15
Lec. 5 Digestion of Lipids
Lipids
Definition: Organic compounds that supply energy and used to build cell structures.
They include: triglycerides, cholesterol, and phospholipids
Lipid sources
o Triglycerides: are found in plant & animal-based foods
o Saturated fats: found in meat, eggs, milk, palm oil & coconut oil.
o Unsaturated fats: are found in seeds, nuts, & plant oils
Cholesterol is found in liver & egg yolk; small amounts in whole milk, butter, cheese,
& meats.
Plants do not contain cholesterol
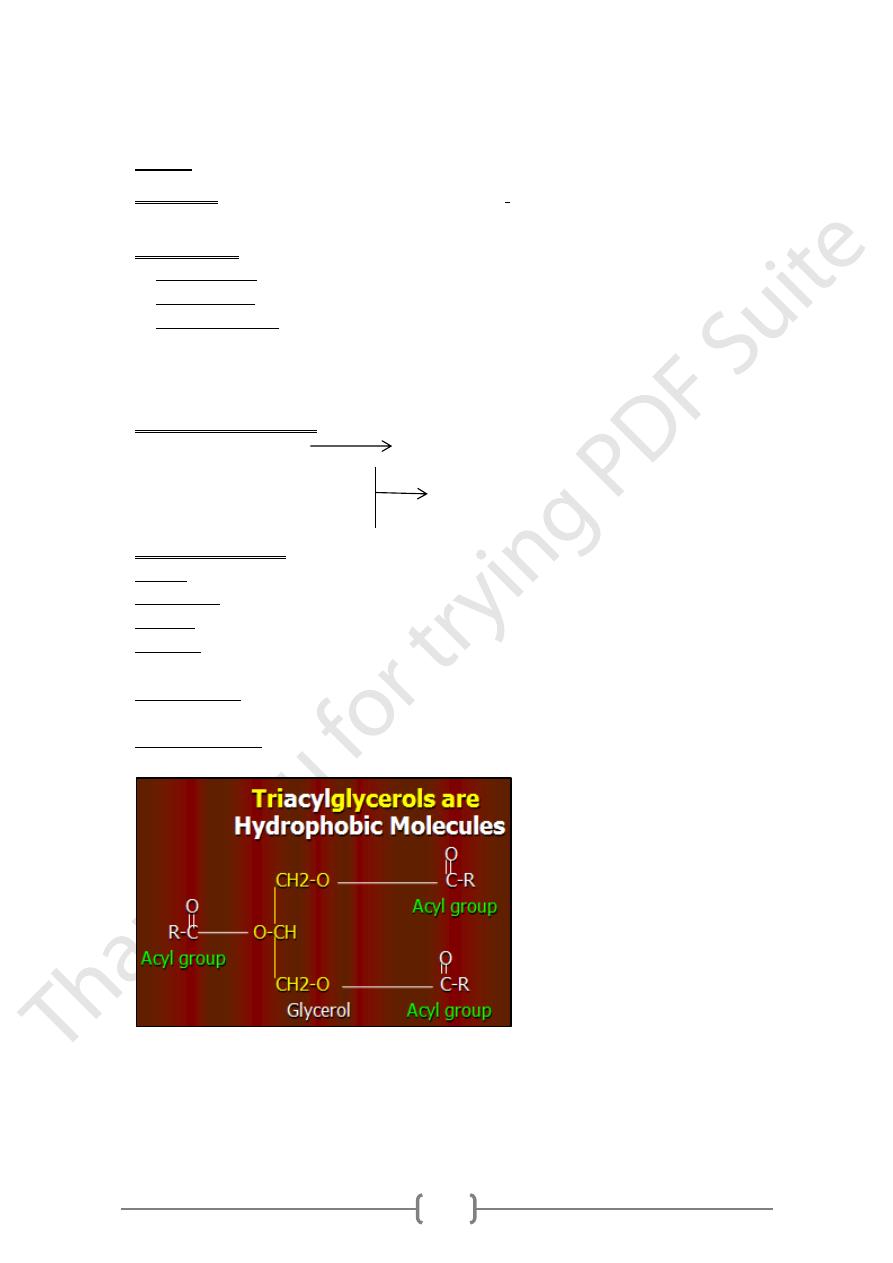
Types of Dietary Lipids
Triacylglycerol (TAG) 90%
Cholesterol & cholesterol ester
Phospholipids 10%
Free fatty acids (FFAs).
Functions of lipids
1) Energy: Lipids provide the greatest reserve (store) of energy, 1g of fat yields 9 Kcal.
2) Membranes: important for formation of biological membranes and nervous tissues.
3) Fixation: They help in the fixation of internal organs e.g. kidney, intestine.
