174
CHAPTER 5
The Abdomen: Part II—The Abdominal Cavity
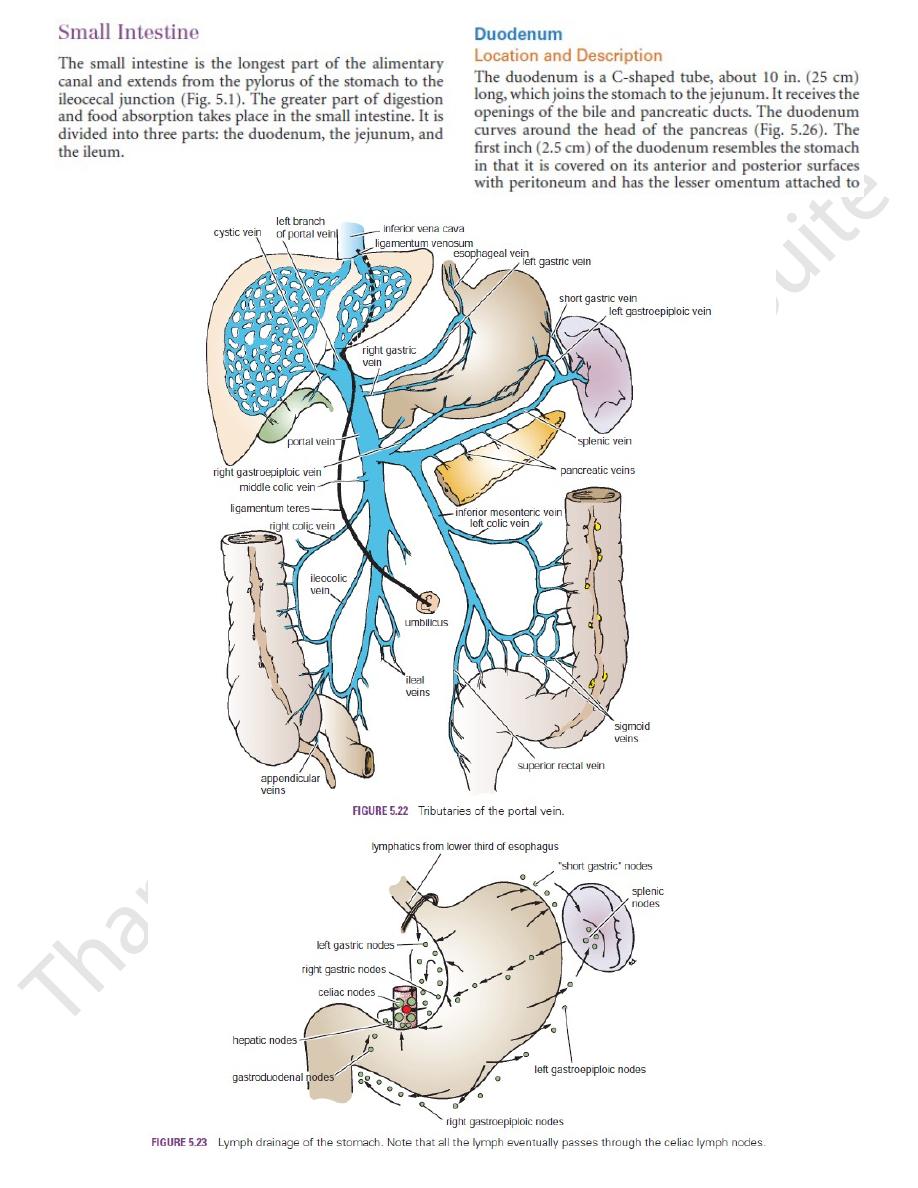
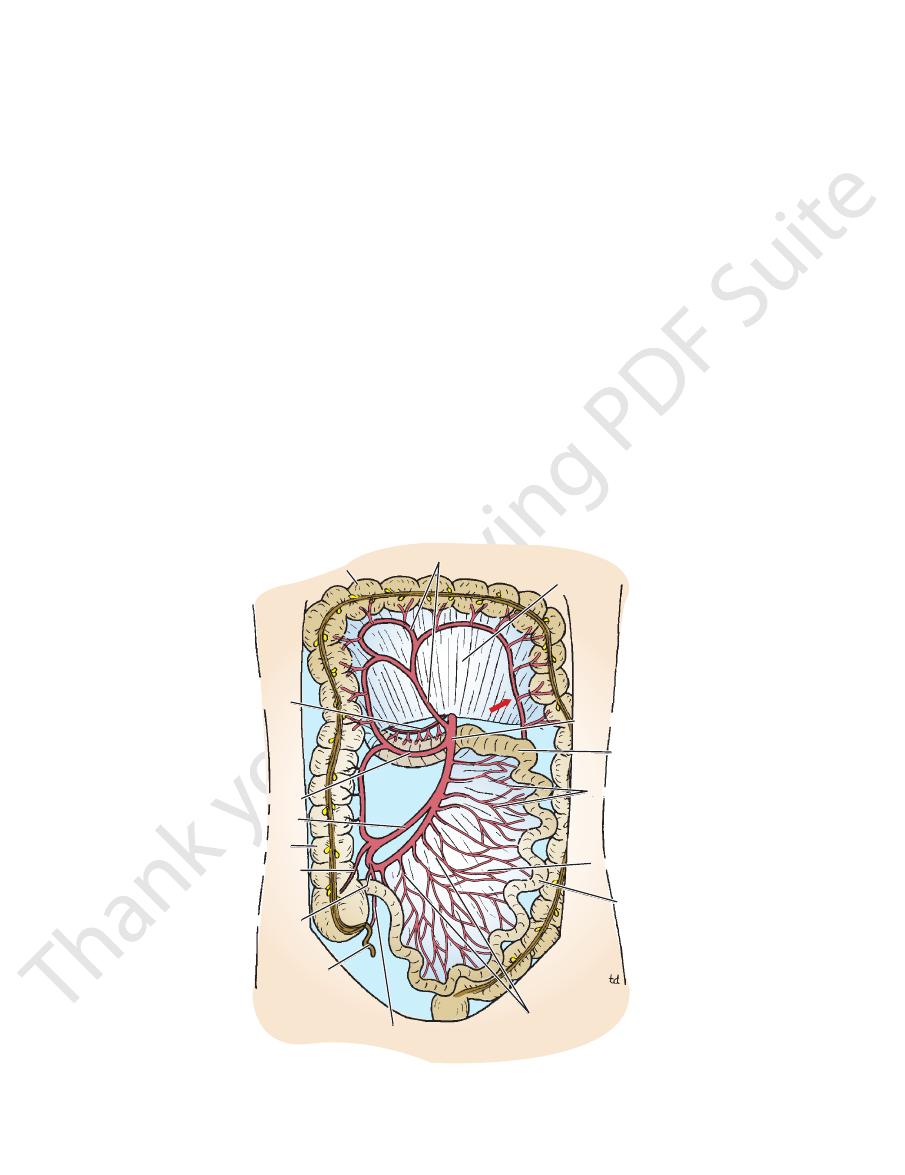
anterior vagal trunk
hepatic branch
pyloric branch
celiac branch
posterior vagal trunk
FIGURE 5.24
Distribution of the anterior and posterior vagal trunks within the abdomen. Note that the celiac branch of the
posterior vagal trunk is distributed with the sympathetic nerves as far down the intestinal tract as the left colic flexure.
Trauma to the Stomach
tric mucous membrane is possible. It is also possible to perform
Gastroscopy is the viewing of the mucous membrane of the
bloc and, with it, its lymphatic field. The continuity of the gut is
cal operation is a desperate attempt to remove the stomach en
the greater curvature, along with the greater omentum. This radi
along the lesser curvature of the stomach; and the nodes along
and body of the pancreas and their associated nodes; the nodes
and their associated lymph nodes; the splenic vessels; the tail
the spleen and the gastrosplenic and splenicorenal ligaments
lower end of the esophagus and the first part of the duodenum;
treated by total gastrectomy, which includes the removal of the
nodes. For these reasons, malignant disease of the stomach is
or bypass the local lymph nodes and are held up in the regional
away from the primary site. Cancer cells also often pass through
cer cells to travel to different parts of the stomach, some distance
Because the lymphatic vessels of the mucous membrane and
and is referred to the epigastrium. It is believed that the pain-
blunt trauma to the abdomen. However, its large size makes it
Apart from its attachment to the esophagus at the cardiac orifice
and its continuity with the duodenum at the pylorus, the stomach
is relatively mobile. It is protected on the left by the lower part
of the rib cage. These factors greatly protect the stomach from
vulnerable to gunshot wounds.
