causes rapid loss of fluid into the urine. In patients with diabetes mellitus, the high
instead, the excess glucose remains in the tubules, acts as an osmotic diuretic, and
centration of about 250 mg/dl, little of the extra glucose is reabsorbed by the tubules;
for glucose). Above a plasma glucose con-
(i.e., exceeds their
blood glucose concentration rises to high levels in diabetes mellitus, the increased
solutes that fail to be reabsorbed from the tubular fluid. For example, when the
tubular fluid into the urine.
of these solutes then greatly reduces water reabsorption, flushing large amounts of
concentration of osmotically active molecules in the tubules. The osmotic pressure
renal tubules, such as urea, mannitol, and sucrose, causes a marked increase in the
by Increasing Osmotic Pressure of Tubular Fluid
Osmotic Diuretics Decrease Water Reabsorption
in Table 31–1.
nephron. The general classes of diuretics and their mechanisms of action are shown
and, therefore, inhibit tubular reabsorption at different sites along the renal
The many diuretics available for clinical use have different mechanisms of action
prompted the use of diuretics in the first place.
cellular fluid volume have occurred, relieving the hypertension or edema that
becomes equal to intake, but only after reductions in arterial pressure and extra-
chronic effects of the diuretic on urine output. Thus, in the steady state, urine output
angiotensin II formation; all these responses, together, eventually override the
volume. For example, a decrease in extracellular fluid volume often reduces arterial
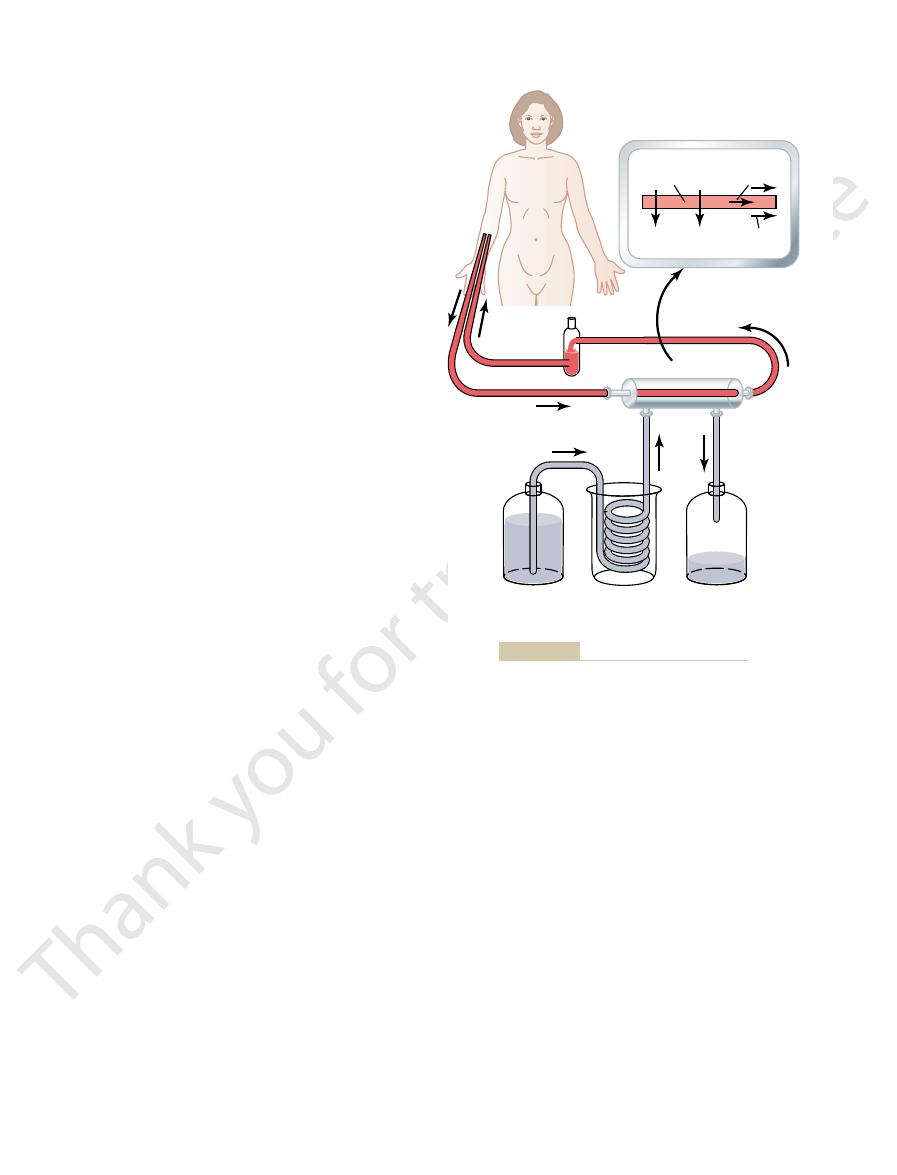
of salt and water subsides within a few days (Figure 31–1). This is due to activation
after they are administered. However, the effect of most diuretics on renal output
volume; therefore, diuretics are most often administered in clinical conditions in
Chapter 25, loss of sodium from the body mainly decreases extracellular fluid
especially in diseases associated with edema and hypertension. As discussed in
The most common clinical use of diuretics is to reduce extracellular fluid volume,
ondarily by sodium reabsorption, many diuretics raise renal output of these solutes
solutes, such as potassium, chloride, magnesium, and calcium, is also influenced sec-
decrease water reabsorption. Because the renal tubular reabsorption of many
sodium reabsorption, because sodium remaining in the tubules acts osmotically to
most cases, increased water output occurs secondary to inhibition of tubular
sodium output), which in turn causes diuresis (increased water output). That is, in
from the tubules, which causes natriuresis (increased
and chloride. In fact, most diuretics that are used clin-
increase urinary excretion of solutes, especially sodium
volume output, as the name implies. Most diuretics also
Diuretics and Their
C
H
A
P
T
E
R
3
1
402
Kidney Diseases and Diuretics
Mechanisms of Action
A diuretic is a substance that increases the rate of urine
ically act by decreasing the rate of sodium reabsorption
as well.
which extracellular fluid volume is expanded.
Some diuretics can increase urine output more than 20-fold within a few minutes
of other compensatory mechanisms initiated by decreased extracellular fluid
pressure and glomerular filtration rate (GFR) and increases renin secretion and
Injection into the blood stream of substances that are not easily reabsorbed by the
Large volumes of urine are also formed in certain diseases associated with excess
filtered load of glucose into the tubules exceeds their capacity to reabsorb glucose
transport maximum
minutes.
the urine, causing, under acute conditions, urine output
of Henle. Because of these multiple effects, 20 to 30 per
of the kidneys is also greatly reduced. In addition,
is decreased, so that the maximal concentrating ability
quently, reabsorption of fluid from the collecting ducts
fore renal medullary osmolarity, is reduced. Conse-
interstitial fluid concentration of these ions, and there-
excreted along with increased water excretion. Urinary
or dilute the urine. Urinary dilution is impaired because
interstitial fluid. Because of this effect, loop diuretics
tion as well; and (2) they disrupt the countercurrent
solutes delivered to the distal parts of the nephrons, and
two reasons: (1) they greatly increase the quantities of
potassium, and other electrolytes, as well as water, for
the loop diuretics raise urine output of sodium, chloride,