4) Vitamins: provide body with fat-soluble vitamins (A,D,E &K), carotenes and
essential fatty acids.
5) Prostaglandins: Essential fatty acids are used for the synthesis of prostaglandins and
leukotrienes.
6) Steroid hormones: Cholesterol is used for synthesis of steroid h., vit.D
3
, & bile acids.
16
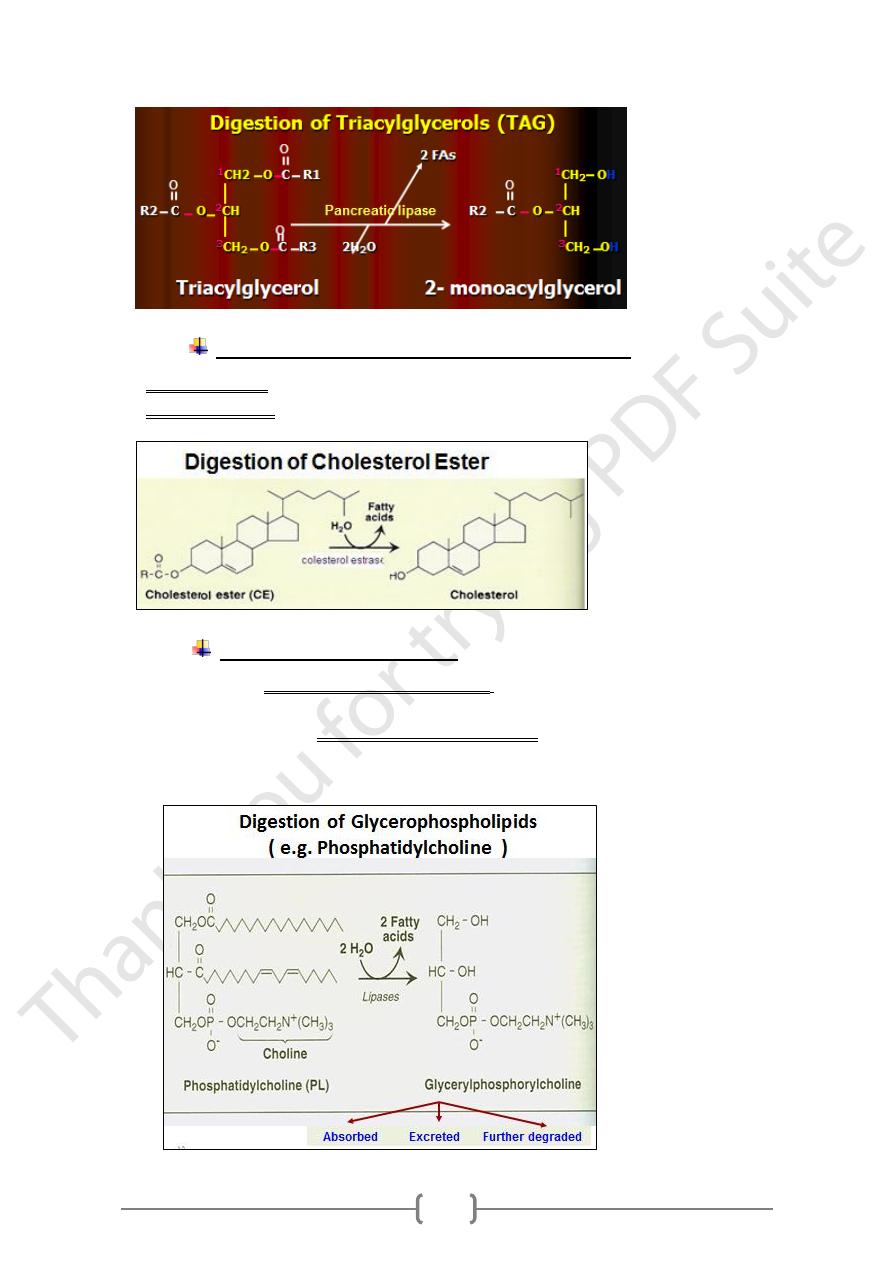
Digestion of Triacylglycerols (TAG)
In the mouth: no digestion of fat.
1. Lingual Lipase:
• Secreted from glands on back of tongue.
• It is an acid-stable lipase, Optimum pH: 4-6
• No action in the mouth.
In the stomach: Gastric lipase
2. Gastric lipase
1) Optimum pH: Neutral (7).
2) Needs prior emulsification of lipids that does not occur in stomach.
3) Specific for digestion of TAG that contain short chain FAs such as those of milk.
4) No action in the stomach.
Action of gastric lipase:
A. In infants: It has significant action because:
1) PH of stomach of infants is suitable (5).
2) Infants are fed milk whose lipids are highly emulsified & contain short chain FAs.
