
Basic Anatomy
ward to the superficial inguinal nodes (see Fig. 4.19).
the axilla; below the level of the iliac crests, it drains down
axillary group of nodes, palpated on the posterior wall of
level of the iliac crests is drained upward to the posterior
(Fig. 4.19). The lymph of the skin of the back above the
downward and laterally to the superficial inguinal nodes
muscle. Below the level of the umbilicus, the lymph drains
pated just beneath the lower border of the pectoralis major
rior axillary (pectoral) group of nodes, which can be pal
wall above the level of the umbilicus is upward to the ante
The lymph drainage of the skin of the anterior abdominal
Superficial Lymph Vessels
Lymph Drainage of the Anterior Abdominal Wall
127
-
-
-
inguinal node) caused by an infection or malignant tumor of
group of lymph nodes is clinically important. For example, it is
Skin and its Regional Lymph Nodes
Knowledge of the areas of the skin that drain into a particular
possible to find a swelling in the groin (enlarged superficial
the skin of the lower part of the anterior abdominal wall or that
of the buttock.
C L I N I C A L N O T E S
Deep Lymph Vessels
part of the posterior wall, namely, the deep inguinal ring.
therefore strongest where it lies opposite the weakest
inguinal ligament (see Figs. 4.3 and 4.8). This wall is
laterally by the origin of the internal oblique from the
External oblique aponeurosis, reinforced
Anterior wall.
Walls of the Inguinal Canal
external spermatic fascia.
give attachment to the
crura,
4.3, 4.5, and 4.8). The margins of the ring, sometimes called
immediately above and medial to the pubic tubercle (see Figs.
in the aponeurosis of the external oblique muscle and lies
is a triangular-shaped defect
superficial inguinal ring
The
the internal covering of the round ligament of the uterus).
(or
internal spermatic fascia
ring give attachment to the
upward from the external iliac vessels. The margins of the
it medially are the inferior epigastric vessels, which pass
and the symphysis pubis (see Figs. 4.4 and 4.8). Related to
ligament midway between the anterior superior iliac spine
transversalis, lies about 0.5 in. (1.3 cm) above the inguinal
* an oval opening in the fascia
deep inguinal ring,
The
Later, as the result of growth, the deep ring moves laterally.
ficial ring so that the canal is considerably shorter at this age.
child, the deep ring lies almost directly posterior to the super
immediately above the inguinal ligament. In the newborn
oblique muscle (see Figs. 4.3 and 4.8). It lies parallel to and
ficial inguinal ring, a hole in the aponeurosis of the external
versalis (see page 137), downward and medially to the super
extends from the deep inguinal ring, a hole in the fascia trans