Gastric Ulcer
The mucous membrane of the body of the stomach and, to a
lesser extent, that of the fundus produce acid and pepsin. The
secretion of the antrum and pyloric canal is mucous and weakly
alkaline (Fig. 5.25). The secretion of acid and pepsin is controlled
by two mechanisms: nervous and hormonal. The vagus nerves
are responsible for the nervous control, and the hormone gas-
trin, produced by the antral mucosa, is responsible for the hor-
monal control. In the surgical treatment of chronic gastric and
duodenal ulcers, attempts are made to reduce the amount of
acid secretion by sectioning the vagus nerves (vagotomy) and by
removing the gastrin-bearing area of mucosa, the antrum (partial
gastrectomy).
Gastric ulcers occur in the alkaline-producing mucosa of the
stomach, usually on or close to the lesser curvature. A chronic
ulcer invades the muscular coats and, in time, involves the peri-
toneum so that the stomach adheres to neighboring structures.
An ulcer situated on the posterior wall of the stomach may per-
forate into the lesser sac or become adherent to the pancreas.
Erosion of the pancreas produces pain referred to the back. The
splenic artery runs along the upper border of the pancreas, and
erosion of this artery may produce fatal hemorrhage. A penetrat-
ing ulcer of the anterior stomach wall may result in the escape
of stomach contents into the greater sac, producing diffuse peri-
tonitis. The anterior stomach wall may, however, adhere to the
liver, and the chronic ulcer may penetrate the liver substance.
Gastric Pain
The sensation of pain in the stomach is caused by the stretch-
ing or spasmodic contraction of the smooth muscle in its walls
transmitting fibers leave the stomach in company with the sym-
pathetic nerves. They pass through the celiac ganglia and reach
the spinal cord via the greater splanchnic nerves.
Cancer of the Stomach
submucosa of the stomach are in continuity, it is possible for can-
-
restored by anastomosing the esophagus with the jejunum.
Gastroscopy
stomach through an illuminated tube fitted with a lens system.
The patient is anesthetized, and the gastroscope is passed into
the stomach, which is then inflated with air. With a flexible fiber-
optic instrument, direct visualization of different parts of the gas-
a mucosal biopsy through a gastroscope.
(continued)
C L I N I C A L N O T E S

Basic Anatomy
175
Nasogastric Intubation
Nasogastric intubation is a common procedure and is performed
to empty the stomach, to decompress the stomach in cases of
intestinal obstruction, or before operations on the gastrointesti-
nal tract; it may also be performed to obtain a sample of gastric
juice for biochemical analysis.
1.
The patient is placed in the semiupright position or left lateral
position to avoid aspiration.
2.
The well-lubricated tube is inserted through the wider nostril
and is directed backward along the nasal floor.
3.
Once the tube has passed the soft palate and entered the oral
pharynx, decreased resistance is felt, and the conscious pa-
tient will feel like gagging.
4.
Some important distances in the adult may be useful. From
The root of the mesentery of the small intes
Anteriorly:
The relations of this part are as follows:
ing the lower margin of the head of the pancreas (Figs. 5.26
plane, passing in front of the vertebral column and follow
duodenum runs horizontally to the left on the subcostal
The third part of the
Third Part of the Duodenum
the main pancreatic duct (Figs. 5.27 and 5.28)
The head of the pancreas, the bile duct, and
Medially:
and the right lobe of the liver (Fig. 5.27)
The ascending colon, the right colic flexure,
Laterally:
ureter (Fig. 5.27)
The hilum of the right kidney and the right
Posteriorly:
small intestine (Fig. 5.29)
lobe of the liver, the transverse colon, and the coils of the
The fundus of the gallbladder and the right
Anteriorly:
The relations of this part are as follows:
nal papilla (Figs. 5.27 and 5.28).
