Basic Anatomy
285
The Uterine Tube as a Conduit for Infection
the uterine cavity in the wall of the uterine tube (Fig. 7.26). This
may follow, with leakage of pus into the peritoneal
tact and ascend through the uterus and enter the uterine tubes.
The uterine tube lies in the upper free border of the broad liga-
ment and is a direct route of communication from the vulva
through the vagina and uterine cavity to the peritoneal cavity.
Pelvic Inflammatory Disease
The pathogenic organism(s) enter the body through sexual con-
Salpingitis
cavity, causing pelvic peritonitis. A pelvic abscess usually fol-
lows, or the infection spreads farther, causing general peritonitis.
Ectopic Pregnancy
Implantation and growth of a fertilized ovum may occur outside
is a variety of ectopic pregnancy. There being no decidua for-
mation in the tube, the eroding action of the trophoblast quickly
destroys the wall of the tube. Tubal abortion or rupture of the
tube, with the effusion of a large quantity of blood into the
peritoneal cavity, is the common result.
ascend into the general peritoneal cavity, giving rise to severe
The blood pours down into the rectouterine pouch (pouch of
Douglas) or into the uterovesical pouch. The blood may quickly
abdominal pain, tenderness, and guarding. Irritation of the subdi-
aphragmatic peritoneum (supplied by phrenic nerves C3, 4, and 5)
ovarian follicles degenerate in the tube proximal to the obstruc
may give rise to referred pain to the shoulder skin (supraclavicu-
lar nerves C3 and 4).
Tubal Ligation
Ligation and division of the uterine tubes is a method of obtain-
ing permanent birth control and is usually restricted to women
who already have children. The ova that are discharged from the
-
tion. If, later, the woman wishes to have an additional child, res-
toration of the continuity of the uterine tubes can be attempted,
and, in about 20% of women, fertilization occurs.
C L I N I C A L N O T E S
Development of the Uterine Tube
coiled; differentiation of the muscle and mucous membrane
on the posterior abdominal wall on the lateral side of the
Early on in development, the paramesonephric ducts appear
mesonephros. The uterine tube on each side is formed from
the cranial vertical and middle horizontal parts of the parame-
sonephric duct (Fig. 7.27). The tube elongates and becomes
takes place; the fimbriae develop; and the infundibulum,
ampulla, and isthmus are identifiable.
E M B R Y O L O G I C N O T E S
(8 cm) long, 2 in. (5 cm) wide, and 1 in. (2.5 cm) thick. It
below the level of the internal os, where the peritoneum
The uterus is covered with peritoneum except anteriorly,
Structure of the Uterus
retroflexed.
is, in addition, bent backward on the cervix, it is said to be
If the body of the uterus
retroverted.
uterus is said to be
touterine pouch (pouch of Douglas). In this situation, the
bent backward on the vagina so that they lie in the rec
In some women, the fundus and body of the uterus are
uterus lies in an almost horizontal plane.
Thus, in the erect position and with the bladder empty, the
(see Fig. 7.25).
anteflexion of the uterus
position is termed
level of the internal os with the long axis of the cervix. This
the long axis of the body of the uterus is bent forward at the
(see Fig. 7.25). Furthermore,
anteversion of the uterus
on the long axis of the vagina. This position is referred to
In most women, the long axis of the uterus is bent forward
Positions of the Uterus
nutrition of the fertilized ovum.
The uterus serves as a site for the reception, retention, and
Function
are attached to the uterine wall just below this level.
and the round ligaments of the ovary and of the uterus
ine tubes enter the superolateral angles of the uterus,
vix is related to the lateral fornix of the vagina. The uter
as it passes forward to enter the bladder. The vaginal cer
Fig. 7.19). The supravaginal cervix is related to the ureter
the broad ligament and the uterine artery and vein (see
The body of the uterus is related laterally to
Laterally:
of ileum or sigmoid colon within it (see Fig. 7.5).
to the rectouterine pouch (pouch of Douglas) with coils
The body of the uterus is related posteriorly
Posteriorly:
is related to the anterior fornix of the vagina.
to the superior surface of the bladder. The vaginal cervix
bladder (see Fig. 7.5). The supravaginal cervix is related
to the uterovesical pouch and the superior surface of the
The body of the uterus is related anteriorly
Anteriorly:
Relations
an anterior lip and a posterior lip (see Fig. 7.25).