transport in the luminal membrane of the loop of Henle,
ically used diuretics.
These diuretics are among the most powerful of the clin-
located in the luminal membrane of the epithelial cells.
the 1-sodium, 2-chloride, 1-potassium co-transporter
Furosemide, ethacrynic acid,
Ascending Loop of Henle
Reabsorption in the Thick
“Loop” Diuretics Decrease Active
Chapter 31
Kidney Diseases and Diuretics
403
urine output is balanced by a high level of fluid intake
owing to activation of the thirst mechanism.
Sodium-Chloride-Potassium
and bumetanide are power-
ful diuretics that decrease active reabsorption in the
thick ascending limb of the loop of Henle by blocking
By blocking active sodium-chloride-potassium co-
these act as osmotic agents to prevent water reabsorp-
multiplier system by decreasing absorption of ions from
the loop of Henle into the medullary interstitium,
thereby decreasing the osmolarity of the medullary
impair the ability of the kidneys to either concentrate
the inhibition of sodium and chloride reabsorption in
the loop of Henle causes more of these ions to be
concentration is impaired because the renal medullary
decreased renal medullary interstitial fluid osmolarity
reduces absorption of water from the descending loop
cent of the glomerular filtrate may be delivered into
to be as great as 25 times normal for at least a few
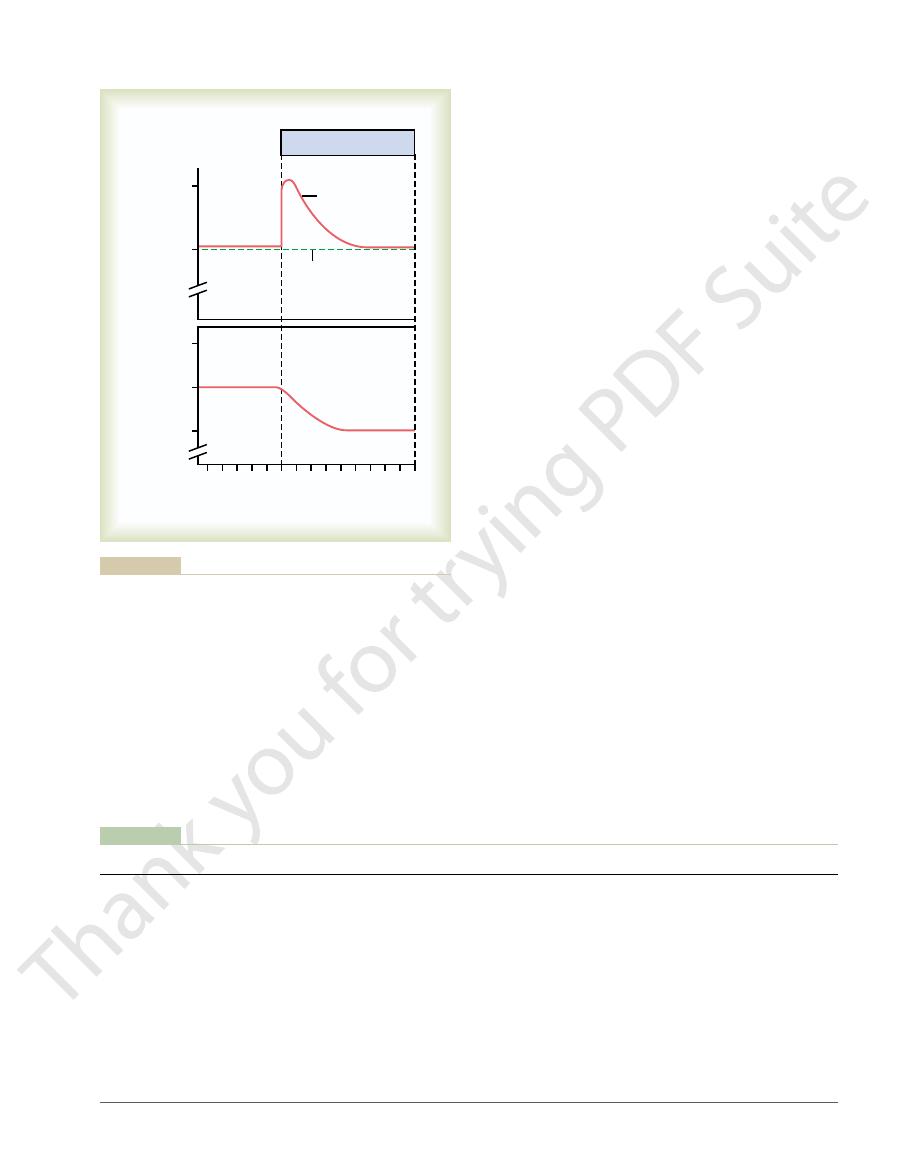
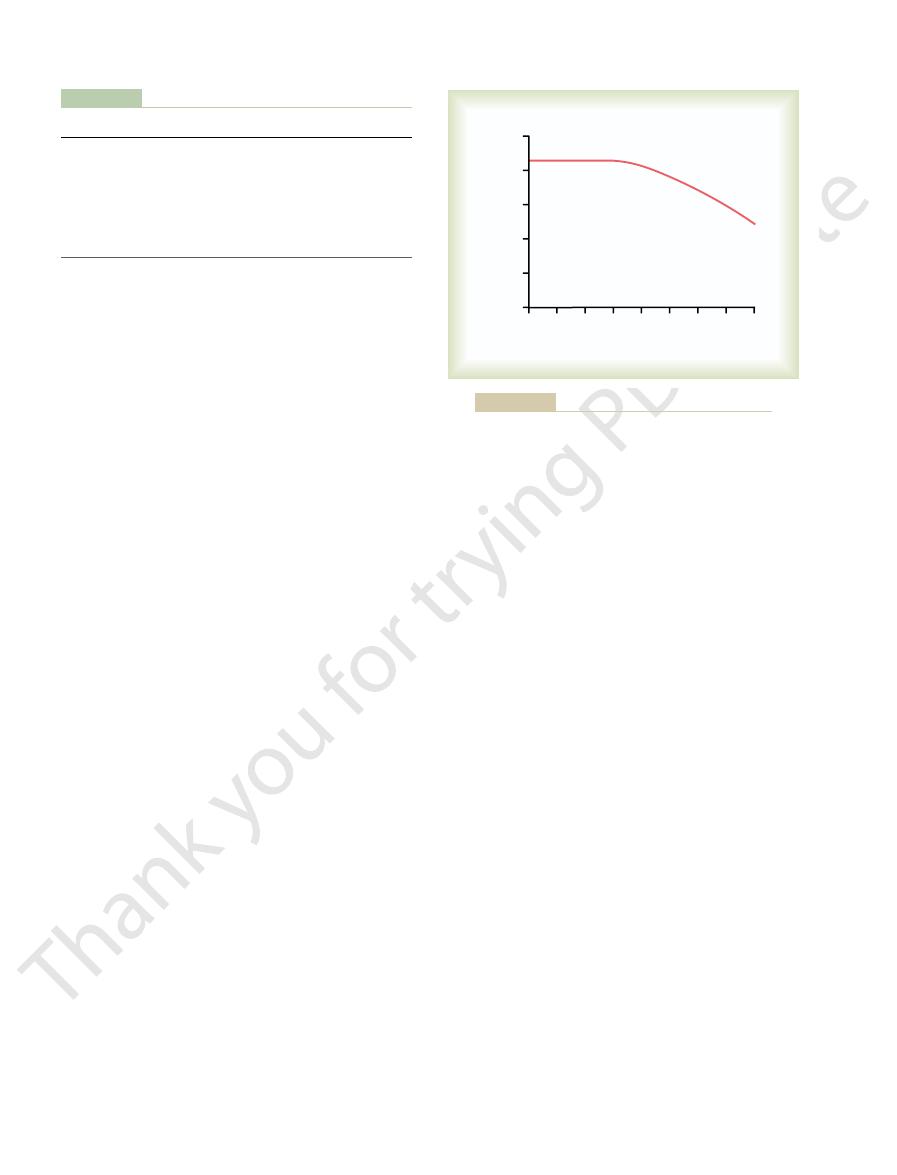
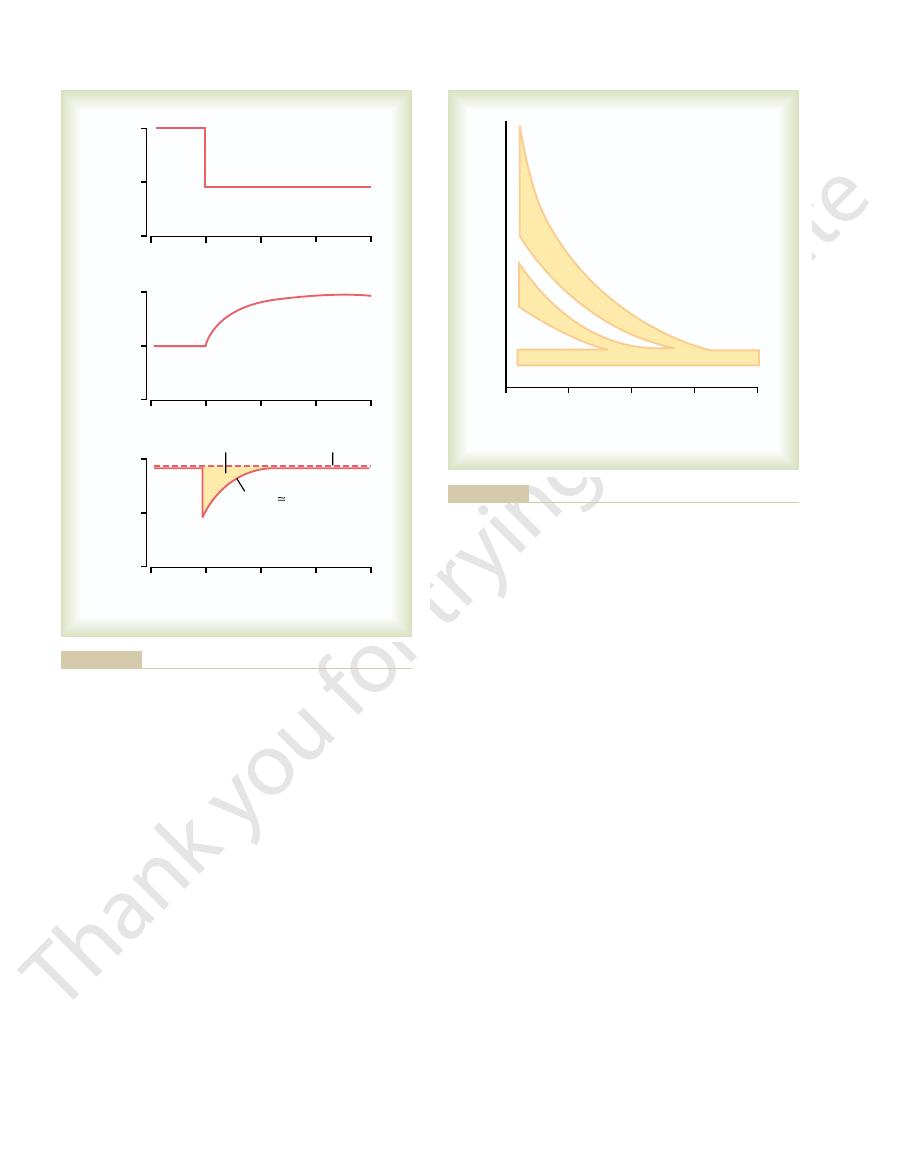
Time (days)
Extracellular fluid
volume (liters)
Sodium excretion or
sodium intake (mEq/day)
200
100
15.0
14.0
13.0
8
6
4
2
0
-
4
-
2
Excretion
Intake
Diuretic therapy
re-establishing sodium balance.
eventually return sodium excretion to equal sodium intake, thus
sodium intake is held constant, compensatory mechanisms will
accompanied by a decrease in extracellular fluid volume. If
administration. The immediate increase in sodium excretion is
Sodium excretion and extracellular fluid volume during diuretic
Figure 31–1
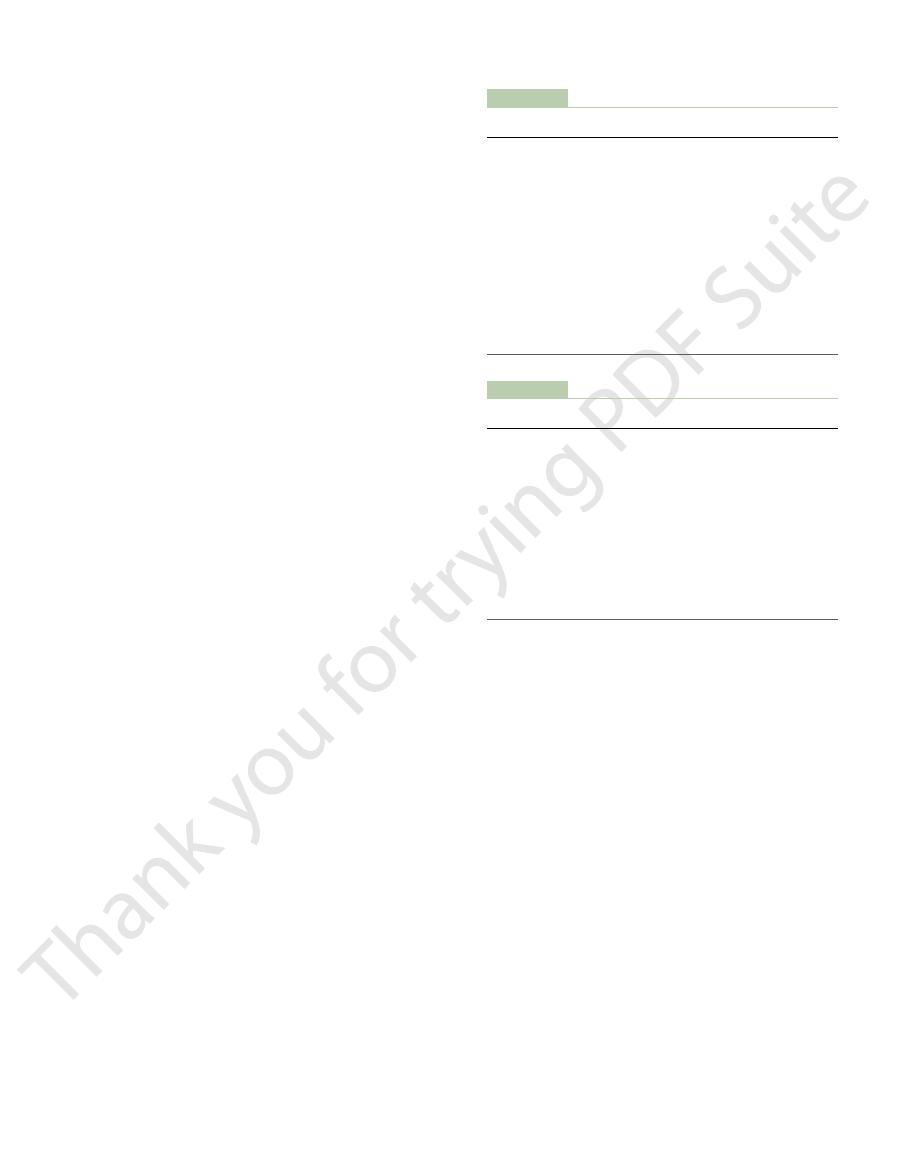
Table 31–1
reabsorption, and
(triamterene, amiloride)
membrane, decrease Na
channels of luminal
Collecting tubules
Sodium channel blockers
Block entry of Na
reabsorption, and decrease
(spironolactone, eplerenone)
decrease Na
Aldosterone antagonists
Inhibit action of aldosterone on tubular receptor,
Collecting tubules
(acetazolamide)
reduces Na
reabsorption, which Proximal
tubules
Carbonic anhydrase inhibitors
Inhibit H
co-transport in luminal membrane
Early distal tubules
Thiazide diuretics (hydrochlorothiazide,
Inhibit Na
co-transport in luminal membrane
Thick ascending loop of Henle
Loop diuretics (furosemide, bumetanide)
Inhibit Na
Osmotic diuretics (mannitol)
Inhibit water and solute reabsorption by increasing
Mainly proximal tubules
Class of Diuretic
Mechanism of Action
Tubular Site of Action
Classes of Diuretics, Their Mechanisms of Action, and Tubular Sites of Action
osmolarity of tubular fluid
+
-K
+
-Cl
-
+
-Cl
-
chlorthalidone)
+
secretion and HCO
3
–
+
reabsorption
+
K
+
secretion
+
into Na
+
+
decrease K
+
secretion
Postrenal acute renal failure,
tubules.
those that affect the blood vessels, glomeruli, or
abnormalities within the kidney itself, including
blood pressure, such as severe hemorrhage.
the kidneys. This can be a
blood supply to the kidneys; this condition is
1. Acute renal failure resulting from decreased
The causes of acute renal failure can be divided into
Acute Renal Failure
important types of kidney diseases.
and bladder. In this chapter, we discuss specific physi-
urinary tract outside the kidney, including the ureters
glomeruli, tubules, renal interstitium, and parts of the
diseases that can affect the kidney blood vessels,
two general categories, there are many specific kidney
ually decreases overall kidney function. Within these
chronic renal failure,
may eventually recover nearly normal function, and
acute renal failure,
categories: (1)
to have chronic kidney disease.
throughout the world. For example, in 2004, more than
tubular fluid. For this reason, the sodium channel block-
adenosine triphosphatase pump. This decreased activity
therefore, decreased activity of the sodium-potassium-
into the epithelial cells, there is also decreased sodium
epithelial cells. Because of this decreased sodium entry
However, at the cellular level, these drugs act directly
tubules, similar to the effects of spironolactone.
