of the previous chapter; their special characteristics are the following.
tors, but many more similar to these also exist. Some were shown in Figure 46–1
There are at least six entirely different types of tactile recep-
Tactile Receptors.
signals, but some of the same types of receptors as those for touch and pressure
tissues; and (3) vibration sensation results from rapidly repetitive sensory
skin; (2) pressure sensation generally results from deformation of deeper
principal differences among them: (1) touch sensation generally results from
they are all detected by the same types of receptors. There are three
touch, pressure, and vibration are frequently classified as separate sensations,
Interrelations Among the Tactile Sensations of Touch, Pressure, and Vibration.
Tactile Sensations
Detection and Transmission of
muscles, and bone. These include mainly “deep” pressure, pain, and vibration.
are those that come from deep tissues, such as from fasciae,
one usually refers specifically to sensations from the internal organs.
are those from the viscera of the body; in using this term,
Visceral sensations
often considered a “special” sensation rather than a somatic sensation).
from the bottom of the feet, and even the sensation of equilibrium (which is
including position sensations, tendon and muscle sensations, pressure sensations
are those having to do with the physical state of the body,
are those from the surface of the body.
grouped together in other classes, as follows.
senses.
rate of movement
senses, and the position senses
tickle
, and
touch
Chapter 48 discusses the thermoreceptive and pain senses. The tactile senses
This chapter deals with the mechanoreceptive tactile and position senses.
, which is activated by any factor that damages the tissues.
, which detect heat and cold; and (3) the
, which include both
mechanoreceptive somatic senses
The somatic senses can be classified into three physiologic types: (1) the
CLASSIFICATION OF SOMATIC SENSES
smell, taste, and equilibrium.
, which mean specifically vision, hearing,
These senses are in contradistinction to the
collect sensory information from all over the body.
The
Position Senses
Organization, the Tactile and
Somatic Sensations: I. General
C
H
A
P
T
E
R
4
7
585
somatic senses are the nervous mechanisms that
special
senses
tactile and position sensa-
tions that are stimulated by mechanical displacement of some tissue of the body;
(2) the thermoreceptive senses
pain
sense
include
, pressure, vibration
include static position and
Other Classifications of Somatic Sensations.
Somatic sensations are also often
Exteroreceptive sensations
Proprio-
ceptive sensations
Deep sensations
Although
stimulation of tactile receptors in the skin or in tissues immediately beneath the
are used.
Meissner’s corpuscles, Iggo dome receptors, hair
Almost all specialized sensory receptors, such as
Transmission of Tactile Signals in Peripheral Nerve Fibers.
mechanical state of the tissues.
second. Therefore, they are particularly important for
skin and deep in the fascial tissues of the body. They
detail in Chapter 46, lie both immediately beneath the
Sixth, pacinian corpuscles, which were discussed in
heavy prolonged touch and pressure signals. They are
continuous states of deformation of the tissues, such as
very slowly and, therefore, are important for signaling
endings, as shown in Figure 46–1. These endings adapt
, which are multibranched, encapsulated
Ruffini’s
Fifth, located in the deeper layers of the skin and
initial contact with the body.
and, like Meissner’s corpuscles, detects mainly (a)
are also a touch receptor. This receptor adapts readily
hair and its basal nerve fiber, called the
stimulates a nerve fiber entwining its base. Thus, each
Fourth, slight movement of any hair on the body
along with the Meissner’s corpuscles discussed earlier,
). These receptors,
myelinated nerve fiber (type A
group of Merkel’s discs is innervated by a single large
extremely sensitive receptor. Also note that the entire
outward, thus creating a dome and constituting an
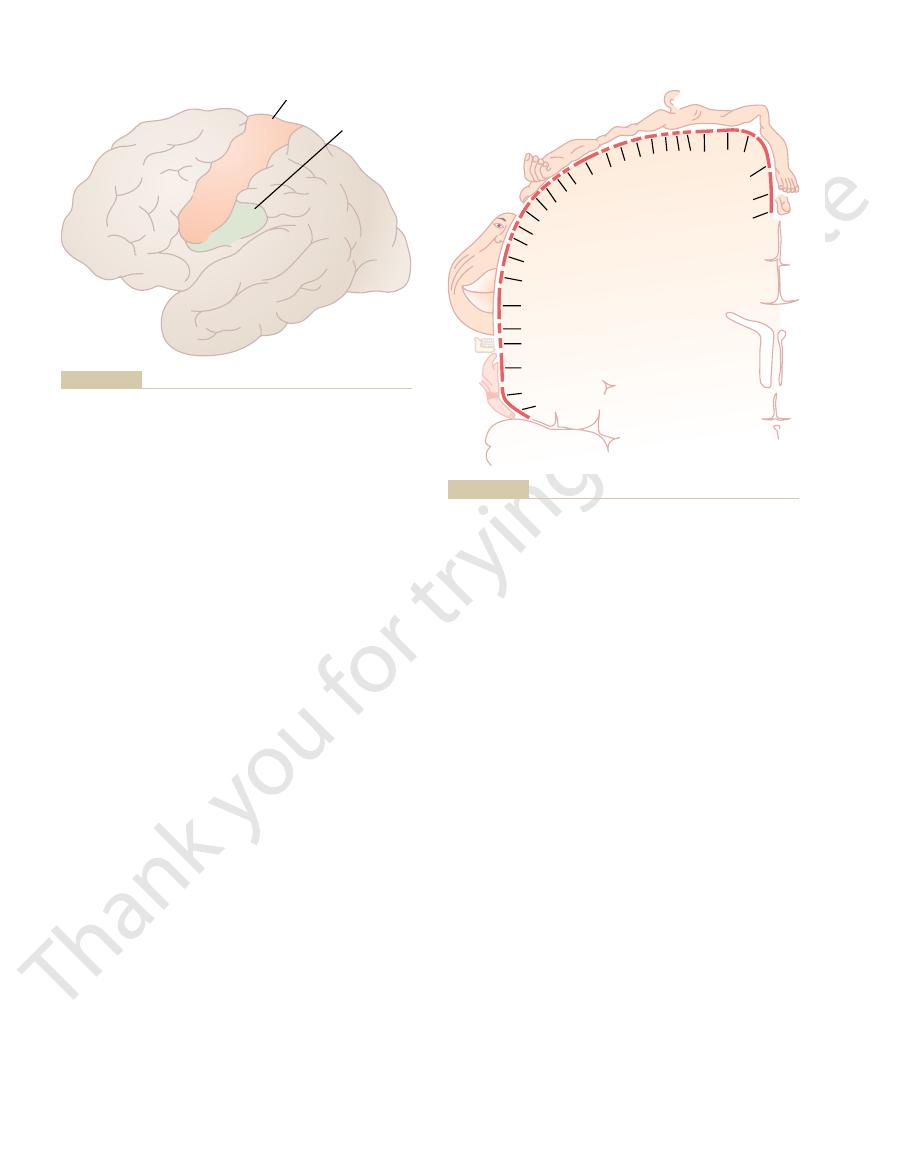
lium of the skin, as also shown in Figure 47–1. This
, which
Merkel’s discs are often grouped together in a
only slowly. Therefore, they are responsible for giving
receptors differ from Meissner’s corpuscles in that
they have almost no Meissner’s corpuscles. These
ate numbers of expanded tip receptors, even though
47–1. The hairy parts of the skin also contain moder-
shown in Figure
Merkel’s discs,
large numbers of Meissner’s corpuscles usually also
Third, the fingertips and other areas that contain
frequency vibration.
fraction of a second after they are stimulated, which
highly developed. Meissner’s corpuscles adapt in a
tips, lips, and other areas of the skin where one’s ability
These corpuscles are present in the nonhairy parts of
lation are many branching terminal nerve filaments.
) myelinated sensory nerve fiber. Inside the capsu-
(illustrated in Figure 46–1), an
Meissner’s corpuscle
Second, a touch receptor with great sensitivity is the
can nevertheless elicit touch and pressure sensations.
other type of nerve ending besides free nerve endings,
contact with the cornea of the eye, which contains no
detect touch and pressure. For instance, even light
everywhere in the skin and in many other tissues, can
, which are found
First, some
The Nervous System: A. General Principles and Sensory Physiology
586
Unit IX
free nerve endings
elongated encapsulated nerve ending of a large (type
A
b
the skin and are particularly abundant in the finger-
to discern spatial locations of touch sensations is
means that they are particularly sensitive to movement
of objects over the surface of the skin as well as to low-
contain large numbers of expanded tip tactile receptors,
one type of which is
they transmit an initially strong but partially adapting
signal and then a continuing weaker signal that adapts
steady-state signals that allow one to determine con-
tinuous touch of objects against the skin.
receptor organ called the Iggo dome receptor
projects upward against the underside of the epithe-
causes the epithelium at this point to protrude
b
play extremely important roles in localizing touch
sensations to specific surface areas of the body and in
determining the texture of what is felt.
hair end-organ,
movement of objects on the surface of the body or (b)
also in still deeper internal tissues are many
end-organs
also found in joint capsules and help to signal the
degree of joint rotation.
are stimulated only by rapid local compression of the
tissues because they adapt in a few hundredths of a
detecting tissue vibration or other rapid changes in the
10
m
m
FF
CF
A
AA
C
E
cle in hairy skin. J Physiol 200:
AR: The structure and function of
epithelium. (From Iggo A, Muir
tightly the undersurface of the
multiple numbers of Merkel’s
Iggo dome receptor. Note the
Figure 47–1
discs connecting to a single large
myelinated fiber and abutting
a slowly adapting touch corpus-
763, 1969.)
systems.
With this differentiation in mind, we can now
mechanoreceptive sensations.
The dorsal system is limited to discrete types of
pain, warmth, cold, and crude tactile sensations;
that the dorsal system does not have: the ability to
The anterolateral system has a special capability
column–medial lemniscal system; that which does not
two systems. That is, sensory information that must
system has much less spatial orientation. These
with respect to their origin, while the anterolateral
40 m/sec.
signals to the brain at velocities of 30 to 110 m/sec,
posed of large, myelinated nerve fibers that transmit
The dorsal column–medial lemniscal system is com-
thalamus.
and lateral white columns of the cord. They terminate
horns of the spinal gray matter, then cross to the oppo-
dorsal spinal nerve roots, synapse in the dorsal
Conversely, signals in the anterolateral system,
site side in the medulla, they continue upward through
Then, after the signals synapse and cross to the oppo-
name implies, carries signals upward to the medulla of
The dorsal column–medial lemniscal system, as its
of the thalamus.
. These
native sensory pathways: (1) the
the entry point into the cord and then to the brain, the
dorsal roots of the spinal nerves. However, from
Nervous System
Transmitting Somatic
Sensory Pathways for
in the cord by lateral inhibition, as described in
or if the scratch is strong enough to elicit pain. The
maneuvers that rid the host of the irritant. Itch can
crawling on the skin or a fly about to bite, and the
The purpose of the itch sensation is presumably to
nated fibers similar to those that transmit the aching,
sations are transmitted by very small type C, unmyeli-
and itch sensations usually can be elicited. These sen-
skin, which is also the only tissue from which the tickle
and itch sensations. Furthermore, these endings are
tence of very sensitive, rapidly adapting mechano-
TICKLE AND ITCH
than pacinian corpuscles.
Meissner’s corpuscles, which are less rapidly adapting
in contrast, stimulate other tactile receptors, especially
frequency vibrations from 2 up to 80 cycles per second,
transmit as many as 1000 impulses per second. Low-
nerve fibers, which can
mit their signals over type A
rapid deformations of the tissues, and they also trans-
signal vibrations from 30 to 800 cycles per second
quencies of vibration. Pacinian corpuscles can detect
tion, although different receptors detect different fre-
Detection of Vibration
nerve bundle than the fast fibers.
tickle, are transmitted by way of much slower, very
crude pressure, poorly localized touch, and especially
fibers. Conversely, the cruder types of signals, such as
the skin, minute gradations of intensity, or rapid
Thus, the more critical types of sensory signals—
serving mainly the sensation of tickle.
the spinal cord and lower brain stem, probably sub-
tion of a meter up to 2 m/sec; these send signals into
30 m/sec.
mit signals mainly by way of the small type A
Conversely, free nerve ending tactile receptors trans-
transmission velocities ranging from 30 to 70 m/sec.
transmit their signals in type A
receptors, pacinian corpuscles, and Ruffini’s endings,
Somatic Sensations: I. General Organization, the Tactile and Position Senses
Chapter 47
587
b nerve fibers that have
d myeli-
nated fibers that conduct at velocities of only 5 to
Some tactile free nerve endings transmit by way of
type C unmyelinated fibers at velocities from a frac-
those that help to determine precise localization on
changes in sensory signal intensity—are all transmit-
ted in more rapidly conducting types of sensory nerve
small nerve fibers that require much less space in the
All tactile receptors are involved in detection of vibra-
because they respond extremely rapidly to minute and
b
Neurophysiologic studies have demonstrated the exis-
receptive free nerve endings that elicit only the tickle
found almost exclusively in superficial layers of the
slow type of pain.
call attention to mild surface stimuli such as a flea
elicited signals then activate the scratch reflex or other
be relieved by scratching if this removes the irritant
pain signals are believed to suppress the itch signals
Chapter 48.
Signals into the Central
Almost all sensory information from the somatic seg-
ments of the body enters the spinal cord through the
sensory signals are carried through one of two alter-
dorsal column–medial
lemniscal system or (2) the anterolateral system
two systems come back together partially at the level
the brain mainly in the dorsal columns of the cord.
the brain stem to the thalamus by way of the medial
lemniscus.
immediately after entering the spinal cord from the
site side of the cord and ascend through the anterior
at all levels of the lower brain stem and in the
whereas the anterolateral system is composed of
smaller myelinated fibers that transmit signals at
velocities ranging from a few meters per second up to
Another difference between the two systems is
that the dorsal column–medial lemniscal system has a
high degree of spatial orientation of the nerve fibers
differences immediately characterize the types of
sensory information that can be transmitted by the
be transmitted rapidly and with temporal and
spatial fidelity is transmitted mainly in the dorsal
need to be transmitted rapidly or with great spatial
fidelity is transmitted mainly in the anterolateral
system.
transmit a broad spectrum of sensory modalities—
most of these are discussed in detail in Chapter 48.
list the types of sensations transmitted in the two

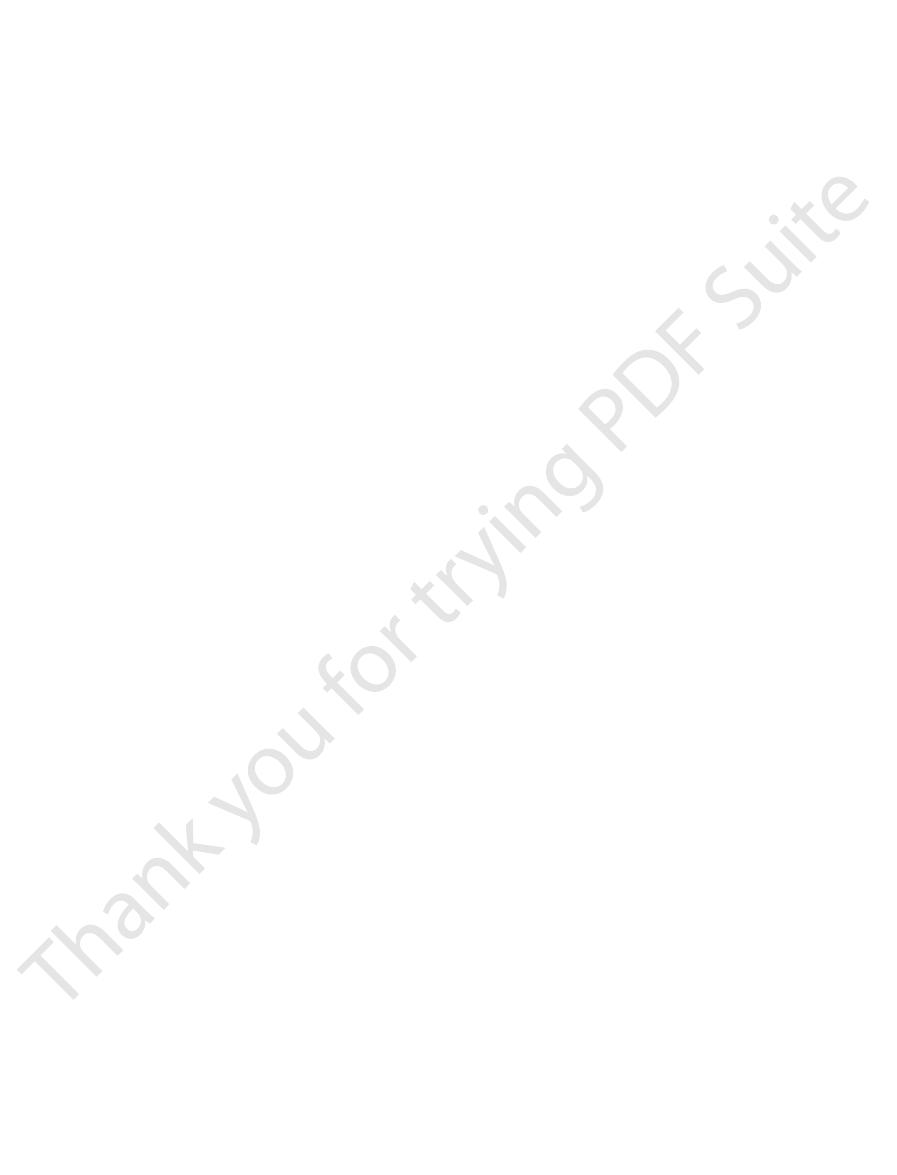
second-order neurons
). From there,
pass uninterrupted up to the dorsal medulla, where
47–3 that nerve fibers entering the dorsal columns
Note in Figure
The Dorsal Column–Medial Lemniscal Pathway.
Others give rise to the spinocerebellar tracts, which we
cord reflexes, which are discussed in Chapter 54. (3)
local neurons in turn serve three functions: (1) A major
and anterior portions of the cord gray matter. These
gray matter, then divides many times to provide termi-
The lateral branch enters the dorsal horn of the cord
then upward in the dorsal column, proceeding by way
Figure 47–2. The medial branch turns medially first and
, shown by
lateral branch
medial branch
dorsal roots, the large myelinated fibers from the spe-
Anatomy of the Dorsal
Transmission in the
5. Sexual sensations
4. Tickle and itch sensations
3. Crude touch and pressure sensations capable only
2. Thermal sensations, including both warmth and
1. Pain
6. Pressure sensations having to do with fine degrees
5. Position sensations from the joints
4. Sensations that signal movement against the skin
3. Phasic sensations, such as vibratory sensations
2. Touch sensations requiring transmission of fine
1. Touch sensations requiring a high degree of
The Nervous System: A. General Principles and Sensory Physiology
588
Unit IX
Dorsal Column–Medial
Lemniscal System
localization of the stimulus
gradations of intensity
of judgment of pressure intensity
Anterolateral System
cold sensations
of crude localizing ability on the surface of the
body
Dorsal Column–Medial
Lemniscal System
Column–Medial Lemniscal System
On entering the spinal cord through the spinal nerve
cialized mechanoreceptors divide almost immediately
to form a
and a
the right-hand fiber entering through the spinal root in
of the dorsal column pathway all the way to the brain.
nals that synapse with local neurons in the intermediate
share of them give off fibers that enter the dorsal
columns of the cord and then travel upward to the brain.