into the duodenum a little higher up on the minor duode
(Fig. 5.28). The accessory pancreatic duct, if present, opens
that opens on the summit of the major duodenal papilla
pierce the duodenal wall. They unite to form the ampulla
medial border, the bile duct and the main pancreatic duct
bar vertebrae (Figs. 5.26 and 5.27). About halfway down its
the right kidney on the right side of the 2nd and 3rd lum
denum runs vertically downward in front of the hilum of
The second part of the duo
Second Part of the Duodenum
The head of the pancreas (Fig. 5.26)
Inferiorly:
loic foramen) (Figs. 5.7 and 5.11)
The entrance into the lesser sac (the epip
Superiorly:
the inferior vena cava (Fig. 5.27)
troduodenal artery, the bile duct and the portal vein, and
The lesser sac (first inch only), the gas
Posteriorly:
bladder (Fig. 5.10)
The quadrate lobe of the liver and the gall
Anteriorly:
The relations of this part are as follows:
tebra (Figs. 5.26 and 5.27).
on the transpyloric plane at the level of the 1st lumbar ver
num begins at the pylorus and runs upward and backward
The first part of the duode
First Part of the Duodenum
four parts.
regions and, for purposes of description, is divided into
The duodenum is situated in the epigastric and umbilical
Parts of the Duodenum
only partially covered by peritoneum.
The remainder of the duodenum is retroperitoneal, being
lower border; the lesser sac lies behind this short segment.
its upper border and the greater omentum attached to its
neuver opens the normally collapsed esophagus and permits
the esophagus (11.2 in. [28 cm]), and where the esophagus
curved course taken by the tube from the cardiac orifice to
the nostril (external nares) to the cardiac orifice of the stom-
ach is about 17.2 in. (44 cm), and from the cardiac orifice to
the pylorus of the stomach is 4.8 to 5.6 in. (12 to 14 cm). The
the pylorus is usually longer, 6.0 to 10.0 in. (15 to 25 cm) (see
Fig. 3.51).
Anatomic Structures That May Impede the Passage
of the Nasogastric Tube
■
■
A deviated nasal septum makes the passage of the tube
difficult on the narrower side.
■
■
Three sites of esophageal narrowing may offer resistance
to the nasogastric tube—at the beginning of the esopha-
gus behind the cricoid cartilage (7.2 in. [18 cm]), where the
left bronchus and the arch of the aorta cross the front of
enters the stomach (17.2 in. [44 cm]). The upper esophageal
narrowing may be overcome by gently grasping the wings of
the thyroid cartilage and pulling the larynx forward. This ma-
the tube to pass down without further delay.
Anatomy of Complications
■
■
The nasogastric tube enters the larynx instead of the esopha-
gus.
■
■
Rough insertion of the tube into the nose will cause nasal
bleeding from the mucous membrane.
■
■
Penetration of the wall of the esophagus or stomach. Always
aspirate tube for gastric contents to confirm successful
entrance into the stomach.
-
-
■
■
-
■
■
-
■
■
-
■
■
-
-
-
■
■
■
■
■
■
■
■
-
and 5.27).
■
■
-
and coils of jejunum (Figs. 5.26 and 5.27)
tine, the superior mesenteric vessels contained within it,
FIGURE 5.25
Areas of the stomach that produce acid and
pepsin (blue) and alkali and gastrin (red).
176
CHAPTER 5
and coils of jejunum (Fig. 5.30)
The beginning of the root of the mesentery
Anteriorly:
The relations of this part are as follows:
attached to the right crus of the diaphragm (Fig. 5.12).