Channels in the Collecting Tubules
contrast to the aldosterone antagonists, which “spare”
other diuretics cause loss of potassium in the urine, in
potassium-sparing diuretics.
centration to increase excessively. For this reason,
instances, this causes extracellular fluid potassium con-
sium from the cells to the extracellular fluid. In some
the tubules, they decrease the excretion of potassium.
well as sodium. Because these drugs also block the
osmotic diuretic, causing increased excretion of water as
sequence, sodium remains in the tubules and acts as an
secretion of potassium in this tubular segment.As a con-
therefore, can decrease the reabsorption of sodium and
Collecting Tubule
Secretion into the Cortical
Reabsorption from and Potassium
ions in the urine.
diuretic. Predictably, a disadvantage of the carbonic
sodium reabsorption. The blockage of sodium and
counter-transport mechanism in the luminal membrane,
lecting tubule.
tubular cells, such as in the intercalated cells of the col-
primary site of action of carbonic anhydrase inhibitors.
bonic anhydrase is abundant in the proximal tubule, the
the proximal tubule, as discussed in Chapter 30. Car-
carbonic anhydrase,
Acetazolamide
Tubules
Carbonic Anhydrase Inhibitors
normally reabsorbed by the distal tubules.
into the urine. This is about the same amount of sodium
tubular cells. Under favorable conditions, these agents
The thiazide derivatives, such as chlorothiazide, act
Distal Tubule
404
Unit V
The Body Fluids and Kidneys
Thiazide Diuretics Inhibit Sodium-
Chloride Reabsorption in the Early
mainly on the early distal tubules to block the sodium-
chloride co-transporter in the luminal membrane of the
cause 5 to 10 per cent of the glomerular filtrate to pass
Block Sodium-Bicarbonate
Reabsorption in the Proximal
inhibits the enzyme
which is critical for the reabsorption of bicarbonate in
Some carbonic anhydrase is also present in other
Because hydrogen ion secretion and bicarbonate
reabsorption in the proximal tubules are coupled to
sodium reabsorption through the sodium-hydrogen ion
decreasing bicarbonate reabsorption also reduces
bicarbonate reabsorption from the tubular fluid causes
these ions to remain in the tubules and act as an osmotic
anhydrase inhibitors is that they cause some degree of
acidosis because of the excessive loss of bicarbonate
Competitive Inhibitors of
Aldosterone Decrease Sodium
Spironolactone and eplerenone are aldosterone antago-
nists that compete with aldosterone for receptor sites
in the cortical collecting tubule epithelial cells and,
effect of aldosterone to promote potassium secretion in
Aldosterone antagonists also cause movement of potas-
spironolactone and other aldosterone inhibitors are
referred to as
Many of the
the loss of potassium.
Diuretics That Block Sodium
Decrease Sodium Reabsorption
Amiloride and triamterene also inhibit sodium reab-
sorption and potassium secretion in the collecting
to block the entry of sodium into the sodium channels
of the luminal membrane of the collecting tubule
transport across the cells’ basolateral membranes and,
reduces the transport of potassium into the cells and
ultimately decreases the secretion of potassium into the
ers are also potassium-sparing diuretics and decrease
the urinary excretion rate of potassium.
Kidney Diseases
Diseases of the kidneys are among the most important
causes of death and disability in many countries
20 million adults in the United States were estimated
Severe kidney diseases can be divided into two main
in which the kidneys
abruptly stop working entirely or almost entirely but
(2)
in which there is progressive
loss of function of more and more nephrons that grad-
ologic abnormalities that occur in a few of the more
three main categories:
often referred to as prerenal acute renal failure
to reflect the fact that the abnormality occurs
in a system before
consequence of heart failure with reduced cardiac
output and low blood pressure or conditions
associated with diminished blood volume and low
2. Intrarenal acute renal failure resulting from
3.
resulting from
obstruction of the urinary collecting system
proliferate, but mainly the mesangial cells that lie
glomeruli, many of the cells of the glomeruli begin to
in the glomeruli, especially in the basement membrane
that damages the kidneys. Instead, over a few weeks, as
coccal infection of the skin. It is not the infection itself
cal sore throat, streptococcal tonsillitis, or even strepto-
streptococci. The infection may have been a streptococ-
body, usually caused by certain types of group A beta
patients with this disease, damage to the glomeruli
that damages the glomeruli. In about 95 per cent of the
of intrarenal acute renal failure are listed in Table 31–3.
can lead to damage of the renal blood vessels. Causes
lead to tubular damage, and primary tubular damage
interdependent, damage to the renal blood vessels can
tion refers to the primary site of injury, but because the
damage to the renal interstitium. This type of classifica-
renal tubular epithelium, and (3) conditions that cause
other small renal vessels, (2) conditions that damage the
This category of
intrarenal acute renal failure.
Within the Kidney
Caused by Abnormalities
Intrarenal Acute Renal Failure
failure.
patients. Table 31–2 shows some of the common causes
cussed later. Acute reduction of renal blood flow is a
can evolve into intrarenal acute renal failure, as dis-
persists longer than a few hours, this type of renal failure
tubular epithelial cells. If the cause of prerenal acute
damage or even death of the renal cells, especially the
decreases in renal blood flow, if prolonged, will cause
flow, the renal cells start to become hypoxic, and further
reduced below this basal requirement, which is usually
they are not reabsorbing sodium. When blood flow is
reduced. As the GFR approaches zero, oxygen con-
kidney. Therefore, as renal blood flow and GFR fall,
that must be reabsorbed by the tubules, which uses most
reduced. This decreases the amount of sodium chloride
blood flow is reduced, the GFR and the amount of
the renal cells occurs. The reason for this is that as renal
Unlike some tissues, the kidney can endure a relatively
20 to 25 per cent of normal, acute renal failure can
output can occur, a condition referred to as
blood flow is markedly reduced, total cessation of urine
mulation of water and solutes in the body fluids. If renal
the level of intake of water and solutes.This causes accu-
of water and solutes. Consequently, conditions that
Therefore, decreased renal blood flow is usually accom-
lation of body fluid volumes and solute concentrations.
cardiac output.The main purpose of this high blood flow
of about 1100 ml/min, or about 20 to 25 per cent of the
The kidneys normally receive an abundant blood supply
Prerenal Acute Renal Failure
calcium, urate, or cystine.
are kidney stones, caused by precipitation of
the bladder. The most common causes of
Chapter 31
Kidney Diseases and Diuretics
405
anywhere from the calyces to the outflow from
obstruction of the urinary tract outside the kidney
Caused by Decreased Blood Flow
to the Kidney
to the kidneys is to provide enough plasma for the high
rates of glomerular filtration needed for effective regu-
panied by decreased GFR and decreased urine output
acutely diminish blood flow to the kidneys usually cause
oliguria, which refers to diminished urine output below
anuria.
As long as renal blood flow does not fall below about
usually be reversed if the cause of the ischemia is cor-
rected before damage to the renal cells has occurred.
large reduction in blood flow before actual damage to
sodium chloride filtered by the glomeruli (as well as
the filtration rate of water and other electrolytes) are
of the energy and oxygen consumed by the normal
the requirement for renal oxygen consumption is also
sumption of the kidney approaches the rate that is
required to keep the renal tubular cells alive even when
less than 20 to 25 per cent of the normal renal blood
renal failure is not corrected and ischemia of the kidney
common cause of acute renal failure in hospitalized
of decreased renal blood flow and prerenal acute renal
Abnormalities that originate within the kidney and that
abruptly diminish urine output fall into the general cat-
egory of
acute renal failure can be further divided into (1)
conditions that injure the glomerular capillaries or
renal vasculature and tubular system are functionally
Acute Renal Failure Caused by Glomerulonephritis.
Acute
glomerulonephritis is a type of intrarenal acute renal
failure usually caused by an abnormal immune reaction
occurs 1 to 3 weeks after an infection elsewhere in the
antibodies develop against the streptococcal antigen,
the antibodies and antigen react with each other to form
an insoluble immune complex that becomes entrapped
portion of the glomeruli.
Once the immune complex has deposited in the
Table 31–2
Renal artery stenosis, embolism, or thrombosis of renal artery
Primary renal hemodynamic abnormalities
Sepsis, severe infections
Peripheral vasodilation and resultant hypotension
Valvular damage
Cardiac failure
Hemorrhage (trauma, surgery, postpartum, gastrointestinal)
Intravascular volume depletion
Some Causes of Prerenal Acute Renal Failure
Diarrhea or vomiting
Burns
Myocardial infarction
Anaphylactic shock
Anesthesia
or vein
Table 31–3
glycol, insecticides, poison mushrooms, carbon tetrachloride)
Acute tubular necrosis due to toxins (heavy metals, ethylene
Tubular epithelial injury (tubular necrosis)
Vasculitis (polyarteritis nodosa)
Small vessel and/or glomerular injury
Some Causes of Intrarenal Acute Renal Failure
Cholesterol emboli
Malignant hypertension
Acute glomerulonephritis
Acute tubular necrosis due to ischemia
Renal interstitial injury
Acute pyelonephritis
Acute allergic interstitial nephritis
of chronic renal failure. In general, chronic renal
Table 31–4 gives some of the most important causes
75 per cent below normal. In fact, relatively normal
versible loss of large numbers of functioning nephrons.
Nephrons
An Irreversible Decrease
Chronic Renal Failure:
failure.
as well as treatment with an artificial kidney, are dis-
metabolism. Other effects of diminished urine output,
retained water, electrolytes, and waste products of
plete anuria occurs. The patient will die in 8 to 14 days
In the most severe cases of acute renal failure, com-
failure develop metabolic acidosis, which in itself can
sufficient hydrogen ions, patients with acute renal
fatal. Because the kidneys are also unable to excrete
to patients with acute renal failure, because increases
of potassium, however, is often a more serious threat
lead to edema and hypertension. Excessive retention
can lead to water and salt overload, which in turn can
waste products of metabolism, and electrolytes. This
retention in the blood and extracellular fluid of water,
Physiologic Effects of Acute
bladder obstruction, and (3) obstruction of the urethra.
renal pelvises caused by large stones or blood clots, (2)
kidney damage. Some of the causes of postrenal acute
lasting for several days or weeks, can lead to irreversible
hours. But chronic obstruction of the urinary tract,
failure, normal kidney function can be restored if the
extracellular fluid volume. With this type of renal
output of only one kidney is diminished, no major
and other functions are initially normal. If the urine
Lower Urinary Tract
Caused by Abnormalities of the
Postrenal Acute Renal Failure
10 to 20 days.
of the membrane, so that the tubule repairs itself within
is destroyed. If the basement membrane remains intact,
tubules. In some instances, the basement membrane also
death of many of them. As a result, the epithelial cells
toxic action on the renal tubular epithelial cells, causing
certain cancers. Each of these substances has a specific
-platinum, which is used in treating
antibiotics, and
(such as tetracyclines) used as
insecticides,
is a major component in antifreeze), various
carbon tetrachloride, heavy
failure. Some of these are
There is a long list of renal poisons and medications that
Acute Tubular Necrosis Caused by Toxins or Medications.
this chapter.
associated with circulatory shock, as discussed earlier in
normal, as long as the tubules remain plugged. The most
blocked nephrons; the affected nephrons often fail to
nephrons, so that there is no urine output from the
happens, tubular cells “slough off” and plug many of the
destruction of the epithelial cells can occur. When this
cells, and if the insult is prolonged, damage or eventual
impairs the blood supply to the kidney. If the ischemia
Acute Tubular Necrosis Caused by Severe Renal
epithelial cells.
poisons, toxins, or medications that destroy the tubular
tubules. Some common causes of tubular necrosis are
sis,
Tubular Necrosis as a Cause of Acute Renal Failure.
described in a subsequent section of this chapter.
chronic renal failure,
continues indefinitely, leading to
percentage of patients, progressive renal deterioration
glomeruli are destroyed beyond repair, and in a small
weeks to few months. Sometimes, however, many of the
sides in about 2 weeks, and in most patients, the kidneys
The acute inflammation of the glomeruli usually sub-
almost complete renal shutdown occurs.
the glomerular filtrate. In severe cases, either total or
permeable, allowing both protein and red blood cells to
become blocked by this inflammatory reaction, and
entrapped in the glomeruli. Many of the glomeruli
tion, large numbers of white blood cells become
between the endothelium and the epithelium. In addi-
406
Unit V
The Body Fluids and Kidneys
those that are not blocked usually become excessively
leak from the blood of the glomerular capillaries into
return to almost normal function within the next few
as
Another
cause of intrarenal acute renal failure is tubular necro-
which means destruction of epithelial cells in the
(1) severe ischemia and inadequate supply of oxygen
and nutrients to the tubular epithelial cells and (2)
Ischemia.