The canal is about 1.5 in. (4 cm) long in the adult and
from the uterus to the labium majus.
females, it allows the round ligament of the uterus to pass
structures to pass to and from the testis to the abdomen. In
part of the anterior abdominal wall. In the males, it allows
The inguinal canal is an oblique passage through the lower
and para-aortic (lumbar) nodes.
the internal thoracic, external iliac, posterior mediastinal,
The deep lymph vessels follow the arteries and drain into
Inguinal Canal
-
-
-
*
the
caput medusae
anterior axillary lymph nodes
superficial inguinal nodes
posterior axillary lymph nodes
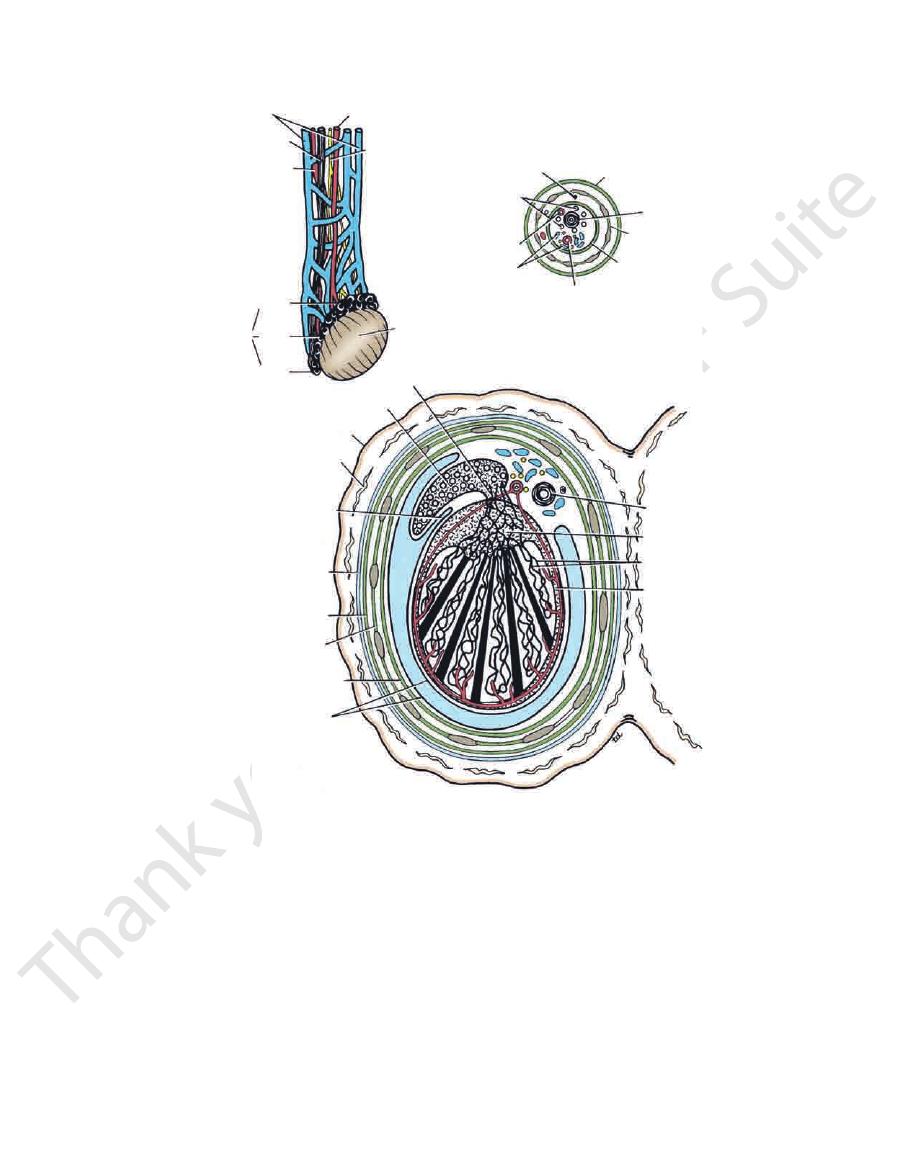
FIGURE 4.19
Lymph drainage of the skin of the anterior and posterior abdominal walls. Also shown is an example of caput
medusae in a case of portal obstruction caused by cirrhosis of the liver.
openings for the fingers when the glove is viewed from the outside.
with the openings for the fingers seen inside a glove with the absence of
edges of the rings cannot be observed externally. Compare this arrangement
fascia is attached to the margins of the superficial inguinal ring so that the
attached to the margins of the deep inguinal ring and the external spermatic
rings as openings. One must remember that the internal spermatic fascia is
*A common frustration for medical students is the inability to observe these

128
CHAPTeR 4
to lessen this weakness.
interesting to consider how the design of this canal attempts
inal wall is a site of potential weakness in both sexes. It is
The inguinal canal in the lower part of the anterior abdom
Mechanics of the Inguinal Canal
the labium majus.
sage of the round ligament of the uterus from the uterus to
scrotum.) In the female, the smaller canal permits the pas
the abdominal cavity to enter a cooler environment in the
(Normal spermatogenesis takes place only if the testis leaves
to pass to and from the testis to the abdomen in the male.
The inguinal canal allows structures of the spermatic cord
Function of the Inguinal Canal
(see Fig. 4.7).
nal ligament and, at its medial end, the lacunar ligament
Upturned lower edge of the ingui
Floor or inferior wall.
oblique and transversus abdominis muscles (see Fig. 4.7).
Arching lowest fibers of the internal
Roof or superior wall.
anterior wall, namely, the superficial inguinal ring.
strongest where it lies opposite the weakest part of the
salis laterally (see Figs. 4.4 and 4.8). This wall is therefore
Conjoint tendon medially, fascia transver
Posterior wall.
The Abdomen: Part I—The Abdominal Wall
-
-
-
-
1.
Except in the newborn infant, the canal is an oblique
and deep rings, lying some distance apart.
passage with the weakest areas, namely, the superficial
2.