B. In adults: It is of limited value because:
1) PH in their stomach is highly acidic (1-2), so it is unsuitable for the action of the
enzyme.
2) Emulsification of fat, which is an important step before fat digestion, does not
occur in the stomach.
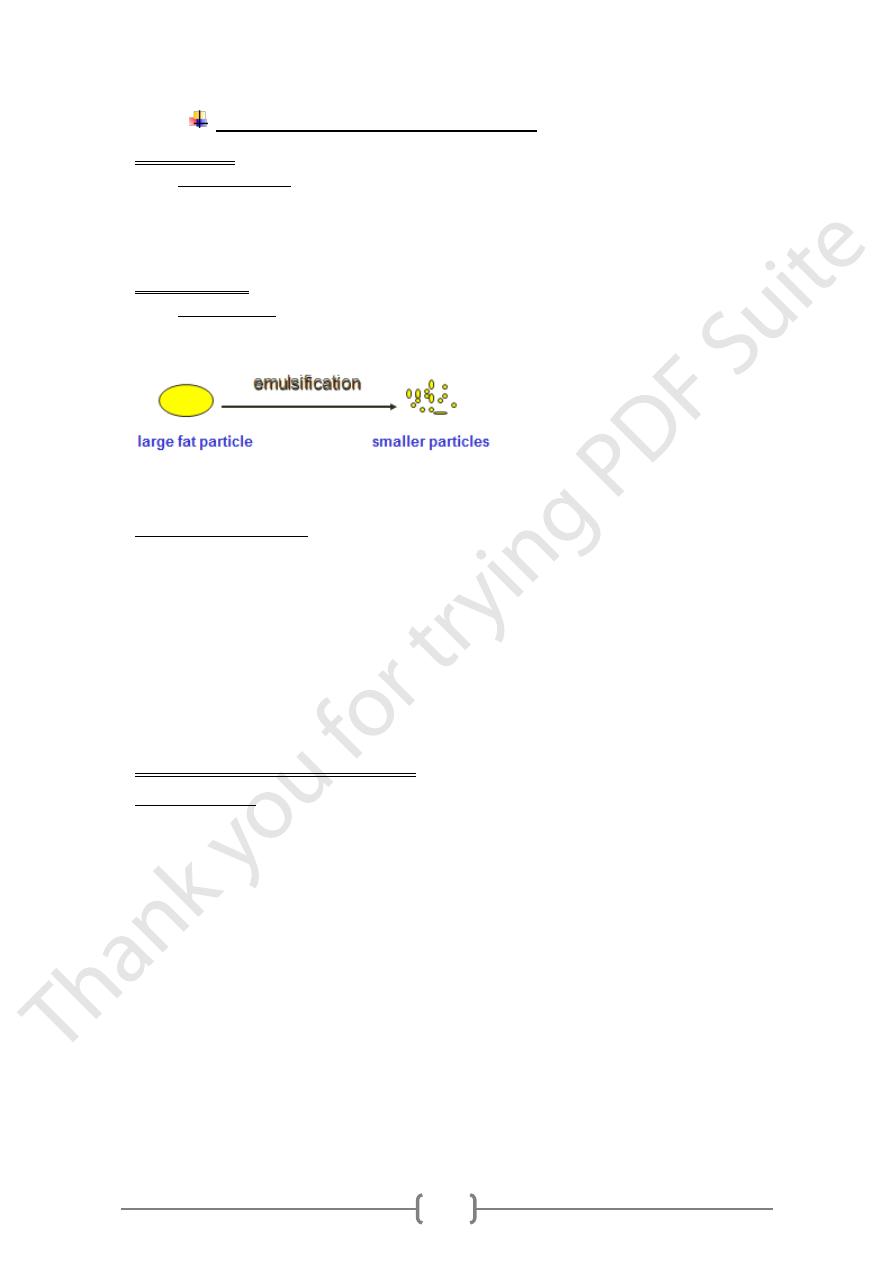
Lipid digestion In the small intestine
is the main enzyme in TAG digestion.
Pancreatic lipase
1) Optimum pH: 7-8 and the PH of intestine is 7-8.
2) Needs prior emulsification of lipids carried out by:
a. Bile salts.
b. Mechanical agitation of lipids by intestinal peristalsis.
3) Activated by:
a. Bile salts.
b. Colipse: a protein present in pancreatic secretion.
c. It fixes the enzyme to the surface of the lipid particle.
4) Action: It hydrolyzes the ester bonds of TAG at positions1 & 3producing
2-monoacylglycerol & 2 FAs.
17
Digestion of Cholesterol and Cholesterol Ester
Free cholesterol: is not digested and is absorbed as such.
Cholesterol ester: is digested by: cholesterol esterase into free cholesterol and FFA
Digestion of Phospholipids
• Are digested by pancreatic phospholipase A2 (acts on ester bond at position 2) in
the phospholipids.