Severe ischemia of the kidney can result from
circulatory shock or any other disturbance that severely
is severe enough to seriously impair the delivery of
nutrients and oxygen to the renal tubular epithelial
excrete urine even when renal blood flow is restored to
common causes of ischemic damage to the tubular
epithelium are the prerenal causes of acute renal failure
can damage the tubular epithelium and cause acute renal
metals (such as mercury and lead), ethylene glycol (which
various medications
cis
slough away from the basement membrane and plug the
new tubular epithelial cells can grow along the surface
Multiple abnormalities in the lower urinary tract can
block or partially block urine flow and therefore lead to
acute renal failure even when the kidneys’ blood supply
change in body fluid composition will occur because the
contralateral kidney can increase its urine output suffi-
ciently to maintain relatively normal levels of extracel-
lular electrolytes and solutes as well as normal
basic cause of the problem is corrected within a few
failure include (1) bilateral obstruction of the ureters or
Renal Failure
A major physiologic effect of acute renal failure is
in plasma potassium concentration (hyperkalemia) to
more than about 8 mEq/L (only twice normal) can be
be lethal or can aggravate the hyperkalemia.
unless kidney function is restored or unless an artifi-
cial kidney is used to rid the body of the excessive
cussed in the next section in relation to chronic renal
in the Number of Functional
Chronic renal failure results from progressive and irre-
Serious clinical symptoms often do not occur until the
number of functional nephrons falls to at least 70 to
blood concentrations of most electrolytes and normal
body fluid volumes can still be maintained until the
number of functioning nephrons decreases below 20
to 25 per cent of normal.
As discussed in Chapter 78, type II diabetes, which is
approximately 70 per cent of all chronic renal failure.
of end-stage renal disease, together accounting for
disease. In recent years,
stage renal disease. In the early 1980s,
Table 31–5 gives the most common causes of end-
angiotensin II antagonists.
hydrostatic pressure, especially by using drugs such
disease (Figure 31–2). The only proven method
remaining nephrons, and a slowly progressing vicious
kidney function, further adaptive changes in the
ate the glomerulus, leading to further reduction in
tissue). These sclerotic lesions can eventually obliter-
vasodilation or increased blood pressure; the chronic
glomeruli, which occurs as a result of functional
The cause of this additional injury is not known, but
of these nephrons.
the remaining nephrons, particularly to the glomeruli
normal. Over a period of several years, however, the
nephrons. These adaptive changes permit a person to
increased urine output in the surviving nephrons. The
that lead to increased blood flow, increased GFR, and
end-stage renal disease.
with a functional kidney to survive. This condition is
In many cases, an initial insult to the kidney leads to
Failure Leading to End-Stage
Vicious Circle of Chronic Renal
decrease in the number of functional nephrons.
failure, the end result is essentially the same—a
interstitium, and lower urinary tract. Despite the wide
disorders of the blood vessels, glomeruli, tubules, renal
failure, like acute renal failure, can occur because of
Chapter 31
Kidney Diseases and Diuretics
407
variety of diseases that can lead to chronic renal
Renal Disease
progressive deterioration of kidney function and
further loss of nephrons to the point where the person
must be placed on dialysis treatment or transplanted
referred to as
Studies in laboratory animals have shown that sur-
gical removal of large portions of the kidney initially
causes adaptive changes in the remaining nephrons
exact mechanisms responsible for these changes are
not well understood but involve hypertrophy (growth
of the various structures of the surviving nephrons) as
well as functional changes that decrease vascular
resistance and tubular reabsorption in the surviving
excrete normal amounts of water and solutes even
when kidney mass is reduced to 20 to 25 per cent of
renal functional changes may lead to further injury of
some investigators believe that it may be related in
part to increased pressure or stretch of the remaining
increase in pressure and stretch of the small arterioles
and glomeruli are believed to cause sclerosis of these
vessels (replacement of normal tissue with connective
circle that eventually terminates in end-stage renal
of slowing down this progressive loss of kidney func-
tion is to lower arterial pressure and glomerular
as angiotensin-converting enzyme inhibitors or
glomeru-
lonephritis in all its various forms was believed to be
the most common initiating cause of end-stage renal
diabetes mellitus and hyper-
tension have become recognized as the leading causes
Excessive weight gain (obesity) appears to be the
most important risk factor for the two main causes of
end-stage renal disease—diabetes and hypertension.
Table 31–4
Polycystic disease
Nephrotoxins (analgesics, heavy metals)
Tuberculosis
Polyarteritis nodosa
Renal vascular disorders
Metabolic disorders
Some Causes of Chronic Renal Failure
Diabetes mellitus
Obesity
Amyloidosis
Hypertension
Atherosclerosis
Nephrosclerosis-hypertension
Immunologic disorders
Glomerulonephritis
Lupus erythematosus
Infections
Pyelonephritis
Primary tubular disorders
Urinary tract obstruction
Renal calculi
Hypertrophy of prostate
Urethral constriction
Congenital disorders
Congenital absence of kidney tissue (renal hypoplasia)
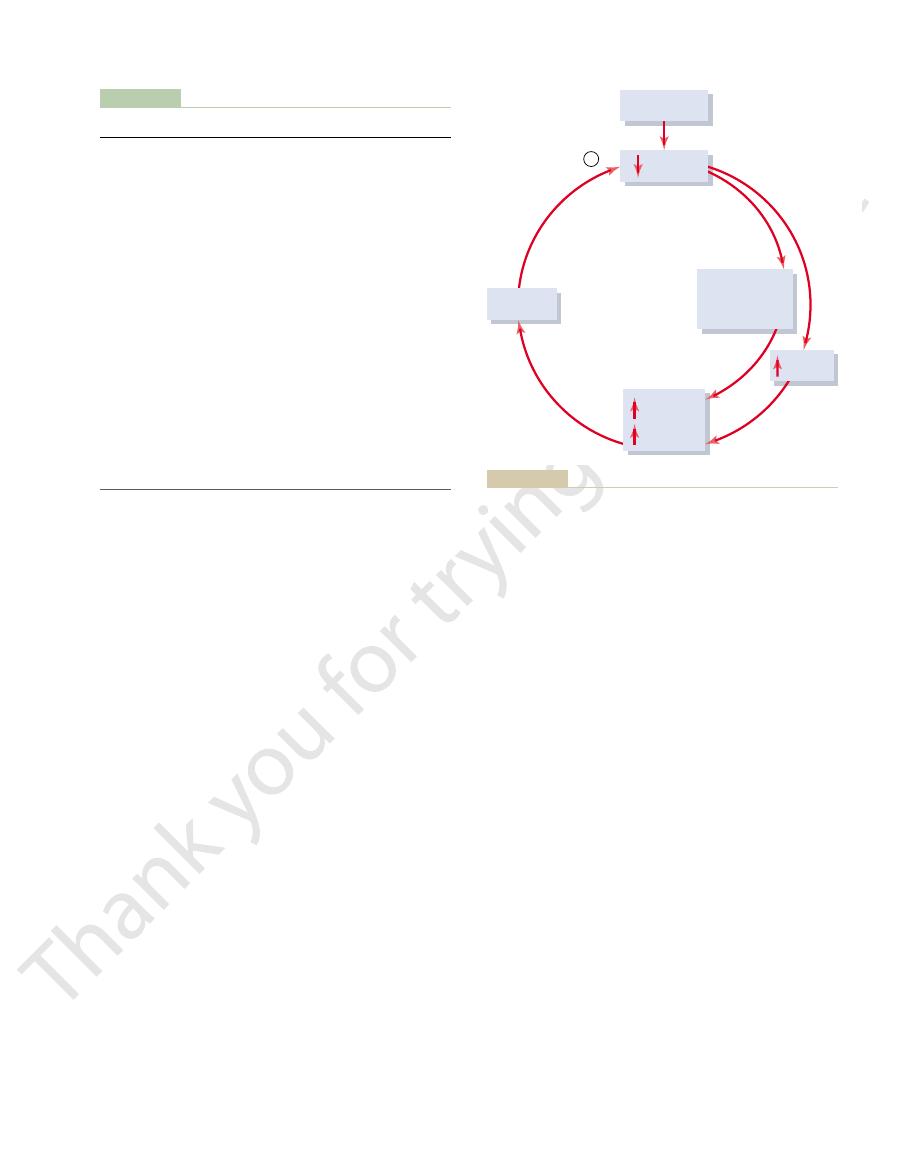
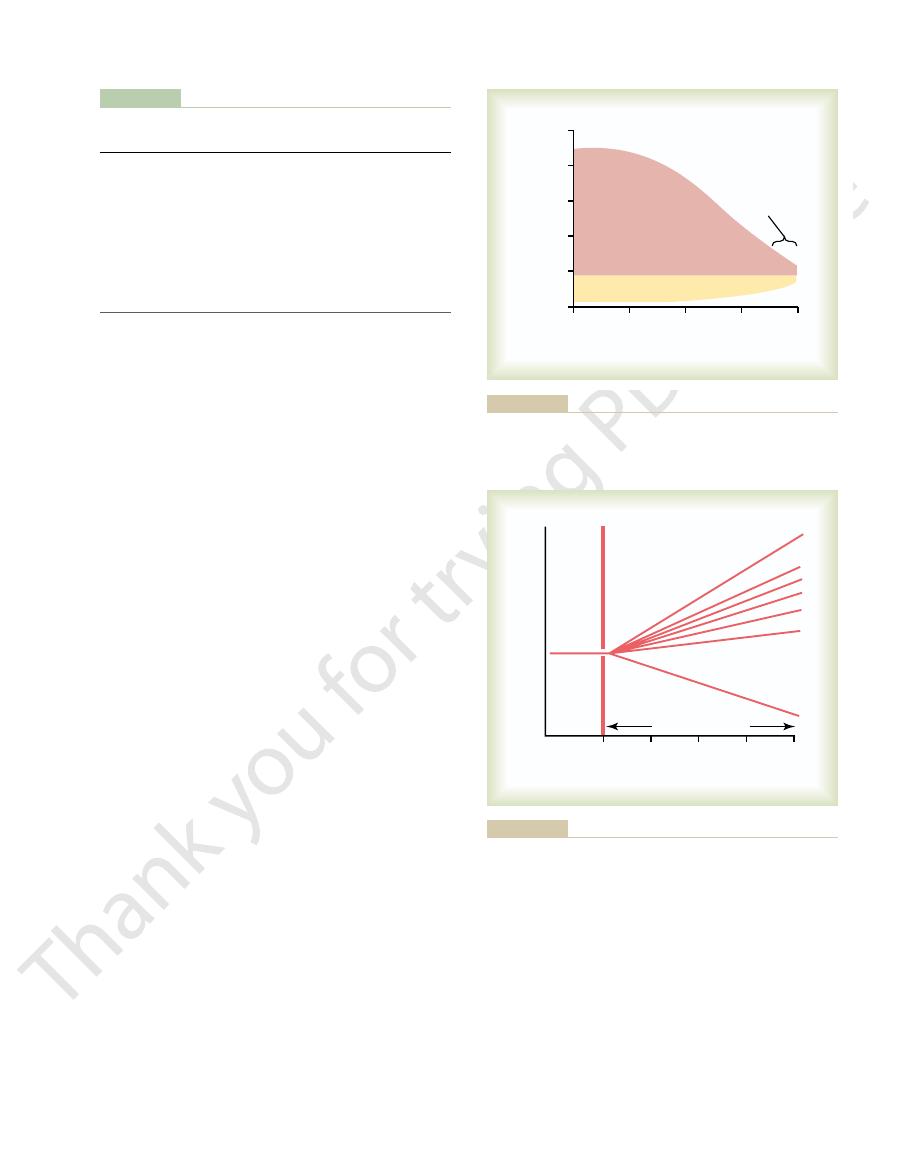
Glomerular
sclerosis
+
Glomerular
pressure
and/or
filtration
Arterial
pressure
Nephron
number
Primary
kidney disease
Hypertrophy
and vasodilation
of surviving
nephrons
sclerosis and eventual loss of these glomeruli.
