muscle membrane and its subneural clefts below.
of the details of this mechanism can be seen in Figure 7–2, which shows an
of acetylcholine are released from the terminals into the synaptic space. Some
When a nerve impulse reaches the neuromuscular junction, about 125 vesicles
Secretion of Acetylcholine by the Nerve Terminals
vesicles.
acetylcholinesterase,
of which are normally in the terminals of a single end plate. In the synaptic
synaptic vesicles,
fiber membrane. Acetylcholine is synthesized in the cytoplasm of the terminal,
The acetylcholine in turn excites the muscle
acetylcholine.
phate (ATP), the energy source that is used for synthesis of an excitatory
subneural clefts,
This space is 20 to 30 nanometers wide. At the bottom of the gutter are numer-
a single axon terminal and the muscle fiber membrane. The invaginated mem-
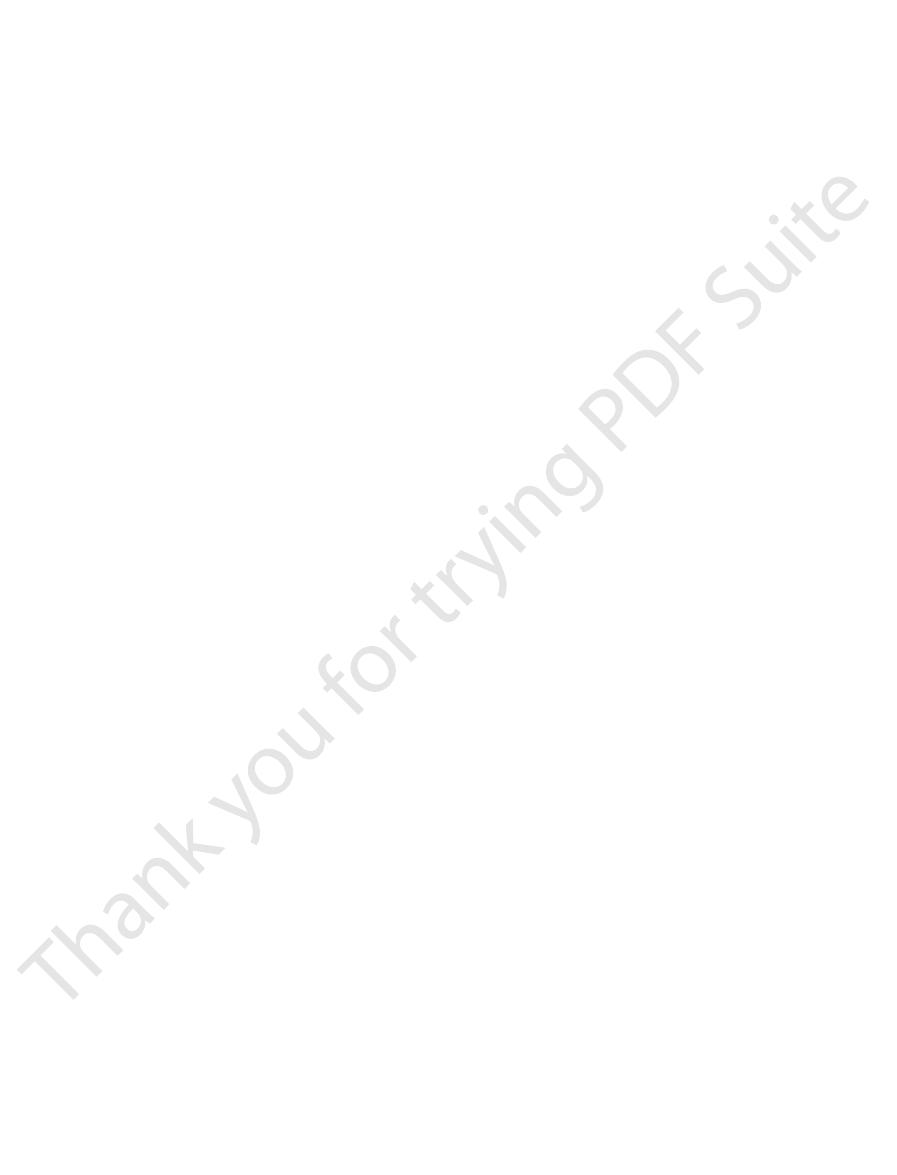
Figure 7–1
surrounding fluids.
plate.
muscle fiber plasma membrane. The entire structure is called the
branching nerve
to a skeletal muscle fiber. The nerve fiber forms a complex of
shows the neuromuscular junction from a large, myelinated nerve fiber
Figure 7–1
of the muscle fibers, there is only one such junction per muscle fiber.
directions toward the muscle fiber ends. With the exception of about 2 per cent
with the muscle fiber near its midpoint. The
several hundred skeletal muscle fibers. Each nerve ending makes a junction,
entering the muscle belly, normally branches and stimulates from three to
horns of the spinal cord. As pointed out in Chapter 6, each nerve fiber, after
The skeletal muscle fibers are innervated by large,
The Neuromuscular
from Nerve Endings to
Transmission of Impulses
Neuromuscular Transmission and
C
H
A
P
T
E
R
7
85
Excitation of Skeletal Muscle:
Excitation-Contraction Coupling
Skeletal Muscle Fibers:
Junction
myelinated nerve fibers that originate from large motoneurons in the anterior
called the neuromuscular junction,
action potential initiated in the muscle fiber by the nerve signal travels in both
Physiologic Anatomy of the Neuromuscular Junction—The Motor End Plate.
A
and B
terminals that invaginate into the surface of the muscle fiber but lie outside the
motor end
It is covered by one or more Schwann cells that insulate it from the
C shows an electron micrographic sketch of the junction between
brane is called the synaptic gutter or synaptic trough, and the space between the
terminal and the fiber membrane is called the synaptic space or synaptic cleft.
ous smaller folds of the muscle membrane called
which greatly
increase the surface area at which the synaptic transmitter can act.