the external os becomes a transverse slit so that it possesses
parous woman, the vaginal part of the cervix is larger, and
the birth of the first child, the external os is circular. In a
Before
external os.
and with that of the vagina through the
internal os
nicates with the cavity of the body through the
commu
cervical canal,
7.25). The cavity of the cervix, the
section, but it is merely a cleft in the sagittal plane (see Fig.
of the uterine body is triangular in coronal
cavity
The
vaginal parts of the cervix.
aginal
suprav
anterior wall of the vagina and is divided into the
is the narrow part of the uterus. It pierces the
cervix
The
entrance of the uterine tubes.
is the part of the uterus that lies below the
body
The
entrance of the uterine tubes.
is the part of the uterus that lies above the
fundus
The
is divided into the fundus, body, and cervix (see Fig. 7.25).
-
and
-
■
■
■
■
■
■
-
-
as
-
286
CHAPTER 7
The Pelvis: Part II—The Pelvic Cavity
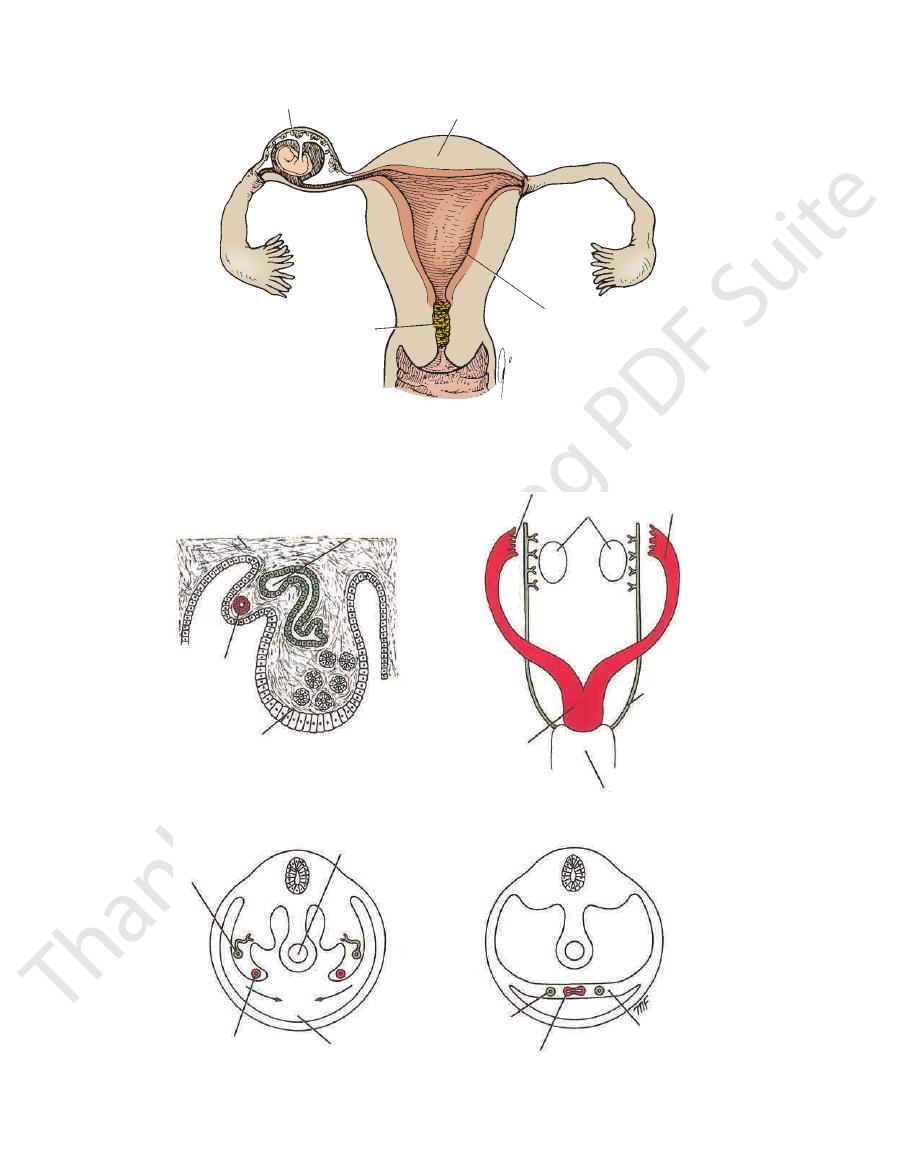
thin-walled uterine tube
fundus of uterus
thick decidua lining
body of uterus
mucous plug
FIGURE 7.26
An ectopic pregnancy located where the ampulla of the uterine tube narrows down to join the isthmus. Note
the thin tubal wall compared to the thick decidua that lines the body of the uterus.