• Are further digested by intestinal phospholipase A1 (acts on ester bond at position
1) in the: glyceryl phosphoryl base (e.g. glyceryl phosphoryl choline) which is
excreted, absorbed, or further degraded.
18
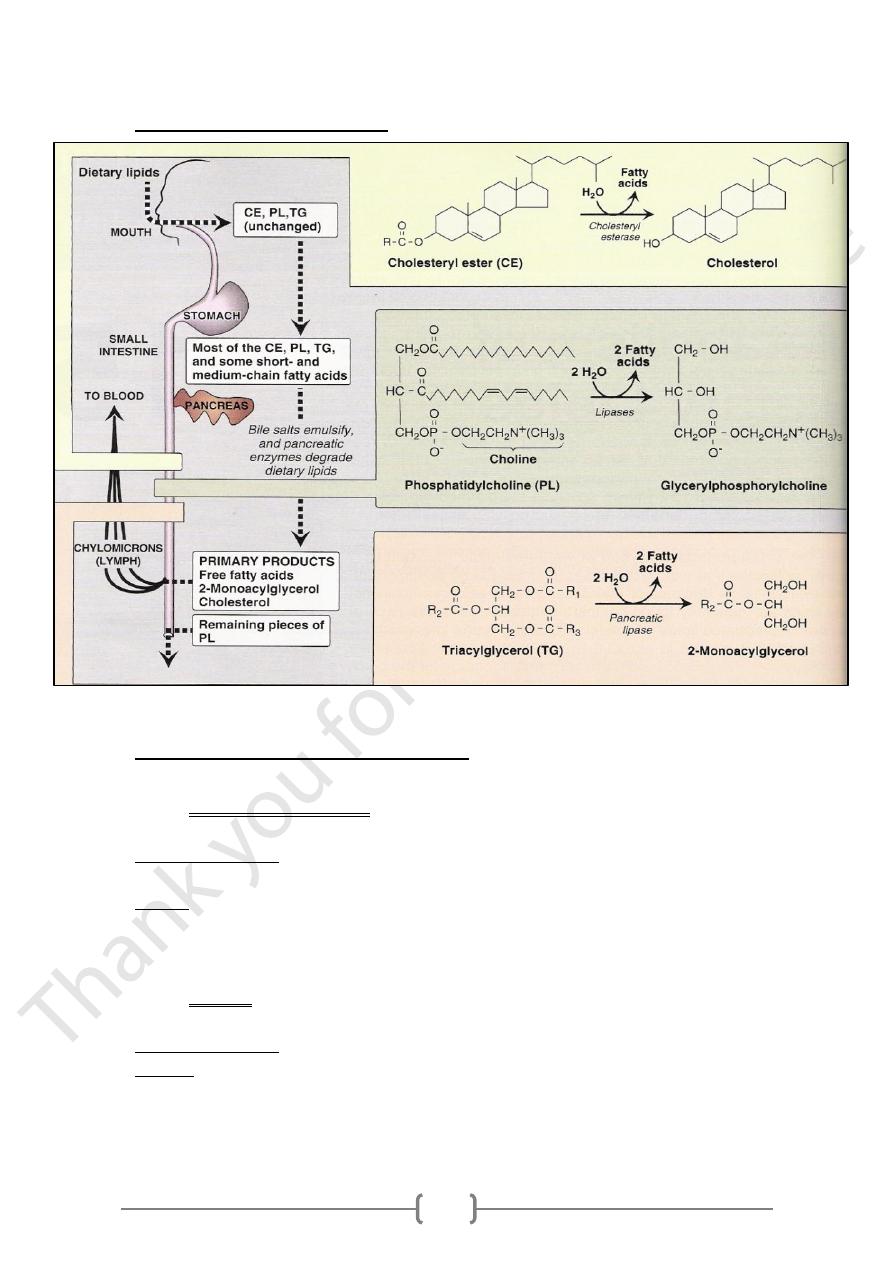
Overview of Lipid Digestion
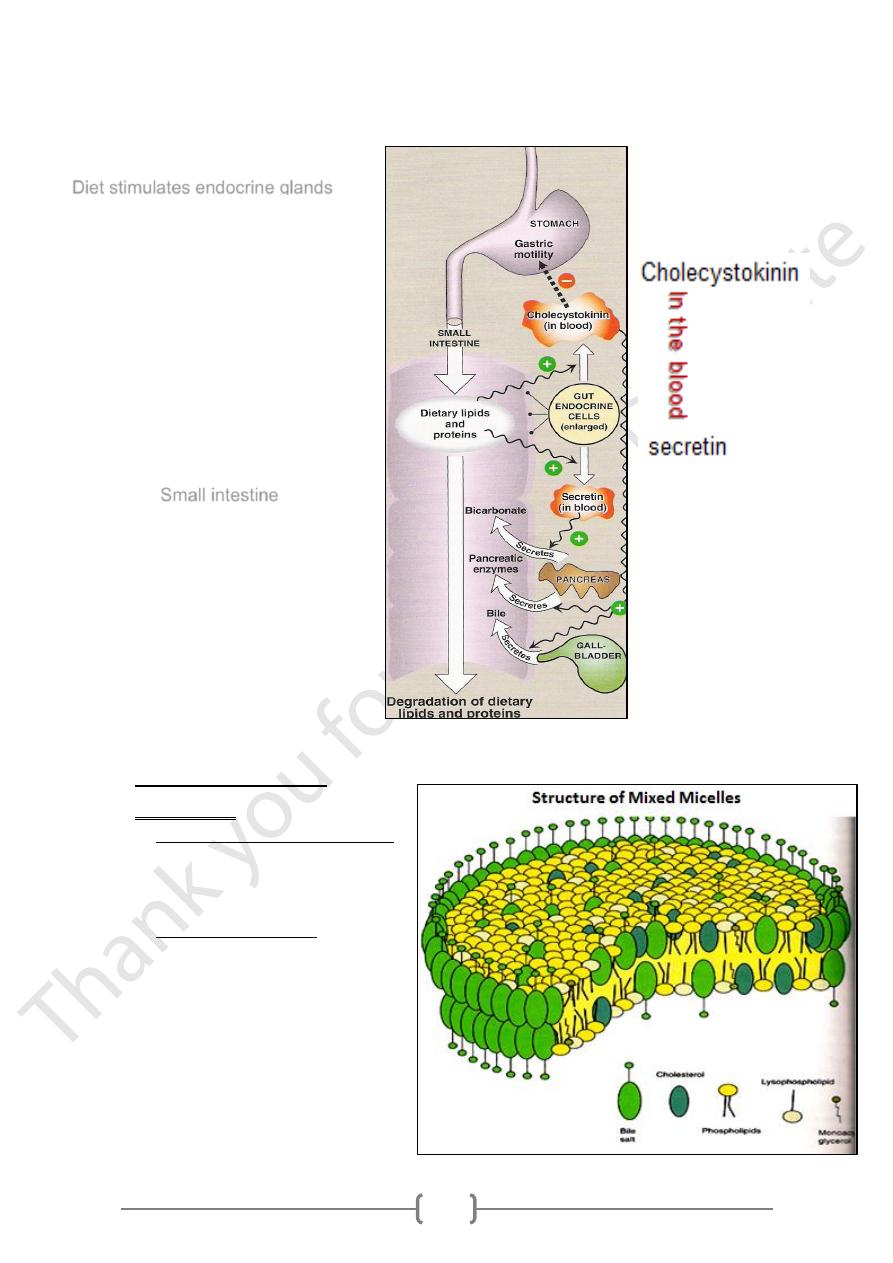
Hormonal Control of Lipid Digestion
The small intestine secretes 2 peptide hormones: Cholecystokinin (CCK) & Secretin.
1. Cholecystokinin (CCK)
• It is a peptide hormone produced by mucosal cells of the lower duodenum & jejunum.
• Stimulus for release: The presence of lipids & partially digested proteins in the
intestine.
• Action:
1) On gall bladder → contraction & release of bile.
2) On pancreas → release of pancreatic enzymes
3) On stomach → decrease gastric motility.
2. Secretin
• It is a peptide hormone produced by mucosal cells.
• Stimulus for release: Low pH of chyme entering the intestine.
• Action: It stimulates the pancreas to:
1) release a watery solution rich in bicarbonate,
2) neutralize the pH of intestinal contents and make it suitable for the action of the
digestive enzymes in the intestine.