(2) Many of the fibers are very short and terminate
locally in the spinal cord gray matter to elicit local spinal
will discuss in Chapter 56 in relation to the function of
the cerebellum.
they synapse in the dorsal column nuclei (the cuneate
and gracile nuclei
VII
VI
V
IV
III
II
I
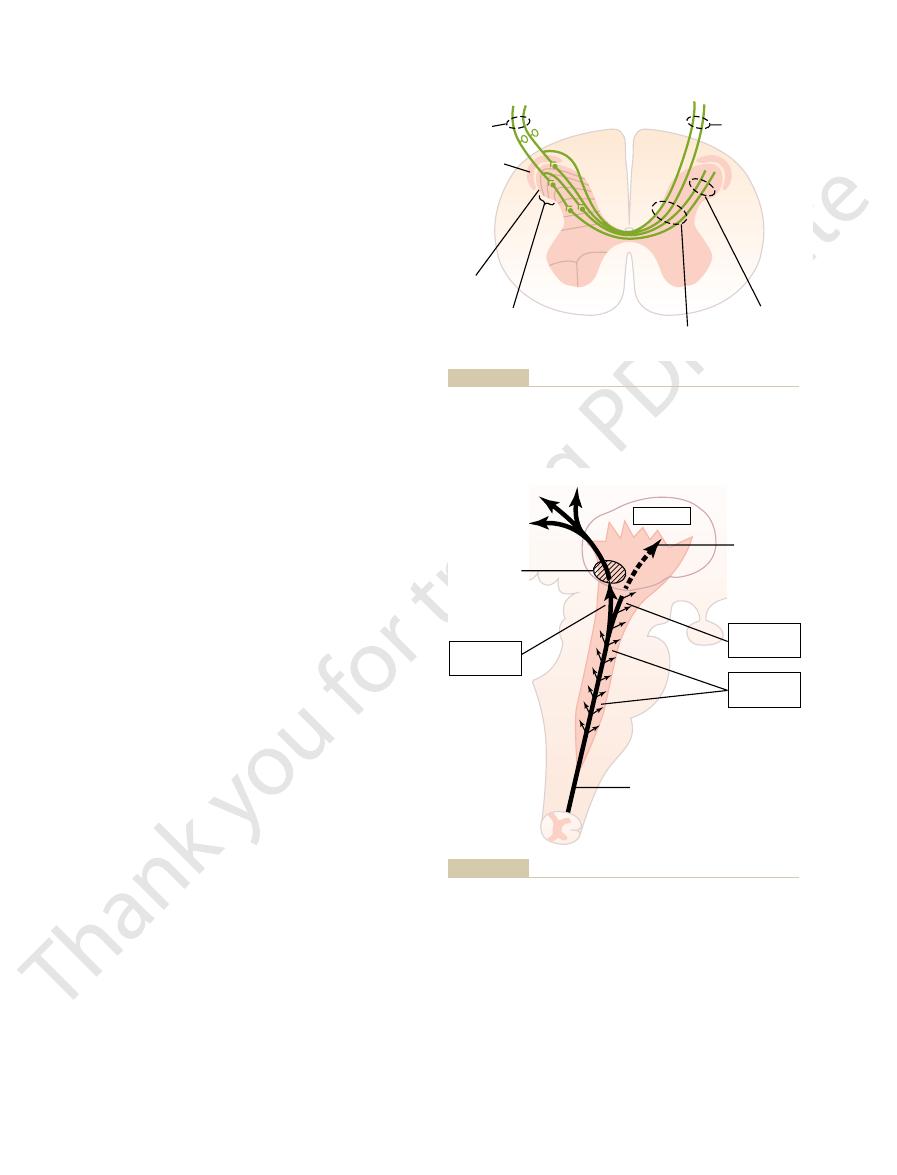
VIII
IX
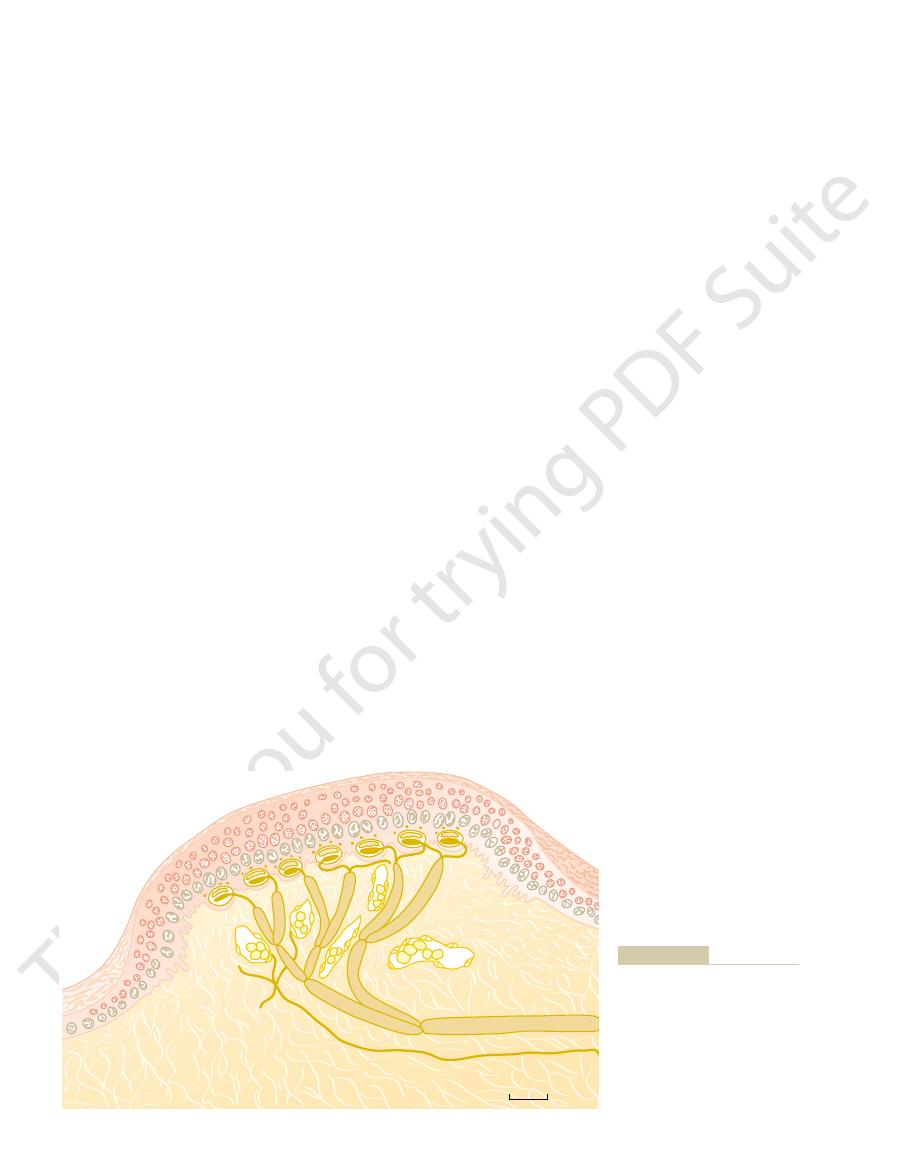
Dorsal
column
Anterolateral
spinothalamic
pathway
Lamina marginalis
Substantia gelatinosa
Spinal nerve
Tract of
Lissauer
Spinocervical
tract
Dorsal
spinocerebellar
tract
Ventral
spinocerebellar
tract
of the spinal cord.
gray matter and of ascending sensory tracts in the white columns
Cross section of the spinal cord, showing the anatomy of the cord
Figure 47–2
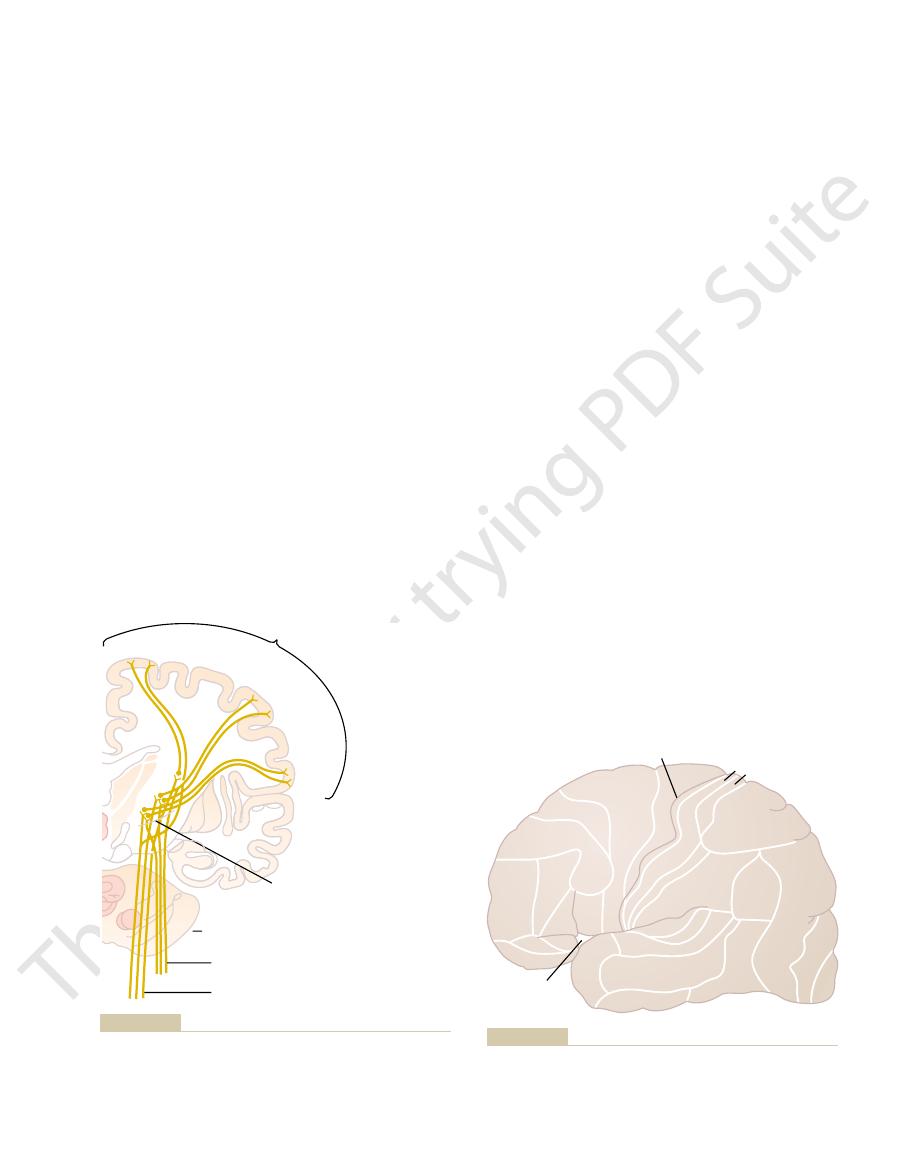
Medulla oblongata
Cortex
Spinal cord
Dorsal root and spinal
ganglion
Medial lemniscus
Dorsal column nuclei
Ascending branches of
dorsal root fibers
Spinocervical tract
Ventrobasal
complex
of thalamus
Internal
capsule
ical types of tactile signals. (Modified from Ranson SW, Clark SL:
Figure 47–3
The dorsal column–medial lemniscal pathway for transmitting crit-
Anatomy of the Nervous System. Philadelphia: WB Saunders Co,
1959.)
contractions and body movements. A major share of
Conversely, that portion of the cerebral cortex ante-
in the temporal lobe.
terminate in the occipital lobe, and
Visual signals
. But the posterior
generally, the anterior half of the parietal lobe is
immediately posterior to the central fissure. And,
the brain. In general, sensory signals from all modali-
based on histological structural differences. This map
Brodmann’s areas
of the human cerebral cortex, showing that it is divided
the various areas of the cortex. Figure 47–5 is a map
somatic sensation, we need to give an orientation to
the thalamus.
mus, and the right side of the body in the left side of
of the medial lemnisci in the medulla, the left side of
medial areas of the complex. Because of the crossing
maintained, with the tail end of the body represented
In the thalamus, distinct spatial orientation is still
laterally.
cord, whereas those that enter the cord at progres-
in the dorsal columns of the spinal cord, the fibers from
the body that is maintained throughout. For instance,
Spatial Orientation of the Nerve Fibers in the
(as shown in Figure 47–6,
, which is
project, as shown in Figure 47–4, mainly to
third-order
From the ventrobasal complex,
in the thalamic sensory relay area, called the
In the thalamus, the medial lemniscal fibers terminate
that the dorsal column fibers subserve for the body.
; these
to the thalamus. In this pathway through the brain stem,
Somatic Sensations: I. General Organization, the Tactile and Position Senses
Chapter 47
589
decussate immediately to the opposite side of the brain
stem and continue upward through the medial lemnisci
each medial lemniscus is joined by additional fibers
from the sensory nuclei of the trigeminal nerve
fibers subserve the same sensory functions for the head
ventrobasal
complex.
nerve fibers
the postcentral gyrus of the cerebral cortex
called somatic sensory area I
these fibers also project to a smaller area in the lateral
parietal cortex called somatic sensory area II).
Dorsal Column-Medial Lemniscal System
One of the distinguishing features of the dorsal
column–medial lemniscal system is a distinct spatial
orientation of nerve fibers from the individual parts of
the lower parts of the body lie toward the center of the
sively higher segmental levels form successive layers
by the most lateral portions of the ventrobasal
complex and the head and face represented by the
the body is represented in the right side of the thala-
Somatosensory Cortex
Before discussing the role of the cerebral cortex in
into about 50 distinct areas called
is important because virtually all neurophysiologists
and neurologists use it to refer by number to many of
the different functional areas of the human cortex.
Note in the figure the large central fissure (also
called central sulcus) that extends horizontally across
ties of sensation terminate in the cerebral cortex
concerned almost entirely with reception and inter-
pretation of somatosensory signals
half of the parietal lobe provides still higher levels of
interpretation.
auditory signals
rior to the central fissure and constituting the poste-
rior half of the frontal lobe is called the motor cortex
and is devoted almost entirely to control of muscle
this motor control is in response to somatosensory
Lower extremity
Upper
extremity
Ventrobasal complex of thalamus
POSTCENTRAL GYRUS
MESENCEPHALON
Spinothalamic tract
Medial lemniscus
Trunk
Face
University Press.)
York: Oxford University Press, 1969, by permission of Oxford
A: Neurological Anatomy in Relation to Clinical Medicine. New
the thalamus to the somatosensory cortex. (Modified from Brodal
Projection of the dorsal column–medial lemniscal system through
Figure 47–4
Central fissure
Lateral fissure
4
5
3 2
7a
7a
39
19
18
17
37
21
20
38
45
47
11
10
46
9
8
6
1
40
41
42
22
43
44
somatosensory association area
, and areas 5 and 7, which con-
primary somatosensory area I
cerebral cortex. Note specifically areas 1, 2, and 3, which consti-
Structurally distinct areas, called Brodmann’s areas, of the human
Figure 47–5
tute
stitute the
.
in other layers. Some of these functions are:
Figure 47–8. As would be expected, the neurons in
extending progressively deeper to layer VI, shown in
layers of neurons,
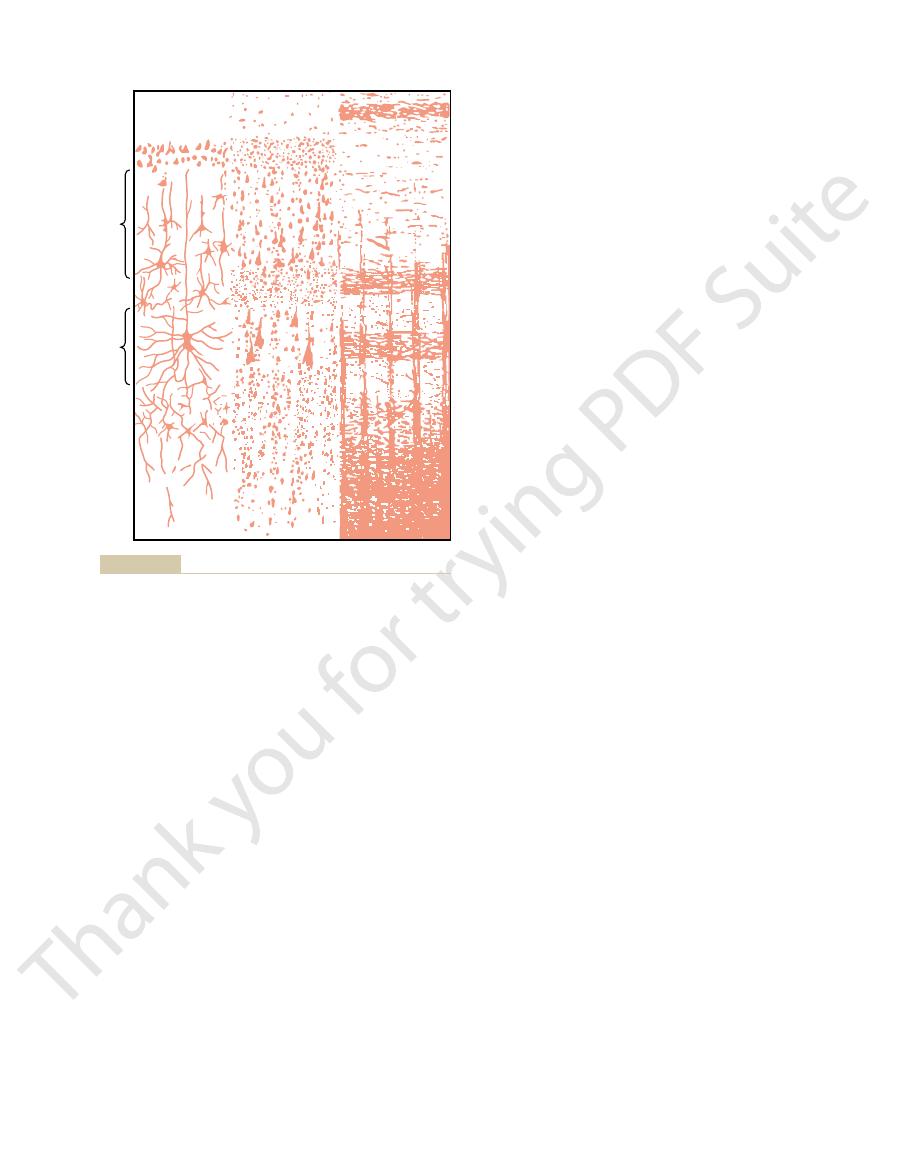
The cerebral cortex contains
Layers of the Somatosensory Cortex and
part of the body is represented medially.
lateral portion of somatosensory area I, and the lower
endings are found in the lips and thumb, whereas only
body. For instance, a great number of specialized nerve
tively small areas. The sizes of these areas are directly
Some areas of the body are represented by large
site side of the body.
however, that each lateral side of the cortex receives
separate regions of somatosensory area I. Note,
at the level of the postcentral gyrus, demonstrating
Figure 47–7 shows a cross section through the brain
Brodmann’s areas 3, 1, and 2).
immediately behind the central fissure, located in the
in Somatosensory Area I.
somatosensory area I. Thus, much of what we know
However, removal of parts of somatosensory area II
auditory areas. Projections from somatosensory area I
sensory areas of the brain, even from the visual and
the body. In addition, many signals come secondarily
the brain stem, transmitted upward from both sides of
area II. It is known that signals enter this area from
the arms centrally, and the legs posteriorly.
