9
2) Free fatty acid mobilization from adipose tissue; directly
affects the level of ketogenesis
the factors regulating mobilization of free fatty acids from
adipose tissue are important in controlling ketogenesis.
3) The activity of carnitine palmitoyl transferase- I in liver,
which determines the proportion of the fatty acid flux that is
oxidized rather than esterified; HOW
• CPT-I activity is low in the fed state, leading to decrease fatty
acid oxidation, and , high in starvation, allowing fatty acid
oxidation to increase
• Malonyl-CoA, formed by acetyl-CoA carboxylase in the fed
state, is a potent inhibitor of CPT-I.
• Concentration of free fatty acids increases with the onset of
starvation, acetyl- CoA carboxylase is inhibited and malonyl-
CoA decreases, CPT-I transport more of acyl-CoA to
mitochondria to be oxidized (increase production of Acetyl-
CoA).
• These events are reinforced in starvation by decrease in the
[insulin]/[glucagon] ratio.
Lec. 5 - Ketosis
Higher level of ketone bodies than normal present in the blood
(ketonemia) or urine (ketonuria).
Ketoacidosis: increase acidity of the blood due to presence of
high concentration of ketone bodies.
ketone bodies are moderately strong acids and buffered with
alkali reserve (plasma bicarbonate) when present in blood but
their continuous production in large quantity progressively
depletes this reserve, causing ketoacidosis .
The higher ketone bodies conc. in the blood or urine due to
increased production by liver rather than decrease in their
utilization by extrahepatic tissues.
Ketoacidosis develops from excessive production of acetyl –
CoA due to body attempts to obtain energy from stored fat in
the absence of adequate carbohydrate metabolites. This
condition reinforced by : Inadequate incorporation of acetyl-
CoA into TCA due to decrease of the oxaloacetate
concentration
Ketosis reflects excessive use of fat due to:
1- Intracellular glucose deficiency
2- Low insulin level & activity:
How
This will increase rate of production of gluconeogenic
substrate by glycolysis & proteolysis & rate of hepatic