injure these “normal” capillaries as well, thus causing progressive
the surviving glomerular capillaries, which in turn may eventually
nephrons because of disease may increase pressure and flow in
Vicious circle that can occur with primary kidney disease. Loss of
Figure 31–2
the membranes, and eventual invasion of the glomeruli
membranes are inflammation, progressive thickening of
form of glomerulonephritis. The results of the accumu-
glomerulonephritis, streptococcal infections account for
plexes in the glomerular membrane. In contrast to acute
In most cases, chronic glomerulonephritis begins with
erythematosus.
may be secondary to systemic diseases, such as
kidney disease, following acute glomerulonephritis, or it
leads to irreversible renal failure. It may be a primary
trast to the acute form of this disease, chronic glomeru-
capillary loops in the glomeruli of the kidneys. In con-
degrees of severity of hypertension or diabetes.
reasons, the incidence of malignant nephrosclerosis and
occurring in the affected nephrons. For unknown
gressive thickening of the vessels, with severe ischemia
The characteristic histologi-
malignant nephrosclerosis.
ously. Thus, benign nephrosclerosis in association with
causes of end-stage renal disease, as discussed previ-
In fact, diabetes mel-
diabetes mellitus.
The frequency and severity of nephrosclerosis and
people, kidney plasma flow and GFR decrease by 40 to
in both renal blood flow and GFR. Even in “normal”
(Figure 31–3). This loss of glomeruli and overall
life, causing about a 10 per cent decrease in the number
glomerulosclerosis.
tissue. When sclerosis occurs in the glomeruli, the injury
number of nephrons. Therefore, much of the kidney
tion among the smaller renal arteries, occlusion of one
them. Because there is essentially no collateral circula-
tually constricts the vessels and, in some cases, occludes
develop in the medial layers of these vessels, followed
of these vessels. This causes fibrinoid deposits to
afferent arterioles of the kidney. It is believed to begin
die after the age of 60. This type of vascular lesion
kidney disease, is seen to at least some extent in about
Benign nephrosclerosis,
still normal, a condition analogous to “two-kidney”
kidney function. As discussed in Chapter 19, hyperten-
other and, therefore, cause unilaterally diminished
the smaller arteries, arterioles, and glomeruli.
nephrosclerosis,
large arteries, which also causes occlusion of the vessels;
ies, with progressive sclerotic constriction of the vessels;
ischemia and death of kidney tissue. The most common
Injury to the Renal Vasculature as a
kidney disease.
sion, obesity may have additive or synergistic effects
for developing hypertension in adults. In addition to
90 per cent of all diabetes mellitus. Excess weight gain
closely linked to obesity, accounts for approximately
408
Unit V
The Body Fluids and Kidneys
is also a major cause of essential hypertension,
accounting for as much as 65 to 75 per cent of the risk
causing renal injury through diabetes and hyperten-
to worsen renal function in patients with pre-existing
Cause of Chronic Renal Failure
Many types of vascular lesions can lead to renal
of these are (1) atherosclerosis of the larger renal arter-
(2) fibromuscular hyperplasia of one or more of the
and (3)
caused by sclerotic lesions of
Atherosclerotic or hyperplastic lesions of the large
arteries frequently affect one kidney more than the
sion often occurs when the artery of one kidney is
constricted while the artery of the other kidney is
Goldblatt hypertension.
the most common form of
70 per cent of postmortem examinations in people who
occurs in the smaller interlobular arteries and in the
with leakage of plasma through the intimal membrane
by progressive thickening of the vessel wall that even-
or more of them causes destruction of a comparable
tissue becomes replaced by small amounts of fibrous
is referred to as
Nephrosclerosis and glomerulosclerosis occur to
some extent in most people after the fourth decade of
of functional nephrons each 10 years after age 40
nephron function is reflected by a progressive decrease
50 per cent by age 80.
glomerulosclerosis are greatly increased by concurrent
hypertension or
litus and hypertension are the two most important
severe hypertension can lead to a rapidly progressing
cal features of malignant nephrosclerosis include large
amounts of fibrinoid deposits in the arterioles and pro-
severe glomerulosclerosis is significantly higher in
blacks than in whites of similar ages who have similar
Injury to the Glomeruli as a Cause
of Chronic Renal Failure—
Glomerulonephritis
Chronic glomerulonephritis can be caused by several
diseases that cause inflammation and damage to the
lonephritis is a slowly progressive disease that often
lupus
accumulation of precipitated antigen-antibody com-
only a small percentage of patients with the chronic
lation of antigen-antibody complex in the glomerular
Table 31–5
Polycystic kidney disease
2
Glomerulonephritis
8
Hypertension
26
Diabetes mellitus
44
Cause
Percentage of Total ESRD Patients
Most Common Causes of End-Stage Renal Disease (ESRD)
Other/unknown
20
0
20
40
60
80
Glomeruli (x 10
6
)
0.5
0.0
1.0
2.0
2.5
1.5
Age (years)
Effect of aging on the number of functional glomeruli.
Figure 31–3
nephrons that have been destroyed.The reason for this
products of metabolism, such as urea and creatinine,
In contrast to the electrolytes, many of the waste
however, leads to electrolyte and fluid retention, and
Further reduction in the number of nephrons,
accumulation of any of these in the body fluids.
solutes. Yet patients who have lost as much as 75 per
nephrons, which reduces the GFR, would also cause
to Excrete More Water and Solutes.
Loss of Functional Nephrons Requires the Surviving Nephrons
Nephron Function in Chronic
edema, as discussed in Chapter 25.
all over the body into most of the tissues, causing severe
plasma, large amounts of fluid leak from the capillaries
a normal value of 28 to less than 10 mm Hg. As a con-
below 2 g/dl, and the colloid osmotic pressure falls from
fore, the child’s plasma protein concentration often falls
which is an extreme amount for a young child. There-
40 grams of plasma protein loss into the urine each day,
of 2 and 6 years. Increased permeability of the glomeru-
Minimal change nephropathy can occur in adults, but
plasma proteins.
albumin, to pass through the glomerular membrane
glomerular capillaries allows proteins,
especially
from antibody attack on the membrane. Loss of normal
abnormal immune reactions in some cases, suggesting
membrane. Immunologic studies have also shown
26, minimal change nephropathy has been found to
detected with light microscopy. As discussed in Chapter
drome,
minimal change nephrotic syn-
of the glomeruli; and (3)
amyloidosis,
chronic glomerulonephritis,
brane can cause the nephrotic syndrome. Such diseases
permeability of the glomerular membrane. Therefore,
The cause of the protein loss in the urine is increased
it is associated with some degree of renal failure.
major abnormalities of kidney function, but more often
some instances, this occurs without evidence of other
large quantities of plasma proteins into the urine. In
, which is characterized by loss of
of Protein in the Urine Because of
can develop.
functional renal tissue are lost, and chronic renal failure
throughout the kidney. Consequently, large parts of
damage of renal tubules, glomeruli, and other structures
With long-standing pyelonephritis, invasion of the
have markedly impaired ability to concentrate the urine.
trating urine, patients with pyelonephritis frequently
than it affects the cortex, at least in the initial stages.
inflammation associated with pyelonephritis.
medulla, where they can initiate the infection and
is propelled upward toward the kidney, carrying with it
ureter during micturition; as a result, some of the urine
tion. This condition is called
or in some people, bacteria may reach the renal pelvis
may remain localized without ascending to the kidney,
Once cystitis has occurred, it
cystitis.
bacteria multiply and the bladder becomes inflamed, a
impaired ability to flush bacteria from the bladder, the
(2) the existence of obstruction of urine outflow. With
completely, leaving residual urine in the bladder, and
the bladder: (1) the inability of the bladder to empty
readily, there are two general clinical conditions that
ureters to the kidneys.
either by way of the blood stream or, more commonly,
of the urinary tract. These bacteria reach the kidneys
Escherichia coli
The infection can result
pyelonephritis.
bacterial infections.
damage to the renal interstitium by poisons, drugs, and
destroys individual nephrons, or it can involve primary
result from vascular, glomerular, or tubular damage that
In general, this can
interstitial nephritis.
Injury to the Renal Interstitium as a
tissue and are, therefore, unable to filter fluid.
the disease, many glomeruli are replaced by fibrous
thickened glomerular membranes. In the final stages of
by fibrous tissue. In the later stages of the disease, the
Chapter 31
Kidney Diseases and Diuretics
409
glomerular capillary filtration coefficient becomes
greatly reduced because of decreased numbers of filter-
ing capillaries in the glomerular tufts and because of
Cause of Chronic Renal Failure—
Pyelonephritis
Primary or secondary disease of the renal interstitium
is referred to as
Renal interstitial injury caused by bacterial infec-
tion is called
from different types of bacteria but especially from
that originate from fecal contamination
by ascension from the lower urinary tract by way of the
Although the normal bladder is able to clear bacteria
may interfere with the normal flushing of bacteria from
condition termed
because of a pathological condition in which urine is
propelled up one or both of the ureters during micturi-
vesicoureteral reflux and is
due to the failure of the bladder wall to occlude the
bacteria that can reach the renal pelvis and renal
Pyelonephritis begins in the renal medulla and there-
fore usually affects the function of the medulla more
Because one of the primary functions of the medulla is
to provide the countercurrent mechanism for concen-
kidneys by bacteria not only causes damage to the renal
medulla interstitium but also results in progressive
Nephrotic Syndrome—Excretion
Increased Glomerular Permeability
Many patients with kidney disease develop the
nephrotic syndrome
any disease that increases the permeability of this mem-
include (1)
which affects
primarily the glomeruli and often causes greatly
increased permeability of the glomerular membrane;
(2)
which results from deposition of an
abnormal proteinoid substance in the walls of the blood
vessels and seriously damages the basement membrane
which is associated with no major abnormality
in the glomerular capillary membrane that can be
be associated with loss of the negative charges that are
normally present in the glomerular capillary basement
that the loss of the negative charges may have resulted
negative charges in the basement membrane of the
with ease because the negative charges in the basement
membrane normally repel the negatively charged
more frequently it occurs in children between the ages
lar capillary membrane occasionally allows as much as
sequence of this low colloid osmotic pressure in the
Renal Failure
It would be reasonable
to suspect that decreasing the number of functional
major decreases in renal excretion of water and
cent of their nephrons are able to excrete normal
amounts of water and electrolytes without serious
death usually ensues when the number of nephrons
falls below 5 to 10 per cent of normal.
accumulate almost in proportion to the number of
large decreases in the total GFR, normal rates of renal
that cause the blood vessels to vasodilate. Even with
vessels and glomeruli, as well as functional changes
ing nephrons, owing to hypertrophy of the blood
as under normal conditions (Table 31–6).
nephrons, each surviving nephron must excrete four
For example, with a 75 per cent loss of functional
creasing tubular reabsorption of these electrolytes.
Figure 31–5). This is accomplished by greatly de-
In the case of sodium and chloride ions, their plasma
secretion rates.
sorption or, in some instances, by increasing tubular
as shown in curve B of Figure 31–5. Maintenance of
stances rise, but not in proportion to the fall in GFR,
Thereafter, the plasma concentrations of these sub-
gen ions, are often maintained near the normal range
Some solutes, such as phosphate, urate, and hydro-
Figure 31–5.
creatinine concentration, as shown in curve A of
tions in GFR; however, this normal rate of creatinine
equals the rate of creatinine production, despite reduc-
steady-state conditions, the creatinine excretion rate
is produced in the body (Figure 31–4). Thus, under
tion rate also transiently decreases, causing accumula-
Therefore, if GFR decreases, the creatinine excre-
Creatinine, for example, is not reabsorbed at all, and
they are not reabsorbed as avidly as the electrolytes.
largely on glomerular filtration for their excretion, and
410
Unit V
The Body Fluids and Kidneys
is that substances such as creatinine and urea depend
the excretion rate is equal to the rate at which it is
filtered.