In the axon terminal are many mitochondria that supply adenosine triphos-
transmitter
but it is absorbed rapidly into many small
about 300,000
space are large quantities of the enzyme
which destroys
acetylcholine a few milliseconds after it has been released from the synaptic
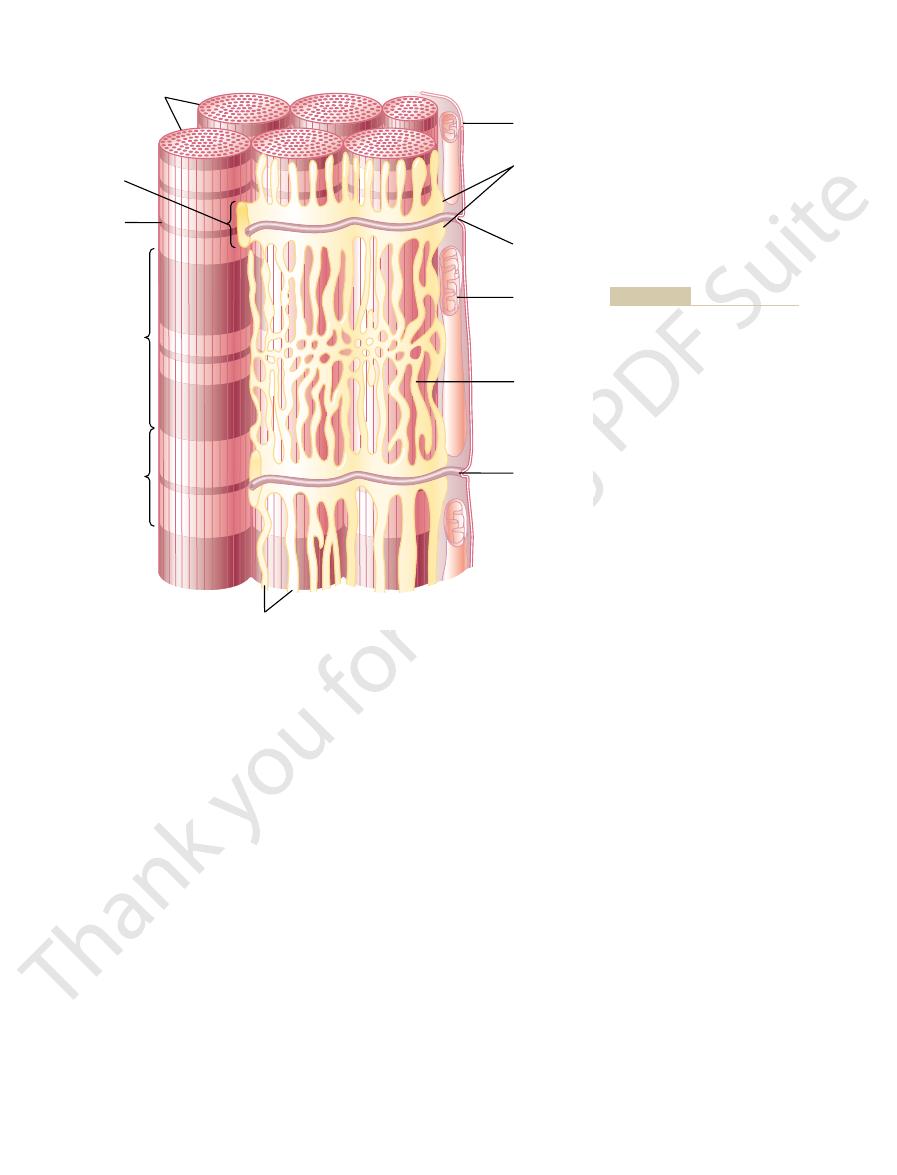
expanded view of a synaptic space with the neural membrane above and the
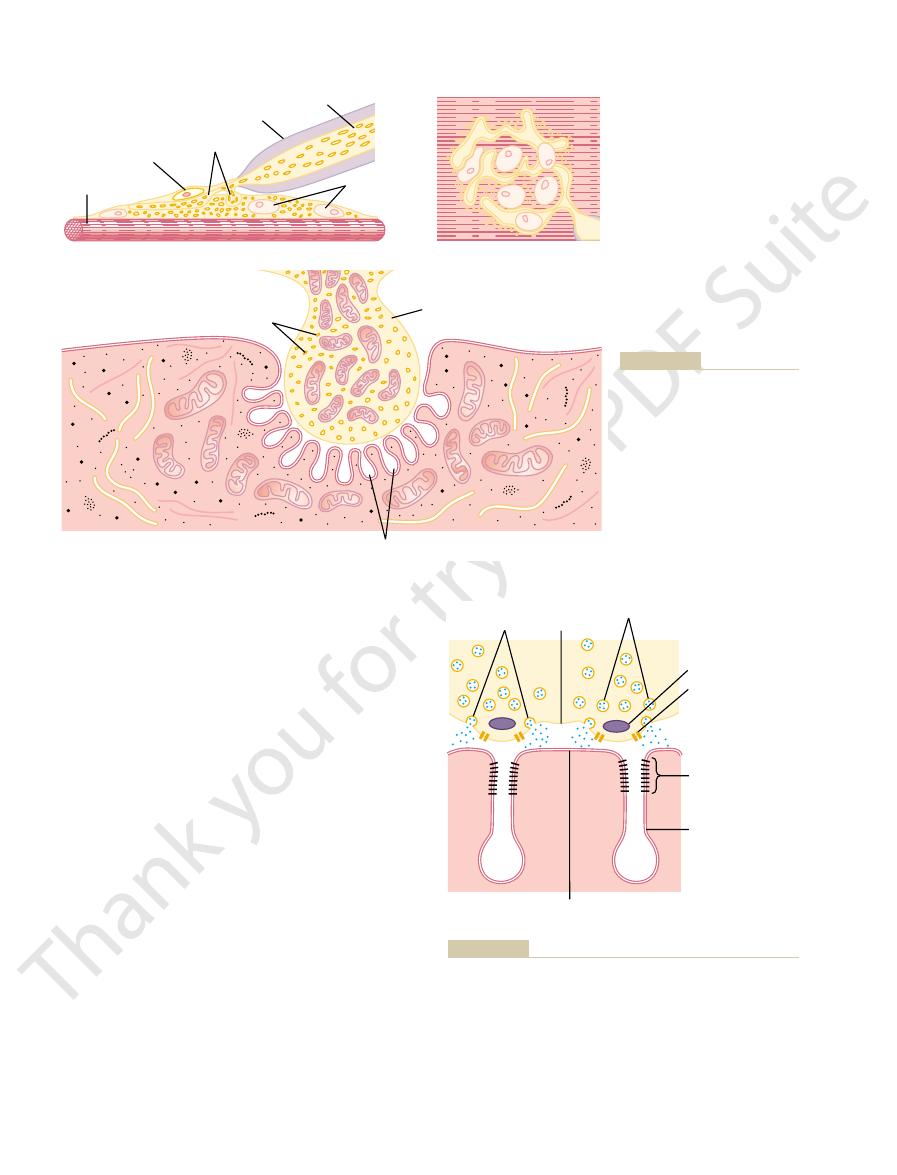
molecular weight of 275,000. The complex is composed
into the synaptic space.