posterior abdominal wall
mesonephric duct
paramesonephric duct
developing ovary
ostium
paramesonephric duct
developing ovaries
vertical
horizontal
vertical
fused lower ends of
paramesonephric ducts
mesonephric duct
urogenital sinus
mesonephric duct
paramesonephric duct
gut
pelvic cavity
mesonephric duct
fused paramesonephric ducts
broad ligament
A
B
C
D
FIGURE 7.27
The relationship of the mesonephric and paramesonephric ducts to the developing ovary.
of the pelvis. Note the developing broad ligament.
Anterior view of ovaries and ducts.
developing ovary.
A. Cross section of a
B.
C and D. Mesonephric and paramesonephric ducts in a cross section
Basic Anatomy
descending branch that supplies the cervix and the vagina.
in supplying the uterus. The uterine artery gives off a small
by anastomosing with the ovarian artery, which also assists
margin of the uterus within the broad ligament and ends
(see Fig. 7.25). The artery then ascends along the lateral
angles and reaches the cervix at the level of the internal os
ligament (see Fig. 7.19). It crosses above the ureter at right
the uterus by running medially in the base of the broad
ine artery, a branch of the internal iliac artery. It reaches
The arterial supply to the uterus is mainly from the uter
Arteries
on each side of the cervix.
It is in this fascia that the uterine artery crosses the ureter
parametrium.
ceral pelvic fascia, which is referred to as the
The supravaginal part of the cervix is surrounded by vis
cycle in response to the ovarian hormones.
trium undergoes extensive changes during the menstrual
submucosa. From puberty to menopause, the endome
metrium is applied directly to the muscle, there being no
with the mucous membrane lining the cervix. The endo
the mucous membrane lining the uterine tubes and below
It is continuous above with
endometrium.
known as the
lining the body of the uterus is
mucous membrane
The
up of smooth muscle supported by connective tissue.
is thick and made
myometrium,
or
muscular wall,
The
ligament.
space between the attachment of the layers of the broad
passes forward onto the bladder. Laterally, there is also a
the cervix of the uterus by the pelvic fascia (Fig. 7.28).
the anterior parts of the levatores ani muscles are attached to
mitted downward through the pelvis. The medial edges of
pelvic viscera and resist the intra-abdominal pressure trans
vic fascia on their upper surface, they effectively support the
stretching across the pelvic cavity, and, together with the pel
described in Chapter 6. They form a broad muscular sheet
The origin and the insertion of the levatores ani muscles are
The Levatores Ani Muscles and the Perineal Body
form three important ligaments.
ani muscles and the condensations of pelvic fascia, which
The uterus is supported mainly by the tone of the levatores
Supports of the Uterus
the inferior hypogastric plexuses.
Sympathetic and parasympathetic nerves from branches of
Nerve Supply
into the superficial inguinal lymph nodes.
ligament of the uterus through the inguinal canal and drain
nal iliac lymph nodes. A few lymph vessels follow the round
from the body and cervix drain into the internal and exter
nodes at the level of the first lumbar vertebra. The vessels
pany the ovarian artery and drain into the para-aortic
The lymph vessels from the fundus of the uterus accom
Lymph Drainage
internal iliac vein.
