx or edema of the mucous
Bronchoscopy enables a physician to examine the interior of the
to enter the right instead of the left bronchus. From there, they
traveling to the central nervous system accompany autonomic
display this phenomenon. The afferent fibers from these organs
not under normal conditions directly relayed to consciousness
It seems that organs possessing a sensory innervation that is
give rise to discomfort that is felt in the midline (see page 224).
pain. Many thoracic and abdominal viscera, when diseased,
burning sensation felt deep to the sternum instead of actual
monary plexus. A tracheitis or bronchitis gives rise to a raw,
The mucosa lining the trachea is innervated by the recurrent
laryngeal nerve and, in the region of its bifurcation, by the pul-
nerves.
Inhaled Foreign Bodies
Inhalation of foreign bodies into the lower respiratory tract is
common, especially in children. Pins, screws, nuts, bolts, pea-
nuts, and parts of chicken bones and toys have all found their
way into the bronchi. Parts of teeth may be inhaled while a
patient is under anesthesia during a difficult dental extraction.
Because the right bronchus is the wider and more direct con-
tinuation of the trachea (Figs. 3.18 and 3.19), foreign bodies tend
usually pass into the middle or lower lobe bronchi.
Bronchoscopy
trachea; its bifurcation, called the carina; and the main bronchi
(Figs. 3.12 and 3.13). With experience, it is possible to examine
the interior of the lobar bronchi and the beginning of the first
segmental bronchi. By means of this procedure, it is also pos-
sible to obtain biopsy specimens of mucous membrane and to
remove inhaled foreign bodies (even an open safety pin).
to relieve complete obstruction is tracheostomy (see page 654).
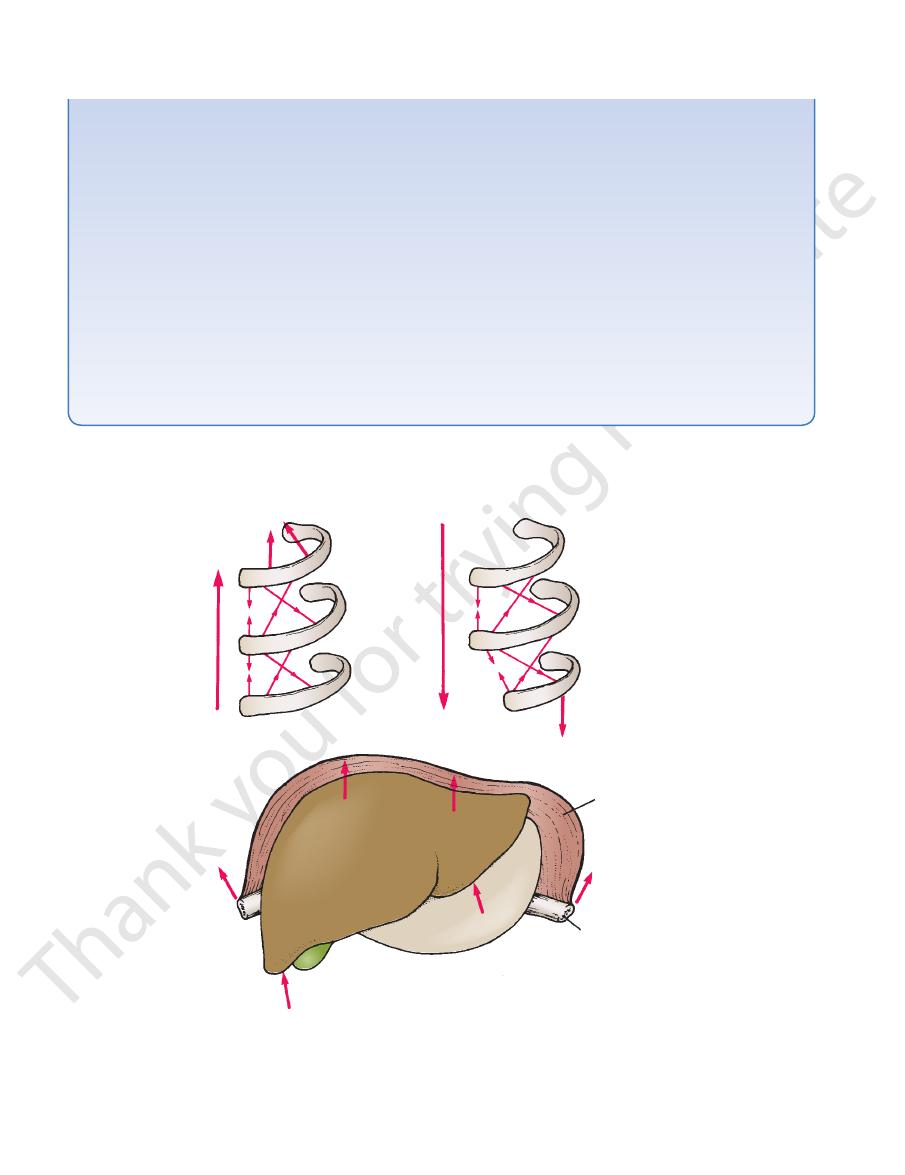
scalenus anterior
and medius muscles
intercostal
muscles
inspiration
forced
expiration
intercostal
muscles
quadratus lumborum
muscle
diaphragm
rib
liver
A
B
C
FIGURE 3.10
diaphragm to raise the lower ribs.
How the liver provides the platform that enables the
12th rib is fixed or is made to descend by the abdominal muscles.
How the intercostal muscles can be used in forced expiration, provided that the
or, in forced inspiration, raise the 1st rib.
How the intercostal muscles raise the ribs during inspiration. Note that the scaleni muscles fix the 1st rib
A.
B.
C.
Basic Anatomy
67
trachea
left principal bronchus
right principal
bronchus
right
upper
bronchus
left pulmonary
artery
pulmonary trunk
right
pulmonary
artery
FIGURE 3.11
Relationship of the pulmonary arteries to the
bronchial tree.
FIGURE 3.12
The bifurcation of the trachea as seen through
(Courtesy of E.D. Andersen.)
the right, which is a more direct continuation of the trachea.
the center and the opening into the right main bronchus on
an operating bronchoscope. Note the ridge of the carina in
FIGURE 3.13
The interior of the left main bronchus as seen
lobe bronchus are indicated. (Courtesy of E.D. Andersen.)
left upper lobe bronchus and its division and the left lower
through an operating bronchoscope. The openings into the
P
A
M
T
FIGURE 3.14
Position of the heart valves. P, pulmonary
least interference.
indicate position where valves may be heard with
Arrows
valve; A, aortic valve; M, mitral valve; T, tricuspid valve.
the lung. This is
y well seen in city dwellers and
especiall
dust particles that become trapped in the phagocytes of
become dark and mottled because of the inhalation of
volume. In the child, they are pink, but with age, they
lungs would immediately shrink to one third or less in
and very elastic. If the thoracic cavity were opened, the
During life, the right and left lungs are soft and spongy
only by its root (Fig. 3.4).
its own pleural cavity, being attached to the mediastinum
cal, covered with visceral pleura, and suspended free in
other structures in the mediastinum. Each lung is coni
rated from each other by the heart and great vessels and
each side of the mediastinum. They are therefore sepa
coal miners. The lungs are situated so that one lies on
-
-
Lungs