The anterior wall of the canal is reinforced by the fibers
the deep ring.
of the internal oblique muscle immediately in front of
3.
The posterior wall of the canal is reinforced by the strong
conjoint tendon immediately behind the superficial ring.
4.
On coughing and straining, as in micturition, defeca
canal is virtually closed (Fig. 4.20).
the contents of the canal against the floor so that the
ered toward the floor. The roof may actually compress
contract, flattening out the arched roof so that it is low
internal oblique and transversus abdominis muscles
tion, and parturition, the arching lowest fibers of the
-
-
5.
When great straining efforts may be necessary, as in def
into the inferior vena cava on the right side.
wall and drains into the left renal vein on the left side and
vein is formed. This runs up on the posterior abdominal
about the level of the deep inguinal ring, a single testicular
the plexus ascends, it becomes reduced in size so that at
leaves the posterior border of the testis (see Fig. 4.21). As
pampiniform plexus,
An extensive venous plexus, the
Testicular Veins
(see Fig. 4.21).
the inguinal canal and supplies the testis and the epididymis
and descends on the posterior abdominal wall. It traverses
lumbar vertebra), the testicular artery is long and slender
A branch of the abdominal aorta (at the level of the 2nd
Testicular Artery
transports spermatozoa from the epididymis to the urethra.
part of the scrotum. It is a thick-walled muscular duct that
that can be palpated between finger and thumb in the upper
The vas deferens is a cordlike structure (see Figs. 4.5 and 4.21)
Vas Deferens (Ductus Deferens)
plies the cremaster muscle
Genital branch of the genitofemoral nerve, which sup
Remains of the processus vaginalis
Autonomic nerves
Testicular lymph vessels
Testicular veins (pampiniform plexus)
Testicular artery
Vas deferens
The structures are as follows:
Structures of the Spermatic Cord
inferior epigastric artery and ends at the testis.
(Fig. 4.21). It begins at the deep inguinal ring lateral to the
pass through the inguinal canal to and from the testis
The spermatic cord is a collection of structures that
the thighs (see Fig. 4.20).
lower part of the anterior abdominal wall is protected by
against the anterior abdominal wall. By this means, the
and the anterior surfaces of the thighs are brought up
assume the squatting position; the hip joints are flexed,
ecation and parturition, the person naturally tends to
-
Spermatic Cord
■
■
■
■
■
■
■
■
■
■
■
■
■
■
-
transversus
internal oblique
spermatic cord
conjoint
tendon
superficial
inguinal
ring
conjoint
tendon
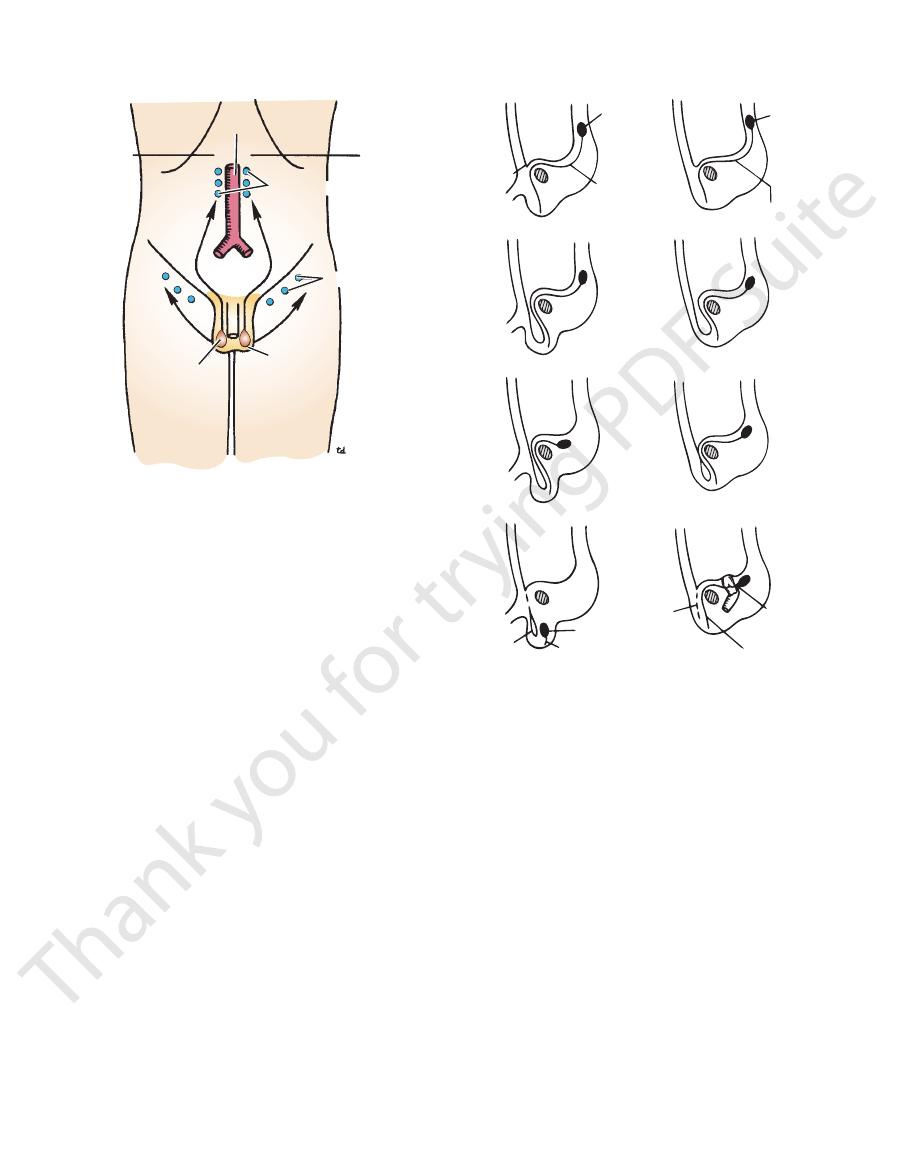
FIGURE 4.20
Action of the muscles on the inguinal canal.
contract. Note also that the anterior surface of the thigh
Note that the canal is “obliterated” when the muscles
protects the inguinal region when one assumes the squat-
ting position.
Basic Anatomy
superficial inguinal ring
oblique aponeurosis and attached to the margins of the
