34
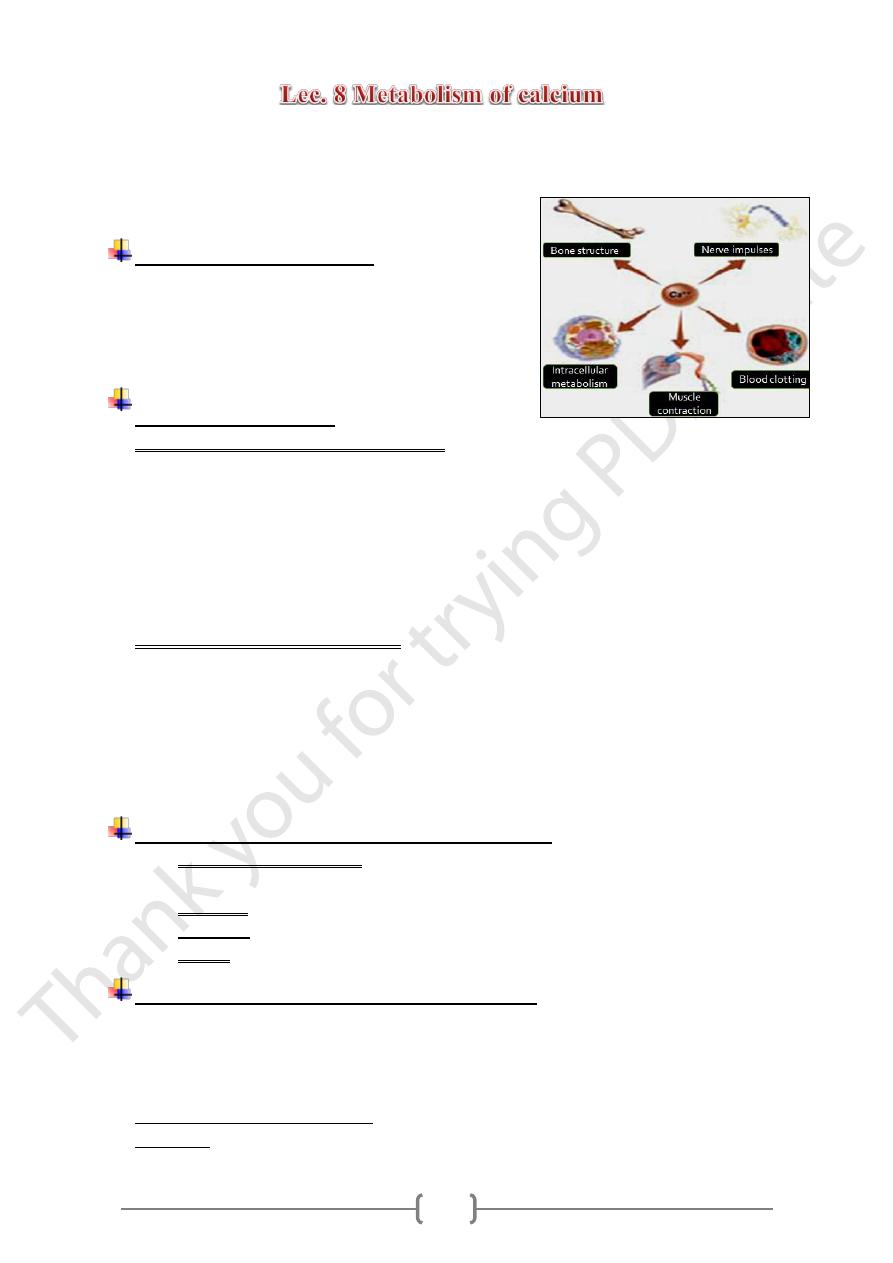
• Calcium is the most abundant mineral in human tissues.
• There is about one Kg of calcium in the adult body.
o 99% Ca in skeleton (bones and teeth).
o 1% is present in blood & other tissues.
Main functions of calcium
1. Building of bones and teeth.
2. Stimulates blood clotting
3. Muscle contractions
4. Transmission of nerve impulses
5. Intracellular metabolism
Absorption of calcium
• Absorption is regulated by the action of:
1,25 dihydroxycholecalciferol. The actions of 1,25 dihydorxycholecalciferol:
A. Synthesis of certain proteins which acts as Ca transporter across the intestinal
epithelium.
B. Synthesis of a Ca++ dependent ATPase which is involved in Ca++ active
transport.
C. In low Ca intake or hypocalcaemia: production of 1,25 DHCC is increased
leading to a higher Ca absorption.
• Factors causing low Ca absorption
A. Adrenal glucocorticoid hormones inhibit Ca
++
absorption.
B. Low estrogen levels: (postmenopausal women)
C. High concentrations of phytate & Oxalates in ileal mucosa.
D. High amounts of fatty acids in the intestine.
E. In steatorrhoea due to biliary obstruction and pancreatic or liver disease which
leads to insoluble Ca salts.