which is
ligament of Treitz,
tion by a peritoneal fold, the
(Figs. 5.26 and 5.27). The flexure is held in posi
flexure
duodenojejunal
denum runs upward and to the left to the
The fourth part of the duo
Fourth Part of the Duodenum
Coils of jejunum
Inferiorly:
The head of the pancreas (Fig. 5.26)
Superiorly:
inferior vena cava, and the aorta (Fig. 5.27)
The right ureter, the right psoas muscle, the
Posteriorly:
The Abdomen: Part II—The Abdominal Cavity
■
■
■
■
■
■
-
-
■
■
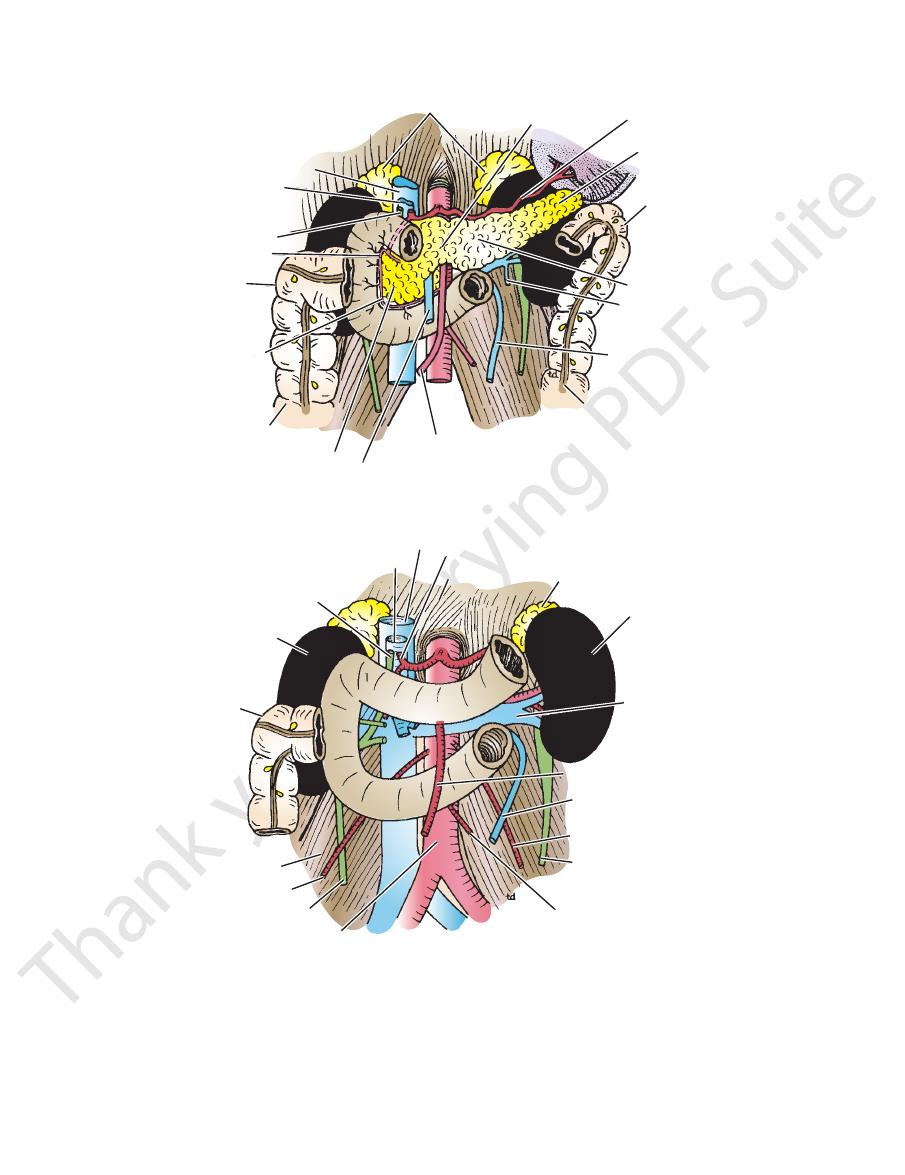
inferior vena cava
portal vein
bile duct
superior
pancreaticoduodenal
artery
right colic
flexure
inferior
pancreaticoduodenal
artery
ascending colon
head of pancreas
superior mesenteric vein
superior mesenteric artery
descending colon
inferior mesenteric vein
left testicular vein
body of pancreas
left colic flexure
tail of pancreas
splenic artery
neck of pancreas
suprarenal glands
FIGURE 5.26
Pancreas and anterior relations of the kidneys.
inferior vena cava
portal vein
bile duct
right kidney
right
colic flexure
psoas muscle
right testicular artery
right ureter
abdominal aorta
inferior mesenteric artery
left ureter
left testicular artery
inferior mesenteric vein
left renal vein
left kidney
suprarenal gland
diaphragm
hepatic artery
superior mesenteric artery
1
2
3
4
FIGURE 5.27
Posterior relations of the duodenum and the pancreas. The numbers represent the four parts of the duodenum.