19
Hormonal Control of Lipid Digestion
Absorption of Lipids
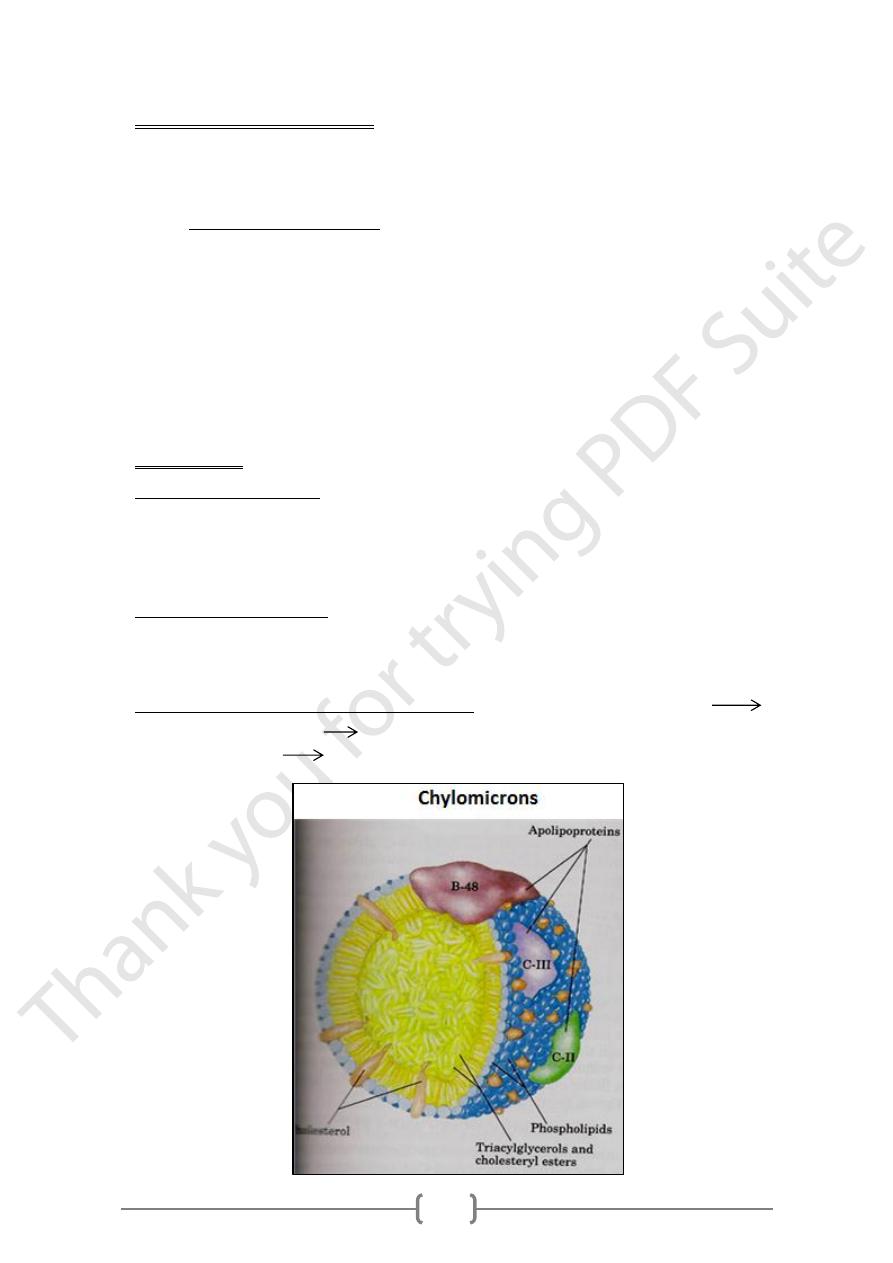
1) The micelles:
• The mixed micelles is formed by:
Long chain Fas,
Monoacylglycerol, Cholesterol,
Phospholipids & Bile salts
• In the mixed micelles:
o The hydrophilic regions are
directed outwards facing the
aqueous environment of the
intestinal lumen.
o The hydrophobic regions are
located in the center of the
micelle.
Diet stimulates endocrine glands
Small intestine
21
2) Short and Medium chain FFAs
Are not incorporated in the micelles. But carried by plasma albumin and pass to the
portal blood then to the liver.