dense bar areas, where the acetylcholine is emptied
acetylcholine-gated ion channels,
membrane; these are
acetylcholine receptors
Figure 7–2 also shows many
brane to Open Ion Channels.
adjacent to the dense bars.
speculative, it is known that the effective stimulus for
exocytosis.
membrane adjacent to the dense bars. The vesicles
the acetylcholine vesicles, drawing them to the neural
in turn, are believed to exert an attractive influence on
to the interior of the nerve terminal. The calcium ions,
spreads over the terminal, these channels open and
When an action potential
gated calcium channels.
that penetrate the neural membrane; these are
To each side of each dense bar are protein particles
shown in cross section in Figure 7–2.
dense bars,
Membrane Physiology, Nerve, and Muscle
86
Unit II
On the inside surface of the neural membrane are
linear
voltage-
allow calcium ions to diffuse from the synaptic space
then fuse with the neural membrane and empty their
acetylcholine into the synaptic space by the process of
Although some of the aforementioned details are
causing acetylcholine release from the vesicles is entry
of calcium ions and that acetylcholine from the vesi-
cles is then emptied through the neural membrane
Effect of Acetylcholine on the Postsynaptic Muscle Fiber Mem-
very small
in the muscle fiber
and they are located almost entirely near the mouths
of the subneural clefts lying immediately below the
Each receptor is a protein complex that has a total
Terminal nerve
Teloglial cell
Axon
Myofibrils
A
C
B
branches
Muscle
nuclei
Myelin
sheath
Synaptic vesicles
Axon terminal in
synaptic trough
Subneural clefts
DW: A Textbook of Histology.
Couteaux R, in Bloom W, Fawcett
Fawcett DW, as modified from
fiber membrane. (Redrawn from
axon terminal and the muscle
micrographic appearance of the
Electron
Surface
through the end plate.
Different views of the motor end
Figure 7–1
plate. A, Longitudinal section
B,
view of the end plate. C,
contact point between a single
Philadelphia: WB Saunders,
1986.)
Vesicles
Calcium
channels
Neural
membrane
Muscle
membrane
Release
sites
Dense bar
Basal lamina
and
acetylcholinesterase
Acetylcholine
receptors
Subneural cleft
receptors in the muscle membrane, at the mouths of the subneural
the release sites in the neural membrane to the acetylcholine
membrane of the neuromuscular junction. Note the proximity of
Release of acetylcholine from synaptic vesicles at the neural
Figure 7–2
clefts.
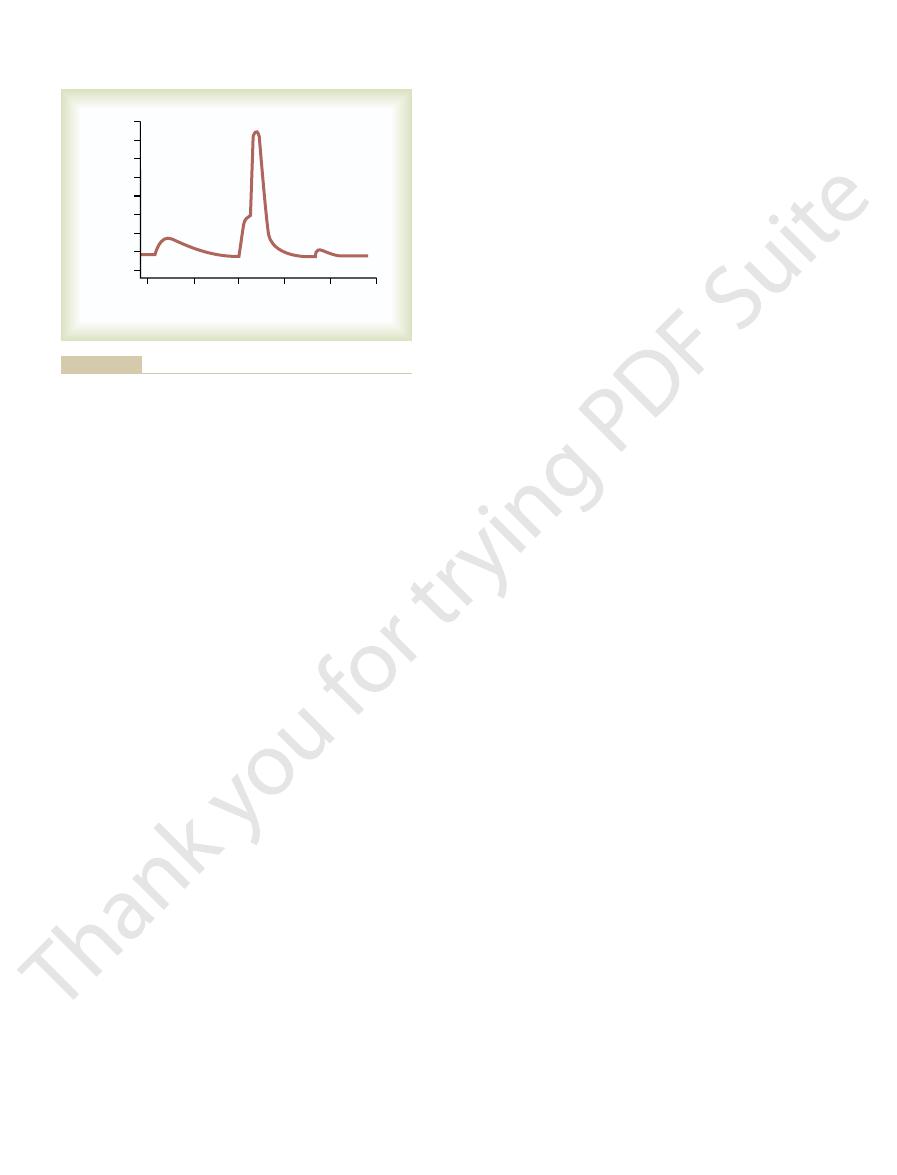
voltage changes, as recorded in the figure. By contrast,
potential, but they do produce weak local end plate
potentials A and C are too weak to elicit an action
shows three separate end plate potentials. End plate
potential initiating the action potential. This figure
Figure 7–4 shows the principle of an end plate
membrane.