gluconeogenesis.
Lead to increase rate of glucose released into the
extracellular, this is appropriate in starvation, but aggravates
the hyperglycemia in DM.
ketosis can be reversed by restoring adequate of
carbohydrate metabolism.
1) In starvation:
Restorations consist of adequate carbohydrate ingestion.
2) In diabetic ketosis :
can be reversed by insulin administration ,which permits
circulating blood glucose to be taken up by the cells ,with
production of oxaloacetate (the acceptor of acetyl –CoA ),
normal metabolism is restored & decrease release of FA from
adipose tissues .
10
Types of Ketoacidosis:
1) Fasting Ketoacidosis (ketotic hypoglycemia):
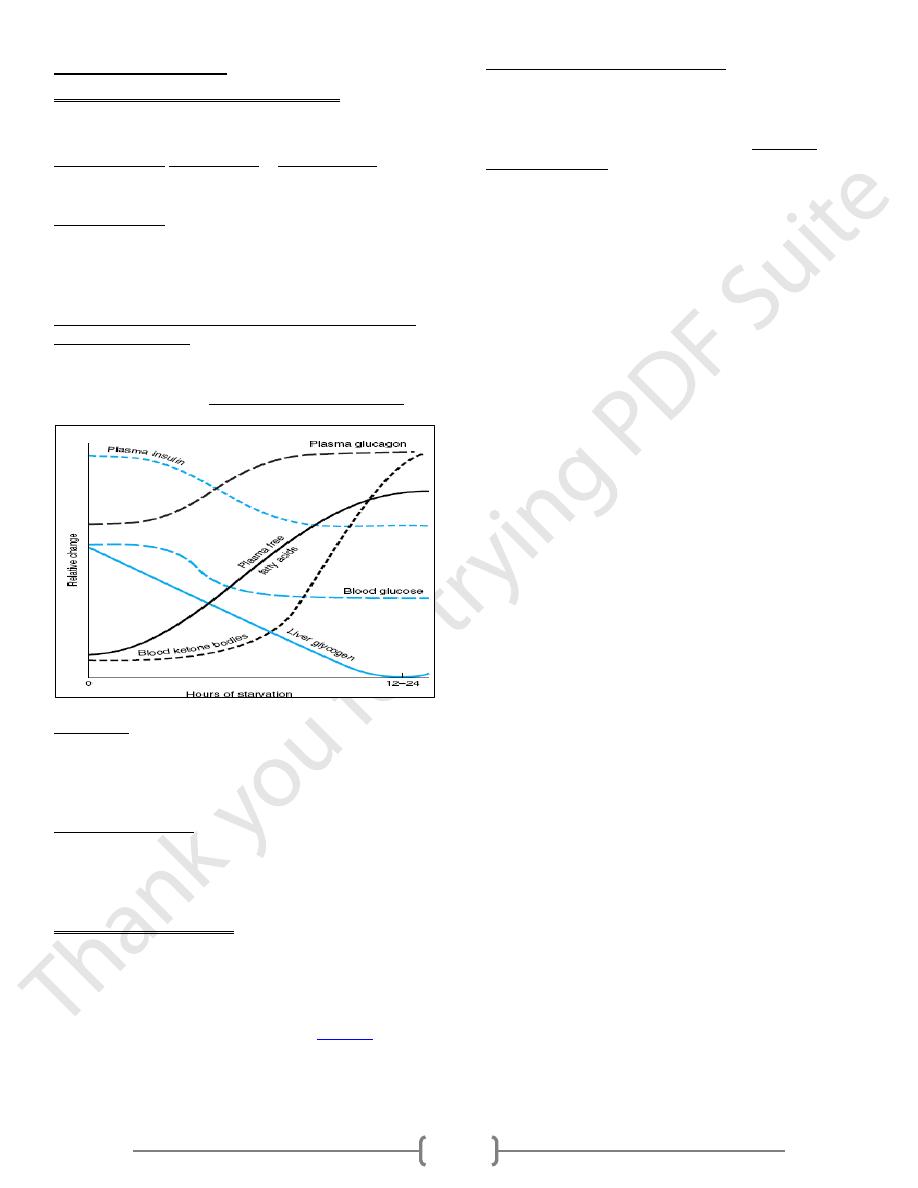
Ketosis occurs in starvation due to depletion of available
carbohydrate coupled with mobilization of FFA.
1. During starvation glycogenolysis & gluconeogenesis
increased, leads to depletion of TCA intermediates, diverting
acetyl-CoA to ketone body production
2. During starvation lipolysis increased & lipogenesis decreased
due to decreased insulin secretion, increase glucagon secretion
which lead to mobilization of FFA in order to use as major
energy source, resulted in increase hepatic production of
ketone bodies in blood.
3. Brain may tolerate ketotic hypoglycemia better than insulin-
induced hypoglycemia because: in ketotic hypoglycemia,
brain adapts to ketone bodies metabolism ,while in insulin
induced hypoglycemia, ketone concentration are low ,thus
depriving the brain of it's only non-glucose energy source .
4. In starvation, glucose must be provided for the brain and
erythrocytes, so that muscle and other tissues reduce glucose
uptake in response to fall in blood glucose level & lowered
insulin secretion in order to spare glucose, also they oxidize
fatty acids and ketone bodies preferentially to glucose.
5. In prolonged starvation, as adipose tissue reserves are
depleted, there is a considerable increase in the protein
catabolism to provide amino acid as substrates for
gluconeogenesis & as the metabolic fuel of the tissues.