Creatinine filtration rate
= GFR ¥ Plasma creatinine concentration
= Creatinine excretion rate
tion of creatinine in the body fluids and raising plasma
concentration until the excretion rate of creatinine
returns to normal—the same rate at which creatinine
excretion occurs at the expense of elevated plasma
until GFR falls below 20 to 30 per cent of normal.
relatively constant plasma concentrations of these
solutes as GFR declines is accomplished by excreting
progressively larger fractions of the amounts of these
solutes that are filtered at the glomerular capillaries;
this occurs by decreasing the rate of tubular reab-
concentrations are maintained virtually constant
even with severe decreases in GFR (see curve C of
times as much sodium and four times as much volume
Part of this adaptation occurs because of increased
blood flow and increased GFR in each of the surviv-
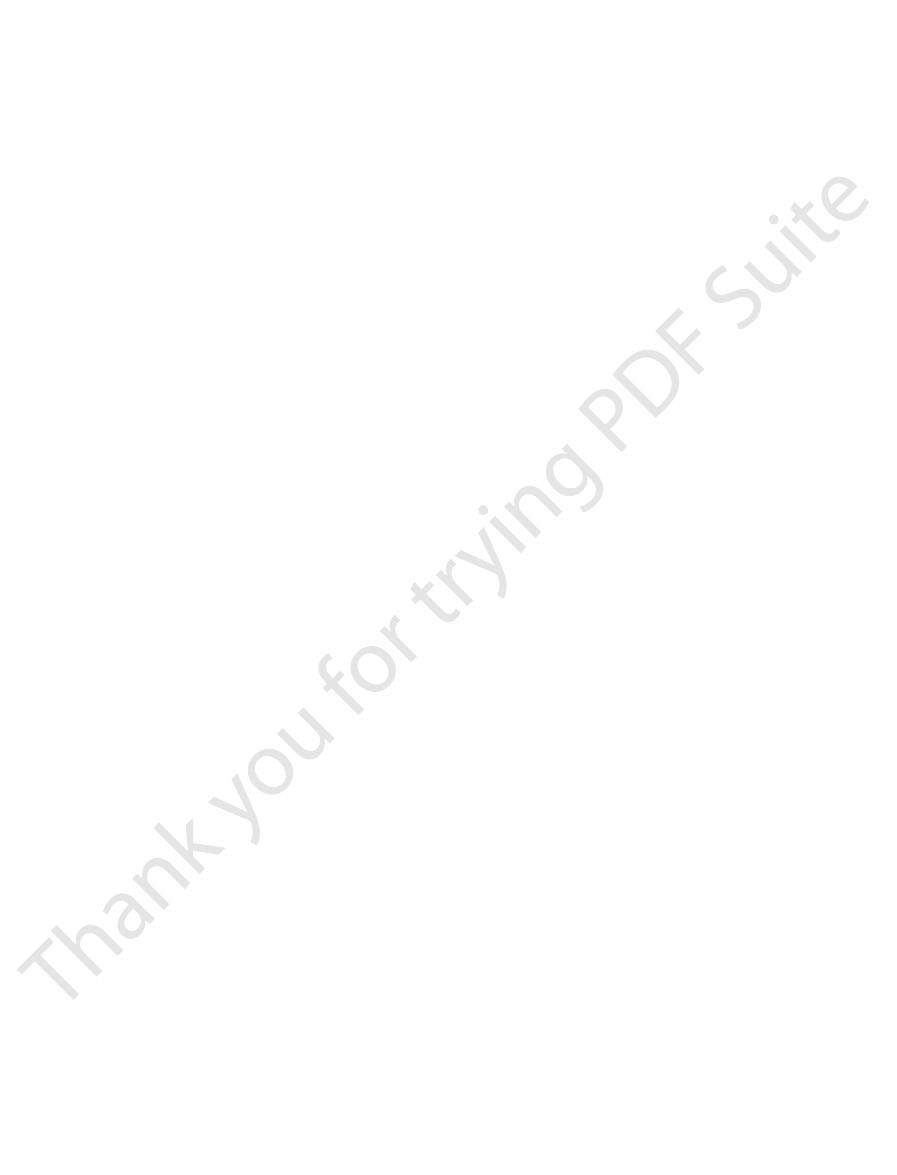
Positive balance
Production
0
1
2
3
4
Creatinine production and
renal excretion (g/day)
Days
2
1
0
Excretion GFR x P
Creatinine
Serum creatinine
concentration (mg/dl)
2
1
0
GFR (ml/min)
100
50
0
when the production rate of creatinine remains constant.
on serum creatinine concentration and on creatinine excretion rate
Effect of reducing glomerular filtration rate (GFR) by 50 per cent
Figure 31–4
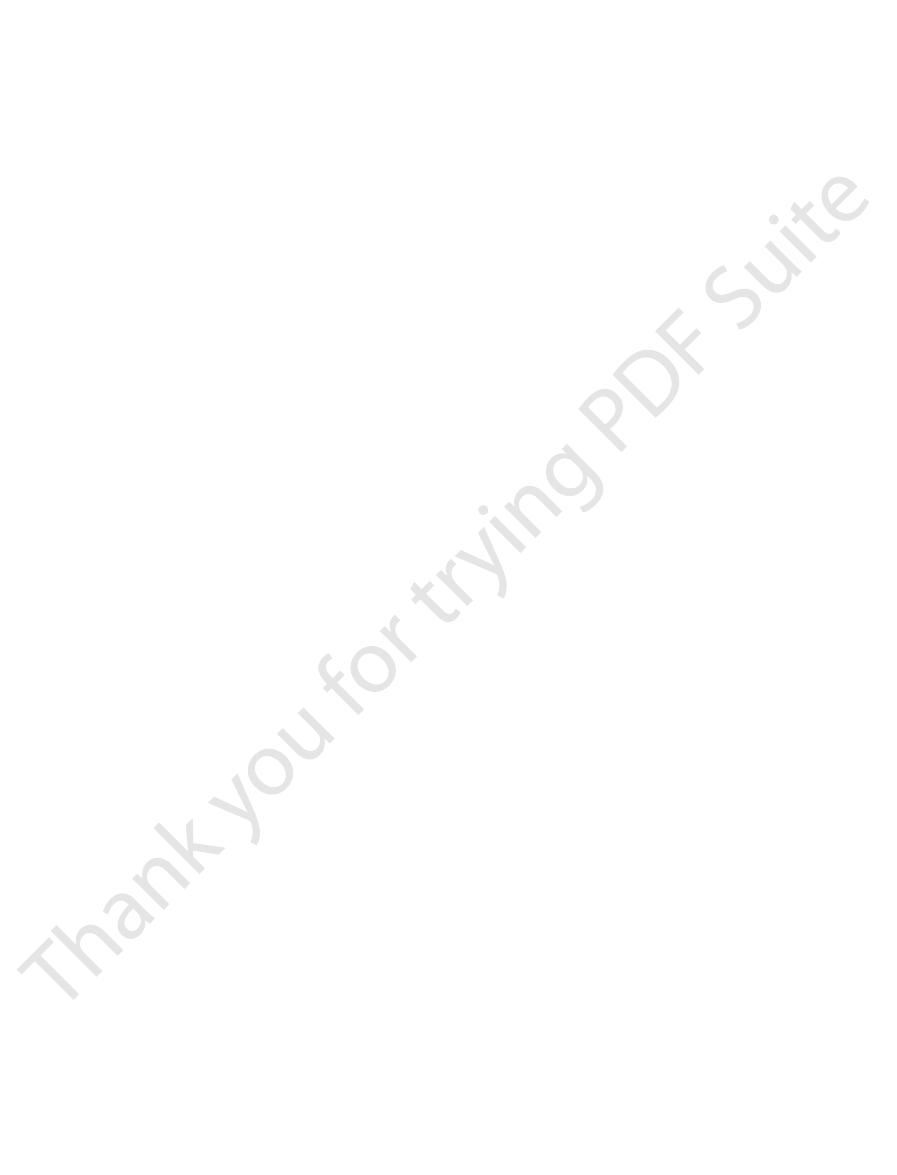
0
25
50
75
100
Plasma concentration
Glomerular filtration rate
(percentage of normal)
A
B
C
urate. Curve C shows the approximate concentrations for solutes
approximate concentrations for solutes such as phosphate and
urea that are filtered and poorly reabsorbed. Curve B shows the
in the plasma concentrations of solutes such as creatinine and
in chronic renal failure. Curve A shows the approximate changes
Representative patterns of adaptation for different types of solutes
Figure 31–5
such as sodium and chloride.
the high concentration of urea in the body fluids.
This total condition is called
bases.
phenols, sulfates, phosphates, potassium,
excreted by the kidney, including
end products of proteins, and (4)
—especially urea, creatinine, and uric acid—result-
products, (3)
water and salt retention, (2)
generalized edema
approximately those shown in Figure 31–7. Important
the same amounts of water and food, the concentrations
degree of impairment of renal function. Assuming that
The effect of complete renal failure on the body fluids
Effects of Renal Failure on the Body
restricted for 12 or more hours.
concentrate urine when a person’s water intake is
chronic renal failure, an important clinical test of renal
approach those of the glomerular filtrate. Because the
quence, the diluting capacity of the kidney is impaired,
tubular fluid of this part of the nephron. As a conse-
The diluting mechanism in the kidney is also
Figure 31–6.
specific gravity of the glomerular filtrate, as shown in
concentrating ability of the kidney declines, and urine
gressively more nephrons are destroyed, the maximum
medullary interstitial fluid solutes. Therefore, as pro-
ing ducts prevents adequate water reabsorption, and
ability to concentrate or dilute the urine. The concen-
rate at which the tubules reabsorb water and solutes.
Chapter 31
Kidney Diseases and Diuretics
411
excretion can still be maintained by decreasing the
Isosthenuria—Inability of the Kidney to Concentrate or Dilute
the Urine.
One important effect of the rapid rate of
tubular flow that occurs in the remaining nephrons of
diseased kidneys is that the renal tubules lose their
trating ability of the kidney is impaired mainly because
(1) the rapid flow of tubular fluid through the collect-
(2) the rapid flow through both the loop of Henle and
the collecting ducts prevents the countercurrent mech-
anism from operating effectively to concentrate the
osmolarity and specific gravity (a measure of the total
solute concentration) approach the osmolarity and
impaired when the number of nephrons decreases
because the rapid flushing of fluid through the loops
of Henle and the high load of solutes such as urea
cause a relatively high solute concentration in the
and the minimal urine osmolality and specific gravity
concentrating mechanism becomes impaired to a
greater extent than does the diluting mechanism in
function is to determine how well the kidneys can
Fluids—Uremia
depends on (1) water and food intake and (2) the
a person with complete renal failure continues to ingest
of different substances in the extracellular fluid are
effects include (1)
resulting from
acidosis resulting from
failure of the kidneys to rid the body of normal acidic
high concentration of the nonprotein nitro-
gens
ing from failure of the body to excrete the metabolic
high concentrations of
other substances
and guanidine
uremia because of
Total Kidney Excretion and Excretion per Nephron in
Table 31–6
Volume excreted per nephron
0.75
3.0
Volume excreted for all
1.5
1.5
Single nephron GFR (nl/min)
62.5
80
Total GFR (ml/min)
125
40
Number of nephrons
2,000,000
500,000
Normal
Nephrons
Renal Failure
75% Loss of
nephrons (ml/min)
(nl/min)
GFR, glomerular filtration rate.
500,000
0
2,000,000 1,500,000 1,000,000
Specific gravity of urine
Isosthenuria
Glomerular filtrate specific gravity
1.000
1.010
1.020
1.030
1.040
1.050
Number of nephrons in both kidneys
of functional nephrons.