to initiate more and more sodium channel opening,
much as 50 to 75 millivolts, creating a
The sudden insurgence of sodium ions into the muscle
End Plate Potential and Excitation of the Skeletal Muscle Fiber.
is sufficient to excite the muscle fiber. Then the rapid
The short time that the acetylcholine remains in the
to act on the muscle fiber membrane.
brane. (2) A small amount of acetylcholine diffuses out
acetylcholinesterase,
means: (1) Most of the acetylcholine is destroyed
in the space. However, it is removed rapidly by two
the synaptic space, continues to activate the acetyl-
The acetylcholine, once released into
In turn, this end plate potential initiates an
inside the muscle fiber membrane, called the
charges. This creates a local positive potential change
the fiber, carrying with them large numbers of positive
, the principal effect of
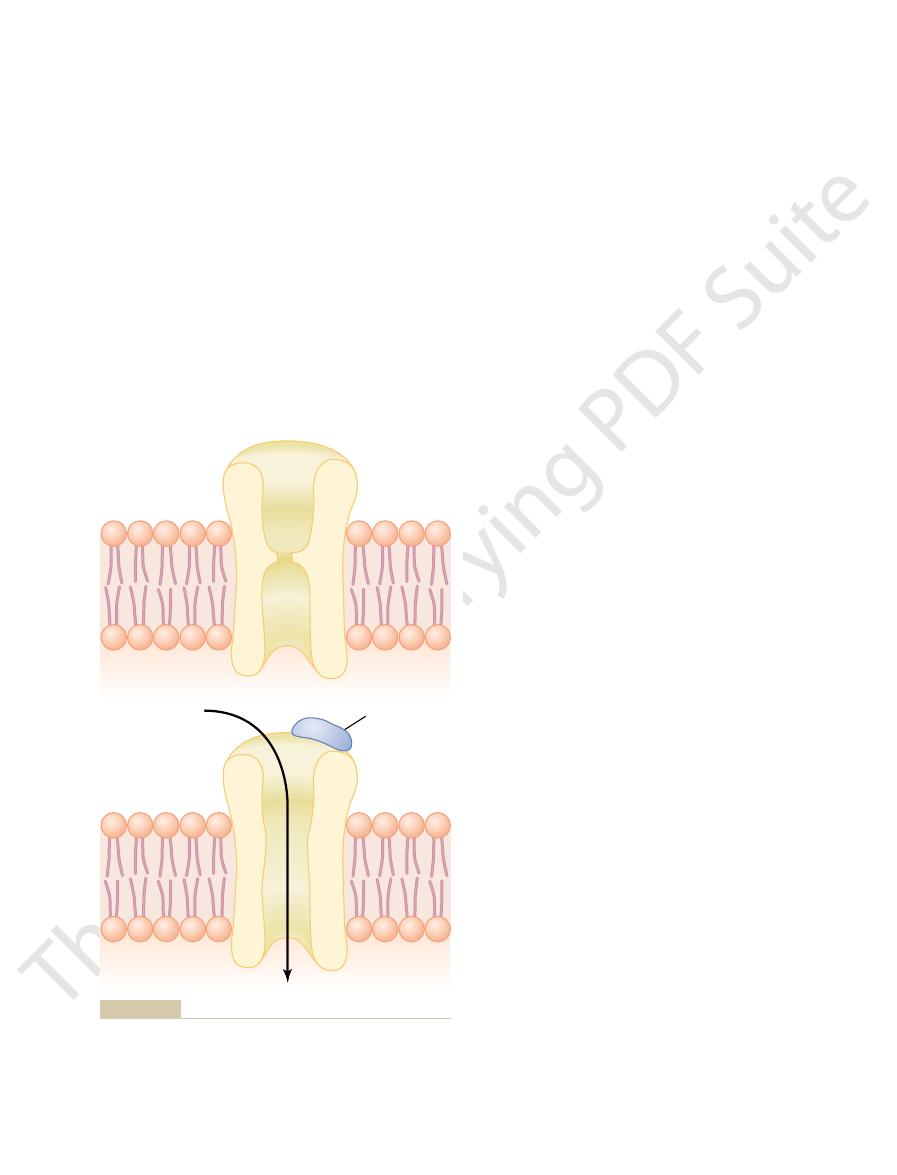
As shown in Figure 7–3
charged sodium ions to the inside of the fiber, while
membrane, –80 to –90 millivolts, pulls the positively
and potassium ions in the intracellular fluid. Second,
concentration: sodium ions in the extracellular fluid,
reasons. First, there are only two positive ions in large
acetylcholine channels than any other ions, for two
In practice, far more sodium ions flow through the
negative ions.