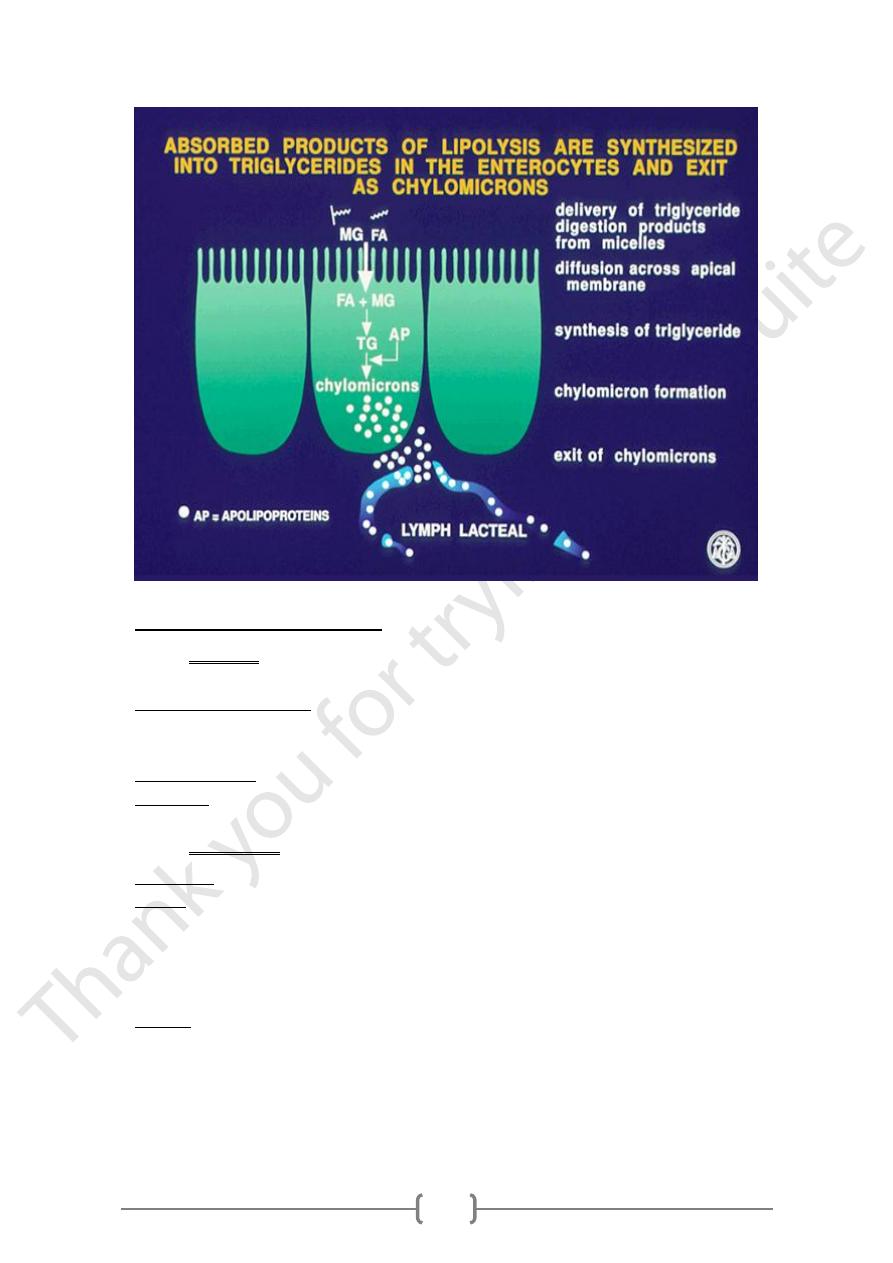
- Synthesis of chylomicrons
• The 2-monoacylglycerol and fatty acids absorbed into the intestinal mucosal cells are
converted again into triacylglycerols (TAG).
• Free cholesterol is converted again into cholesterol esters (CE).
• Because the synthesized TAG and CE are very hydrophobic and non-polar, they are
surrounded by a single layer of the amphipathic phospholipids together with a protein
called apolipoprotein B-48 (Apo B-48).
• This apolipoprotein stabilizes the particle and increases its solubility.
• This particle is a lipoprotein called chylomicron.
3) Chylomicrons
• Chylomicrons are formed in the mucosal cells from the absorbed lipid particles:
Triglycerides, free cholesterol + cholesterol ester, phospholipids & proteins called
apolipoproteins (Apo)
• Form a water-soluble lipoprotein complex called chylomicrons in the mucosal cells
of the small intestine.
• Structure of chylomicrons:
o
Amphipathic lipids (free cholesterol, phospholipids): form the outer part of
chylomicrons,
o
Hydrophobic lipids (tag + cholesterol ester): form the interior of the particle.
• Chylomicrons are released by exocytosis from: the intestinal mucosal cells into
the intestinal lymphatics. thoracic duct
left subclavian vein systemic circulation.
21
Nutrition and Git disorders
Diarrhea: watery stool
• Occurs when the colon absorbs too little water
• Causes of acute diarrhea:
1) Infection from: bacteria, viruses, or parasites
2) Antibiotics.