II, although roughly, the face is represented anteriorly,
By contrast, localization is poor in somatosensory area
names of virtually all parts of the body in Figure 47–6.
tion of the different parts of the body, as shown by the
“somatosensory cortex” almost always means area I.
somatosensory area II that in popular usage, the term
areas. However, somatosensory area I is so much
. The
Figure 47–6 shows two sep-
Somatosensory Areas I and II.
ent body parts.
cortex, which keep the motor cortex informed at each
The Nervous System: A. General Principles and Sensory Physiology
590
Unit IX
signals received from the sensory portions of the
instant about the positions and motions of the differ-
arate sensory areas in the anterior parietal lobe called
somatosensory area I and somatosensory area II
reason for this division into two areas is that a distinct
and separate spatial orientation of the different
parts of the body is found in each of these two
more extensive and so much more important than
Somatosensory area I has a high degree of localiza-
Little is known about the function of somatosensory
from somatosensory area I as well as from other
are required for function of somatosensory area II.
has no apparent effect on the response of neurons in
about somatic sensation appears to be explained by
the functions of somatosensory area I.
Spatial Orientation of Signals from Different Parts of the Body
Somatosensory area I lies
postcentral gyrus of the human cerebral cortex (in
representations of the different parts of the body in
sensory information almost exclusively from the oppo-
areas in the somatic cortex—the lips the greatest of all,
followed by the face and thumb—whereas the trunk
and lower part of the body are represented by rela-
proportional to the number of specialized sensory
receptors in each respective peripheral area of the
a few are present in the skin of the body trunk.
Note also that the head is represented in the most
Their Function
six
beginning with layer I next to the brain surface and
each layer perform functions different from those
Somatosensory
area I
Somatosensory
area II
Thigh
Thorax
Neck
Shoulder
Hand
Fingers
Tongue
Leg
Arm
Face
Abdomen
Two somatosensory cortical areas, somatosensory areas I and II.
Figure 47–6
Intra-abdominal
Pharynx
Tongue
Teeth, gums, and jaw
Lower lip
Lips
Upper lip
Face
Nose
Eye
Thumb
Index finger
Middle finger
Ring finger
Little finger
Hand
Wrist
For
earm
Elbow
A
rm
Shoulder
Head Neck
Trunk
Hip
Leg
Foot
Toes
Genital
s
New York: Hafner, 1968.)
bral Cortex of Man: A Clinical Study of Localization of Function.
sory area I of the cortex. (From Penfield W, Rasmussen T: Cere-
Representation of the different areas of the body in somatosen-
Figure 47–7
objects. This is called
4. The person is unable to judge shapes or forms of
objects.
3. The person is unable to judge the weights of
pressure against the body.
2. The person is unable to judge critical degrees of
legs. Thus, it is clear that the brain stem, thalamus,
a major level of the body trunk, or to one of the
sensations crudely, such as to a particular hand, to
body. However, he or she can localize these
1. The person is unable to localize discretely the
Widespread bilateral excision of somatosensory area I
Functions of Somatosensory Area I
discuss subsequently.
, as we
from somatosensory area I into the parietal cortex, an
tation of sensory signals; the process becomes even
direction. Thus, this is a still higher order of interpre-
I, about 6 per cent of the vertical columns respond only
sensitive to deep pressure.
farther posteriorly, greater numbers of the columns are
slowly adapting cutaneous receptors, and then still
central fissure. These signals play a major role in
sensory columns then spread anteriorly, directly to
stretch receptors. Many of the signals from these
vertical columns respond to muscle, tendon, and joint
Brodmann’s area 3a, an especially large share of the
central gyrus, located deep in the central fissure in
initiate analysis of the meanings of the sensory signals.
At other levels of the columns, interactions occur that
function almost entirely separately from one another.
signals first enter the cortex, the columns of neurons
and so forth. At layer IV, where the input sensory
around joints, some to stimulation of tactile hairs,
ity, some columns responding to stretch receptors
taining perhaps 10,000 neuronal cell bodies. Each of
through the six layers of the cortex, each column
Functionally, the neurons of the somatosensory cortex
Specific Sensory Modality
Different Sensory Spot on the Body with a
Columns of Neurons; Each Column Detects a
The Sensory Cortex Is Organized in Vertical
thalamus.
numbers of axons extend to the thalamus,
transmission. From layer VI, especially large
areas, such as to the basal ganglia, brain stem,
deeper parts of the nervous system. Those in layer
4. The neurons in layers V and VI send axons to the
3. The neurons in layers II and III send axons to
described in Chapter 57. This input mainly
specific regions of the cortex; this system is
2. Layers I and II receive diffuse, nonspecific input
layers.
layer IV first; then the signal spreads toward the
1. The incoming sensory signal excites neuronal
Somatic Sensations: I. General Organization, the Tactile and Position Senses
Chapter 47
591
surface of the cortex and also toward deeper
signals from lower brain centers that facilitate
controls the overall level of excitability of the
respective regions stimulated.
related portions of the cerebral cortex on the
opposite side of the brain through the corpus
callosum.
V are generally larger and project to more distant
and spinal cord where they control signal
providing signals from the cerebral cortex that
interact with and help to control the excitatory
levels of incoming sensory signals entering the
are arranged in vertical columns extending all the way
having a diameter of 0.3 to 0.5 millimeter and con-
these columns serves a single specific sensory modal-
others to discrete localized pressure points on the skin,
In the most anterior 5 to 10 millimeters of the post-
the motor cortex located immediately forward of the
controlling the effluent motor signals that activate
sequences of muscle contraction.
As one moves posteriorly in somatosensory area I,
more and more of the vertical columns respond to
In the most posterior portion of somatosensory area
when a stimulus moves across the skin in a particular
more complex as the signals spread farther backward
area called the somatosensory association area
causes loss of the following types of sensory judgment:
different sensations in the different parts of the
or parts of the cerebral cortex not normally
considered to be concerned with somatic
sensations can perform some degree of
localization.
astereognosis.
I
VIb
VIa
V
IV
III
II
Brodmann]: Anatomy of the Nervous System. Philadelphia: WB
fusiform or polymorphic cells. (From Ranson SW, Clark SL [after
nal granular layer; V, large pyramidal cell layer; and VI, layer of
external granular layer; III, layer of small pyramidal cells; IV, inter-
Structure of the cerebral cortex, showing I, molecular layer; II,
Figure 47–8
Saunders, 1959.)
1 to 2 millimeters. However, on the person’s back,
the fingers, a person can distinguish two separate
points of stimulus are felt or one point. On the tips of
the same time, and the person determines whether two
test, two needles are pressed lightly against the skin at
so-called “two-point” discriminatory ability. In this
test tactile discrimination is to determine a person’s
Two-Point Discrimination.
center.
fire, but those in the center discharge at a considerably
fire. A stronger stimulus causes still more neurons to
cortical “field” for each respective receptor. Thus, a
synaptic stage, divergence occurs. The upper curves of
dorsal column pathway, demonstrating that at each
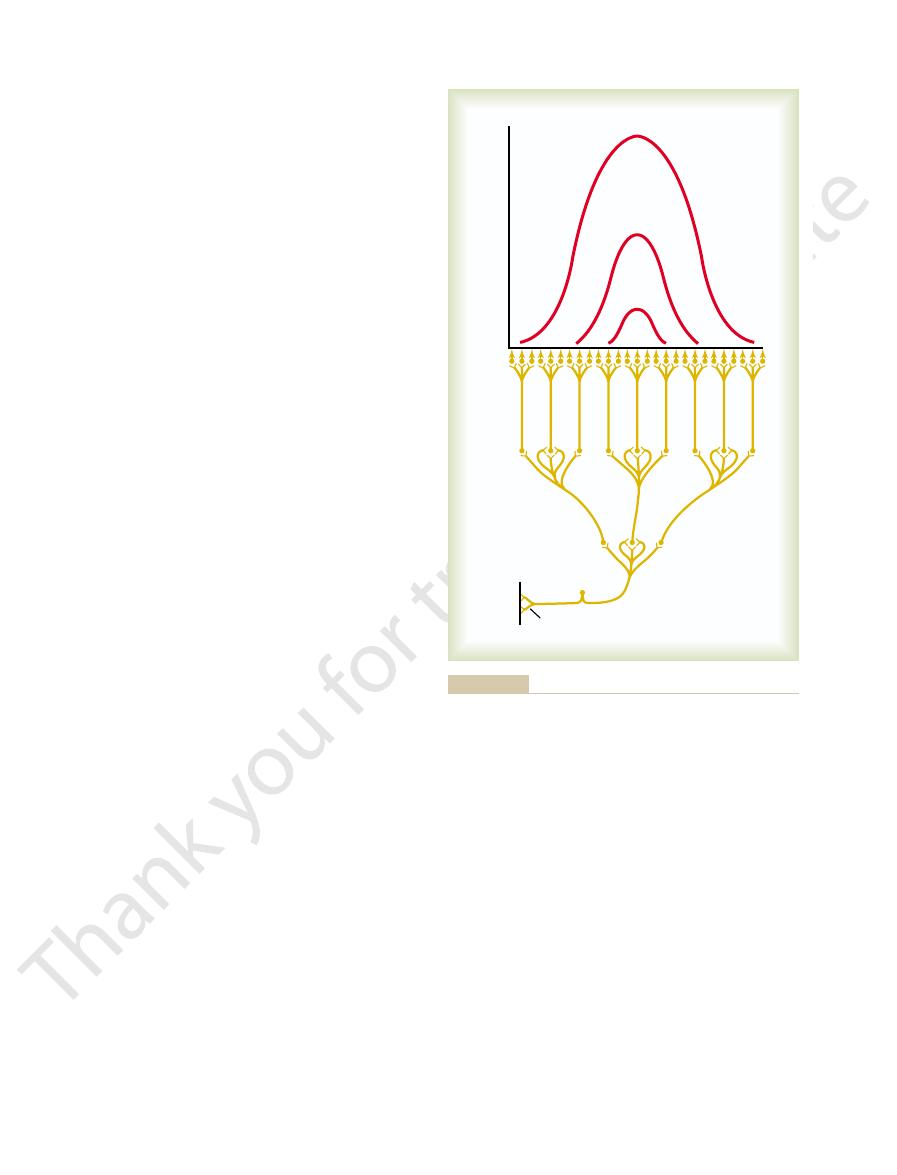
The lower part of Figure 47–9 shows the basic
in the Dorsal Column
Transmission and Analysis
even exists. This complex sensory deficit is called
feeling objects, the person tends to recognize only
side for motor functions as well. Likewise, when
Therefore, he or she also often forgets to use the other
side of the body—that is, forgets that it is there.
In fact, the person is mainly oblivious to the opposite
or her own body or body parts on the opposite side.
tion, he or she loses most of the sense of form of his
forms felt on the opposite side of the body. In addi-
area is removed on one side of the brain, the person
When the somatosensory association
Effect of Removing the Somatosensory Association Area—
thalamus, (4) the visual cortex, and (5) the auditory
trobasal nuclei of the thalamus, (3) other areas of the
signals from (1) somatosensory area I, (2) the ven-
decipher its meaning. This also fits with the anatomi-
Therefore, it seems clear that the somatosensory asso-
the “feeling” of an object such as a knife or a ball.
experience a complex body sensation, sometimes even
in the somatosensory areas. Therefore, these areas are
area I (see Figure 47–5), play important roles in deci-
Brodmann’s areas 5 and 7 of the cerebral cortex,
somatosensory area I to localize the source.
intensity. But the sensations are poorly localized, indi-
of only somatosensory area I, appreciation of these
of pain and temperature sense. In specific absence
5. The person is unable to judge texture of materials
The Nervous System: A. General Principles and Sensory Physiology
592
Unit IX
because this type of judgment depends on highly
critical sensations caused by movement of the
fingers over the surface to be judged.
Note that in the list nothing has been said about loss
sensory modalities is still preserved both in quality and
cating that pain and temperature localization depend
greatly on the topographical map of the body in
Somatosensory Association Areas
located in the parietal cortex behind somatosensory
phering deeper meanings of the sensory information
called somatosensory association areas.
Electrical stimulation in a somatosensory associa-
tion area can occasionally cause an awake person to
ciation area combines information arriving from mul-
tiple points in the primary somatosensory area to
cal arrangement of the neuronal tracts that enter the
somatosensory association area because it receives
cortex.
Amorphosynthesis.
loses ability to recognize complex objects and complex
one side of the object and forgets that the other side
amorphosynthesis.
Overall Characteristics of Signal
–Medial
Lemniscal System
Basic Neuronal Circuit in the Dorsal Column–Medial Lemniscal
System.
organization of the neuronal circuit of the spinal cord
the figure show that the cortical neurons that discharge
to the greatest extent are those in a central part of the
weak stimulus causes only the centralmost neurons to
more rapid rate than do those farther away from the
A method frequently used to
points even when the needles are as close together as
the needles must usually be as far apart as 30 to 70
Discharges per second
Cortex
Thalamus
Dorsal column nuclei
Single-point stimulus on skin
Strong stimulus
Moderate
stimulus
Weak
stimulus
Transmission of a pinpoint stimulus signal to the cerebral cortex.
Figure 47–9
As a partial explanation of these effects, Figure 46–4
pressure differences of 10,000 to 100,000 times.
as much as a half million times; and the skin can detect
two experiences can vary more than 10 billion times; the
sive sound, even though the sound intensities of these
ences of tremendously varying intensities? For instance,
The first question that comes to mind is, how is it pos-
roundings. Therefore, it is important that we discuss
The ultimate goal of most sensory stimulation is to
Interpretation of Sensory
tional integrity of the dorsal columns.
reason, application of vibration (e.g., from a “tuning
mitted only in the dorsal column pathway. For this
Meissner’s corpuscles as well. These signals are trans-
skin and deeper tissues, but lower-frequency signals
cycles per second. The higher-frequency vibratory
Vibratory signals are rapidly
Vibratory Sensation.
potentials, this system can recognize changing stimuli
peripheral conditions. Based on recorded action
The dorsal column system also is of particular impor-
Transmission of Rapidly Changing and Repetitive Sensations.
two red curves in Figure 47–10, showing complete
lation is blocked. This effect is demonstrated by the
stand out, and much of the surrounding diffuse stimu-
excitatory signal. As a result, the peaks of excitation
and (3) the cortex itself. At each of these levels, the
medulla, (2) the ventrobasal nuclei of the thalamus,
instance, in (1) the dorsal column nuclei of the
In the case of the dorsal column system, lateral
lateral spread of the excitatory signals and, therefore,
The importance of
secrete an inhibitory transmitter.
inhibitory signals to the surrounding neurons. That is,
excitatory signal, short lateral pathways transmit
in a dorsal column nucleus. Aside from the central
neurons. For instance, consider an excited neuron
signals; these spread to the
sensory pathway, when excited, gives rise simultane-
As pointed out in Chapter 46, virtually every
, as
point. The capability of the sensorium to distinguish
ence of two stimulatory points, rather than a single
a valley, allow the sensory cortex to detect the pres-
has two separate peaks. These two peaks, separated by
taneously. Note that the resultant zone of excitation
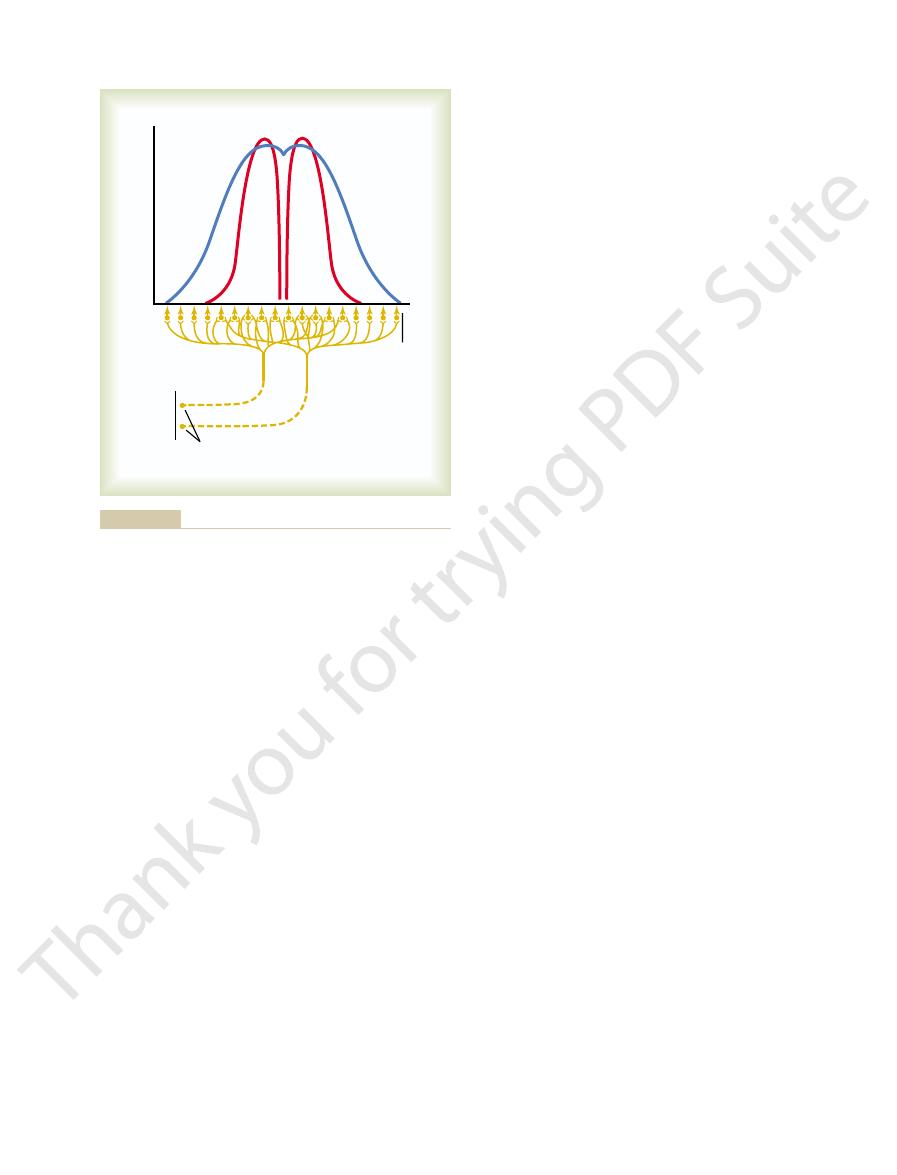
The blue curve shows the spatial pattern of cortical
are excited by signals from the two stimulated points.
mation. This figure shows two adjacent points on the
Figure 47–10 shows the mechanism by which the
areas.
detected. The reason for this difference is the different
Somatic Sensations: I. General Organization, the Tactile and Position Senses
Chapter 47
593
millimeters before two separate points can be
numbers of specialized tactile receptors in the two
dorsal column pathway (as well as all other sensory
pathways) transmits two-point discriminatory infor-
skin that are strongly stimulated as well as the areas
of the somatosensory cortex (greatly enlarged) that
excitation when both skin points are stimulated simul-
this presence of two points of stimulation is strongly
influenced by another mechanism, lateral inhibition
explained in the next section.