ions, do not pass through because of strong negative
opening. Conversely, negative ions, such as chloride
), and calcium (Ca
), potassium
about 0.65 nanometer, which is large enough to allow
The opened acetylcholine channel has a diameter of
section B of the figure.
tional change that opens the channel, as shown in
subunit proteins. This causes a conforma-
constricted, as shown in section A of the figure, until
channel, illustrated in Figure 7–3. The channel remains
brane, lying side by side in a circle to form a tubular
proteins. These protein
beta, delta,
of five subunit proteins, two
Excitation of Skeletal Muscle: Neuromuscular Transmission and Excitation-Contraction Coupling
Chapter 7
87
alpha proteins and one
each of
and gamma
molecules penetrate all the way through the mem-
two acetylcholine molecules attach respectively to the
two alpha
the important positive ions—sodium (Na
+
(K
+
++
)—to move easily through the
charges in the mouth of the channel that repel these
the very negative potential on the inside of the muscle
simultaneously preventing efflux of the positively
charged potassium ions when they attempt to pass
outward.
B
opening the acetylcholine-gated channels is to allow
large numbers of sodium ions to pour to the inside of
end plate
potential.
action potential that spreads along the muscle mem-
brane and thus causes muscle contraction.
Destruction of the Released Acetylcholine by Acetyl-
cholinesterase.
choline receptors as long as the acetylcholine persists
by the enzyme
which is attached
mainly to the spongy layer of fine connective tissue
that fills the synaptic space between the presynaptic
nerve terminal and the postsynaptic muscle mem-
of the synaptic space and is then no longer available
synaptic space—a few milliseconds at most—normally
removal of the acetylcholine prevents continued
muscle re-excitation after the muscle fiber has re-
covered from its initial action potential.
fiber when the acetylcholine channels open causes the
electrical potential inside the fiber at the local area of
the end plate to increase in the positive direction as
local potential
called the end plate potential. Recall from Chapter 5
that a sudden increase in nerve membrane potential
of more than 20 to 30 millivolts is normally sufficient
thus initiating an action potential at the muscle fiber
end plate potential B is much stronger and causes
enough sodium channels to open so that the self-
regenerative effect of more and more sodium ions
Ach
Na
+
A
–
–
–
–
–
–
–
–
–
–
–
–
B
channel mouth that prevent passage of negative ions such as
(Ach) has become attached and a conformational change has
Figure 7–3
Acetylcholine channel. A, Closed state. B, After acetylcholine
opened the channel, allowing sodium ions to enter the muscle
fiber and excite contraction. Note the negative charges at the
chloride ions.
fiber as does acetylcholine. The difference between
nicotine,
bachol,
methacholine, car-
Many compounds, including
Neuromuscular Junction
Block Transmission at the
release.
they are then ready for a new cycle of acetylcholine
is transported to the interior of these vesicles, and
vesicles. Within another few seconds, acetylcholine
to the interior of the membrane, thus forming new
original vesicles. Within about 20 seconds, the
nerve ending, especially the protein
membrane, caused by contractile proteins in the
over, “coated pits” appear in the terminal nerve
Within a few seconds after each action potential is
junction, new vesicles need to be re-formed rapidly.
few thousand nerve-to-muscle impulses. Therefore,
4. The number of vesicles available in the nerve
milliseconds.
reused to form new acetylcholine. This sequence of
into acetate ion and choline, and the choline is
action potential. Then, after a few milliseconds, the
of acetylcholine into the synaptic space.
fusion makes many of the vesicles rupture, allowing
the terminal membrane about 10,000-fold. This
increases about 100-fold, which in turn increases
calcium channels. As a result, the calcium ion
terminal, it opens many calcium channels in the
3. When an action potential arrives at the nerve
each vesicle.
form, about 10,000 molecules of acetylcholine in
interior, where it is stored in highly concentrated
2. Acetylcholine is synthesized in the cytosol of the
muscle end plate.
nerve fibers. About 300,000 of these small vesicles
are then transported by axoplasm that “streams”
the motoneuron in the spinal cord. These vesicles
1. Small vesicles, about 40 nanometers in size, are
cal transmission have been worked out. The formation
be studied easily, it is one of the few synapses of the
Acetylcholine Formation
exhausting levels of muscle activity.
junction occurs rarely, and even then only at the most
conditions, measurable fatigue of the neuromuscular
synapses are overexcited. Under normal functioning
lar junction, and it is the same effect that causes fatigue
muscle fiber. This is called
However, stimulation of the nerve fiber
safety factor.
required to stimulate the muscle fiber. Therefore, the
Ordinarily, each impulse that
Safety Factor for Transmission at the Neuromuscular Junction;
nerve terminals.
botulinum toxin,
peting for the acetylcholine receptor sites. The weak-
curare,
point A was caused by poisoning of the muscle fiber
potential. The weakness of the end plate potential at
Membrane Physiology, Nerve, and Muscle
88
Unit II
flowing to the interior of the fiber initiates an action
with
a drug that blocks the gating action of
acetylcholine on the acetylcholine channels by com-
ness of the end plate potential at point C resulted from
the effect of
a bacterial poison that
decreases the quantity of acetylcholine release by the
Fatigue of the Junction.