Regulation of storage and excretion of calicum
A. The storage compartment: the skeleton where Ca may be deposited or released
according to the needs of the body.
B. Excretion through the kidneys or intestine.
C. Hormonal: parathyroid hormone, calcitonin & vit. D3
D. Plasma low in protein causes low total Ca.
Action of hormones on plasma Ca regulation
A. Vitamin D3 from kidney.
B. Parathyroid hormone (PTH).
C. Calcitonin from thyroid gland.
D. Estrogen from the ovaries.
.
++
Act to increase plasma Ca
:
PTH and Vitamin D3 & estrogen
Acts to decrease plasma Ca.
:
Calcitonin
35
Responses to low plasma calcium
Increase in parathyroid hormone which stimulates the conversion of inactive vitamin
D to 1,25dihydorxycholecalciferol: This leads to: Increases in blood calcium by:
1. Increased absorption from Small intestine.
2. Increased reabsorption in the kidneys.
3. Mobilization of Ca from the bones.
Abnormal plasma Ca concentrations
A. hypocalcaemia:
The commonest causes of hypocalcaemia are:
1. Inadequate intake of Ca or vit D.
2. Hypoparathyroidsim.
3. Hypoproteinemia.
4. Chronic renal failure.
5. Nephrotic syndrome.
Acute hypocalcaemia: Will cause tetany
• Tetany: spasm and twitching of the muscles of the face, hands and feet.
• Main causes of tetany: Rickets, Alkalosis & Hypoparathyroidsim.
Chronic hypocalcaemia:
• Leads to diseases of the bone by Decalcification &Abnormal bone metabolism
• and causes:
1. Rickets………………. In children.
2. Osteomalacia….. In adults.
3. Osteoporosis ….. In old age.
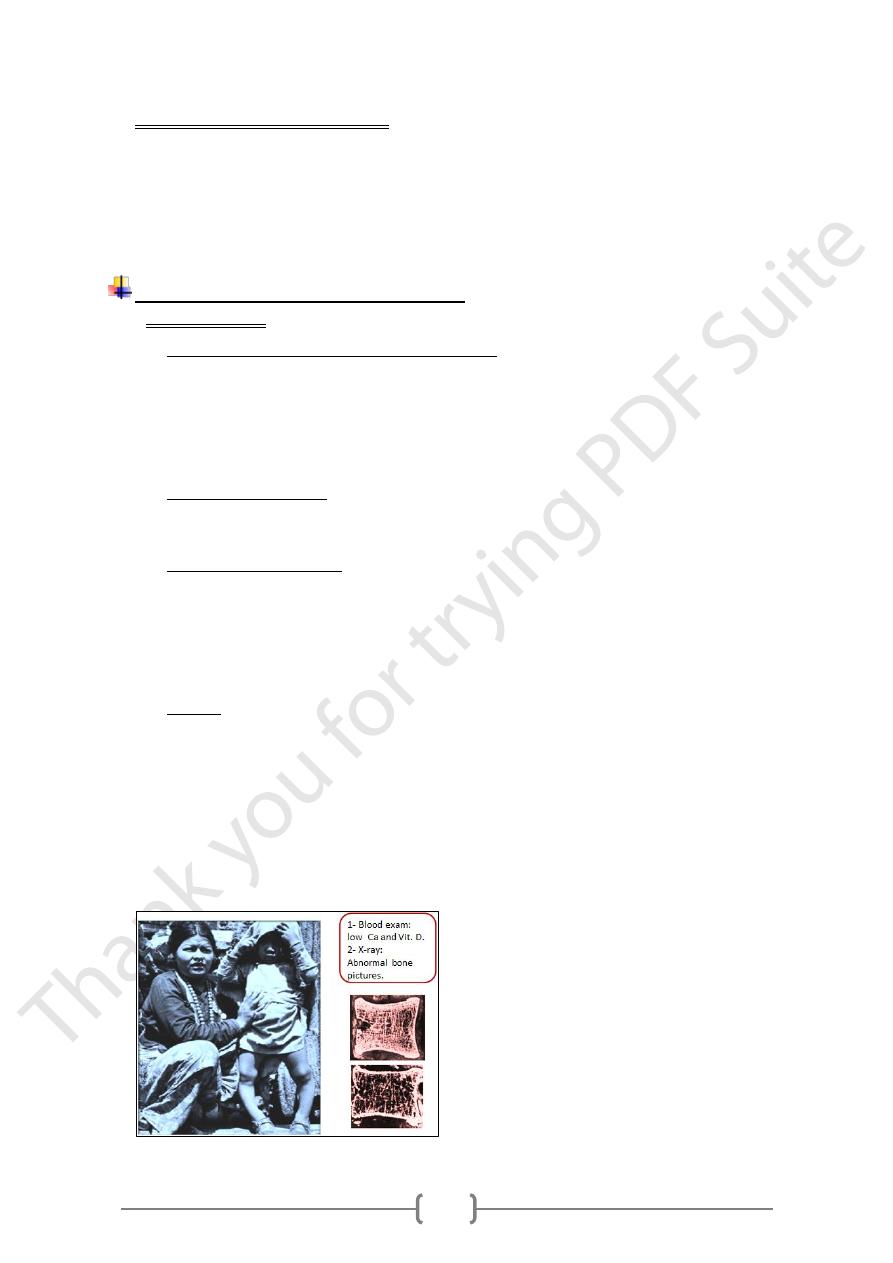
Rickets: is a disease of childhood:
• Due to low Ca and vit D intake.