Development of isosthenuria in a patient with decreased numbers
Figure 31–6
9
12
Water
Decrease
Increase
3
0
6
Kidney shutdown
Normal
NPN
Phenols
HPO
4
=
HCO
3
-
SO
4
=
K
+
H
+
Na
+
Days
nonprotein nitrogens.
Effect of kidney failure on extracellular fluid constituents. NPN,
Figure 31–7
mainly in the cortical collecting tubules.
secretion, which increases sodium reabsorption
thickening of the glomerular capillary membranes,
glomerulonephritis, which causes inflammation and
which reduces GFR. An example of this is chronic
hypertension caused by renal artery stenosis.
renal blood flow and GFR. An example is
Increased renal vascular resistance,
varying degrees. Some specific types of renal abnormal-
fore, lesions that either
and water almost invariably cause hypertension. There-
Sodium and Water Promote Hypertension.
following.
tension. A classification of kidney disease relative
uremia without hypertension. Nevertheless, some types
forth, until end-stage renal disease develops.
kidneys, further increases in blood pressure, and so
pressure, which in turn causes further damage to the
circle: primary kidney damage leads to increased blood
disease can, in some instances, propagate a vicious
19. Thus, the relation between hypertension and kidney
can cause hypertension, as discussed in detail in Chapter
disease. Conversely, abnormalities of kidney function
As discussed earlier in this chapter, hypertension can
bones, causing further demineralization of the bones.
secretion. This secondary hyperparathy-
calcium concentration, which in turn stimulates
ionized
plasma, thus decreasing the plasma serum
decreased GFR. This rise in serum phosphate causes
ability of calcium to the bones.
vitamin D, which in turn
calcium absorption from the intestine. Therefore,
first in the liver and then in the kidneys, into 1,25–
Vitamin D must be converted by a two-stage process,
absorbed and, therefore, become greatly weakened. An
Osteomalacia in Chronic Renal Failure Caused by Decreased
of erythropoietin, which leads to diminished red blood
damaged, they are unable to form adequate quantities
produce red blood cells. If the kidneys are seriously
The most im-
Anemia in Chronic Renal Failure Caused by Decreased Erythro-
drastically, and the patient will become comatose and
when this buffering power is used up, the blood pH falls
few thousand millimoles of hydrogen ion. However,
cellular fluid hydrogen ion concentration, and the phos-
to function, acid accumulates in the body fluids. The
than metabolic alkali. Therefore, when the kidneys fail
failure.
stances, especially of urea and creatinine, provides an
reason, measuring the concentrations of these sub-
the degree of reduction in functional nephrons. For this
weeks of total renal failure. With chronic renal failure,
cells. The concentrations of these, particularly of urea,
These, in general, are the end products of protein
acid, creatinine, and a few less important compounds.
The nonprotein nitrogens include urea, uric
Uremia—Increase in Urea and Other Nonprotein Nitrogens
group, removal of the ischemic kidneys usually corrects
excess sodium has been removed by dialysis. In this
by dialysis can control the hypertension. The remaining
develop hypertension. In most of these patients, severe
chronic renal failure. Almost all patients with kidney
kidney disease, often causes severe hypertension in
tion that does occur, along with increased secretion of
amounts of salt and water. Even the small fluid reten-
previously, is that the surviving nephrons excrete larger
cent of normal or lower. The reason for this, as discussed
are not excessive, until kidney function falls to 25 per
fluid may not be severe, as long as salt and fluid intake
With chronic partial kidney failure, accumulation of
and rapidly.
anisms, the body fluids begin to increase immediately
only slightly increased. If fluid intake is not limited and
failure begins, the total body fluid content may become
Water Retention and Development of Edema in Renal Failure.
412
Unit V
The Body Fluids and Kidneys
If
water intake is restricted immediately after acute renal
the patient drinks in response to the normal thirst mech-
renin and angiotensin II that usually occurs in ischemic
function so reduced as to require dialysis to preserve life
reduction of salt intake or removal of extracellular fluid
patients continue to have hypertension even after
the hypertension (as long as fluid retention is prevented
by dialysis) because it removes the source of excessive
renin secretion and subsequent increased angiotensin II
formation.
(Azotemia).
metabolism and must be removed from the body to
ensure continued normal protein metabolism in the
can rise to as high as 10 times normal during 1 to 2
the concentrations rise approximately in proportion to
important means for assessing the degree of renal
Acidosis in Renal Failure.
Each day the body normally pro-
duces about 50 to 80 millimoles more metabolic acid
buffers of the body fluids normally can buffer 500 to
1000 millimoles of acid without lethal increases in extra-
phate compounds in the bones can buffer an additional
die if the pH falls below about 6.8.
poietin Secretion.
Patients with severe chronic renal
failure almost always develop anemia.
portant cause of this is decreased renal secretion of
erythropoietin, which stimulates the bone marrow to
cell production and consequent anemia.
Production of Active Vitamin D and by Phosphate Retention by
the Kidneys.
Prolonged renal failure also causes osteo-
malacia, a condition in which the bones are partially
important cause of this condition is the following:
dihydroxycholecalciferol before it is able to promote
serious damage to the kidney greatly reduces the blood
concentration of active
decreases intestinal absorption of calcium and the avail-
Another important cause of demineralization of the
skeleton in chronic renal failure is the rise in serum
phosphate concentration that occurs as a result of
increased binding of phosphate with calcium in the
parathy-
roid hormone
roidism then stimulates the release of calcium from
Hypertension and Kidney Disease
exacerbate injury to the glomeruli and blood vessels of
the kidneys and is a major cause of end-stage renal
Not all types of kidney disease cause hypertension,
because damage to certain portions of the kidney cause
of renal damage are particularly prone to cause hyper-
to hypertensive or nonhypertensive effects is the
Renal Lesions That Reduce the Ability of the Kidneys to Excrete
Renal lesions that
decrease the ability of the kidneys to excrete sodium
decrease GFR or increase
tubular reabsorption usually lead to hypertension of
ities that can cause hypertension are as follows:
1.
which reduces
2. Decreased glomerular capillary filtration coefficient,
thereby reducing the glomerular capillary filtration
coefficient.
3. Excessive tubular sodium reabsorption. An example
is hypertension caused by excessive aldosterone
to the renal tubules.
orders, or it can occur as a result of widespread injury
metabolic acidosis, as discussed in Chapter 30. This type
ually lost in the urine. This causes a continued state of
result, large amounts of sodium bicarbonate are contin-
to secrete adequate amounts of hydrogen ions. As a
In this condition, the renal tubules are unable
Renal Tubular Acidosis—Failure of the Tubules to Secrete Hydro-
Chapter 79.
response of the usual type of rickets, as discussed in
tory to vitamin D therapy, in contrast to the rapid
person to develop rickets. This type of rickets is refrac-
causes diminished calcification of the bones, causing the
function. Over a long period, a low phosphate level
not cause serious immediate abnormalities, because
body fluids falls very low. This condition usually does
In renal hypophosphatemia,
the renal
ently has no major clinical significance.
to be reabsorbed; or (3)
renal stones; (2)
in which large amounts of cystine fail to be
sorption of all amino acids; more frequently, deficiencies
generalized aminoaciduria
distinct transport systems. Rarely, a condition called
reabsorption, whereas other amino acids have their own
making a diagnosis of diabetes mellitus.
is a relatively benign condition, must be ruled out before
presence of glucose in the urine, renal glycosuria, which
large amounts of glucose pass into the urine each day.
Consequently, despite a normal blood glucose level,
be normal, but the transport mechanism for tubular
In this condition, the blood glucose concentration may
can cause important renal tubular disorders.
through the tubular membrane. In addition, damage to
renal tubular epithelial cells. For this reason, many
happens to be absent or abnormal, the tubules may be
respective gene in the nucleus. If any required gene
Chapter 3, we also point out that each cellular enzyme
stances across the tubular epithelial membranes. In
In Chapter 27, we point out that several mechanisms are
Specific Tubular Disorders
case, the kidneys simply cannot clear adequate quanti-
imposed, such as eating a large amount of salt. In this
However, a patient with this type of abnormality may
to promote enough water and salt excretion in the urine,
not cause clinically significant hypertension, because
and the salt intake is not excessive, this condition might
is great enough. If the remaining nephrons are normal
of one kidney and part of another kidney, almost always
numbers of whole nephrons, such as occurs with the loss
Kidney Diseases That Cause Loss of Entire Nephrons Lead to Renal
pressure.
is maintained, but at the expense of high blood
excretion of sodium and water by the kidney, so that
hypertension develops, which restores the overall
nephrons to excrete sodium and water. As a result,
II formation. The high levels of angiotensin II then
amounts of renin, which causes increased angiotensin
portions of the kidneys. When this occurs, the ischemic
tension in the usual manner.
and water; and (3) excess salt and water cause hyper-
nonischemic kidney tissue, causing it also to retain salt
quent increased angiotensin II formation, affects the
the renin secreted by the ischemic kidney, and subse-
excretes less than normal amounts of water and salt; (2)
Chapter 19, is (1) the ischemic kidney tissue itself
of events in causing this hypertension, as discussed in
which can cause hypertension. The most likely sequence
This secretion leads to the formation of angiotensin II,
occurs when one renal artery is severely constricted, the
ischemic and the remainder is not ischemic, such as
Hypertension Caused by Patchy Renal Damage and Increased
arterial pressure.
Chapter 19, normal excretion of sodium and water at an
water other than the hypertension. As explained in
pressure rises. Thus, after hypertension develops, there
aldosterone secretion, the urinary excretion rate is ini-
reabsorption is increased, as occurs with excessive
arterial blood pressure rises. Likewise, when tubular
decreases in the glomerular capillary coefficient, the
and water become balanced once again. Even when
sure diuresis, so that intake and output of sodium
Once hypertension has developed, renal excretion of
Chapter 31
Kidney Diseases and Diuretics
413
sodium and water returns to normal because the high
arterial pressure causes pressure natriuresis and pres-
there are large increases in renal vascular resistance or
GFR may still return to nearly normal levels after the
tially reduced but then returns to normal as arterial
may be no sign of impaired excretion of sodium and
elevated arterial pressure means that pressure natriure-
sis and pressure diuresis have been reset to a higher
Renal Secretion of Renin.
If one part of the kidney is
ischemic renal tissue secretes large quantities of renin.
A similar type of hypertension can result when patchy
areas of one or both kidneys become ischemic as a
result of arteriosclerosis or vascular injury in specific
nephrons excrete less salt and water but secrete greater
impair the ability of the surrounding otherwise normal
balance between intake and output of salt and water
Failure But May Not Cause Hypertension.
Loss of large
leads to renal failure if the amount of kidney tissue lost
even a slight rise in blood pressure will raise the GFR
and decrease tubular sodium reabsorption sufficiently
even with the few nephrons that remain intact.
become severely hypertensive if additional stresses are
ties of salt with the small number of functioning
nephrons that remain.
responsible for transporting different individual sub-
and each carrier protein is formed in response to a
deficient in one of the appropriate carrier proteins or
one of the enzymes needed for solute transport by the
hereditary tubular disorders occur because of the trans-
port of individual substances or groups of substances
the tubular epithelial membrane by toxins or ischemia
Renal Glycosuria—Failure of the Kidneys to Reabsorb Glucose.
reabsorption of glucose is greatly limited or absent.
Because diabetes mellitus is also associated with the
Aminoaciduria—Failure of the Kidneys to Reabsorb Amino Acids.