arrives at the neuromuscular junction causes about
three times as much end plate potential as that
normal neuromuscular junction is said to have a high
at rates greater than 100 times per second for several
minutes often diminishes the number of acetylcholine
vesicles so much that impulses fail to pass into the
fatigue of the neuromuscu-
of synapses in the central nervous system when the
Molecular Biology of
and Release
Because the neuromuscular junction is large enough to
nervous system for which most of the details of chemi-
and release of acetylcholine at this junction occur in the
following stages:
formed by the Golgi apparatus in the cell body of
through the core of the axon from the central
cell body in the spinal cord all the way to the
neuromuscular junction at the tips of the peripheral
collect in the nerve terminals of a single skeletal
nerve fiber terminal but is immediately transported
through the membranes of the vesicles to their
membrane of the nerve terminal because this
terminal has an abundance of voltage-gated
concentration inside the terminal membrane
the rate of fusion of the acetylcholine vesicles with
exocytosis
About 125 vesicles usually rupture with each
acetylcholine is split by acetylcholinesterase
reabsorbed actively into the neural terminal to be
events occurs within a period of 5 to 10
ending is sufficient to allow transmission of only a
for continued function of the neuromuscular
clathrin, which
is attached to the membrane in the areas of the
proteins contract and cause the pits to break away
Drugs That Enhance or
Drugs That Stimulate the Muscle Fiber by Acetylcholine-Like
Action.
and
have the same effect on the muscle
+ 20
+ 40
+ 60
0
15
30
45
60
75
Milliseconds
Millivolts
C
B
A
0
– 20
– 40
– 60
– 80
–100
toxin that decreases end plate release of acetylcholine, again too
Weakened end plate potential caused by botulinum
Normal end plate potential eliciting a muscle action
tial recorded in a curarized muscle, too weak to elicit an action
Weakened end plate poten-
Figure 7–4
End plate potentials (in millivolts). A,
potential. B,
potential. C,
weak to elicit a muscle action potential.
internal extensions of the cell membrane. Therefore,
lumens. In other words, the T tubules are actually
the extracellular fluid surrounding the muscle fiber,
Therefore, they communicate with
of the muscle fiber.
from the cell membrane, they are open to the exterior
where the T tubules originate
separate myofibrils. Also,
of T tubules interlacing among all the
side. Not shown in the figure is the fact that these
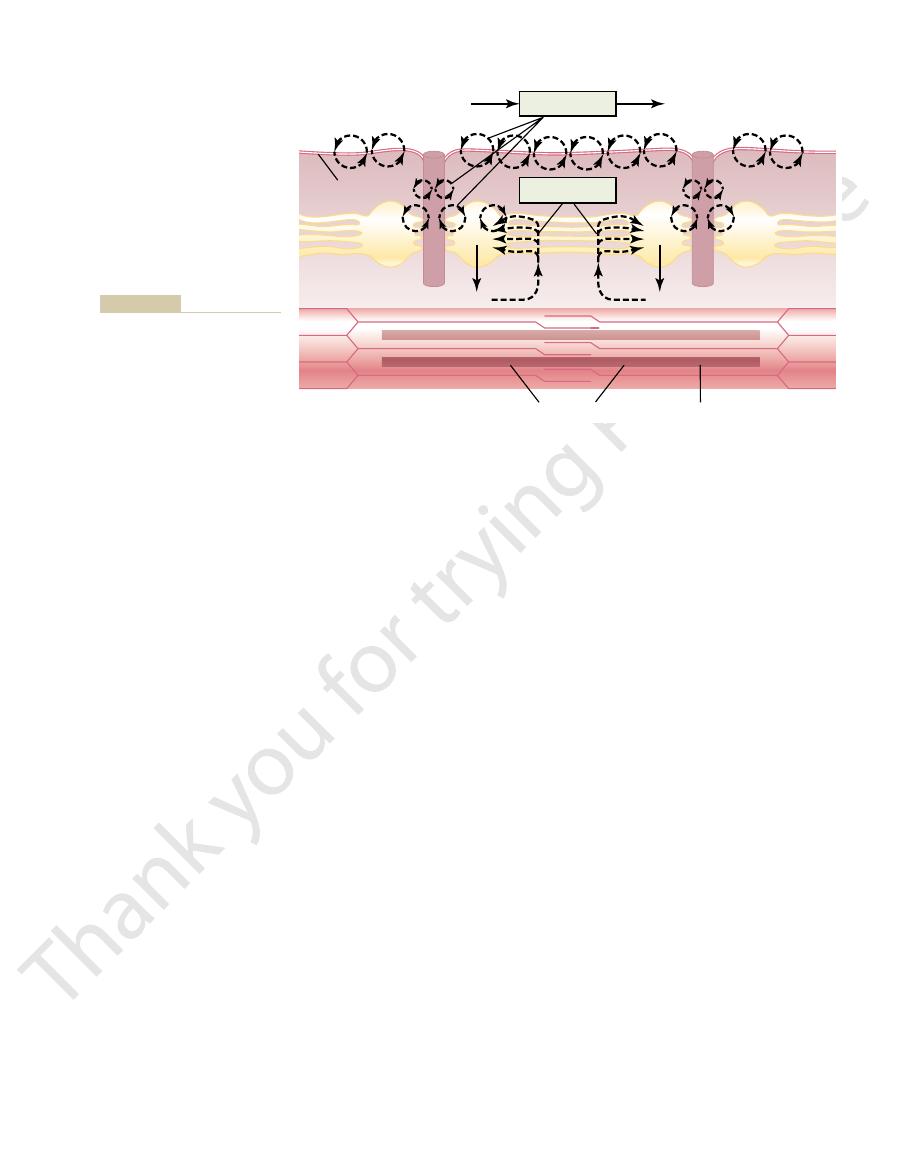
They begin at the cell membrane and penetrate all the
are very small and run transverse to the myofibrils.
tubule–sarcoplasmic reticulum system. The T tubules
Figure 7–5 shows myofibrils surrounded by the T
Reticulum System
Transverse Tubule–Sarcoplasmic
coupling.
ions then cause contraction. This overall process is
immediate vicinity of the myofibrils, and these calcium
Figure 7–5. The T tubule action potentials cause
from one side of the fiber to the other, as illustrated in
separate myofibrils. This is achieved by transmission of
cause maximum muscle contraction, current must pen-
almost no current flow deep within the fiber. Yet, to
The skeletal muscle fiber is so large that action poten-
“Transverse Tubules”
Interior of the Muscle Fiber by Way of
Spread of the Action Potential to the
nerve fibers that excite skeletal muscle.