derived from the external
External spermatic fascia
the abdominal wall (Fig. 4.23).
vaginalis descends into the scrotum through the layers of
abdominal wall. Each covering is acquired as the processus
tric layers of fascia derived from the layers of the anterior
The coverings of the spermatic cord are three concen
Fasciae)
Coverings of the Spermatic Cord (the Spermatic
(see page 222).
This nerve supplies the cremaster muscle (see Fig. 4.21)
Genital Branch of the Genitofemoral Nerve
the cord (see below).
The remains of the processus vaginalis are present within
Processus Vaginalis
nerves accompany the efferent sympathetic fibers.
the renal or aortic sympathetic plexuses. Afferent sensory
Sympathetic fibers run with the testicular artery from
the aorta at the level of the 1st lumbar vertebra (Fig. 4.22).
reach the lumbar (para-aortic) lymph nodes on the side of
canal and pass up over the posterior abdominal wall to
The testicular lymph vessels ascend through the inguinal
Lymph Vessels
129
Autonomic Nerves
-
■
■
pampiniform plexus
vas deferens
artery of vas
posterior
head
body
tail
epididymis
testis
anterior
lymph vessels
testicular artery
genitofemoral nerve
lymph vessels
artery of vas
pampiniform plexus
internal spermatic fascia
cremasteric fascia
vas deferens
external spermatic fascia
efferent ductules
skin of scrotum
epididymis
dartos muscle
membranous layer of
superficial fascia
(Colles' fascia)
external
spermatic fascia
cremasteric fascia
internal spermatic fascia
tunica vaginalis
vas deferens
mediastinum testis
seminiferous tubules
tunica albuginea
testicular artery
sinus of epididymis
FIGURE 4.21
Testis and epididymis, spermatic cord, and scrotum. Also shown are the testis and epididymis cut across in
horizontal section.
130
CHAPTeR 4
(see Figs. 4.4 and 4.5). It is in this
external spermatic fascia
inguinal ring and acquires a third tubular fascial coat, the
the external oblique, it evaginates this to form the superficial
from this abdominal layer. On reaching the aponeurosis of
abdominis muscle and therefore does not acquire a covering
vaginalis passes under the arching fibers of the transversus
(see Fig. 4.4). The processus
cremasteric fascia
known as the
are embedded in fascia, and thus the second tubular sheath is
The muscle fibers
cremaster muscle.
fibers, which form the
internal oblique muscle, it takes with it some of its lowest
(see Fig. 4.4). As it passes through the lower part of the
internal spermatic fas
and acquires a tubular covering, the
It traverses the fascia transversalis at the deep inguinal ring
as it does so, acquires a tubular covering from each layer.
layers of the lower part of the anterior abdominal wall and,
(see Fig. 4.23). The processus vaginalis passes through the
is formed
processus vaginalis
toneal diverticulum called the
of origin high on the posterior abdominal wall (L1), a peri
Before the descent of the testis and the ovary from their site
Development of the Inguinal Canal
must first consider the development of the inguinal canal.