Basic Anatomy
der of the duodenum, it is thrown into numerous circular
part of the duodenum, it is smooth (Fig. 5.28). In the remain
of the duodenum is thick. In the first
mucous membrane
The
Mucous Membrane and Duodenal Papillae
border of the left psoas muscle (Fig. 5.27)
The left margin of the aorta and the medial
Posteriorly:
177
■
■
-
superior
mesenteric
artery
ileocecal
junction
duodenojejunal
flexure
root of mesentery
of small intestine
FIGURE 5.30
Attachment of the root of the mesentery of the
mesentery of the small
fold of peritoneum known as the
attached to the posterior abdominal wall by a fan-shaped
The coils of jejunum and ileum are freely mobile and are
flexure, and the ileum ends at the ileocecal junction.
one to the other. The jejunum begins at the duodenojejunal
has distinctive features, but there is a gradual change from
upper two fifths of this length make up the jejunum. Each
The jejunum and ileum measure about 20 ft (6 m) long; the
Location and Description
Jejunum and Ileum
teric plexuses.
thetic (vagus) nerves from the celiac and superior mesen
The nerves are derived from sympathetic and parasympa
the origin of the superior mesenteric artery.
coduodenal nodes to the superior mesenteric nodes around
and then to the celiac nodes and downward via pancreati
pancreaticoduodenal nodes to the gastroduodenal nodes
The lymph vessels follow the arteries and drain upward via
Lymph Drainage
mesenteric vein (Fig. 5.22).
into the portal vein; the inferior vein joins the superior
The superior pancreaticoduodenal vein drains
Veins
superior mesenteric artery.
the inferior pancreaticoduodenal artery, a branch of the
artery (Figs. 5.20 and 5.26). The lower half is supplied by
creaticoduodenal artery, a branch of the gastroduodenal
The upper half is supplied by the superior pan
Arteries
about 0.75 in. (1.9 cm) above the major duodenal papilla.
if present, opens into the duodenum on a smaller papilla
(Fig. 5.28). The accessory pancreatic duct,
duodenal papilla
major
the second part is a small, rounded elevation called the
duct and the main pancreatic duct pierce the medial wall of
At the site where the bile
plicae circulares.
folds called the
superior mesenteric artery lies in the root of the mesentery.
downward, and to the right to the ileocecal junction. The
extends from the duodenojejunal flexure on left of the aorta,
small intestine to the posterior abdominal wall. Note that it
Blood Supply
-
-
Nerve Supply
-
-
smooth mucous membrane
plicae
circulares
major
duodenal papilla
bile duct
accessory pancreatic
duct
main pancreatic
duct
FIGURE 5.28
Entrance of the bile duct and the main and
accessory pancreatic ducts into the second part of the
duodenum. Note the smooth lining of the first part of the
duodenum, the plicae circulares of the second part, and the
major duodenal papilla.
left hepatic duct
portal vein
lesser omentum
hepatic artery
accessory pancreatic
duct
main pancreatic duct
transverse colon
second part of
duodenum
right hepatic duct
common hepatic duct
cystic duct
bile duct
neck
fundus
gallbladder
body
FIGURE 5.29
The bile ducts and the gallbladder. Note the
relation of the gallbladder to the transverse colon and the
duodenum.