3. Velocity of conduction: 3 to 5 m/sec—about 1/13
large myelinated nerves.
2. Duration of action potential: 1 to 5 milliseconds in
myelinated nerve fibers.
1. Resting membrane potential: about –80 to –90
for quantitative differences. Some of the quantitative
fibers applies equally to skeletal muscle fibers, except
few hours later.
normally, until a new dose of neostigmine is required a
mulate in the synaptic space. Within minutes, some of
or some other anticholinesterase drug, which allows
the respiratory muscles. The disease usually can be ame-
the patient dies of paralysis—in particular, paralysis of
late the muscle fibers. If the disease is intense enough,
Regardless of the cause, the end plate potentials that
acetylcholine-activated ion channels.
myasthenia gravis. Therefore, it is believed that myas-
fibers. Pathologically, antibodies that attack the acetyl-
20,000 persons, causes muscle paralysis because of
Myasthenia gravis,
tors, thus preventing sufficient increase in permeability
muscle. For instance, D-tubocurarine blocks the action
Drugs That Block Transmission at the Neuromuscular Junction.
cholinesterase for weeks, which makes this a particu-
as a powerful “nerve” gas poison, inactivates acetyl-
propyl fluorophosphate, which has military potential
esterase once again becomes active. Conversely, diiso-
for up to several hours, after which these drugs are
due to laryngeal spasm, which smothers the person.
reach the muscle. Unfortunately, it also can cause death
lates and stimulates the muscle fiber repetitively. This
sive nerve impulse, additional acetylcholine accumu-
hydrolyzes acetylcholine. Therefore, with each succes-
diisopropyl fluorophosphate,
neostigmine,
physostigmine,
known drugs,
Three particularly well-
virtue of leaking ions, initiate a new action potential,
from a previous contraction, these depolarized areas, by
are located. Then, every time the muscle fiber recovers
several hours. The drugs work by causing localized areas
Excitation of Skeletal Muscle: Neuromuscular Transmission and Excitation-Contraction Coupling
Chapter 7
89
these drugs and acetylcholine is that the drugs are not
destroyed by cholinesterase or are destroyed so slowly
that their action often persists for many minutes to
of depolarization of the muscle fiber membrane at the
motor end plate where the acetylcholine receptors
thereby causing a state of muscle spasm.
Drugs That Stimulate the Neuromuscular Junction by
Inactivating Acetylcholinesterase.
and
inactivate the acetyl-
cholinesterase in the synapses so that it no longer
causes muscle spasm when even a few nerve impulses
Neostigmine and physostigmine combine with acetyl-
cholinesterase to inactivate the acetylcholinesterase
displaced from the acetylcholinesterase so that the
larly lethal poison.
A
group of drugs known as curariform drugs can prevent
passage of impulses from the nerve ending into the
of acetylcholine on the muscle fiber acetylcholine recep-
of the muscle membrane channels to initiate an action
potential.
Myasthenia Gravis
which occurs in about 1 in every
inability of the neuromuscular junctions to transmit
enough signals from the nerve fibers to the muscle
choline-gated sodium ion transport proteins have been
demonstrated in the blood of most patients with
thenia gravis is an autoimmune disease in which the
patients have developed immunity against their own
occur in the muscle fibers are mostly too weak to stimu-
liorated for several hours by administering neostigmine
larger than normal amounts of acetylcholine to accu-
these paralyzed people can begin to function almost
Muscle Action Potential
Almost everything discussed in Chapter 5 regarding
initiation and conduction of action potentials in nerve
aspects of muscle potentials are the following:
millivolts in skeletal fibers—the same as in large
skeletal muscle—about five times as long as in
the velocity of conduction in the large myelinated
tials spreading along its surface membrane cause
etrate deeply into the muscle fiber to the vicinity of the
action potentials along transverse tubules (T tubules)
that penetrate all the way through the muscle fiber
release of calcium ions inside the muscle fiber in the
called excitation-contraction
Excitation-Contraction
Coupling
way from one side of the muscle fiber to the opposite
tubules branch among themselves so that they form
entire planes
and they themselves contain extracellular fluid in their
when an action potential spreads over a muscle fiber
Conversely, full excitation of the T tubule and
ited and maintains a relaxed state of the muscle.
little to elicit contraction. Therefore, the troponin-
ions in the cytosol that bathes the myofibrils is too
The normal resting
Excitatory “Pulse” of Calcium Ions.
the tubules. In addition, inside the reticulum is a
brils back into the sarcoplasmic tubules. This pump can
high concentration. However, a continually active
have diffused among the myofibrils, muscle contrac-
traction, as discussed in Chapter 6.
this time, enough calcium ions are released into the
channels remain open for a few milliseconds; during
well as their attached longitudinal tubules. These
ticular cisternae where they abut the T tubule. This in
Figure 7–6 shows that the action potential of the T
potential occurs in the adjacent T tubule.
calcium ions in high concentration, and many of these
Release of Calcium Ions by the
round all surfaces of the actual contracting myofibrils.
tubules, and (2) long longitudinal tubules that sur-
that abut the T
yellow. This is composed of two major parts: (1) large
Figure 7–5 also shows a
electrical currents surrounding these T tubules then
T tubules to the deep interior of the muscle fiber. The
membrane, a potential change also spreads along the
Membrane Physiology, Nerve, and Muscle
90
Unit II
elicit the muscle contraction.
sarcoplasmic reticulum, in
chambers called terminal cisternae
Sarcoplasmic Reticulum
One of the special features of the sarcoplasmic reticu-
lum is that within its vesicular tubules is an excess of
ions are released from each vesicle when an action
tubule causes current flow into the sarcoplasmic re-
turn causes rapid opening of large numbers of calcium
channels through the membranes of the cisternae as
sarcoplasm surrounding the myofibrils to cause con-
Calcium Pump for Removing Calcium Ions from the Myofibrillar
Fluid After Contraction Occurs.