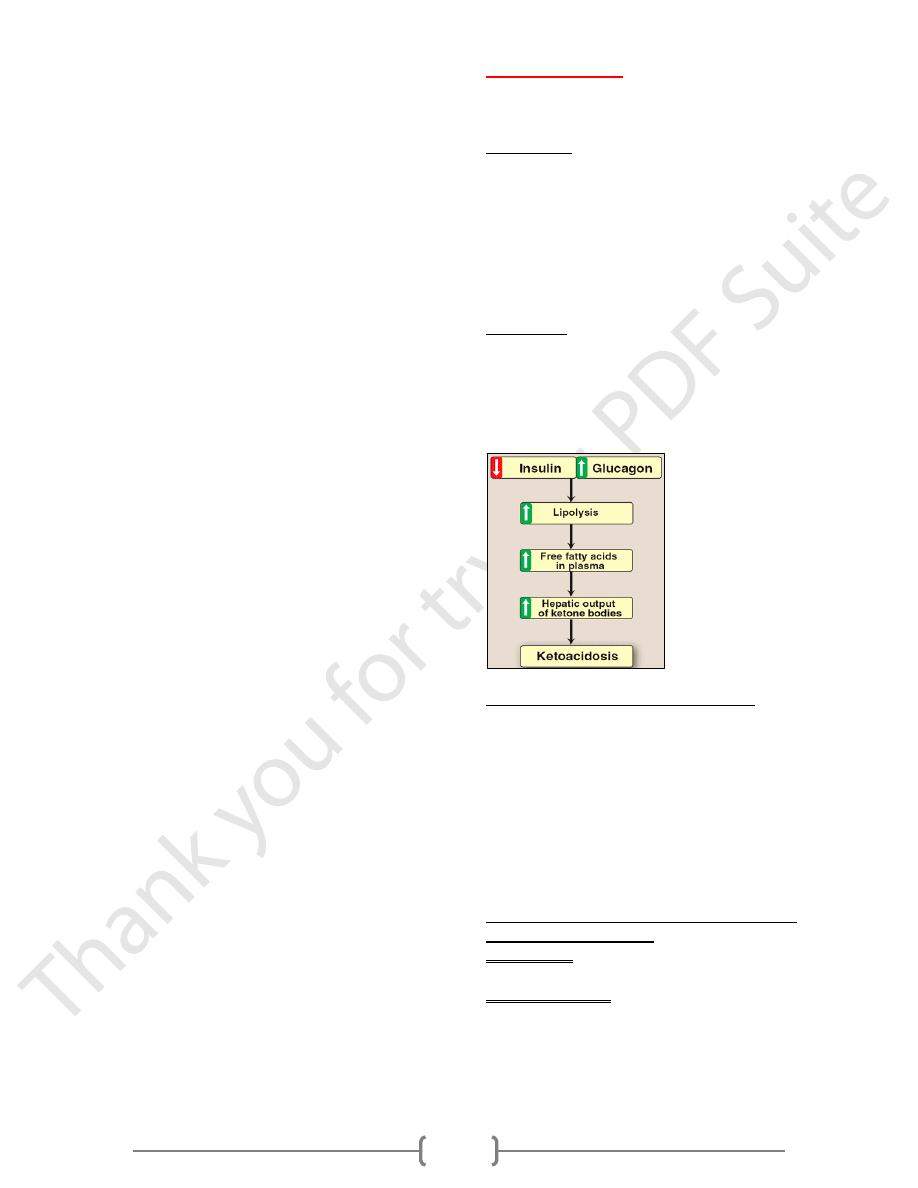
2) Diabetic Ketoacidosis DKA:
Insulin deficiency increases lipolysis and therefore free fatty
acid delivery to the liver.
Glucagon stimulates the adipose tissue to release fatty acids
stored in triglycerides, the FFA enter the circulation and are
taken up by the liver where they undergo β-
oxidation
to acetyl
CoA.
Differentiated from fasting ketoacidosis by hyperglycemia but
both cases due to intracellular glucose deficiency & in
diabetic ketosis is due to low insulin level & activity.
In uncontrolled DM, extrahepatic tissues cannot take up
glucose efficiently from the blood, either as fuel or for
conversion to TAG so that patients becomes hyperglycemic,
as a result of lack of insulin & because of increased
gluconeogenesis.
The increased blood levels of keton body lower the blood pH,
causing the acidosis.
Hyperglycemia produces an osmotic diuresis that leads to loss
of water and electrolytes in the urine. The ketones are also
excreted in the urine and this result in an obligatory loss of
Na+ and K+.