The uterine vein follows the artery and drains into the
Veins
287
-
-
-
-
-
-
-
Blood Supply
-
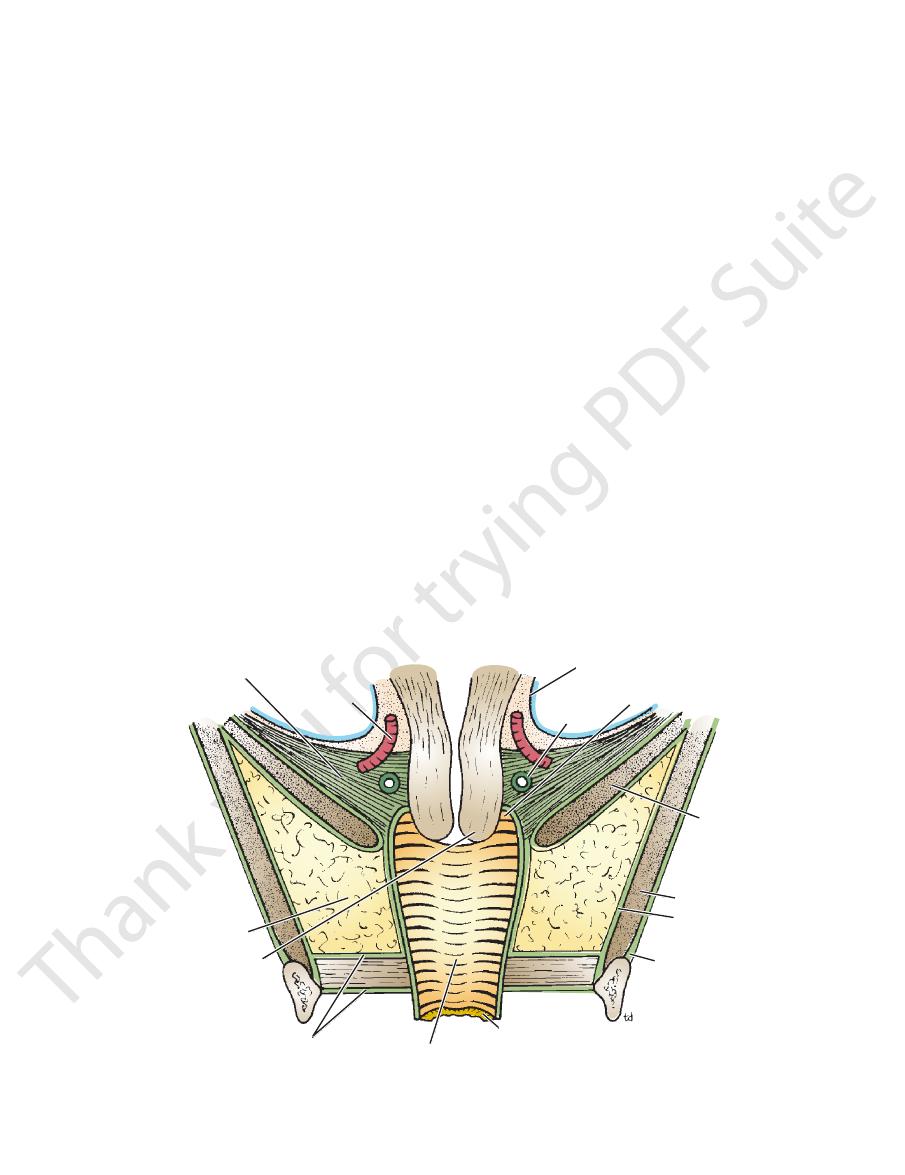
transverse cervical ligament
uterine artery
peritoneum
ureter
lateral fornix
levator ani
obturator internus
fascia of
obturator internus
obturator membrane
hymen
vagina
urogenital diaphragm
cervix
pelvic fascia
FIGURE 7.28
erse cervical liga
Coronal section of the pelvis showing relation of the levatores ani muscles and the transv
pelvic fascia.
ments to the uterus and vagina. Note that the transverse cervical ligaments are formed from a condensation of visceral
-

288
CHAPTER 7
Some of the fibers of levator ani are inserted into a
premature parturition.
tions. Severe emotional disturbance, however, can cause
thesia does not interfere with the normal uterine contrac
the extrinsic innervation. In women in labor, spinal anes
The uterine muscular activity is largely independent of
the force of the contractions of the uterine body.
that a nervous reflex mechanism is initiated and increases
ally the fetal head) starts to stretch the cervix, it is thought
withdrawal of progesterone. Once the presenting part (usu
is possible that the onset of labor is triggered by the sudden
ticularly sensitive to the actions of oxytocin at this time. It
been fully developed in response to estrogen, and it is par
By the end of pregnancy, the contractility of the uterus has
The cause of the onset of labor is not definitely known.
term.
time the pregnancy is said to be at
takes place at the end of the 10th lunar month, at which
from the genital tract of the mother. Normally, this process
baby, the fetal membranes, and the placenta are expelled
Labor, or parturition, is the series of processes by which the
Role of the Uterus in Labor
of the myometrium, although some hyperplasia takes place.