178
CHAPTER 5
ileum by the following features:
In the living, the jejunum can be distinguished from the
mesentery.
the space between the two layers of peritoneum forming the
mesenteric artery and vein, lymph vessels, and nerves into
permits the entrance and exit of the branches of the superior
region of the right sacroiliac joint. The root of the mesentery
right from the left side of the 2nd lumbar vertebra to the
nal wall along a line that extends downward and to the
ous with the parietal peritoneum on the posterior abdomi
the mobile intestine. The short root of the fold is continu
(Fig. 5.30). The long free edge of the fold encloses
intestine
The Abdomen: Part II—The Abdominal Cavity
-
-
Trauma to the Duodenum
gallbladder wall into the duodenum. Operations on the colon and
been reported in which a large gallstone ulcerated through the
colon, and the right kidney should be remembered. Cases have
The relation to the duodenum of the gallbladder, the transverse
The importance of the duodenal recesses and the occurrence of
ferential diagnosis between a perforated duodenal ulcer and a
paracolic gutter and thus down to the right iliac fossa. The dif
transverse colon directs the escaping fluid into the right lateral
upper part of the greater sac, above the transverse colon. The
rior wall of the first inch of the duodenum may perforate into the
production of a duodenal ulcer at this site. An ulcer of the ante
of the duodenum. This is thought to be an important factor in the
chyme is squirted against the anterolateral wall of the first part
As the stomach empties its contents into the duodenum, the acid
away from crush injuries. In severe crush injuries to the anterior
terior abdominal wall by peritoneum and therefore cannot move
Apart from the first inch, the duodenum is rigidly fixed to the pos-
abdominal wall, the third part of the duodenum may be severely
crushed or torn against the third lumbar vertebra.
Duodenal Ulcer
-
-
perforated appendix may be difficult.
An ulcer of the posterior wall of the first part of the duodenum
may penetrate the wall and erode the relatively large gastroduo-
denal artery, causing a severe hemorrhage.
The gastroduodenal artery is a branch of the hepatic artery, a
branch of the celiac trunk (Fig. 5.4).
Duodenal Recesses
herniae of the intestine were already alluded to on page 163.
Important Duodenal Relations
right kidney have resulted in damage to the duodenum.
C L I N I C A L N O T E S
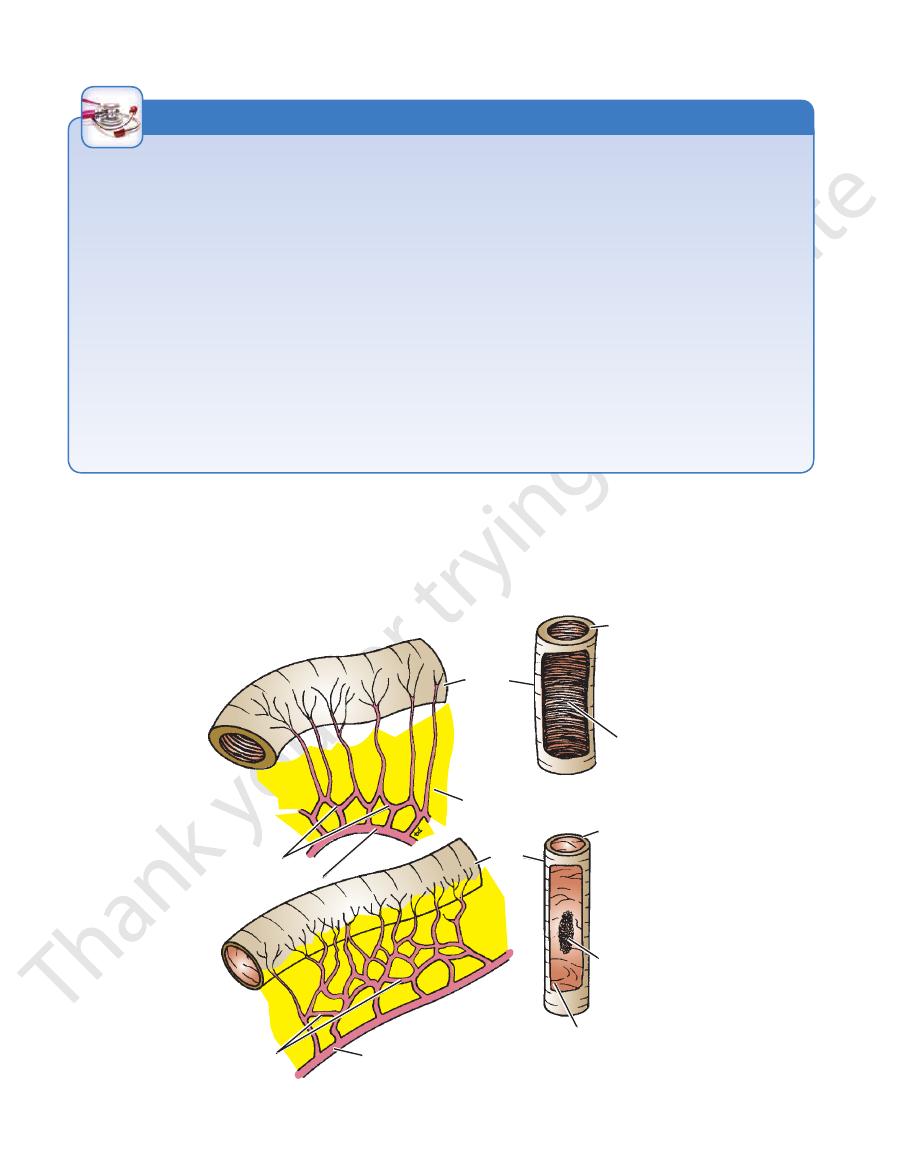
arterial arcades
superior mesenteric artery
fat
thick wall
plicae circulares
arterial arcades
superior mesenteric artery
ileum
thin wall
Peyer's patch
smooth mucous membrane
jejunum
FIGURE 5.31
Some external and internal differences between the jejunum and the ileum.
Basic Anatomy
pathetic (vagus) nerves from the superior mesenteric plexus.