Once the calcium ions
have been released from the sarcoplasmic tubules and
tion continues as long as the calcium ions remain in
calcium pump located in the walls of the sarcoplasmic
reticulum pumps calcium ions away from the myofi-
concentrate the calcium ions about 10,000-fold inside
protein called calsequestrin that can bind up to 40
times more calcium.
state concentration (less than 10
-7
molar) of calcium
tropomyosin complex keeps the actin filaments inhib-
sarcoplasmic reticulum system causes enough re-
lease of calcium ions to increase the concentration
in the myofibrillar fluid to as high as 2
¥ 10
-4
molar
Terminal
Transverse
Transverse
Triad of the
A band
I band
Sarcotubules
Myofibrils
Z line
reticulum
Sarcolemma
tubule
tubule
cisternae
Mitochondrion
Sarcoplasmic
reticulum
Colard Keene.)
DW: A Textbook of Histology.
(Redrawn from Bloom W, Fawcett
two T tubules per sarcomere,
mammalian heart muscle, but
sarcomere, located at the Z line. A
This illustration was drawn from frog
tubules that surround all sides of
longitudinal sarcoplasmic reticulum
deep in the muscle fiber, each T
mic reticulum system. Note that
Transverse (T) tubule–sarcoplas-
Figure 7–5
the T tubules communicate with the
outside of the cell membrane, and
tubule lies adjacent to the ends of
the actual myofibrils that contract.
muscle, which has one T tubule per
similar arrangement is found in
mammalian skeletal muscle has
located at the A-I band junctions.
Philadelphia: WB Saunders, 1986.
Modified after Peachey LD: J Cell
Biol 25:209, 1965. Drawn by Sylvia
Sci 998:324, 2003.
myasthenia gravis and related disorders. Ann N Y Acad
Vincent A, McConville J, Farrugia ME, et al: Antibodies in
gravis. Nat Rev Immunol 10:797, 2002.
Vincent A: Unraveling the pathogenesis of myasthenia
74:899, 1994.
the vertebrate neuromuscular junction. Physiol Rev
Van der Kloot W, Molgo J: Quantal acetylcholine release at
FEBS Lett 555:106, 2003.
-ATPase of sarcoplasmic reticulum.
Toyoshima C, Nomura H, Sugita Y: Structural basis of ion
Biosci 7:583, 2002.
proteins involved in excitation-contraction coupling. Front
Tang W, Sencer S, Hamilton SL: Calmodulin modulation of
Pharmacol Sci 23:569, 2002.
control of skeletal muscle fiber type and size. Trends
Schiaffino S, Serrano A: Calcineurin signaling and neural
motoneuronal excitability. Physiol Rev 80:767, 2000.
Rekling JC, Funk GD, Bayliss DA, et al: Synaptic control of
skeletal muscle. J Appl Physiol 90:1119, 2001.
Pette D: Historical perspectives: plasticity of mammalian
Sport Sci Rev 32:36, 2004.
contraction uncoupling in aging skeletal muscle. Exerc
Payne AM, Delbono O: Neurogenesis of excitation-
111:436, 2003.
channel function via channel dysfunction. J Clin Invest
Leite JF, Rodrigues-Pinguet N, Lester HA: Insights into
98:143, 2003.
neuromuscular blocking muscle relaxants. Pharmacol Ther
Lee C: Conformation, action, and mechanism of action of
thenia gravis. Muscle Nerve 29:484, 2004.
Keesey JC: Clinical evaluation and management of myas-
formation. Trends Neurosci 26:335, 2003.
Hoch W: Molecular dissection of neuromuscular junction
control. J Appl Physiol 96:407, 2004.
Haouzi P, Chenuel B, Huszczuk A: Sensing vascular disten-
neuromuscular junction. Ann N Y Acad Sci 998:138,
thenic syndromes: multiple molecular targets at the
Engel AG, Ohno K, Shen XM, Sine SM: Congenital myas-
Lancet 363:978, 2004.
Chaudhuri A, Behan PO: Fatigue in neurological disorders.
cular dystrophies. Annu Rev Med 48:457, 1997.
Brown RH Jr: Dystrophin-associated proteins and the mus-
York: Churchill Livingstone, 1998.
Amonof MJ: Electromyography in Clinical Practice. New
central and peripheral factors. Muscle Nerve 25:785, 2002.
Allman BL, Rice CL: Neuromuscular fatigue and aging:
action potentials, as discussed in Chapter 6.
ruption for long intervals, a series of calcium pulses
occurs. If the contraction is to continue without inter-
During this calcium pulse, muscle contraction
about 1/3 of a second because of the long duration of
less in others. (In heart muscle, the calcium pulse lasts
lasts about 1/20 of a second, although it may last
this calcium “pulse” in the usual
depletes the calcium ions again. The total duration of
contraction. Immediately thereafter, the calcium pump
concentration, a 500-fold increase, which is about 10
Excitation of Skeletal Muscle: Neuromuscular Transmission and Excitation-Contraction Coupling
Chapter 7
91
times the level required to cause maximum muscle
skeletal muscle fiber
several times as long in some fibers and several times
the cardiac action potential.)
must be initiated by a continuous series of repetitive
References
Also see references for Chapters 5 and 6.
2003.
sion in skeletal muscle by slow conducting afferent fibers:
neurophysiological basis and implication for respiratory
pumping by Ca
2
+
ATP
Action potential
Calcium pump
required
Actin filaments
Sarcolemma
Myosin filaments
Ca
Ca
Ca
++
Ca
++
calcium pump.
mic reticulum and then (2) re-
calcium ions from the sarcoplas-
potential that causes release of
Figure 7–6
Excitation-contraction coupling in
the muscle, showing (1) an action
uptake of the calcium ions by a