is largely a result of hypertrophy of the smooth muscle fibers
month it has reached the xiphoid process. The increase in size
month the fundus rises out of the pelvis, and by the ninth
placenta. At first, it remains as a pelvic organ, but by the third
terone, first by the corpus luteum of the ovary and later by the
result of the increasing production of estrogens and proges
During pregnancy, the uterus becomes greatly enlarged as a
Uterus in Pregnancy
no longer produce estrogens and progesterone.
and less vascular. These changes occur because the ovaries
After menopause, the uterus atrophies and becomes smaller
Uterus after Menopause
gens secreted by the ovaries.
puberty, when they enlarge greatly in response to the estro
The fundus and body of the uterus remain small until
Uterus in the Child
during pregnancy.
anteflexed (bent forward) but is considerably stretched
The Pelvis: Part II—The Pelvic Cavity
-
-
-
-
-
-
fibromuscular structure called the
(see
perineal body
Fig. 7.5). This structure is important in maintaining the
helps keep the uterus anteverted (tilted forward) and
cutaneous tissue of the labium majus (see Fig. 7.18). It
the deep inguinal ring and inguinal canal, to the sub
between the superolateral angle of the uterus, through
remains of the lower half of the gubernaculum, extends
which represents the
round ligament of the uterus,
The
role in supporting the uterus.
become taut. Clinically, they are considered to play a minor
or pushed down for a considerable distance before they
uterus are lax structures, and the uterus can be pulled up
The broad ligaments and the round ligaments of the
either side of the rectouterine pouch (pouch of Douglas).
the lower end of the sacrum. They form two ridges, one on
pass to the cervix and the upper end of the vagina from
sist of two firm fibromuscular bands of pelvic fascia that
The sacrocervical ligaments con
Sacrocervical Ligaments
(pubovesical ligaments).
which they give some support
positioned on either side of the neck of the bladder, to
cervix from the posterior surface of the pubis. They are
sist of two firm bands of connective tissue that pass to the
The pubocervical ligaments con
Pubocervical Ligaments
vagina from the lateral walls of the pelvis.
vic fascia that pass to the cervix and the upper end of the
cervical ligaments are fibromuscular condensations of pel
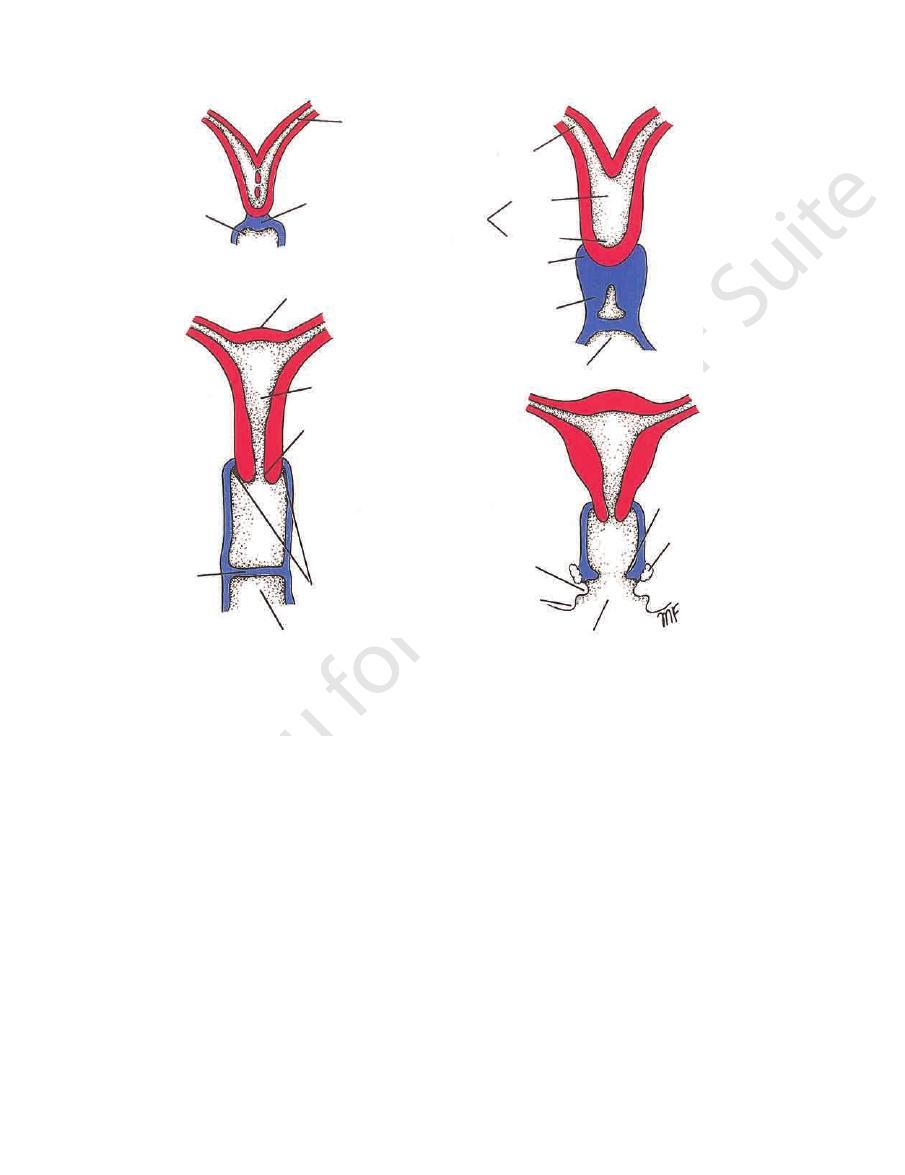
Transverse
Transverse Cervical (Cardinal) Ligaments
and keeping the cervix in its correct position (Figs. 7.28
vagina and play an important part in supporting the uterus
cles. They are attached to the cervix and the vault of the