Some amino acids share mutual transport systems for
results from deficient reab-
of specific carrier systems may result in (1) essential
cystinuria,
reabsorbed and often crystallize in the urine to form
simple glycinuria, in which glycine fails
beta-aminoisobutyricaciduria,
which occurs in about 5 per cent of all people but appar-
Renal Hypophosphatemia—Failure of the Kidneys to Reabsorb
Phosphate.
tubules fail to reabsorb large enough quantities of phos-
phate ions when the phosphate concentration of the
the phosphate concentration of the extracellular fluid
can vary widely without causing major cellular dys-
gen Ions.
of renal abnormality can be caused by hereditary dis-
flow may be several hundred milliliters per minute, and
one time is usually less than 500 milliliters, the rate of
The total amount of blood in the artificial kidney at any
In normal operation of the artificial kidney, blood
increasing the flow rate of the blood, the dialyzing fluid,
flow through the artificial kidney, the dissipation of the
with “hemodialysis,” in which blood and dialysate fluid
gradient is dissipated. In a flowing system, as is the case
Thus, the maximum rate of solute transfer occurs ini-
membrane.
area of the membrane, and (4) the length of time
meability of the membrane to the solute, (3) the surface
of the solute between the two solutions, (2) the per-
The rate of movement of solute across the dialyzing
fluid, there will be a
fluid back into the plasma. If the concentration of a sub-
the plasma proteins, to diffuse in both directions—from
enough to allow the constituents of the plasma, except
brane is a dialyzing fluid. The cellophane is porous
two thin membranes of cellophane; outside the mem-
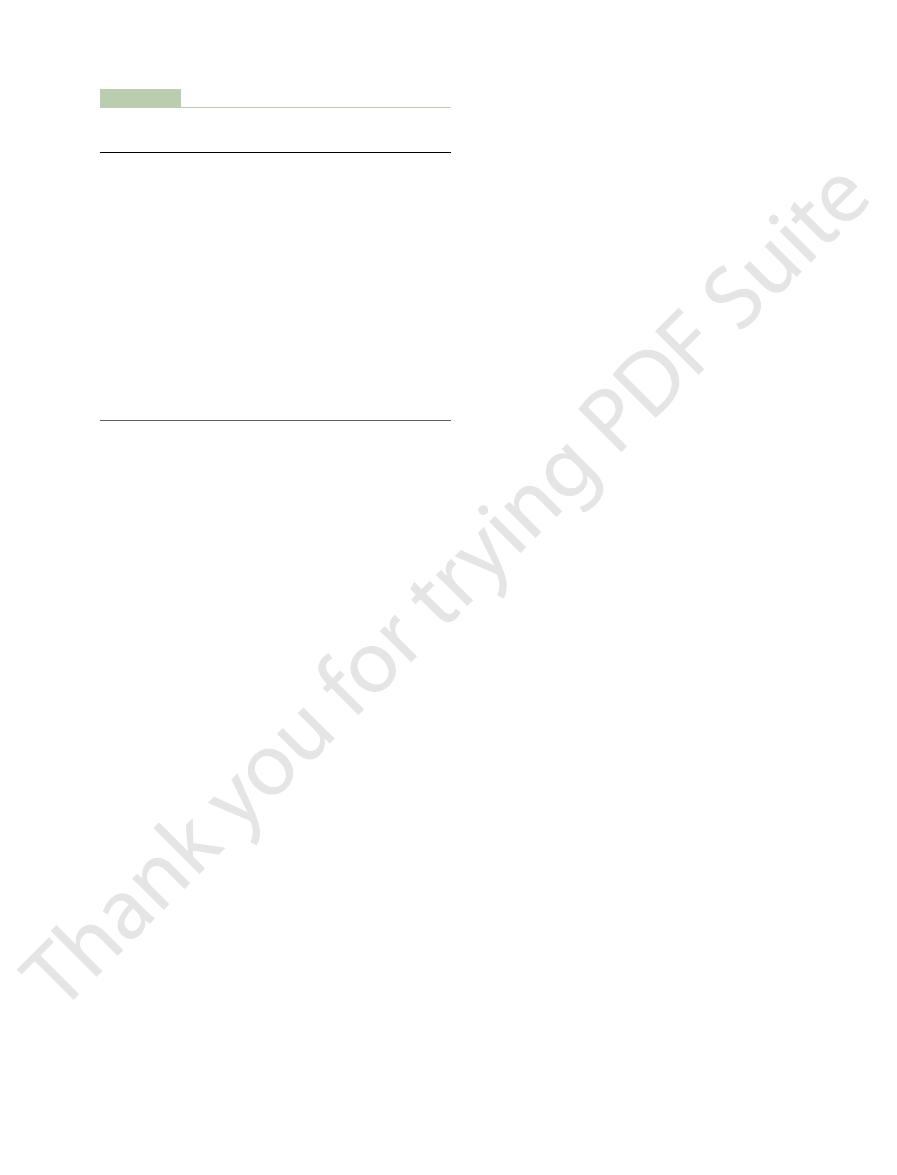
Figure 31–8 shows the components of one type of arti-
channels bounded by a thin membrane. On the other
The basic principle of the arti-
kidneys usually remains significantly impaired. A better
kidneys, the health of patients maintained on artificial
with artificial kidneys. Because dialysis cannot maintain
to maintain life. In the United States alone, nearly
versible, it is necessary to perform dialysis chronically
their function. If the loss of kidney function is irre-
types of acute renal failure, an artificial kidney may be
plished by dialysis with an artificial kidney. In certain
and composition toward normal. This can be accom-
ically, is a threat to life and requires removal of toxic
Severe loss of kidney function, either acutely or chron-
Artificial Kidney
Treatment of Renal Failure
can cause damage.
drome caused by tubular injury, because these cells
tubular cells are especially affected in Fanconi’s syn-
tubular cells as a result of ischemia. The proximal
renal tubular epithelial cells, and (3) injury to the renal
port mechanisms, (2) toxins or drugs that injure the
tubular cells to transport various substances. Some of
There are multiple causes of Fanconi’s syndrome,
insipidus.
and sometimes calcium; and (3) nephrogenic diabetes
metabolic acidosis; (2) increased excretion of potassium
to reabsorb sodium bicarbonate, which results in
manifestations are also observed, such as (1) failure
acids, glucose, and phosphate. In severe cases, other
Fanconi’s syndrome is usually associated
Renal Tubules.
Fanconi’s Syndrome—A Generalized Reabsorptive Defect of the
adequate quantities of water are not available, the
dition seldom causes severe difficulty. However, when
as the person is supplied with plenty of water, this con-
large quantities of dilute urine to be excreted. As long
tubules do not respond to antidiuretic hormone, causing
Occasionally, the renal
414
Unit V
The Body Fluids and Kidneys
Nephrogenic Diabetes Insipidus—Failure of the Kidneys to
Respond to Antidiuretic Hormone.
person rapidly becomes dehydrated.
with increased urinary excretion of virtually all amino
which results from a generalized inability of the renal
these causes include (1) hereditary defects in cell trans-
reabsorb and secrete many of the drugs and toxins that
by Dialysis with an
waste products and restoration of body fluid volume
used to tide the patient over until the kidneys resume
300,000 people with irreversible renal failure or even
total kidney removal are being maintained by dialysis
completely normal body fluid composition and cannot
replace all the multiple functions performed by the
treatment for permanent loss of kidney function is to
restore functional kidney tissue by means of a kidney
transplant.
Basic Principles of Dialysis.
ficial kidney is to pass blood through minute blood
side of the membrane is a dialyzing fluid into which
unwanted substances in the blood pass by diffusion.
ficial kidney in which blood flows continually between
plasma into the dialyzing fluid or from the dialyzing
stance is greater in the plasma than in the dialyzing
net transfer of the substance from
the plasma into the dialyzing fluid.
membrane depends on (1) the concentration gradient
that the blood and fluid remain in contact with the
tially when the concentration gradient is greatest (when
dialysis is begun) and slows down as the concentration
concentration gradient can be reduced and diffusion of
solute across the membrane can be optimized by
or both.
flows continually or intermittently back into the vein.
Bubble
trap
Fresh dialyzing
solution
Used dialyzing
solution
Constant
temperature
bath
Semipermeable
membrane
Flowing
dialysate
Flowing
blood
Dialyzer
Blood in
Blood out
Dialysate
in
Dialysate
out
Waste
products
Water
Principles of dialysis with an artificial kidney.
Figure 31–8
chronic renal disease. J Am Soc Nephrol 13:798, 2002.
Wilcox CS: New insights into diuretic use in patients with
United States Renal Data System. http://www.usrds.org/.
289:747, 2003.
Singri N, Ahya SN, Levin ML: Acute renal failure. JAMA
284:F11, 2003.
transporter to clinical use. Am J Physiol Renal Physiol
Shankar SS, Brater DC: Loop diuretics: from the Na-K-2Cl
www.kidneyatlas.org/.
Schrier RW: Atlas of Diseases of the Kidney. http://
Hypertension 42:1050, 2003.
as a risk factor for development of cardiovascular disease.
Sarnak MJ, Levey AS, Schoolwerth AC, et al: Kidney disease
renal failure. J Am Soc Nephrol 14:265, 2003.
Molitoris BA: Transitioning to therapy in ischemic acute
WB Saunders, 2000, pp 567-570.
(eds): Cecil Textbook of Medicine, 21st ed. Philadelphia:
Mitch WE: Acute renal failure. In: Goldman F, Bennett JC
WB Saunders, 2000, pp 571-578.
(eds): Cecil Textbook of Medicine, 21st ed. Philadelphia:
Luke RG: Chronic renal failure. In: Goldman F, Bennett JC
on Cardiovascular Disease. Am J Kidney Dis 32:853, 1998.
we go from here? National Kidney Foundation Task Force
What do we know? What do we need to learn? Where do
demic of cardiovascular disease in chronic renal disease.
Levey AS, Beto JA, Coronado BE, et al: Controlling the epi-
sion of renal disease. J Am Soc Nephrol 14(Suppl 2):S144,
Hostetter TH: Prevention of the development and progres-
11:41, 2004.
cause of chronic renal disease? Adv Ren Replace Ther
Hall JE, Henegar JR, Dwyer TM, et al: Is obesity a major
41:625, 2003.
Hall JE: The kidney, hypertension, and obesity. Hypertension
sis patients. Semin Dial 15:144, 2002.
Fishbane SA, Scribner BH: Blood pressure control in dialy-
Philadelphia: WB Saunders, 2004.
Andreoli TE (ed): Cecil’s Essentials of Medicine, 6th ed.
secretion of erythropoietin, which is necessary for red
some of the other functions of the kidneys, such as
kidney replaces the normal kidneys. Also, it is important
three times a week. Therefore, the overall plasma clear-
the artificial kidney is used for only 4 to 6 hours per day,
together, whose urea clearance is only 70 ml/min. Yet
for the excretion of urea, the artificial kidney can func-
at a rate of 100 to 225 ml/min, which shows that at least
themselves to rid the body of unwanted substances.
discussed in Chapter 27, is the primary means for
cleared of different substances each minute, which, as
The effectiveness of the artificial kidney can be
Therefore, when a uremic patient is dialyzed, these sub-
or creatinine in the dialyzing fluid; however, these are
Note that there is no phosphate, urea, urate, sulfate,
solutes through the membrane during dialysis.
plasma. Instead, they are adjusted to levels that are
uremic plasma. Note that the concentrations of ions and
Table 31–7 compares the constituents in
bulk flow.
of the dialyzer; such filtration is called
tion to diffusion of solutes, mass transfer of solutes and
into the blood as it enters the artificial kidney. In addi-
the artificial kidney, a small amount of heparin is infused
square meters. To prevent coagulation of the blood in
Chapter 31
Kidney Diseases and Diuretics
415
the total diffusion surface area is between 0.6 and 2.5
water can be produced by applying a hydrostatic pres-
sure to force the fluid and solutes across the membranes
Dialyzing Fluid.
a typical dialyzing fluid with those in normal plasma and
other substances in dialyzing fluid are not the same as
the concentrations in normal plasma or in uremic
needed to cause appropriate movement of water and
present in high concentrations in the uremic blood.
stances are lost in large quantities into the dialyzing
fluid.
expressed in terms of the amount of plasma that is
expressing the functional effectiveness of the kidneys
Most artificial kidneys can clear urea from the plasma
tion about twice as rapidly as two normal kidneys
ance is still considerably limited when the artificial
to keep in mind that the artificial kidney cannot replace
blood cell production.
References
2003.
Table 31–7
Comparison of Dialyzing Fluid with Normal and Uremic
Urea
26
0
200
Glucose
100
125
100
0.5
0
3
0.3
0
2
3
0
9
1.2
1.2
1.2
24
35.7
14
107
105
107
1.5
1.5
1.5
3
3.0
2
5
1.0
7
142
133
142
Constituent
Plasma
Fluid
Plasma
Normal Dialyzing
Uremic
Plasma
Electrolytes (mEq/L)
Na
+
K
+
Ca
++
Mg
++
Cl
–
HCO
3
–
Lactate
–
HPO
4
=
Urate
–
Sulfate
=
Nonelectrolytes
Creatinine
1
0
6