To understand the coverings of the spermatic cord, one
salis and attached to the margins of the deep inguinal ring
derived from the fascia transver
Internal spermatic fascia
muscle
derived from the internal oblique
Cremasteric fascia
The Abdomen: Part I—The Abdominal Wall
■
■
■
■
-
-
-
cia
manner that the
d in both sexes. (In
inguinal canal is forme
inguinal canal during the seventh and eighth months of fetal
In the male, the testis descends through the pelvis and
(see Fig. 4.23).
gubernaculum
canal to the labioscrotal swelling, has condensed to form
lower pole of the developing gonad through the inguinal
Meanwhile, a band of mesenchyme, extending from the
the covering of the round ligament of the uterus.)
the female, the term spermatic fascia should be replaced by
the
life. The normal stimulus for the descent of the testis is testos
in the female, the only structures that pass through the
Thus,
round ligament of the uterus.
majus persists as the
lum extending from the uterus into the developing labium
the gonad descends no farther. That part of the gubernacu
becomes attached to the side of the developing uterus, and
ing the gubernaculum (see Fig. 4.23). The gubernaculum
In the female, the ovary descends into the pelvis follow
cia, the cremasteric fascia, and the internal spermatic fascia.
by three concentric layers of fascia: the external spermatic fas
down the inguinal canal. Thus, the spermatic cord is covered
vaginalis, they acquire the same three coverings as they pass
so on, follow the course previously taken by the processus
Because the testis and its accompanying vessels, ducts, and
in the developing scrotum by the end of the eighth month.
nerves, and lymph vessels. The testis takes up its final position
the processus vaginalis and pulls down its duct, blood vessels,
the posterior abdominal wall. The testis then passes behind
the gubernaculum and descends behind the peritoneum on
terone, which is secreted by the fetal testes. The testis follows
-
-
-
-
aorta
lumbar lymph nodes
superficial inguinal
lymph nodes
scrotal skin
testis
transpyloric
plane
FIGURE 4.22
Lymph drainage of the testis and the skin of
the scrotum.
testis
processus
vaginalis
gubernaculum
ovary
gubernaculum
A
B
C
D
tunica
vaginalis
testis
remains of
gubernaculum
remains of
processus
vaginalis
round ligament
of uterus
round
ligament
of ovary
FIGURE 4.23
Origin, development, and fate of the processus
into the scrotum and the descent of the ovary into the pelvis.
vaginalis in the two sexes. Note the descent of the testis
Basic Anatomy
ent motor nerve fibers travel in the genital branch of
of the genitofemoral nerve (L1 and 2), and the effer
ent fibers of this reflex arc travel in the femoral branch
The affer
cremasteric reflex.
the thigh. This is called the
to contract by stroking the skin on the medial aspect of
nerve (see page 222). The cremaster muscle can be made
is supplied by the genital branch of the genitofemoral
from the fascia transversalis. The cremaster muscle
cle; and, finally, the internal spermatic fascia is derived
masteric fascia is derived from the internal oblique mus
the aponeurosis of the external oblique muscle; the cre
explained. The external spermatic fascia is derived from
anterior abdominal wall on each side, as previously
ficial fascia and are derived from the three layers of the
These three layers lie beneath the super
Spermatic fasciae.
and separates the testes from each other.
tribute to a median partition that crosses the scrotum
ischiopubic rami. Both layers of superficial fascia con
membrane (see Fig. 4.1). At the sides, it is attached to the
perineal body and the posterior edge of the perineal
wall (Scarpa’s fascia), and behind it is attached to the
with the membranous layer of the anterior abdominal
(often referred to as Colles’ fascia) is continuous in front
ing skin. The membranous layer of the superficial fascia
fibers and is responsible for the wrinkling of the overly
This is innervated by sympathetic nerve
dartos muscle.
fat is, however, replaced by smooth muscle called the
membranous layers of the anterior abdominal wall; the
This is continuous with the fatty and
Superficial fascia.
remain separate and form the labia majora.)
eral labioscrotal swellings. (In the female, the swellings
in the midline indicates the line of fusion of the two lat
mented and forms a single pouch. A slightly raised ridge
The skin of the scrotum is thin, wrinkled, and pig
Skin.