Effect of Lateral Inhibition (Also Called Surround Inhibition) to
Increase the Degree of Contrast in the Perceived Spatial
Pattern.
ously to lateral inhibitory
sides of the excitatory signal and inhibit adjacent
these signals pass through additional interneurons that
lateral inhibition is that it blocks
increases the degree of contrast in the sensory pattern
perceived in the cerebral cortex.
inhibitory signals occur at each synaptic level—for
lateral inhibition helps to block lateral spread of the
separation of the peaks when the intensity of lateral
inhibition is great.
tance in apprising the sensorium of rapidly changing
that occur in as little as 1/400 of a second.
repetitive and can be detected as vibration up to 700
signals originate from the pacinian corpuscles in the
(below about 200 per second) can originate from
fork”) to different peripheral parts of the body is an
important tool used by neurologists for testing func-
Stimulus Intensity
apprise the psyche of the state of the body and its sur-
briefly some of the principles related to transmission of
sensory stimulus intensity to the higher levels of the
nervous system.
sible for the sensory system to transmit sensory experi-
the auditory system can detect the weakest possible
whisper but can also discern the meanings of an explo-
eyes can see visual images with light intensities that vary
in the previous chapter shows the relation of the recep-
tor potential produced by the pacinian corpuscle to the
Discharges per second
Cortex
Two adjacent points
strongly stimulated
sent the pattern when “surround” inhibition does occur.
tion without “surround” inhibition, and the two red curves repre-
stimuli. The blue curve represents the pattern of cortical stimula-
Transmission of signals to the cortex from two adjacent pinpoint
Figure 47–10
of change. Therefore, multiple different types of recep-
static and dynamic, depends on knowing the degrees
Knowledge of position, both
Position Sensory Receptors.
, also called
movement sense
the body with respect to one another, and (2)
, which means conscious per-
. They can be divided into two subtypes:
The
, K, and k are found, a linear relation
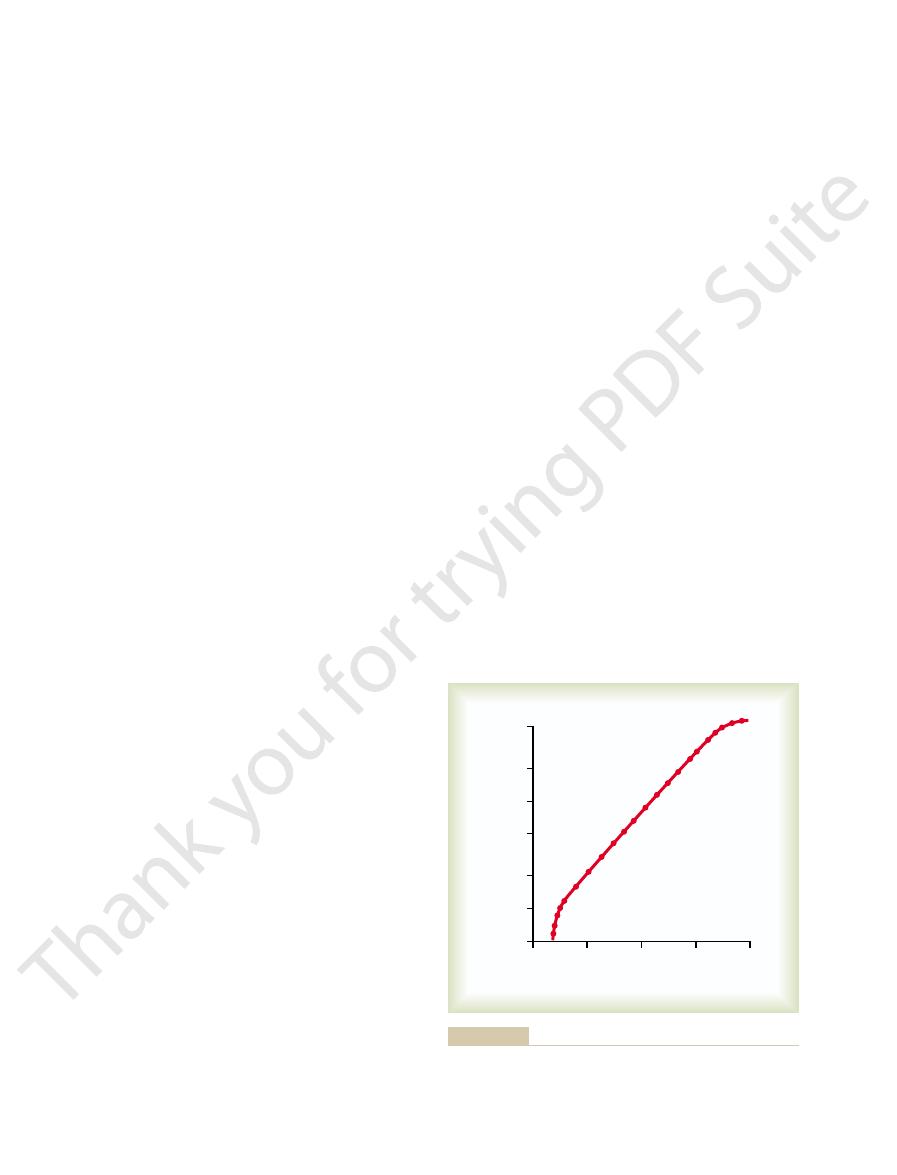
Figure 47–11, and when appropriate quantitative values
using double logarithmic coordinates, as shown in
When this power law relation is plotted on a graph
In this formula, the exponent
formula, known as the power law.
Power Law.
be for the psyche to detect the change.
sensory intensity, the greater an additional change must
Fechner principle is still a good one to remember,
other types of sensory experience. Yet the Weber-
higher intensities of visual, auditory, and cutaneous
Fechner principle is quantitatively accurate only for
More recently, it has become evident that the Weber-
means. To express this mathematically.
about 1 to 30, which is what the logarithmic principle
instance, the
barely detect a 10-gram increase in weight. Thus, in this
And, when already holding 300 grams, he or she can
That is, a person
strength are discriminated approximately in proportion
In the mid-1800s, Weber first and Fechner later
Weber-Fechner Principle—Detection of “Ratio” of Stimulus
Judgment of Stimulus Intensity
sunlight or at twilight; the camera cannot do this without
light. Yet, that person’s own eyes are capable of dis-
sity, a person almost always overexposes the film on
a light meter. Left to intuitive judgment of light inten-
with a camera, to adjust the light exposure without using
the attempts of most people, when taking photographs
operating in the wrong range. This is demonstrated by
range of sensory reception that we can experience, the
Were it not for the tremendous intensity
Importance of the Tremendous Intensity Range of Sensory
intensity levels changing as much as millions of times.
other mechanisms, makes it possible for some sensory
sity on impulse rate in each nerve fiber, as well as several
This mechanism, plus the direct effect of stimulus inten-
fibers, which is another mechanism by which stimulus
point also become stimulated. Thus, signals are trans-
sound intensity increases, many more hair cells in each
at the point of maximum sound vibration. But as the
membrane, weak sound stimulates only those hair cells
When sound stimulates a specific point on the basilar
method for separating gradations of stimulus intensity.
The transduction mechanism for detecting sound by
change
intensity levels, but at high-intensity levels, the change
changes
further increases in receptor potential are slight. Thus,
markedly, whereas at high levels of stimulus intensity,
sity, slight changes in intensity increase the potential
intensity of the sensory stimulus. At low stimulus inten-
The Nervous System: A. General Principles and Sensory Physiology
594
Unit IX
the pacinian corpuscle is capable of accurately measur-
ing extremely minute
in stimulus at low-
in stimulus must be much greater to cause the same
amount of
in receptor potential.
the cochlea of the ear demonstrates still another
direction farther away from the maximum vibratory
mitted over progressively increasing numbers of nerve
intensity is transmitted to the central nervous system.
systems to operate reasonably faithfully at stimulus
Reception.
various sensory systems would more often than not be
bright days and greatly underexposes the film at twi-
criminating with great detail visual objects in bright
very special manipulation because of the narrow criti-
cal range of light intensity required for proper exposure
of film.
Strength.
proposed the principle that gradations of stimulus
to the logarithm of stimulus strength.
already holding 30 grams weight in his or her hand can
barely detect an additional 1-gram increase in weight.
ratio of the change in stimulus strength
required for detection remains essentially constant,
Interpreted signal strength = Log (Stimulus)
+ Constant
sensory experience and applies only poorly to most
because it emphasizes that the greater the background
Another attempt by physiopsychologists to
find a good mathematical relation is the following
Interpreted signal strength = K • (Stimulus
- k)
y
y and the constants K and
k are different for each type of sensation.
for the constants y
can be attained between interpreted stimulus strength
and actual stimulus strength over a large range for
almost any type of sensory perception.
Position Senses
position senses are frequently also called proprio-
ceptive senses
(1) static position sense
ception of the orientation of the different parts of
rate of
kinesthesia or dynamic
proprioception.
of angulation of all joints in all planes and their rates
tors help to determine joint angulation and are used
0
10
100
1000
10,000
Stimulus strength (arbitrary units)
Interpreted stimulus strength
(arbitrary units)
0
10
20
50
100
200
500
or very strong stimulus strengths.
to be. Note that the power law does not hold at either very weak
actual stimulus strength and strength that the psyche interprets it
Graphical demonstration of the “power law” relation between
Figure 47–11
nized in 10 to 20 gradations of strength, rather than as
far less accurate, most of the sensations being recog-
signals is poor; (3) the gradations of intensities are also
and 40 m/sec; (2) the degree of spatial localization of
column–medial lemniscal system, ranging between 8
lowing differences: (1) the velocities of transmission
column–medial lemniscal system, except for the fol-
In general, the same principles apply to transmission
Characteristics of Transmission in the Anterolateral Pathway.
pain signals are further processed, as discussed in
amus. Instead, most pain signals terminate in the retic-
Conversely, only a small fraction of the pain signals
along with the signals from the dorsal columns.
dorsal column tactile signals terminate. From here, the
transmitted mainly into the ventrobasal complex, ter-
. In general, the tactile signals are
of the thalamus, the
mainly twofold: (1) throughout the
The upper terminus of the two spinothalamic tracts is
As shown in Figure 47–13, the anterolateral fibers
These laminae are where many of the dorsal root
dorsal horn laminae I, IV, V, and VI (see Figure 47–2).
spinal cord anterolateral fibers
The
sensations will be discussed specifically.
sexual sensations. In Chapter 48, pain and temperature
include pain, heat, cold, crude tactile, tickle, itch, and
of fine gradations of intensity. These types of signals
trast to the dorsal column pathway, transmits sensory
signals up the spinal cord and into the brain, in con-
The anterolateral pathway for transmitting sensory
Anterolateral Pathway
Sensory Signals in the
Transmission of Less Critical
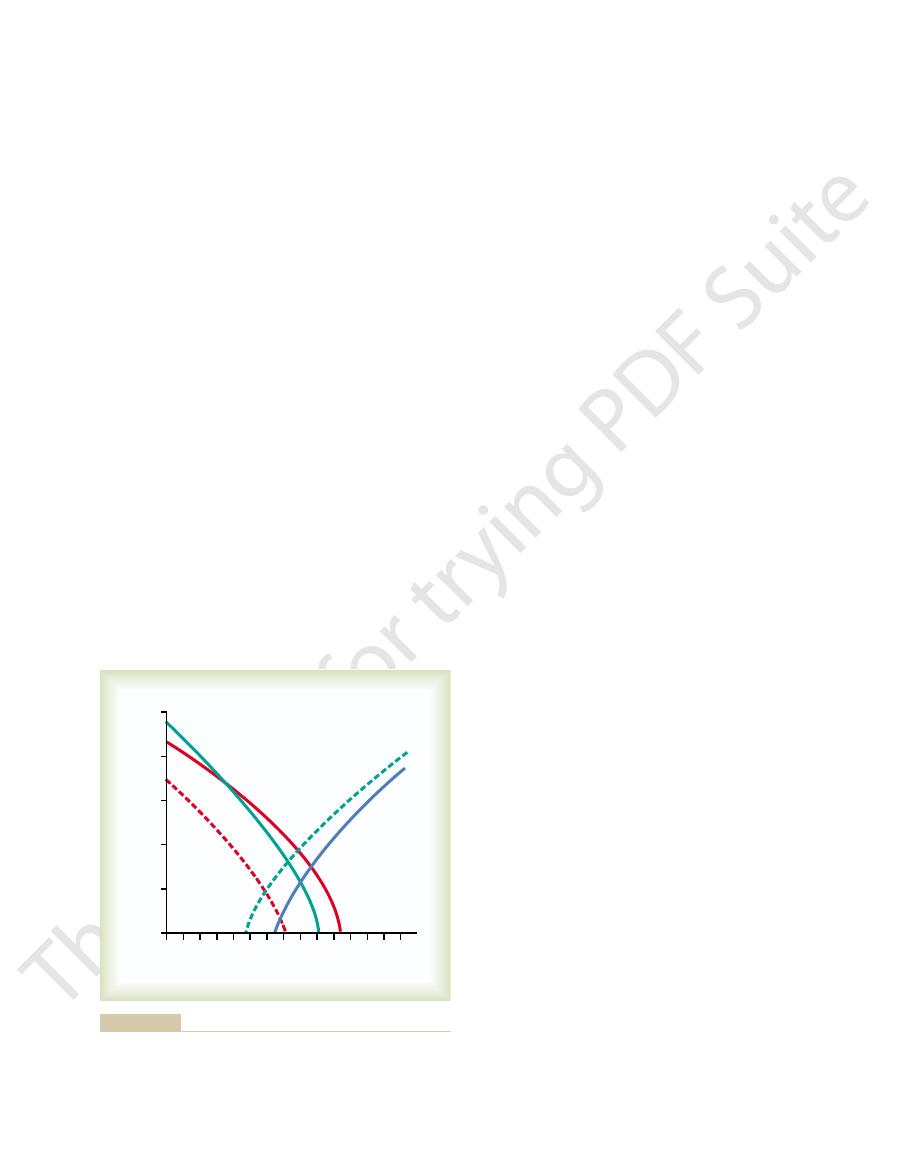
at minimal rotation. Thus, the signals from the indi-
to joint rotation are of two categories: (1) those
47–12, one sees that
Referring to Figure
Column–Medial Lemniscal Pathway.
especially adapted for detecting rapid rates of change.
The pacinian corpuscles and muscle spindles are
Golgi tendon receptors found in muscle tendons.
puscles, Ruffini’s endings, and receptors similar to the
tional important factor in determining position. Types
At the extremes of joint angulation, stretch of the
column system for deciphering joint angulations.
loosened, and the net stretch information from the
in Chapter 54. When the angle of a joint is changing,
in helping to control muscle movement, as we shall see
. They are also exceedingly important
motion, among the most important receptors are the
For determining joint angulation in mid ranges of
Conversely, for most of the larger joints of the body,
believed to be detected through the skin receptors.
abundance, as much as half of position recognition is
case of the fingers, where skin receptors are in great
and deep receptors near the joints are used. In the
together for position sense. Both skin tactile receptors
Somatic Sensations: I. General Organization, the Tactile and Position Senses
Chapter 47
595
deep receptors are more important.
muscle spindles
some muscles are being stretched while others are
spindles is transmitted into the computational system
of the spinal cord and higher regions of the dorsal
ligaments and deep tissues around the joints is an addi-
of sensory endings used for this are the pacinian cor-
It is likely that these are the receptors most responsi-
ble for detecting rate of movement.
Processing of Position Sense Information in the Dorsal
thalamic neurons responding
maximally stimulated when the joint is at full rotation
and (2) those maximally stimulated when the joint is
vidual joint receptors are used to tell the psyche how
much each joint is rotated.
signals that do not require highly discrete localization
of the signal source and do not require discrimination
Anatomy of the
Anterolateral Pathway
originate mainly in
sensory nerve fibers terminate after entering the cord.
cross immediately in the anterior commissure of the
cord to the opposite anterior and lateral white columns,
where they turn upward toward the brain by way of the
anterior spinothalamic and lateral spinothalamic tracts.
reticular nuclei of the
brain stem and (2) in two different nuclear complexes
ventrobasal complex and the
intralaminar nuclei
minating in some of the same thalamic nuclei where the
signals are transmitted to the somatosensory cortex
project directly to the ventrobasal complex of the thal-
ular nuclei of the brain stem and from there are relayed
to the intralaminar nuclei of the thalamus where the
greater detail in Chapter 48.
in the anterolateral pathway as in the dorsal
are only one third to one half those in the dorsal
many as 100 gradations for the dorsal column system;
0
60
80
100
120
140
160
180
Degrees
Impulses per second
0
20
40
60
80
100
#1
#2
#3
#4
#5
varied over an intensive continuum. J Neurophysiol 26:807, 1963.)
G: The relation of thalamic cell response to peripheral stimuli
its range of motion. (Data from Mountcastle VB, Poggie GF, Werner
mic ventrobasal complex when the knee joint is moved through
Typical responses of five different thalamic neurons in the thala-
Figure 47–12

late developments.
netic development of animals, whereas the critical
crimination of these sensibilities. It is interesting that
lower brain stem, the thalamus, and other associated
Therefore, there is much reason to believe that the
a moderate effect on the perception of temperature.
effect on one’s perception of pain sensation and only
Conversely, loss of the somatosensory cortex has little
to discriminate tactile sensation, even though the thala-
does return. Therefore, it must be assumed that the thal-
bilities, but a slight degree of crude tactile sensibility
destroyed, that person loses most critical tactile sensi-
When the somatosensory cortex of a human being is
Function of the Thalamus
Somatosensory Function
pressure.
and sexual sensations, in addition to crude touch and
niscal system. They are pain, temperature, tickle, itch,
column–medial lemniscal system. Even so, certain
Thus, it is evident that the anterolateral system is a
rapidly repetitive signals is poor.
The Nervous System: A. General Principles and Sensory Physiology
596
Unit IX
and (4) the ability to transmit rapidly changing or
cruder type of transmission system than the dorsal
modalities of sensation are transmitted only in this
system and not at all in the dorsal column–medial lem-
Some Special Aspects of
in Somatic Sensation
amus (as well as other lower centers) has a slight ability
mus normally functions mainly to relay this type of
information to the cortex.
basal regions of the brain play dominant roles in dis-
these sensibilities appeared very early in the phyloge-
tactile sensibilities and the somatosensory cortex were
Medulla oblongata
Medial lemniscus
Mesencephalon
Internal
capsule
Cortex
Spinal cord
Dorsal root and spinal
ganglion
Ventrobasal
and intralaminar
nuclei of the
thalamus
Lateral
division of the
anterolateral
pathway
Anterior
division of the
anterolateral
pathway
Anterior and lateral divisions of the anterolateral sensory pathway.
Figure 47–13
C2
T2
T2
T3
T5
T7
T9
T10
T11
T12
L1
S3
S2
S4&5
S2
L5
L3
L1
L2
L3
L4
L5
S1
C2
C3
C4
C5
T4
T5
T4
T2
T5
T6
T7
T8
T9
T10
T12
T11
L2
L3
L4
L5
L5
L4
S1
C6
C7
C8
T4
T6
T8
C3
C4
C5
C Thomas, Publisher, Ltd., Springfield, Illinois.)
ed. Springfield, IL: Charles C Thomas, 1966. Courtesy of Charles
Dermatomes. (Modified from Grinker RR, Sahs AL: Neurology, 6th
Figure 47–14
human brain. Ann N Y Acad Sci 999:364, 2003.
Thaut MH: Neural basis of rhythmic timing networks in the
plasticity in the auditory system. Nat Rev Neurosci 4:783,
Suga N, Ma X: Multiparametric corticofugal modulation and
Curr Opin Neurobiol 13:663, 2003.
Sommer MA: The role of the thalamus in motor control.
sentations. Nat Rev Neurosci 3:741, 2002.
Pouget A, Deneve S, Duhamel JR: A computational per-
lular and systems physiology. Pflugers Arch 447:126, 2003.
Petersen CC: The barrel cortex—integrating molecular, cel-
touch are constant companions. Curr Biol 14:R349, 2004.