• Chronic diarrhea: chronic inflammatory bowel disease
• Treatment: Rehydrate and replace electrolytes
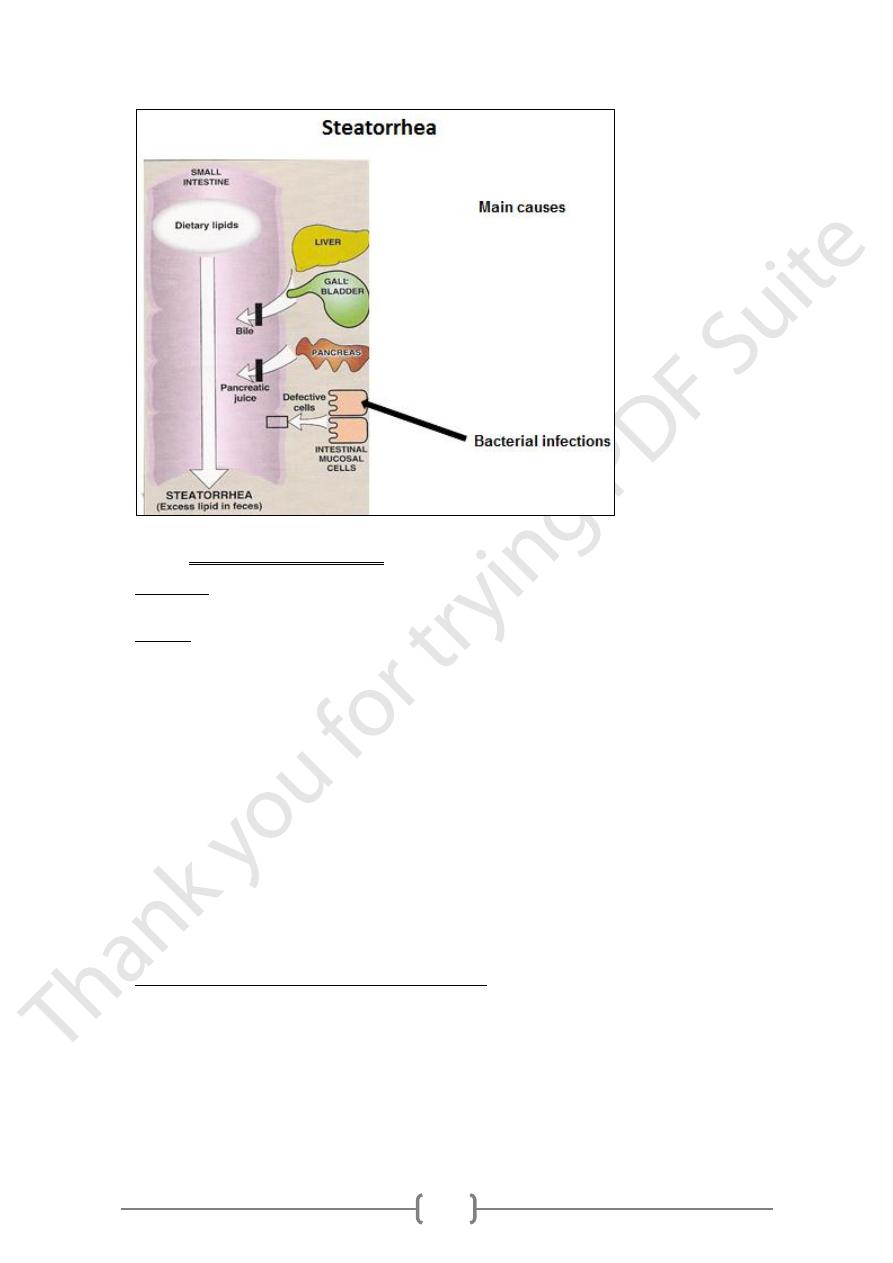
Steatorrhea
• Definition: It means excessive loss of lipids in stools.
• Causes:
1) Defect in the secretion of bile due to liver or gall bladder disease.
2) Defect in the secretion of pancreatic enzymes due to pancreatic disease.
3) Disease of the mucosal cells of the small intestine.
4) Bacterial infections
• Effects:
Deficiency of fat-soluble vitamins and essential fatty acids due to their loss in stool.
22
Malabsorption syndrome
• Definition: is a number of disorders in which nutrients are not digested or absorbed
properly.
• Causes:
1) Bile salt deficiencies: fats and fat-soluble vitamins are not absorbed
2) Lactase deficiency: lactose cannot be broken down for use
3) Pancreatic enzyme deficiency: Pancreatic enzymes are needed for proper
absorption of vitamins and lipid
4) Infections: viral, bacteria, or parasitic
5) Gastric surgery: the most common cause of malabsorption
6) Intestinal surgery: loss of surface area for absorption
7) Lymphatic system blockage:lead to a loss of vit.B12, folic acid, minerals & lipids
8) Decreased blood supply: reduces the absorption of nutrients
9) Crohn’s disease: decreases bile salt absorption and leads to fat malabsorption
10) Ulcerative colitis: leads to fat malabsorption
11) Celiac disease: genetic intolerance to gluten Damage to the lining of the small
intestine leads to decreased absorption of iron, protein, vitamins and calcium.
• Signs and symptoms of malabsorption syndrome
1) Weight loss: The body is unable to absorb needed nutrients
2) Steatorrhea: light-colored, Fatty bulky, foul-smelling stool.
3) Diarrhea: Inadequate absorption of nutrients
4) Edema (swelling): Results from decreased protein absorption
5) Anemia: Results from vit.B12, folic acid, or iron deficiency