The wall of the scrotum has the following layers:
mides, and the lower ends of the spermatic cords (see Figs.
anterior abdominal wall. It contains the testes, the epididy
The scrotum is an outpouching of the lower part of the
Scrotum
Scrotum, Testis, and Epididymides
the uterus to the superficial inguinal nodes.
vessels convey a small amount of lymph from the body of
ligament of the uterus and a few lymph vessels. The lymph
inguinal canal from the abdominal cavity are the round
131
-
4.4 and 4.21).
-
-
-
-
-
-
-
-
-
the genitofemoral nerve. The function of the cremaster
cremaster muscles. It is now recognized that the testicular
be changed reflexly by the contraction of the dartos and
fully understood, but the surface area of the scrotal skin can
The control of testicular temperature in the scrotum is not
perature about 3°C lower than the abdominal temperature.
When they are located in the scrotum, they are at a tem
at a temperature lower than that of the abdominal cavity.
Normal spermatogenesis can occur only if the testes are
Fig. 4.21).
nect the rete testis to the upper end of the epididymis (see
con
efferent ductules
Small
rete testis.
channels called the
The tubules open into a network of
seminiferous tubules.
Lying within each lobule are one to three coiled
lobules.
of fibrous septa that divide the interior of the organ into
Extending from the inner surface of the capsule is a series
tunica albuginea.
fibrous capsule, the
level than the right. Each testis is surrounded by a tough
(see Figs. 4.5 and 4.21). The left testis usually lies at a lower
is a firm, mobile organ lying within the scrotum
testis
The
Testis
drains into the superficial inguinal lymph nodes (see Fig. 4.22).
Lymph from the skin and fascia, including the tunica vaginalis,
Lymph Drainage of the Scrotum
testis.
nalis is thus a closed sac, invaginated from behind by the
the processus and the peritoneal cavity. The tunica vagi
before birth, it becomes shut off from the upper part of
expanded part of the processus vaginalis; normally, just
medial, and lateral surfaces of each testis. It is the lower
within the spermatic fasciae and covers the anterior,
(see Figs. 4.4, 4.5, and 4.21). This lies
Tunica vaginalis
temperature and fertility, see below.
warmth and for protection against injury. For testicular
muscle is to raise the testis and the scrotum upward for
-
-
-
veins in the spermatic cord that form the pampiniform
plexus—together with the branches of the testicular
arteries, which lie close to the veins—probably assist in sta
stances to the seminal fluid to nourish the maturing sperm.
tion of fluid. Another function may be the addition of sub
mature. A main function of the epididymis is the absorp
storage space for the spermatozoa and allows them to
The long length of the duct of the epididymis provides
enters the spermatic cord.
which
vas deferens,
from the tail of the epididymis as the
long, embedded in connective tissue. The tube emerges
The epididymis is a much coiled tube nearly 20 ft (6 m)
(see Fig. 4.21).
sinus of the epididymis
the inner visceral layer of the tunica vaginalis and is called
between the testis and the epididymis, which is lined with
inferiorly. Laterally, a distinct groove lies
and a pointed
body,
head,
Fig. 4.21). It has an expanded upper end, the
testis, with the vas deferens lying on its medial side (see
is a firm structure lying posterior to the
epididymis
The
blood ascending to the abdomen within the veins.
arriving in the artery from the abdomen loses heat to the
heat exchange mechanism. By this means, the hot blood
bilizing the temperature of the testes by a countercurrent
-
Epididymis
a
tail
the
-
-
Vasectomy
postoperative ejaculations, but that is simply an emptying process.
between ligatures. Spermatozoa may be present in the first few
upper part of the scrotal wall, and the vas deferens is divided
infertility. Under local anesthesia, a small incision is made in the
Bilateral vasectomy is a simple operation performed to produce
Now only the secretions of the seminal vesicles and prostate con-
stitute the seminal fluid, which can be ejaculated as before.
C L I N I C A L N O T E S