Pears S, Jackson SR: Cognitive neuroscience: vision and
Biol 13:R531, 2003.
and the body schema: close to hand and within reach. Curr
Maravita A, Spence C, Driver J: Multisensory integration
Physiol Sci 19:22, 2004.
tinguishes between escapable and inescapable pain. News
Lumb BM: Hypothalamic and midbrain circuitry that dis-
Science, 4th ed. New York: McGraw-Hill, 2000.
Kandel ER, Schwartz JH, Jessell TM: Principles of Neural
mechanoreceptors. Curr Opin Neurobiol 11:455, 2001.
Johnson KO: The roles and functions of cutaneous
Behav Brain Res 142:1, 2003.
Jeannerod M: The mechanism of self-recognition in humans.
explained? Lancet Neurol 2:687, 2003.
Janig W, Baron R: Complex regional pain syndrome: mystery
Curr Opin Neurobiol 14:225, 2004.
Ivry RB, Spencer RM: The neural representation of time.
Churchill Livingstone, 2003.
Haines DE, Lancon JA: Review of Neuroscience. New York:
Churchill Livingstone, 1997.
Haines DE: Fundamental Neuroscience. New York:
14:89, 2004.
plasticity in somatosensory cortex. Curr Opin Neurobiol
Foeller E, Feldman DE: Synaptic basis for developmental
gence in central processing.Annu Rev Neurosci 26:1, 2003.
Craig AD: Pain mechanisms: labeled lines versus conver-
Neurosci 3:553, 2002.
movement plans in the posterior parietal cortex. Nat Rev
Cohen YE, Andersen RA: A common reference frame for
tion following injury. Neuroscience 111(4):761, 2002.
Chen R, Cohen LG, Hallett M: Nervous system reorganiza-
lar perspective. Physiol Rev 81:539, 2001.
Bosco G, Poppele RE: Proprioception from a spinocerebel-
disturbed by the injury.
can use a dermatomal map as shown in Figure 47–14 to
ments, which is evident from the dermatomal map. One
ments (L2 to S3), rather than from the distal sacral seg-
most distal portion of the body. The legs originate
matome S5. In the embryo, this is the tail region and the
in the dermatome of the most distal cord segment, der-
The figure shows that the anal region of the body lies
matomes, which is far from true because much overlap
shown in Figure 47–14. They are shown in the figure as
. The different dermatomes are
Each spinal nerve innervates a “segmental field” of the
chapters.
only the somatic system, as explained in subsequent
gal sensory control is used by all sensory systems, not
ferentiate sensory patterns. This principle of corticofu-
sharpness in the signal pattern. Second, it keeps the
cent neurons and, therefore, increases the degree of
in the relay nuclei. This does two things: First, it
that when sensory input intensity becomes too great, the
Corticofugal signals are almost entirely inhibitory, so
mus, medulla, and spinal cord; they control the intensity
Signals
Somatic Sensations: I. General Organization, the Tactile and Position Senses
Chapter 47
597
Cortical Control of Sensory
Sensitivity—“Corticofugal”
In addition to somatosensory signals transmitted from
the periphery to the brain, corticofugal signals are trans-
mitted in the backward direction from the cerebral
cortex to the lower sensory relay stations of the thala-
of sensitivity of the sensory input.
corticofugal signals automatically decrease transmission
decreases lateral spread of the sensory signals into adja-
sensory system operating in a range of sensitivity that is
not so low that the signals are ineffectual nor so high
that the system is swamped beyond its capacity to dif-
Segmental Fields of Sensation—
The Dermatomes
skin called a dermatome
if there were distinct borders between the adjacent der-
exists from segment to segment.
embryologically from the lumbar and upper sacral seg-
determine the level in the spinal cord at which a cord
injury has occurred when the peripheral sensations are
References
spective on the neural basis of multisensory spatial repre-
2003.

type of pain in most of these areas.
other deep tissues are only sparsely supplied with pain endings; nevertheless,
in the cranial vault. Most
joint surfaces,
rial walls,
as well as in certain internal tissues, such as the
tissues are all free nerve endings. They are widespread in the superficial layers
The pain receptors in the skin and other
Pain Receptors Are Free Nerve Endings.
ing. It can occur both in the skin and in almost any deep tissue or organ.
It can lead to prolonged, unbearable suffer-
This type of pain is usually
chronic pain.
throbbing pain, nauseous pain,
slow burning pain, aching pain,
Slow pain also goes by many names, such as
pain is not felt in most deeper tissues of the body.
burned. It is also felt when the skin is subjected to electric shock. Fast-sharp
is stuck into the skin, when the skin is cut with a knife, or when the skin is acutely
This type of pain is felt when a needle
pricking pain, acute pain,
Fast pain is also described by many alternative names, such as
each of them has specific qualities.
and sometimes even minutes. During the course of this chapter, we shall see
is felt within about 0.1 second after a pain stimulus is applied, whereas slow pain
Fast pain
slow pain.
Types of Pain and Their Qualities—Fast Pain
skin at the areas of pressure.
fore, fails to shift. This soon results in total breakdown and desquamation of the
has lost the pain sense, as after spinal cord injury, fails to feel the pain and, there-
ischemia, the person normally shifts weight subconsciously. But a person who
the weight of the body. When the skin becomes painful as a result of the
damaged, and it causes the individual to react to remove the pain stimulus. Even
these reasons, the first part of this chapter is devoted
knowledge of the different qualities of pain. For
eases depends to a great extent on a physician’s
Furthermore, the ability to diagnose different dis-
Many, if not most, ailments of the body cause pain.
Thermal Sensations
II. Pain, Headache, and
C
H
A
P
T
E
R
4
8
598
Somatic Sensations:
mainly to pain and to the physiologic bases of some
associated clinical phenomena.
Pain Is a Protective Mechanism.
Pain occurs whenever any tissues are being
such simple activities as sitting for a long time on the ischia can cause tissue
destruction because of lack of blood flow to the skin where it is compressed by
and Slow Pain
Pain has been classified into two major types: fast pain and
begins only after 1 second or more and then increases slowly over many seconds
that the conduction pathways for these two types of pain are different and that
sharp pain,
and electric pain.
and
associated with tissue destruction.
Pain Receptors and Their Stimulation
of the skin
periosteum, the arte-
the
and the falx and tentorium
any widespread tissue damage can summate to cause the slow-chronic-aching
release of chemical pain-inducing substances.
ischemia even greater, creating ideal conditions for the
olism in the muscle tissue, thus making the relative
ischemia. Also, the spasm increases the rate of metab-
stimulating mechanosensitive pain receptors, but it
clinical pain syndromes. This pain probably results
a common cause of pain, and it is the basis of many
stimulate the pain nerve endings.
of cell damage and that these, in addition to lactic acid,
proteolytic enzymes, are formed in the tissues because
ble that other chemical agents, such as bradykinin and
olism (metabolism without oxygen). It is also proba-
tissues, formed as a consequence of anaerobic metab-
remains zero.
absence of muscle exercise, the pain may not appear
can cause muscle pain within 15 to 20 seconds. In the
ceases, exercise of the forearm muscles sometimes
For instance, if a blood pressure cuff is placed around
lism of the tissue, the more rapidly the pain appears.
within a few minutes. The greater the rate of metabo-
tissue is blocked, the tissue often becomes very painful
When blood flow to a
Tissue Ischemia as a Cause of Pain.
permeable to ions.
causing pain following tissue damage. Also, the inten-
pain receptors can be found in these extracts. One
pain when injected beneath the normal skin. Most of
Special Importance of Chemical Pain Stimuli During Tissue
tusion, and so forth.
such as bacterial infection, tissue ischemia, tissue con-
The intensity of pain is also closely correlated with
rate at which damage to the tissues is occur-
level indefinitely. Therefore, it is immediately apparent
to be damaged by heat; indeed, the tissues are even-
This is also the temperature at which the tissues begin
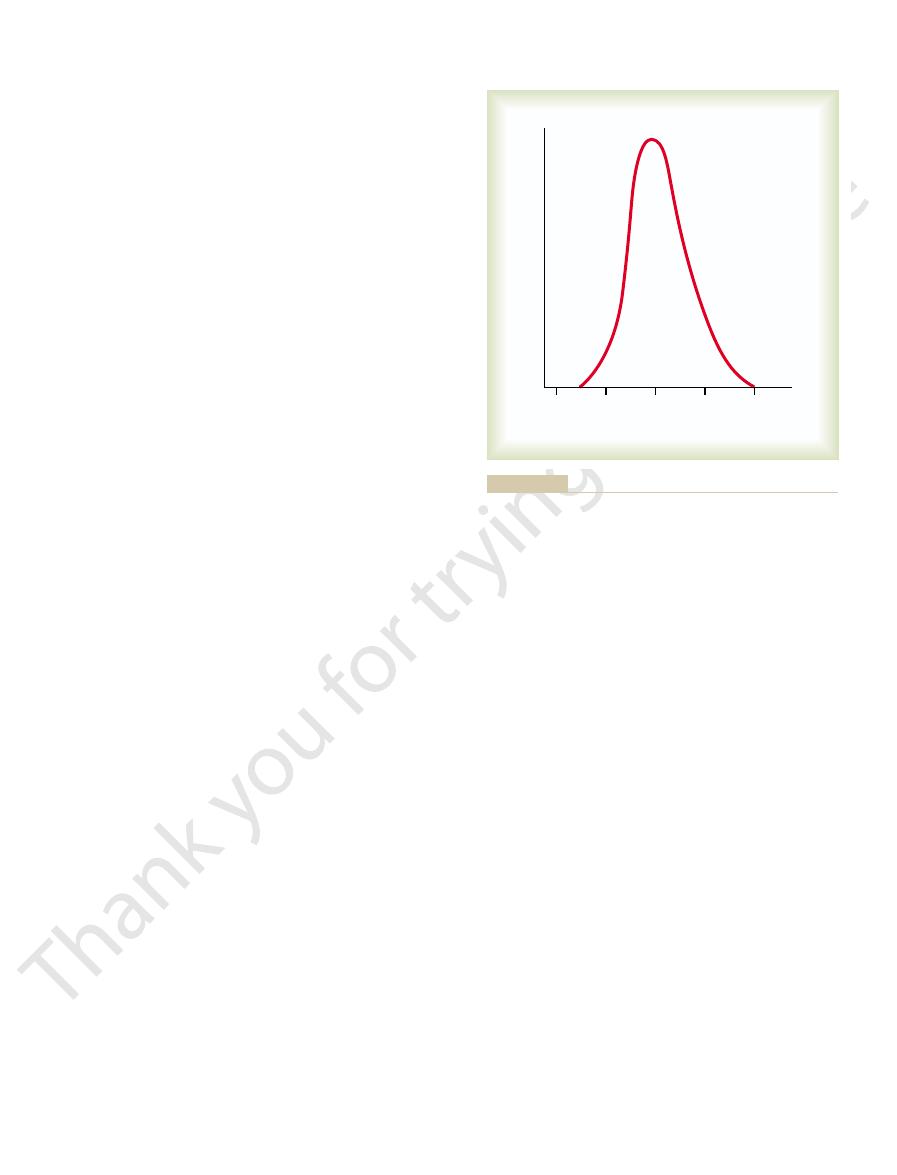
skin is heated above 45°C, as shown in Figure 48–1.
The average person begins to perceive pain when the
Rate of Tissue Damage as a Stimulus
persists.
adapt, because it allows the pain to keep the person
continues. This increase in sensitivity of the pain recep-
slow-aching-nauseous pain, as the pain stimulus
becomes progressively greater, especially so for
under some conditions, excitation of pain fibers
adapt very little and sometimes not at all. In fact,
other sensory receptors of the body, pain receptors
occurs after tissue injury.
tant in stimulating the slow, suffering type of pain that
them. The chemical substances are especially impor-
proteolytic enzymes.
ions, acids, acetylcholine,
bradykinin, serotonin, histamine, potassium
types.
stimuli, whereas slow pain can be elicited by all three
In general, fast pain
chemical pain stimuli.
mechanical,
types of stimuli. They are classified as
Three Types of Stimuli Excite Pain Receptors—Mechanical,
Somatic Sensations: II. Pain, Headache, and Thermal Sensations
Chapter 48
599
Thermal, and Chemical.
Pain can be elicited by multiple
thermal, and
is elicited by the mechanical and thermal types of
Some of the chemicals that excite the chemical type
of pain are
and
In
addition, prostaglandins and substance P enhance the
sensitivity of pain endings but do not directly excite
Nonadapting Nature of Pain Receptors.
In contrast to most
tors is called hyperalgesia. One can readily understand
the importance of this failure of pain receptors to
apprised of a tissue-damaging stimulus as long as it
for Pain
tually destroyed if the temperature remains above this
that pain resulting from heat is closely correlated
with the
ring and not with the total damage that has already
occurred.
the rate of tissue damage from causes other than heat,
Damage.
Extracts from damaged tissue cause intense
the chemicals listed earlier that excite the chemical
chemical that seems to be more painful than others is
bradykinin. Many researchers have suggested that
bradykinin might be the agent most responsible for
sity of the pain felt correlates with the local increase
in potassium ion concentration or the increase in pro-
teolytic enzymes that directly attack the nerve endings
and excite pain by making the nerve membranes more
the upper arm and inflated until the arterial blood flow
for 3 to 4 minutes even though the muscle blood flow
One of the suggested causes of pain during ischemia
is accumulation of large amounts of lactic acid in the
Muscle Spasm as a Cause of Pain.
Muscle spasm is also
partially from the direct effect of muscle spasm in
might also result from the indirect effect of muscle
spasm to compress the blood vessels and cause
43
44
45
46
47
Temperature (
∞
C)
Number of subjects
ified from Hardy DJ: Nature of pain. J Clin Epidemiol 4:22, 1956.)
showing the minimal skin temperature that will cause pain. (Mod-
Distribution curve obtained from a large number of persons
Figure 48–1
for tactile sensations, as was discussed in Chapter 47.
interruption, terminating in the
stem, but most pass all the way to the thalamus without
Termination of the Neospinothalamic Tract in the Brain
columns.
turn upward, passing to the brain in the anterolateral
the neospinothalamic tract. These give rise to long
Figure 48–2, and there excite second-order neurons of
(lamina marginalis) of the dorsal horns, as shown in
thermal pain. They terminate mainly in lamina I
The fast type A
Neospinothalamic Tract for Fast Pain.
pathways to the brain, through (1) the
On entering the spinal cord, the pain signals take two
Paleospinothalamic Tract
Neospinothalamic Tract and the
as shown in Figures 48–2 and 48–3.
dorsal horns. Here again, there are two systems for
roots, the pain fibers terminate on relay neurons in the
pain tends to become greater over time. This sensation
remove himself or herself from the stimulus. The slow
a damaging influence and, therefore, plays an impor-
pathway. The sharp pain apprises the person rapidly of
fiber pathway, followed a second or so
brain by the A
sensation: a fast-sharp pain that is transmitted to the
a sudden painful stimulus often gives a “double” pain
C fibers at velocities between 0.5 and 2 m/sec.
persisting mechanical or thermal stimuli. This slow-
fibers at velocities between 6 and 30 m/sec. Conversely,
peripheral nerves to the spinal cord by small type A
or thermal pain stimuli; they are transmitted in the
The fast-
pain pathway.
slow-chronic
fast-sharp pain pathway
ting pain signals into the central nervous system. The
Even though all pain receptors are free nerve endings,
Nervous System
Transmission of Pain
The Nervous System: A. General Principles and Sensory Physiology
600
Unit IX
Dual Pathways for
Signals into the Central
these endings use two separate pathways for transmit-
two pathways mainly correspond to the two types of
pain—a
and a
Peripheral Pain Fibers—“Fast” and “Slow” Fibers.
sharp pain signals are elicited by either mechanical
d
the slow-chronic type of pain is elicited mostly by
chemical types of pain stimuli but sometimes by
chronic pain is transmitted to the spinal cord by type
Because of this double system of pain innervation,
d
later by a slow pain that is transmitted by the C fiber
tant role in making the person react immediately to
eventually produces the intolerable suffering of long-
continued pain and makes the person keep trying to
relieve the cause of the pain.
On entering the spinal cord from the dorsal spinal
processing the pain signals on their way to the brain,
Dual Pain Pathways in the
Cord and Brain Stem—The
neospinothala-
mic tract and (2) the paleospinothalamic tract.
d
pain fibers transmit mainly mechanical and acute
fibers that cross immediately to the opposite side of
the cord through the anterior commissure and then
Stem and Thalamus.
A few fibers of the neospinothal-
amic tract terminate in the reticular areas of the brain
ventrobasal complex
along with the dorsal column–medial lemniscal tract
A few fibers also terminate in the posterior nuclear
Fast-sharp
pain fibers
Spinal
nerve
C A
d
Slow-chronic
pain fibers
Anterolateral
pathway
IX VIII
VII
VI
V
IV
III
II
I
Substantia
gelatinosa
Lamina
marginalis
Tract of
Lissauer
into and through the spinal cord on their way to the brain.
Transmission of both “fast-sharp” and “slow-chronic” pain signals
Figure 48–2
To: Somatosensory areas
Ventrobasal
complex and
posterior
nuclear
group
"Fast" Pain
Fibers
"Slow" Pain
Fibers
Thalamus
Reticular
formation
Intralaminar
nuclei
Pain tracts
slow burning pain pathway.
cerebral cortex by way of the
Transmission of pain signals into the brain stem, thalamus, and
Figure 48–3
fast pricking pain pathway and the
he or she is in severe pain.
system,” which is discussed in Chapter 59.This explains
areas constitute part of the brain’s principal “arousal
activity throughout the entire brain. In fact, these two
pain terminates, has a strong arousal effect on nervous
, the areas where the slow-suffering type of
Excitability.
centers.
role in interpreting pain quality, even though pain per-
3 per cent of the points stimulated. However, it is
nothing to do with normal pain appreciation; electri-
pain. This does not mean that the cerebral cortex has
stem reticular formation, the thalamus, and other
fore, it is likely that pain impulses entering the brain
not destroy an animal’s ability to perceive pain. There-
nectivity of this pathway. It explains why patients often
This is in keeping with the multisynaptic, diffuse con-
arm or leg but not to a specific point on the arm or leg.
ized only to a major part of the body, such as to one
For instance, slow-chronic pain can usually be local-
ted by way of the paleospinothalamic pathway is poor.
Slow-Chronic Pathway.
ize Precisely the Source of Pain Transmitted in the
Very Poor Capability of the Nervous System to Local-
matized. From the brain stem pain areas, multiple
of Sylvius. These lower regions of the brain appear to
periaqueductal gray region
deep to the superior and inferior colliculi; or (3) the
cephalon; (2) the
of the medulla, pons, and mesen-
mus. Instead, most terminate in one of three areas: (1)
shaded area shown in Figure 48–3. Only one tenth to
terminates widely in the brain stem, in the large
The slow-chronic paleospinothalamic pathway
Chronic Pain Signals) into the Brain Stem and Thala-
Projection of the Paleospinothalamic Pathway (Slow-
nervous system, and substance P is concerned with
tion. Regardless of the yet unknown details, it seems
transmitter gives a faster pain sensation, whereas the
“double” pain sensation one feels after a pinprick
even minutes. In fact, it has been suggested that the
onds. Substance P is released much more slowly, build-
substance P transmitter. The glutamate transmitter
mitter of Type C Nerve Endings.