The nerves are derived from the sympathetic and parasym
enteric artery.
which are situated around the origin of the superior mes
teric nodes and finally reach the superior mesenteric nodes,
The lymph vessels pass through many intermediate mesen
Lymph Drainage
teric vein (Fig. 5.22).
rior mesenteric artery and drain into the superior mesen
The veins correspond to the branches of the supe
Veins
supplied by the ileocolic artery.
form a series of arcades. The lowest part of the ileum is also
tery to reach the gut. They anastomose with one another to
arise from the left side of the artery and run in the mesen
rior mesenteric artery (Fig. 5.32). The intestinal branches
The arterial supply is from branches of the supe
Arteries
from the outside.
ing, these may be visible through the wall of the ileum
along the antimesenteric border (Fig. 5.31). In the liv
present in the mucous membrane of the lower ileum
Aggregations of lymphoid tissue (Peyer’s patches) are
(Fig. 5.31).
out so that it extends from the root to the intestinal wall
ileal end of the mesentery, the fat is deposited through
near the root and is scanty near the intestinal wall. At the
At the jejunal end of the mesentery, the fat is deposited
or even more arcades (Fig. 5.31).
terminal vessels that arise from a series of three or four
the intestinal wall. The ileum receives numerous short
arcades, with long and infrequent branches passing to
The jejunal mesenteric vessels form only one or two
right of the aorta.
whereas the ileal mesentery is attached below and to the
abdominal wall above and to the left of the aorta,
The jejunal mesentery is attached to the posterior
lower part they are absent (Fig. 5.31).
they are smaller and more widely separated and in the
in the jejunum, whereas in the upper part of the ileum
cae circulares, are larger, more numerous, and closely set
permanent infoldings of the mucous membrane, the pli
than the ileum. The jejunal wall feels thicker because the
The jejunum is wider bored, thicker walled, and redder
pelvis (Fig. 5.3).
lon; the ileum is in the lower part of the cavity and in the
neal cavity below the left side of the transverse mesoco
The jejunum lies coiled in the upper part of the perito
179
■
■
-
-
■
■
-
■
■
■
■
■
■
-
■
■
-
Blood Supply
-
-
-
-
-
-
Nerve Supply
-
transverse colon
inferior
pancreaticoduodenal
artery
right colic artery
ileocolic artery
ascending colon
anterior cecal artery
posterior cecal artery
appendix
appendicular artery
ileal arteries
ileum
arterial arcades
jejunal arteries
jejunum
superior mesenteric artery
transverse mesocolon
middle colic artery
FIGURE 5.32
ay down
Superior mesenteric artery and its branches. Note that this artery supplies blood to the gut from halfw
arrow
the second part of the duodenum to the distal third of the transverse colon (
).