pelvic fascia on the upper surface of the levatores ani mus
These three ligaments are subperitoneal condensations of
Sacrocervical Ligaments
The Transverse Cervical, Pubocervical, and
the uterus.
levatores ani and thus supports the vagina and, indirectly,
and the anal canal. It is slung up to the pelvic walls by the
The perineal body lies in the perineum between the vagina
during childbirth, prolapse of the pelvic viscera may occur.
integrity of the pelvic floor; if the perineal body is damaged
-
and 7.29).
-
-
-
-
bladder
pubocervical ligament
transverse cervical
ligament
sacrocervical ligament
rectum
cervix
rectum
transverse cervical ligament
pubocervical ligament
bladder
A
B
sacrocervical
ligament
FIGURE 7.29
Ligamentous supports of uterus.
visceral pelvic fascia.
Lateral view. These ligaments are formed from
As seen from below.
A.
B.
292
CHAPTER 7
The Pelvis: Part II—The Pelvic Cavity
Brief Summary of the Implantation of the Fertilized
blastocyst sinks beneath the surface epithelium and becomes
line (see Fig. 7.34). As the result of the enzymatic digestion of
Ovum in the Uterus
The blastocyst enters the uterine cavity between the fourth
and ninth days after ovulation. Normal implantation takes
place in the endometrium of the body of the uterus, most fre-
quently on the upper part of the posterior wall near the mid-
the uterine epithelium by the trophoblast of the embryo, the
embedded in the stroma by the 11th or 12th day.
E M B R Y O L O G I C N O T E S
Vagina
childbirth, the hymen usually consists only of tags.
which is perforated at its center. After
hymen,
called the
vaginal orifice in a virgin possesses a thin mucosal fold
anterior, posterior, right lateral, and left lateral. The
nices:
surrounds the cervix, is divided into four regions, or
Figs. 7.5 and 7.28). The area of the vaginal lumen, which
pelvic floor and the lower half lies within the perineum (see
remember that the upper half of the vagina lies above the
downward and backward into the vagina. It is important to
end, the anterior wall is pierced by the cervix, which projects
terior walls, which are normally in apposition. At its upper
measures about 3 in. (8 cm) long and has anterior and pos
backward from the vulva to the uterus (see Fig. 7.5). It
The vagina is a muscular tube that extends upward and
Location and Description
-
for-
uterine tube
urogenital sinus
vaginal plate
uterine tube
body
cervix
uterus
sinovaginal bulb
vaginal plate
urogenital sinus
fundus
body
cervix
lateral fornices
of vagina
hymen
urogenital sinus
hymen
vestibular glands
labium minus
labium major
vestibule
FIGURE 7.33
Formation of the uterine tubes, the uterus, and the vagina.