Substance P, the Probable Slow-Chronic Neurotrans-
eral pathway.
of the cord, then upward to the brain in the anterolat-
join the fibers from the fast pain pathway, passing first
mainly lamina V, also in the dorsal horn. Here the last
fiber in Figure 48–2. Most of the signals then pass
horns, which together are called the
pathway, the peripheral fibers terminate in the spinal
fibers as well. In this
mit some signals from type A
slow-chronic type C pain fibers, although it does trans-
The paleospinothalamic pathway is a much older
Paleospinothalamic Pathway for Transmitting Slow-Chronic
action lasting for only a few milliseconds.
central nervous system, usually having a duration of
pain nerve fiber endings. This is one of
at the type A
Glutamate, the Probable Neurotransmitter of the Type
are simultaneously stimulated, the localization can be
or so of the stimulated area. Yet when tactile receptors
be poorly localized, often only within 10 centimeters
ous stimulation of tactile receptors, even fast pain may
pain receptors are stimulated, without the simultane-
body than can slow-chronic pain. However, when only
The fast-sharp type of pain can be local-
in the Body.
Capability of the Nervous System to Localize Fast Pain
group of the thalamus. From these thalamic areas, the
Somatic Sensations: II. Pain, Headache, and Thermal Sensations
Chapter 48
601
signals are transmitted to other basal areas of the brain
as well as to the somatosensory cortex.
ized much more exactly in the different parts of the
that excite the dorsal column–medial lemniscal system
nearly exact.
A
d
Fast Pain Fibers.
It is believed that glutamate is the
neurotransmitter substance secreted in the spinal cord
d
the most widely used excitatory transmitters in the
Pain.
system and transmits pain mainly from the peripheral
d
cord almost entirely in laminae II and III of the dorsal
substantia gelati-
nosa, as shown by the lateral most dorsal root type C
through one or more additional short fiber neurons
within the dorsal horns themselves before entering
neurons in the series give rise to long axons that mostly
through the anterior commissure to the opposite side
Research experi-
ments suggest that type C pain fiber terminals entering
the spinal cord secrete both glutamate transmitter and
acts instantaneously and lasts for only a few millisec-
ing up in concentration over a period of seconds or
might result partly from the fact that the glutamate
substance P transmitter gives a more lagging sensa-
clear that glutamate is the neurotransmitter most
involved in transmitting fast pain into the central
slow-chronic pain.
mus.
one fourth of the fibers pass all the way to the thala-
the reticular nuclei
tectal area of the mesencephalon
surrounding the aqueduct
be important for feeling the suffering types of pain,
because animals whose brains have been sectioned
above the mesencephalon to block pain signals from
reaching the cerebrum still evince undeniable evi-
dence of suffering when any part of the body is trau-
short-fiber neurons relay the pain signals upward into
the intralaminar and ventrolateral nuclei of the thala-
mus and into certain portions of the hypothalamus and
other basal regions of the brain.
Localization of pain transmit-
have serious difficulty in localizing the source of some
chronic types of pain.
Function of the Reticular Formation, Thalamus, and Cerebral
Cortex in the Appreciation of Pain.
Complete removal of
the somatic sensory areas of the cerebral cortex does
lower brain centers cause conscious perception of
cal stimulation of cortical somatosensory areas does
cause a human being to perceive mild pain from about
believed that the cortex plays an especially important
ception might be principally the function of lower
Special Capability of Pain Signals to Arouse Overall Brain
Electrical stimulation in the reticular areas
of the brain stem and in the intralaminar nuclei of the
thalamus
why it is almost impossible for a person to sleep when
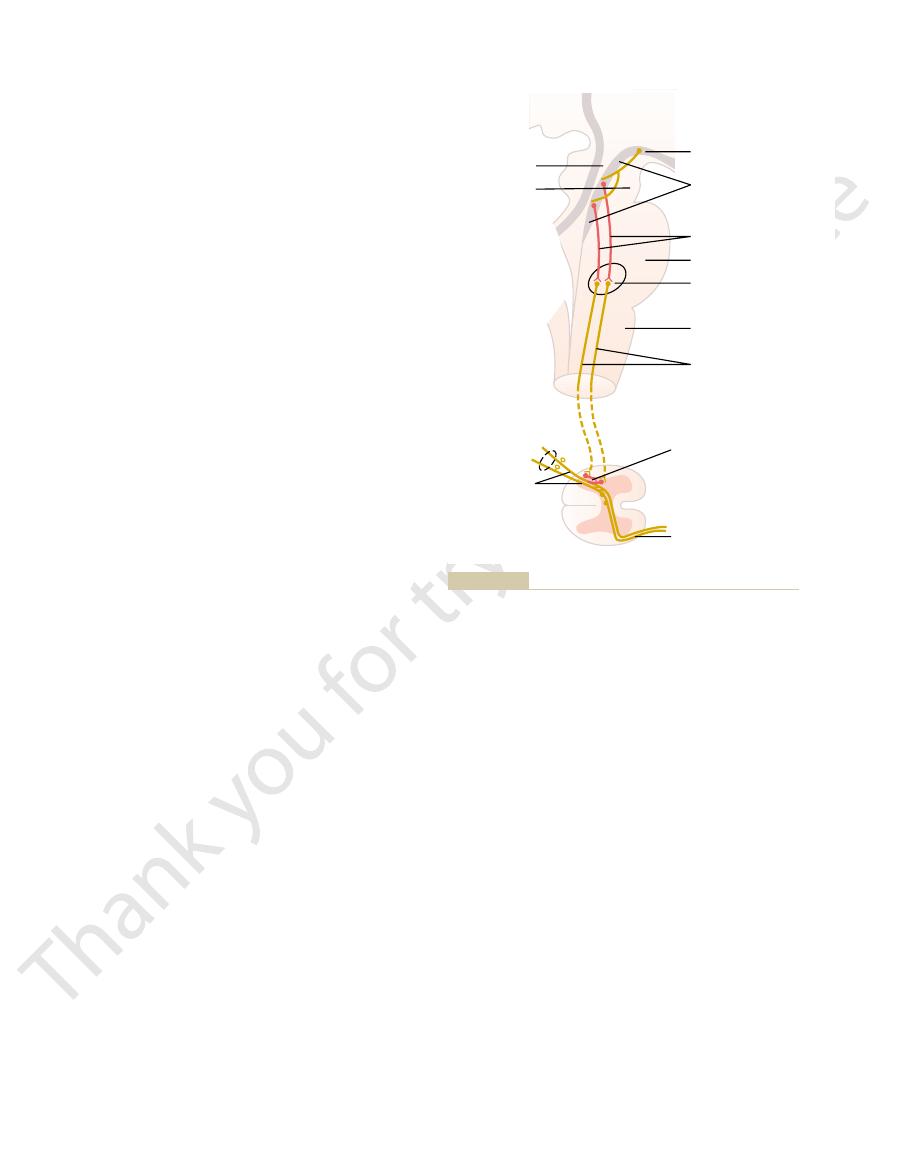
pain signals, especially withdrawal reflexes described
the initial entry point to the spinal cord. In fact, it can
Thus, the analgesia system can block pain signals at
where they synapse in the dorsal horns.
of incoming type C and type A
to secrete enkephalin as well. The enkephalin is
their endings. The serotonin causes local cord neurons
Fibers originating in this area send signals to the
shown in Figure 48–4, the endings of many fibers in
gray area secrete enkephalin at their endings. Thus, as
analgesia system; especially involved are
thalamus.
medial forebrain bundle,
extent, the
adjacent to the third ventricle, and (2) to a lesser
periventricular nuclei in the hypothalamus,
area can also suppress pain. Some of these areas are
spinal roots. Also, stimulation of areas at still higher
At this point, the
the dorsal horns of the spinal cord.
the medulla. From these nuclei, second-order signals
reticularis paragigantocellularis,
the lower pons and upper medulla, and the
magnus nucleus,
Sylvius and portions of the third and fourth ventricles.
ductal gray
consists of three major components: (1) The
The analgesia system is shown in Figure 48–4. It
tremendously. This results partly from a capability of
The degree to which a person reacts to pain varies
Brain and Spinal Cord
Pain Suppression
pain, an important protective mechanism.
pain while leaving intact one’s appreciation of “acute”
in the thalamus, which often relieves suffering types of
pathways in the dorsolateral cord). Another experi-
that normally are too weak to be effectual (e.g., sparse
later, partly as a result of sensitization of other pathways
fibers. Second, pain frequently returns several months
the brain, so that the cordotomy does not transect these
relieving pain, for two reasons. First, many pain fibers
A cordotomy, however, is not always successful in
to interrupt the anterolateral sensory pathway.
to a few months. To do this, the spinal cord on the side
cordotomy
part of the body, a
at any one of several points. If the pain is in the lower
pain. To do this, the pain nervous pathways can be cut
rapidly spreading cancer), it is necessary to relieve the
When a person has
The Nervous System: A. General Principles and Sensory Physiology
602
Unit IX
Surgical Interruption of Pain Pathways.
severe and intractable pain (sometimes resulting from
in the thoracic region of
the spinal cord often relieves the pain for a few weeks
opposite to the pain is partially cut in its anterolateral
quadrant
from the upper part of the body do not cross to the
opposite side of the spinal cord until they have reached
mental operative procedure to relieve pain has been to
cauterize specific pain areas in the intralaminar nuclei
(“Analgesia”) System in the
the brain itself to suppress input of pain signals to the
nervous system by activating a pain control system,
called an analgesia system.
periaque-
and periventricular areas of the mesen-
cephalon and upper pons surround the aqueduct of
Neurons from these areas send signals to (2) the raphe
a thin midline nucleus located in
nucleus
located laterally in
are transmitted down the dorsolateral columns in the
spinal cord to (3) a pain inhibitory complex located in
analgesia signals can block the pain before it is relayed
to the brain.
Electrical stimulation either in the periaqueductal
gray area or in the raphe magnus nucleus can suppress
many strong pain signals entering by way of the dorsal
levels of the brain that excite the periaqueductal gray
(1) the
lying
also in the hypo-
Several transmitter substances are involved in the
enkephalin
and serotonin. Many nerve fibers derived from the
periventricular nuclei and from the periaqueductal
the raphe magnus nucleus release enkephalin when
stimulated.
dorsal horns of the spinal cord to secrete serotonin at
believed to cause both presynaptic and postsynaptic
inhibition
d pain fibers
also block many local cord reflexes that result from
in Chapter 54.
Brain’s Opiate System—Endorphins
and Enkephalins
More than 35 years ago it was discovered that injec-
tion of minute quantities of morphine either into the
periventricular nucleus around the third ventricle or
Periventricular
nuclei
Periaqueductal gray
Mesencephalon
Enkephalin neurons
Pons
Raphe magnus
nucleus
Medulla
Serotonergic
neurons
Enkephalin
neurons
Anterolateral
somatosensory tract
Aqueduct
Fourth
ventricle
Third
ventricle
Pain fibers
Presynaptic
pain inhibition
both the cord and the brain stem.
that suppress pain signals in
enkephalin-secreting neurons
bition of incoming pain signals at the cord level and (2) presence
Analgesia system of the brain and spinal cord, showing (1) inhi-
Figure 48–4
of

causes pain that can be severe. For instance, ischemia
cant pain. Conversely, any stimulus that causes
pain. For instance, a surgeon can cut the gut entirely in
differs from surface pain in several important aspects.
modalities of sensation besides pain. Also, visceral pain
Often, the viscera have sensory receptors for no other
ceral infectious disease, and other visceral ailments.
can be used for diagnosing visceral inflammation, vis-
In clinical diagnosis, pain from the different viscera of
Visceral Pain
sensations originate in the skin itself.
from the skin, and the person has the feeling that the
skin. When the visceral pain fibers are stimulated, pain
figure, branches of visceral pain fibers are shown to
able mechanism by which most pain is referred. In the
Figure 48–5 shows the prob-
surface. Knowledge of the different types of referred
For instance, pain in one of the
fairly remote from the tissue causing the pain. This is
Referred Pain
been reported in some instances. Also, pain relief has
control the degree of stimulation. Dramatic relief has
the diencephalon. The patient can then personally
In some patients, electrodes have been placed stereo-
to stimulate the dorsal sensory columns.
on occasion, implanted over the spinal cord, supposedly
electrodes are placed on selected areas of the skin or,
suppressing pain by electrical stimulation. Stimulating
Treatment of Pain by Electrical
acupuncture.
This mechanism and the simultaneous psychogenic
iments are often useful for pain relief.
in relieving pain. And it probably also explains why lin-
the spinal cord. It explains why such simple maneuvers
This presumably results from local lateral inhibition in
the discovery that stimulation of large type A
by Simultaneous Tactile
Inhibition of Pain Transmission
peripheral nerves.
by morphine-like drugs, can almost totally
pathways
gray and periventricular areas, or
Thus, although the fine details of the brain’s opiate
but in much lower quantities.
is found mainly in the same areas as the enkephalins,
the hypothalamus and the pituitary gland. Dynorphin
described earlier, and
and spinal cord, in the portions of the analgesia system
The two enkephalins are found in the brain stem
-endorphin, met-enkephalin, leu-
opiomelanocortin, proenkephalin,
ent points of the nervous system; all are breakdown
for the natural opiate of the brain. About a dozen such
brain. Therefore, an extensive search was undertaken
assumed that the “morphine receptors” of the analge-
of neurons do so by acting on synaptic receptors, it was
spinal cord. Because most drugs that alter excitability
analgesia system, including the dorsal horns of the
mainly the opiates, also act at many other points in the
studies, it has been found that morphine-like agents,
causes an extreme degree of analgesia. In subsequent
Somatic Sensations: II. Pain, Headache, and Thermal Sensations
Chapter 48
603
into the periaqueductal gray area of the brain stem
sia system must be receptors for some morphine-like
neurotransmitter that is naturally secreted in the
opiate-like substances have now been found at differ-
products of three large protein molecules: pro-
and prodynorphin.
Among the more important of these opiate-like
substances are
b
enkephalin, and dynorphin.
b-endorphin is present in both
system are not understood, activation of the analgesia
system by nervous signals entering the periaqueductal
inactivation of pain
suppress many pain signals entering through the
Sensory Signals
Another important event in the saga of pain control was
b sensory
fibers from peripheral tactile receptors can depress
transmission of pain signals from the same body area.
as rubbing the skin near painful areas is often effective
excitation of the central analgesia system are probably
also the basis of pain relief by
Stimulation
Several clinical procedures have been developed for
taxically in appropriate intralaminar nuclei of the thal-
amus or in the periventricular or periaqueductal area of
been reported to last for as long as 24 hours after only
a few minutes of stimulation.
Often a person feels pain in a part of the body that is
called referred pain.
visceral organs often is referred to an area on the body
pain is important in clinical diagnosis because in many
visceral ailments the only clinical sign is referred pain.
Mechanism of Referred Pain.
synapse in the spinal cord on the same second-order
neurons (1 and 2) that receive pain signals from the
signals from the viscera are conducted through at least
some of the same neurons that conduct pain signals
the abdomen and chest is one of the few criteria that
One of the most important differences between
surface pain and visceral pain is that highly localized
types of damage to the viscera seldom cause severe
two in a patient who is awake without causing signifi-
diffuse
stimulation of pain nerve endings throughout a viscus
Skin nerve
fibers
Visceral
nerve fibers
1
2
Mechanism of referred pain and referred hyperalgesia.
Figure 48–5
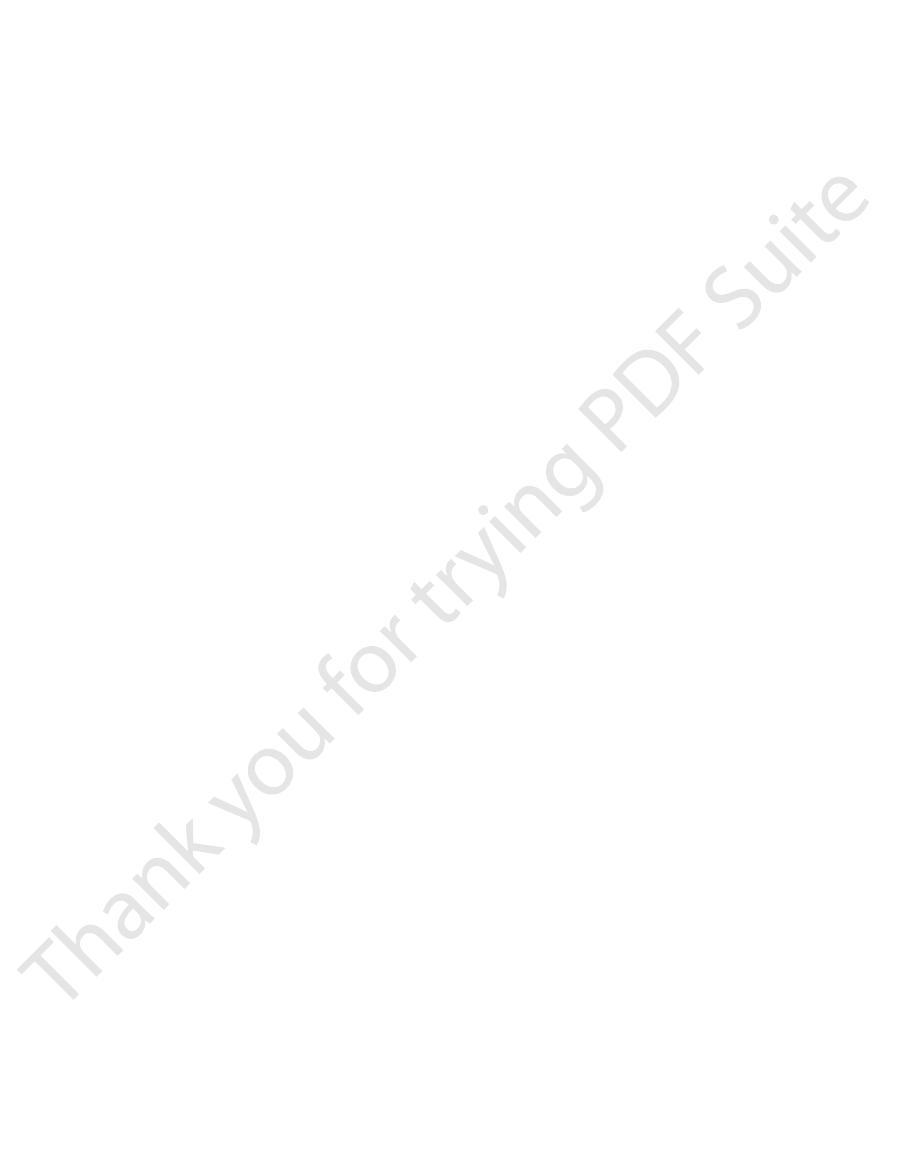
Parietal Pathway for Transmission of Abdominal and Thoracic
organs, representing in general the areas in the embryo
racic segments. Figure 48–6 shows several other surface
gastrium above the umbilicus, which is the surface area
Therefore, stomach pain is referred to the anterior epi-
seventh to ninth thoracic segments of the embryo.