• Leads to:
1. Decalcification of bones.
2. Bone will be soft and malformed.
3. Affects particularly long bones which become bowed.
4. Ribcache become rickety.
5. Rickets could be due to renal disease. (Renal Rickets )
36
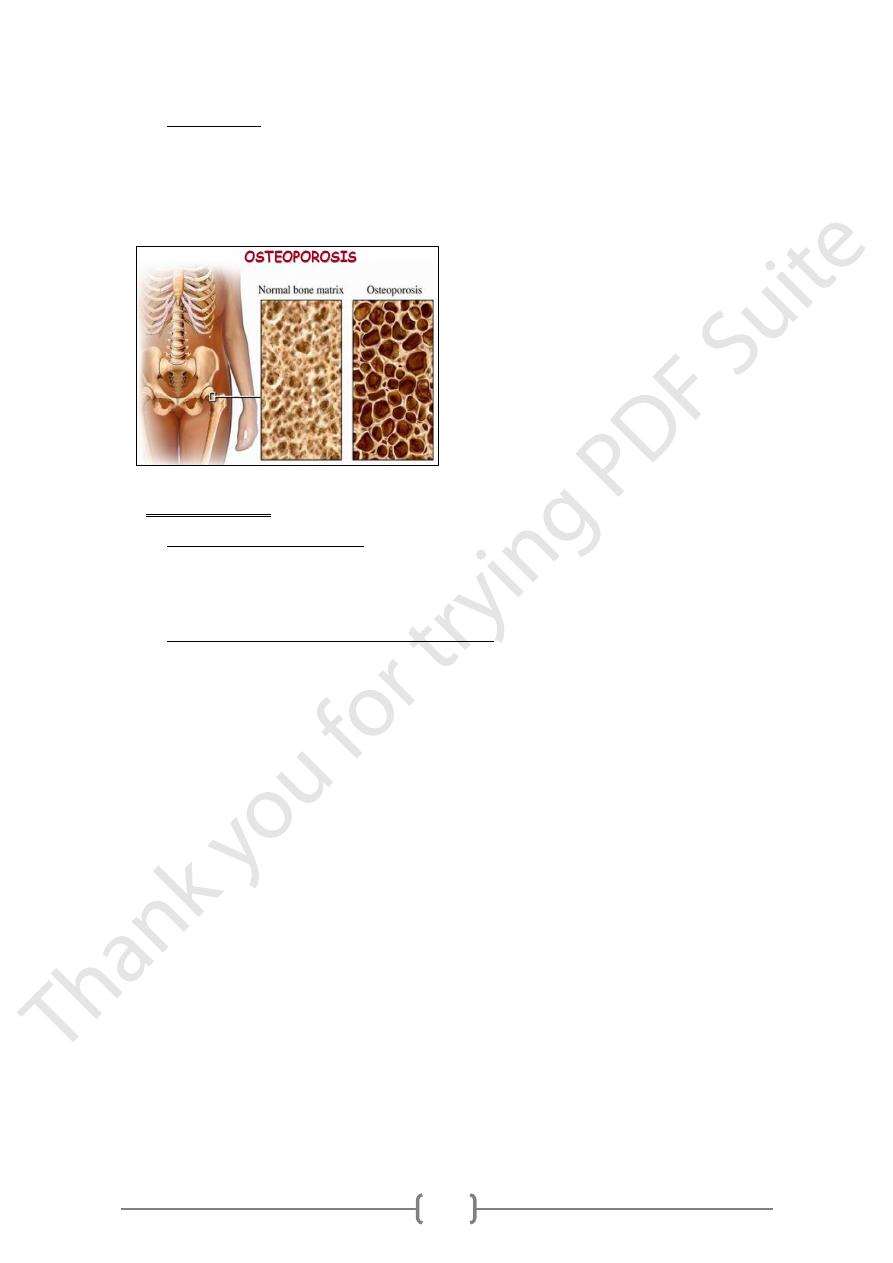
Osteoporosis
1) Loss of bony tissues resulting in bone that is brittle and liable to: fracture,
injury and infection.
2) Generalized osteoporosis is common in the women follows the menopause.
3) It is also a feature of cushings syndrome.
B. Hypercalcaemia
Causes of Hypercalcaemia:
1. Primary hyperparathyroidism.
2. Malignant diseases.
3. Excess intake of: Vit D or Ca or Both.
Chronic hypercalcaemia and calcium toxicity
1. Deposition in soft tissue
2. Impaired kidney function
3. Interference of other nutrient absorption: Iron & zinc
4. Osteocalcinosis.