The stomach originated approximately from the
quently, the pain is on the left side rather than on the
nerve fibers into the C-3 to T-5 cord segments. Most fre-
sternal area of the upper chest. These are the areas of
the pectoral muscles, down the arm, and into the sub-
referred to the side of the neck, over the shoulder, over
fore, as shown in Figure 48–6, pain from the heart is
the spinal cord between segments C-3 and T-5. There-
upper thorax, so that the heart’s visceral pain fibers pass
lies. For instance, the heart originated in the neck and
embryo, not necessarily where the visceral organ now
When visceral pain is referred to the surface of the body,
Localization of Referred Pain Transmitted via Visceral Pathways.
directly over the painful area.
localized
cardium, and these sensations are usually
nerves from the parietal peritoneum, pleura, or peri-
often far from the painful organ. Conversely, parietal
sensory fibers within the autonomic nerve bundles, and
True visceral pain is transmitted via pain
etal pathway.
true visceral pathway
Second, sensations from the abdomen and thorax are
originates internally can be localized only generally.
different internal organs exist; therefore, any pain that
localize, for a number of reasons. First, the patient’s
Transmission Pathways
Pain
and the
Visceral
Localization of Visceral Pain
wall is not very painful, if painful at all.
peritoneum is very painful, whereas a similar
pain and true visceral pain: a knife incision through the
etal wall overlying a viscus is frequently sharp. An
peripheral spinal nerves. Therefore, pain from the pari-
pericardium. These parietal surfaces, like the skin, are
often spreads to the parietal peritoneum, pleura, or
When a disease affects a viscus, the disease process
Visceral Disease
Caused by
bronchi
sitive, both the
to pain. In the lungs, even though the alveoli are insen-
trauma and stretch, and the
parenchyma of the liver and the alveoli of the lungs. Yet
pletely insensitive to pain of any type. These include the
encircle the viscus or that pass into its wall, thus perhaps
because of overstretch of the tissues themselves.
hollow viscus also can result in pain, presumably
turition, gallbladder disease, or ureteral obstruction.
dicitis, gastroenteritis, constipation, menstruation, par-
The cramping type of pain frequently occurs in appen-
along an overly excitable spastic gut, a cramp occurs.
muscle. For instance, each time a peristaltic wave travels
cycles result from periods of contraction of smooth
intermittently, once every few minutes. The intermittent
severity and then subsiding. This process continues
cramps,
muscle’s increased metabolic need for nutrients, thus
diminished blood flow to the muscle, combined with the
tion of the pain nerve endings. Or the spasm might cause
viscus can cause pain, possibly by mechanical stimula-
the gallbladder, a bile duct, a ureter, or any other hollow
usually excruciatingly severe.
thus stimulating broad areas of pain fibers. The pain is
through a ruptured gastric or duodenal ulcer. This juice
For instance, proteolytic acidic gastric juice often leaks
from the gastrointestinal tract into the peritoneal cavity.
On occasion, damaging substances leak
enzymes, or others that stimulate pain nerve endings.
degenerative products such as bradykinin, proteolytic
that it does in other tissues, presumably because of the
mitted through small type C pain fibers and, therefore,
within the viscus. Essentially all visceral pain that orig-
of a hollow viscus, excess distention of a hollow viscus,
the surfaces of the viscera, spasm of the smooth muscle
include ischemia of visceral tissue, chemical damage to
areas of the viscera can cause visceral pain. Such stimuli
Causes of True Visceral Pain
The Nervous System: A. General Principles and Sensory Physiology
604
Unit IX
caused by occluding the blood supply to a large area of
gut stimulates many diffuse pain fibers at the same time
and can result in extreme pain.
Any stimulus that excites pain nerve endings in diffuse
and stretching of the connective tissue surrounding or
inates in the thoracic and abdominal cavities is trans-
can transmit only the chronic-aching-suffering type of
pain.
Ischemia.
Ischemia causes visceral pain in the same way
formation of acidic metabolic end products or tissue-
Chemical Stimuli.
causes widespread digestion of the visceral peritoneum,
Spasm of a Hollow Viscus.
Spasm of a portion of the gut,
causing severe pain.
Often pain from a spastic viscus occurs in the form of
with the pain increasing to a high degree of
Overdistention of a Hollow Viscus.
Extreme overfilling of a
Overdistention can also collapse the blood vessels that
promoting ischemic pain.
Insensitive Viscera.
A few visceral areas are almost com-
the liver capsule is extremely sensitive to both direct
bile ducts are also sensitive
and the parietal pleura are very
sensitive to pain.
“Parietal Pain”
supplied with extensive pain innervation from the
example can emphasize the difference between this
parietal
cut through the visceral peritoneum or through a gut
—
“
”
“Parietal”
Pain from the different viscera is frequently difficult to
brain does not know from firsthand experience that the
transmitted through two pathways to the central
nervous system—the
and the pari-
the sensations are referred to surface areas of the body
sensations are conducted directly into local spinal
the person generally localizes it in the dermatomal
segment from which the visceral organ originated in the
upward along the sympathetic sensory nerves and enter
the body surface that send their own somatosensory
right because the left side of the heart is much more fre-
quently involved in coronary disease than the right.
of the body subserved by the seventh through ninth tho-
areas to which visceral pain is referred from other
from which the respective organs originated.
Pain.
Pain from the viscera is frequently localized to two
surface areas of the body at the same time because of
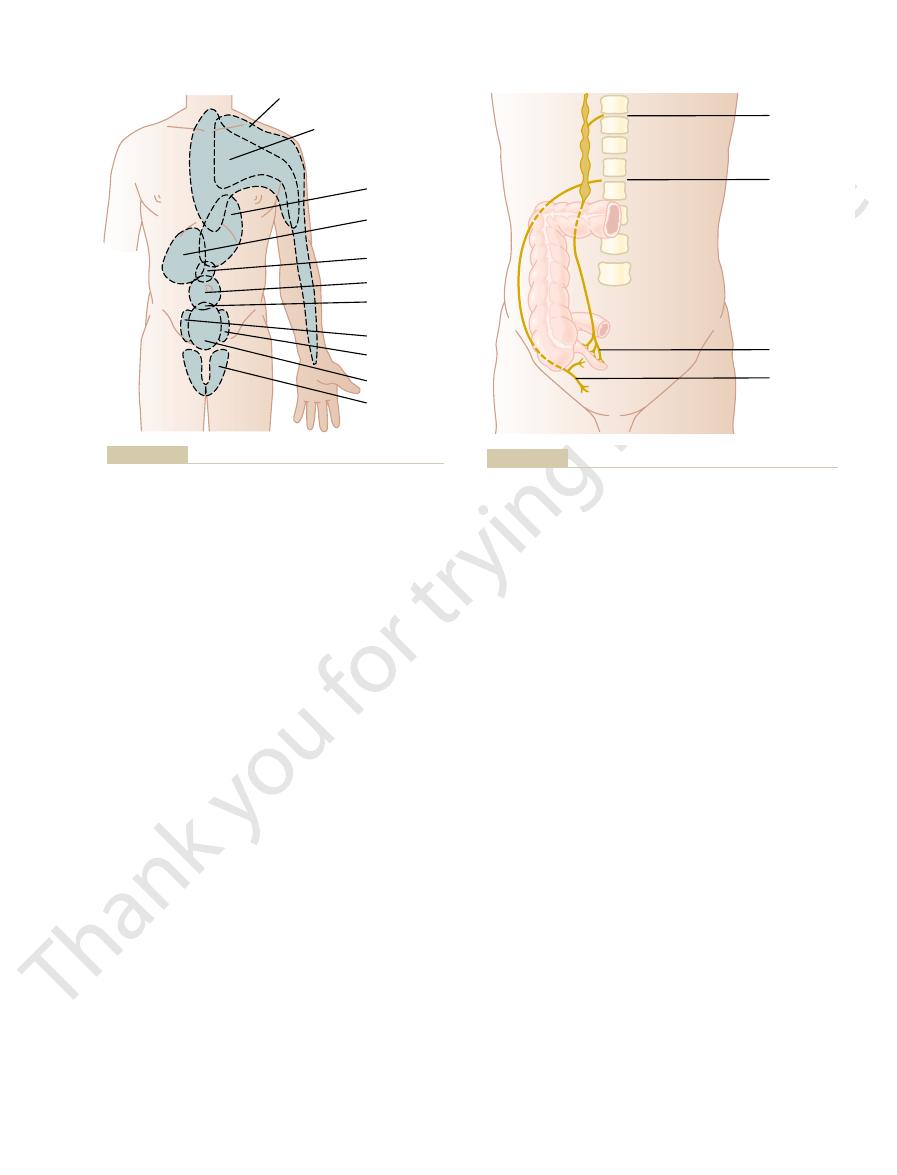
sensitive area. The sensory portion of the fifth nerve is
The pain of tic douloureux can usually be blocked by
mandibular portion of the fifth nerve.
tonsil, it might set off a severe lancinating pain in the
patient swallows a bolus of food, as the food touches a
rather than a pain stimulus. For instance, when the
on the surface of the face, in the mouth, or inside the
few seconds at a time or may be almost continuous.
sudden electrical shocks, and it may appear for only a
). The pain feels like
(or part of the area) of the fifth or ninth nerves; this phe-
Tic Douloureux
and then crusts over within another few days, all of this
ronal peripheral axons to their cutaneous origins. Here
neuronal cytoplasmic flow outward through the neu-
virus. In addition to causing pain, the virus is carried by
The cause of the pain is presumably infection of the
eruption that often ensues.
or “shingles,” because of a skin
herpes zoster,
of pain that circles halfway around the body. The disease
served by the ganglion, thus eliciting a segmental type
This causes severe pain in the dermatomal segment sub-
sequent sections.
thalamus. Several of these lesions are discussed in sub-
prostaglandins, perhaps others. Secondary hyperalgesia
products from the burn—perhaps histamine, perhaps
sensitivity of sunburned skin, which results from
(2) facilitation of sensory transmission, which is called
themselves, which is called
means hypersensitivity to pain. Possible causes of hyper-
sively excitable; this gives rise to
Some Clinical Abnormalities
the abdominal wall. These cause pain of the sharp type
umbilicus and is of the aching, cramping type. Pain
T-10 or T-11; this pain is referred to an area around the
nerve bundles, and then into the spinal cord at about
appendix. Pain impulses pass first from the appendix
Figure 48–7 shows dual transmission from an inflamed
ceral pathway and the direct parietal pathway. Thus,
Somatic Sensations: II. Pain, Headache, and Thermal Sensations
Chapter 48
605
the dual transmission of pain through the referred vis-
through visceral pain fibers located within sympathetic
impulses also often originate in the parietal peritoneum
where the inflamed appendix touches or is adherent to
directly over the irritated peritoneum in the right lower
quadrant of the abdomen.
of Pain and Other
Somatic Sensations
Hyperalgesia
A pain nervous pathway sometimes becomes exces-
hyperalgesia, which
algesia are (1) excessive sensitivity of the pain receptors
primary hyperalgesia, and
secondary hyperalgesia.
An example of primary hyperalgesia is the extreme
sensitization of the skin pain endings by local tissue
frequently results from lesions in the spinal cord or the
Herpes Zoster (Shingles)
Occasionally herpesvirus infects a dorsal root ganglion.
is called
pain neuronal cells in the dorsal root ganglion by the
the virus causes a rash that vesiculates within a few days
occurring within the dermatomal area served by the
infected dorsal root.
Lancinating pain occasionally occurs in some people
over one side of the face in the sensory distribution area
nomenon is called tic douloureux (or trigeminal neural-
gia or glossopharyngeal neuralgia
Often it is set off by exceedingly sensitive trigger areas
throat—almost always by a mechanoreceptive stimulus
surgically cutting the peripheral nerve from the hyper-
H e a r t
E s o p h a g u s
Liver and
gallbladder
Stomach
Pylorus
Umbilicus
Appendix and
small intestine
Right kidney
Left kidney
Colon
Ureter
Surface areas of referred pain from different visceral organs.
Figure 48–6
Visceral pain
T-10
L-1
Parietal pain
Visceral and parietal transmission of pain signals from the
Figure 48–7
appendix.
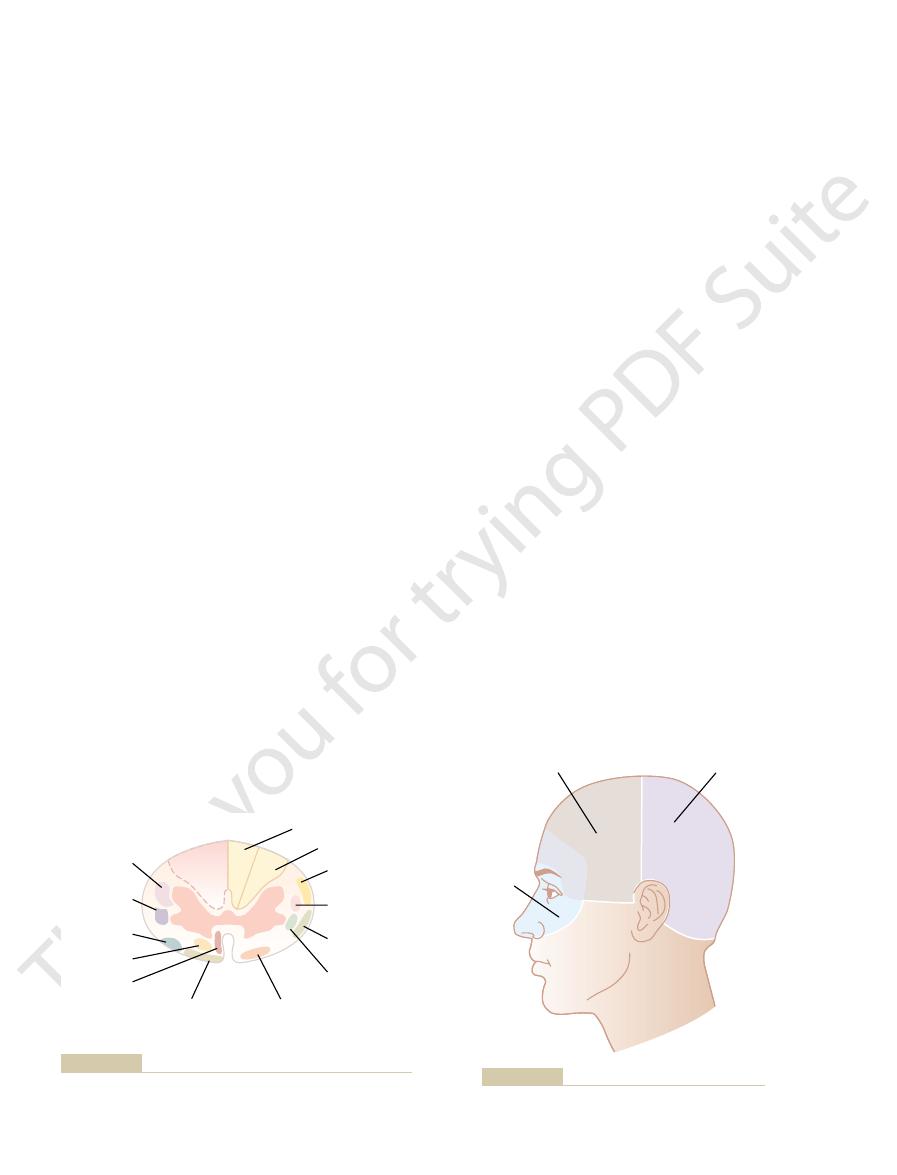
cause “occipital headache” referred to the posterior
and slightly below the ear. Subtentorial pain stimuli
cal nerves, which also supply the scalp above, behind,
through the glossopharyngeal, vagal, and second cervi-
Conversely,
pain impulses from beneath the
cranial nerve, as shown in Figure 48–9.
portion of the fifth nerve and, therefore, causes referred
tentorium itself, initiates pain impulses in the cerebral
above the tentorium, including the upper surface of the
cially sensitive structure is the middle meningeal artery,
can cause headache. An espe-
tizing, crushing, or stretching stimulus to the
ognized as headache. Also, almost any type of trauma-
stretching the dura at
brain, damaging the tentorium,
Conversely,
damage within the brain itself.
sensory cortex stimulated. Therefore, it is likely that
instead, it causes prickly types of paresthesias on the
themselves are almost totally insensitive to pain. Even
The brain tissues
Pain-Sensitive Areas in Cranial Vault.
as from the nasal sinuses.
others result from pain arising outside the cranium, such
result from pain stimuli arising inside the cranium, but
the head from deep head structures. Some headaches
localized, still persists because of partial transmission in
medulla of the brain. “Crude touch,” which is poorly
column, is transected. That is, the fibers in this column
pathway for the transmission of light touch, the dorsal
of the transection. Discrete “light touch” is impaired
ization, and two-point discrimination—are lost
position sensations, vibration sensation, discrete local-
By contrast, the sensations that are transmitted only in
opposite side. The sensations of pain, heat, and cold—
lost on the transected side, and others are lost on the
tion. Yet only some of the modalities of sensation are
knowledge of the cord fiber tracts shown in Figure 48–8.
occurs. The
Brown-Séquard syndrome
one side, the
are blocked, but if the spinal cord is transected on only
If the spinal cord is transected entirely, all sensations
and not in the peripheral nerves.
unsuccessful, indicating that the lesion that causes the
be annoying. Furthermore, sometimes the operation is
leaves the side of the face anesthetic, which in itself may
the sensory elements are destroyed. This operation
needed for many jaw movements, can be spared while
from each other, so that the motor portions, which are
often sectioned immediately inside the cranium, where
The Nervous System: A. General Principles and Sensory Physiology
606
Unit IX
the motor and sensory roots of the fifth nerve separate
pain might be in the sensory nucleus in the brain stem
Brown-Séquard Syndrome
and motor functions distal to the segment of transection
effects of such transection can be predicted from a
All motor functions are blocked on the side of the tran-
section in all segments below the level of the transec-
sensations served by the spinothalamic pathway—are
lost on the opposite side of the body in all dermatomes
two to six segments below the level of the transection.
the dorsal and dorsolateral columns—kinesthetic and
on the
side of the transection in all dermatomes below the level
on the side of the transection because the principal
do not cross to the opposite side until they reach the
the opposite spinothalamic tract.
Headache
Headaches are a type of pain referred to the surface of
Headache of Intracranial Origin
cutting or electrically stimulating the sensory areas
of the cerebral cortex only occasionally causes pain;
area of the body represented by the portion of the
much or most of the pain of headache is not caused by
tugging on the venous sinuses around the
or
the base of the brain can cause intense pain that is rec-
blood
vessels of the meninges
and neurosurgeons are careful to anesthetize this artery
specifically when performing brain operations under
local anesthesia.
Areas of the Head to Which Intracranial Headache Is Referred.
Stimulation of pain receptors in the cerebral vault
headache to the front half of the head in the surface
areas supplied by this somatosensory portion of the fifth
tentorium enter the central nervous system mainly
part of the head.
Lateral
corticospinal
Rubrospinal
Olivospinal
Tectospinal
Vestibulospinal
Descending
Tracts
Ventral
corticospinal
Fasciculus cuneatus
Fasciculus gracilis
Dorsal
spinocerebellar
Ventral
spinocerebellar
Ventral spinothalamic
Spinotectal
Ascending
Tracts
Lateral
spinothalamic
Cross section of the spinal cord, showing principal ascending
Figure 48–8
tracts on the right and principal descending tracts on the left.
Brain stem and
cerebellar vault
headaches
Cerebral vault
headaches
Nasal sinus
and eye
headaches
Areas of headache resulting from different causes.
Figure 48–9
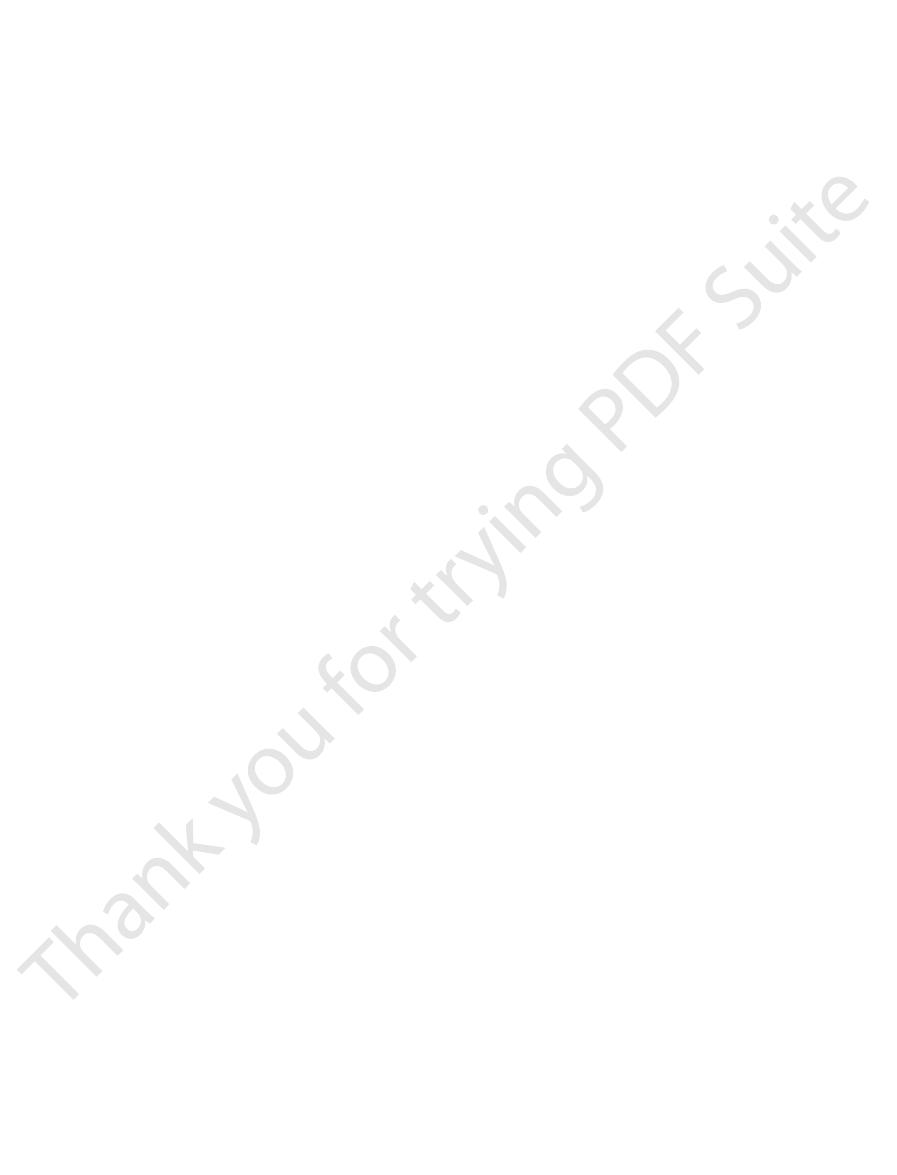
spots.
The cold and warmth receptors are located imme-
“burning hot” sensations.
cold and warmth receptors, for “freezing cold” and
cold and, therefore, are responsible, along with the
warmth receptors, and pain receptors. The pain recep-
three types of sensory receptors: cold receptors,
Thermal gradations are discriminated by at least
cold and heat, from
The human being can perceive different gradations of
Thermal Sensations
cause of the headache.
retina can also burn the retina, and this could be the
the surface of the head or retro-orbitally. However,
irritation of the conjunctivae, and the pain is referred to
hours. The headache sometimes results from “actinic”
tion by light rays, especially ultraviolet light. Looking at
headache.
and extraocular muscles, which is a possible cause of
orbital headache. Also, excessive attempts to focus
Even though these muscles are extremely small, it is
one’s eyes clearly may cause excessive contraction of
illary sinuses, can be felt in the face.
Also, pain from the lower sinuses, such as from the max-
faces of the forehead and scalp, as shown in Figure 48–9.
in the case of frontal sinus infection, to the frontal sur-
and cause headache that is referred behind the eyes or,
Nevertheless, infection or other irritative processes in
nasal sinuses are sensitive to pain, but not intensely so.
The mucous membranes of the nose and
Headache Caused by Irritation of Nasal and Accessory Nasal
lesions do.
headache. The pain of the spastic head muscles suppos-
muscles attached to the occiput, to become spastic, and
often causes many of the muscles of the head, especially
Extracranial Types of Headache
impulses from the colon. Therefore, it may result from
pain sensory tracts in the spinal cord have been cut, we
headache in many people. Because it has been shown
is most likely that alcohol, because it is toxic to tissues,
enced, a headache usually follows an alcoholic binge. It
migraine has been reported in 65 to 90 per cent of cases.
headaches, because a positive family history for
There may be a genetic predisposition to migraine
pression, psychological abnormalities, and vasospasm
of migraine headaches. Other theories of the cause
of the arteries—including some extracranial arteries,
vessels causes them to dilate and pulsate intensely, and
lar tone for 24 to 48 hours. The blood pressure in the
smooth muscle contraction, to allow the blood vessels
happens to the vascular walls, perhaps exhaustion of
Then, as a result of the intense ischemia, something
and this is responsible for the prodromal symptoms.
including arteries that supply the brain. The vasospasm
symptoms.
beginning of the headache. Any theory that explains
of sensory hallucinations. Ordinarily, the prodromal
part of the field of vision, visual aura, and other types
prodromal sensations, such as nausea, loss of vision in
unknown. Migraine headaches often begin with various
cular phenomena, although the exact mechanism is
headache.
by the cerebrospinal fluid. The weight of the brain
headache. Removing this quantity of fluid removes part
upright position, often causes intense intracranial
spinal canal, particularly if the person remains in an
around the venous sinuses. Such intense damage can
causes inflammation of all the meninges, including the
headaches of all is that resulting from meningitis, which
Types of Intracranial Headache
Somatic Sensations: II. Pain, Headache, and Thermal Sensations
Chapter 48
607
Headache of Meningitis.
One of the most severe
sensitive areas of the dura and the sensitive areas
cause extreme headache pain referred over the entire
head.
Headache Caused by Low Cerebrospinal Fluid Pressure.
Removing as little as 20 milliliters of fluid from the
of the flotation for the brain that is normally provided
stretches and otherwise distorts the various dural
surfaces and thereby elicits the pain that causes the
Migraine Headache.
Migraine headache is a special type
of headache that is thought to result from abnormal vas-
symptoms begin 30 minutes to 1 hour before the
migraine headache must also explain the prodromal
One of the theories of the cause of migraine
headaches is that prolonged emotion or tension causes
reflex vasospasm of some of the arteries of the head,
theoretically produces ischemia of portions of the brain,
to become flaccid and incapable of maintaining vascu-
it is postulated that the excessive stretching of the walls
such as the temporal artery—causes the actual pain
of migraine headaches include spreading cortical de-
caused by excess local potassium in the cerebral extra-
cellular fluid.
Migraine headaches also occur about twice as fre-
quently in women as in men.
Alcoholic Headache.
As many people have experi-
directly irritates the meninges and causes the intracra-
nial pain.
Headache Caused by Constipation.
Constipation causes
that constipation headache can occur in people whose
know that this headache is not caused by nervous
absorbed toxic products or from changes in the circula-
tory system resulting from loss of fluid into the gut.
Headache Resulting from Muscle Spasm.
Emotional tension
those muscles attached to the scalp and the neck
it is postulated that this is one of the common causes of
edly is referred to the overlying areas of the head and
gives one the same type of headache as intracranial
Structures.
widespread areas of the nasal structures often summate
Headache Caused by Eye Disorders.
Difficulty in focusing
the eye ciliary muscles in an attempt to gain clear vision.
believed that tonic contraction of them can cause retro-
the eyes can result in reflex spasm in various facial
A second type of headache that originates in the eyes
occurs when the eyes are exposed to excessive irradia-
the sun or the arc of an arc-welder for even a few
seconds may result in headache that lasts from 24 to 48
focusing intense light from an arc or the sun on the
Thermal Receptors and
Their Excitation
freezing cold to cold to cool to
indifferent to warm to hot to burning hot.
tors are stimulated only by extreme degrees of heat or
diately under the skin at discrete separated
In
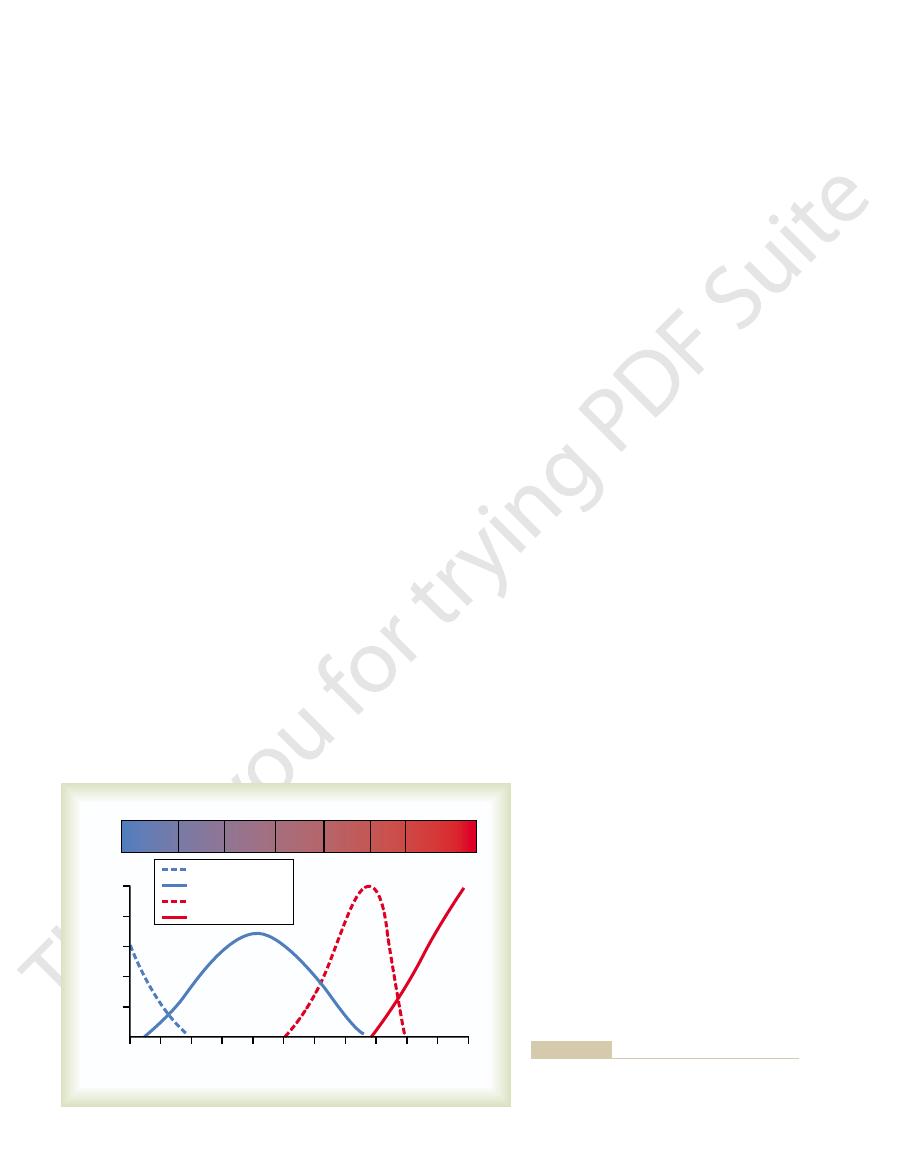
heated room to the out-of-doors on a cold day.
temperature if it were constant. The response to
versely, if the temperature is actively rising, the person
the temperature remains cold at the same level. Con-
actively falling, a person feels much colder than when
This means that when the temperature of the skin is
being able to respond to steady states of temperature.
changes in temperature,
Thus, it is evident that the thermal senses respond
extent, but never 100 per cent.
more. In other words, the receptor “adapts” to a great
becomes strongly stimulated at first, but this stimula-
denly subjected to an abrupt fall in temperature, it
When a cold receptor is sud-
Stimulatory Effects of Rising and Falling Temperature—Adap-
feel almost alike.
tion—that is, freezing cold and burning hot sensations
enough, may give almost the same quality of sensa-
painful and why both these sensations, when intense
different types of endings. One can also understand
One can understand from Figure 48–10 that a
ulated again, possibly because of damage to the cold
paradoxically, some of the cold fibers begin to be stim-
also fade out at about 49°C. Finally, at around 45°C,
warmth receptors begin to be stimulated, but these
out slightly above 40°C. Above about 30°C, the
cease, but the cold receptors begin to be stimulated,
perature rises to +10° to 15°C, the cold-pain impulses
freeze, these fibers cannot be stimulated). As the tem-
even colder, so that it nearly freezes or actually does
cold region, only
temperature. For instance, in the
pain fiber stimulated by heat. Note especially that
by cold, (2) a cold fiber, (3) a warmth fiber, and (4) a
four types of nerve fibers: (1) a pain fiber stimulated
Figure 48–10 shows the
Indifferent, Warm, and Hot.
as cold receptors.
transmitted in type C nerve fibers as well, which sug-
20 m/sec. Some cold sensations are believed to be
tors via type A
dermal cells. Signals are transmitted from these recep-
ending that branches a number of times, the tips of
tified. It is a special, small type A
Conversely, a definitive cold receptor has been iden-
at transmission velocities of only 0.4 to 2 m/sec.
presumed to be free nerve endings, because warmth
they have not been identified histologically. They are
endings is quite certain, based on psychological tests,
cold spots as warmth spots, and the number in differ-
most areas of the body, there are 3 to 10 times as many
The Nervous System: A. General Principles and Sensory Physiology
608
Unit IX
ent areas of the body varies from 15 to 25 cold spots
per square centimeter in the lips to 3 to 5 cold spots
per square centimeter in the finger to less than 1 cold
spot per square centimeter in some broad surface
areas of the trunk.
Although the existence of distinctive warmth nerve
signals are transmitted mainly over type C nerve fibers
d myelinated nerve
which protrude into the bottom surfaces of basal epi-
d nerve fibers at velocities of about
gests that some free nerve endings also might function
Stimulation of Thermal Receptors—Sensations of Cold, Cool,
effects of different temperatures on the responses of
these fibers respond differently at different levels of
very
the cold-pain fibers are stimulated (if the skin becomes
reaching peak stimulation at about 24°C and fading
the heat-pain fibers begin to be stimulated by heat and,
endings caused by the excessive heat.
person determines the different gradations of thermal
sensations by the relative degrees of stimulation of the
why extreme degrees of both cold and heat can be
tation of Thermal Receptors.
tion fades rapidly during the first few seconds and pro-
gressively more slowly during the next 30 minutes or
markedly to
in addition to
feels much warmer than he or she would at the same
changes in temperature explains the extreme degree
of heat one feels on first entering a tub of hot water
and the extreme degree of cold felt on going from a
Warmth receptors
15
25
35
45
55
20
30
40
50
60
Cold
Cool
Warm
Hot
5
10
Freezing
cold
Indiffer-
ent
Burning
hot
10
Cold-pain
Heat-pain
Cold-receptors
8
6
4
2
Temperature (
∞
C)
Impulses per second
heat-pain fiber.
fiber,
warmth
cold fiber,
cold-pain fiber,
tures of a
Discharge frequencies at different skin tempera-
Figure 48–10
a
a
and a
ception (minireview). Endocr Regul 34:195, 2000.
Zubrzycka M, Janecka A: Substance P: transmitter of noci-
states. Physiol Rev 82:981, 2002.
Watkins LR, Maier SF: Beyond neurons: evidence that
J Med 347:362, 2002.
Vogt BA: Knocking out the DREAM to study pain. N Engl
Silberstein SD: Migraine. Lancet 363:381, 2004.
of pain in arthritis. Ann N Y Acad Sci 966:343, 2002.
Schaible HG, Ebersberger A, Von Banchet GS: Mechanisms
tion on underlying mechanisms. Curr Opin Neurol 17:289,
Sanchez-del-Rio M, Reuter U: Migraine aura: new informa-
cool. Curr Biol 13:R476, 2003.
Montell C: Thermosensation: hot findings make TRPNs very
neuropathy. N Engl J Med 348:1243, 2003.
Mendell JR, Sahenk Z: Clinical practice: painful sensory
headache genetics. Curr Opin Neurol 17:283, 2004.
Kors EE, Vanmolkot KR, Haan J, et al: Recent findings in
Science, 4th ed. New York: McGraw-Hill, 2000.
Kandel ER, Schwartz JH, Jessell TM: Principles of Neural
Opin Neurobiol 13:487, 2003.
peppermint: the molecular logic of thermosensation. Curr
Jordt SE, McKemy DD, Julius D: Lessons from peppers and
Churchill Livingstone, 2003.
Haines DE, Lancon JA: Review of Neuroscience. New York:
Churchill Livingstone, 1997.
Haines DE: Fundamental Neuroscience. New York:
Biobehav Rev 27:729, 2004.
Gebhart GF: Descending modulation of pain. Neurosci
spinal gate. Cell 108:297, 2002.
Costigan M, Woolf CJ: No DREAM, no pain: closing the
Pharmacol 3:608, 2003.
controlling gastrointestinal pain pathways. Curr Opin
Cervero F, Laird JM: Role of ion channels in mechanisms
Bruera E, Kim HN: Cancer pain. JAMA 290:2476, 2003.
Bromm B: Brain images of pain. News Physiol Sci 16:244,
Deliv Rev 55:967, 2003.
integrative clinical and basic neurobiology. Adv Drug
Borsook D, Becerra L: Pain imaging: future applications to
N Engl J Med 349:1943, 2003.
Ballantyne JC, Mao J: Opioid therapy for chronic pain.
a neuroanatomical review. Brain Res 1000:40, 2004.
Almeida TF, Roizenblatt S, Tufik S: Afferent pain pathways:
tinguish gradations of temperature.
stimuli on a specific area of the skin. However, removal
complex. Occasionally a neuron in cortical somatic
the ventrobasal complex of the thalamus.
enter long, ascending thermal fibers that cross to the
processing by one or more cord neurons, the signals
horns—the same as for pain. After a small amount of
terminate mainly in laminae I, II, and III of the dorsal
spinal cord, the signals travel for a few segments
parallel to those for pain signals. On entering the
In general, thermal signals are transmitted in pathways
Transmission of Thermal Signals
1 square centimeter in size.
versely, temperature changes 100 times as great often
the entire surface of the body simultaneously. Con-
summate. For instance, rapid changes in temperature
all at once, the thermal signals from the entire area
lated. However, when a large skin area is stimulated
area of the body is slight, it is difficult to judge grada-
as modified by temperature.
words, thermal detection probably results not from
more than twofold for each 10°C change. In other
stimulated by changes in their metabolic rates, and
Thermal Receptors
Somatic Sensations: II. Pain, Headache, and Thermal Sensations
Chapter 48
609
Mechanism of Stimulation of
It is believed that the cold and warmth receptors are
that these changes result from the fact that tempera-
ture alters the rate of intracellular chemical reactions
direct physical effects of heat or cold on the nerve
endings but from chemical stimulation of the endings
Spatial Summation of Thermal Sensations.
Because the
number of cold or warm endings in any one surface
tions of temperature when small skin areas are stimu-
as little as 0.01°C can be detected if this change affects
will not be detected when the affected skin area is only
in the Nervous System
upward or downward in the tract of Lissauer and then
opposite anterolateral sensory tract and terminate in
both (1) the reticular areas of the brain stem and (2)
A few thermal signals are also relayed to the cere-
bral somatic sensory cortex from the ventrobasal
sensory area I has been found by microelectrode
studies to be directly responsive to either cold or warm
of the entire cortical postcentral gyrus in the human
being reduces but does not abolish the ability to dis-
References
2001.
2004.
immune and glial cells contribute to pathological pain
