the middle and widest layer, constitutes about 75 per
zona fasciculata,
2. The
which is necessary for synthesis of aldosterone. The secretion of these cells
aldosterone synthase,
capsule, constitutes about 15 per cent of the adrenal cortex. These cells are
zona glomerulosa,
1. The
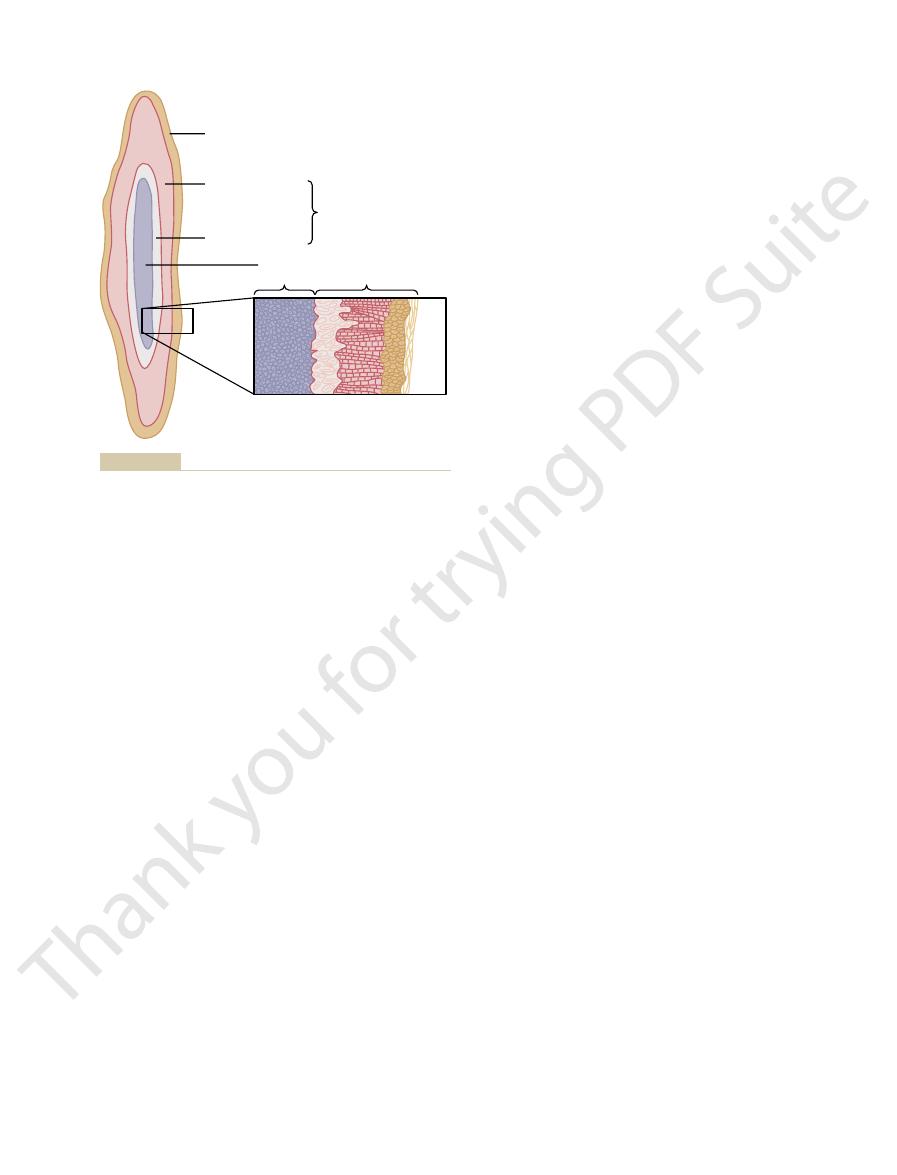
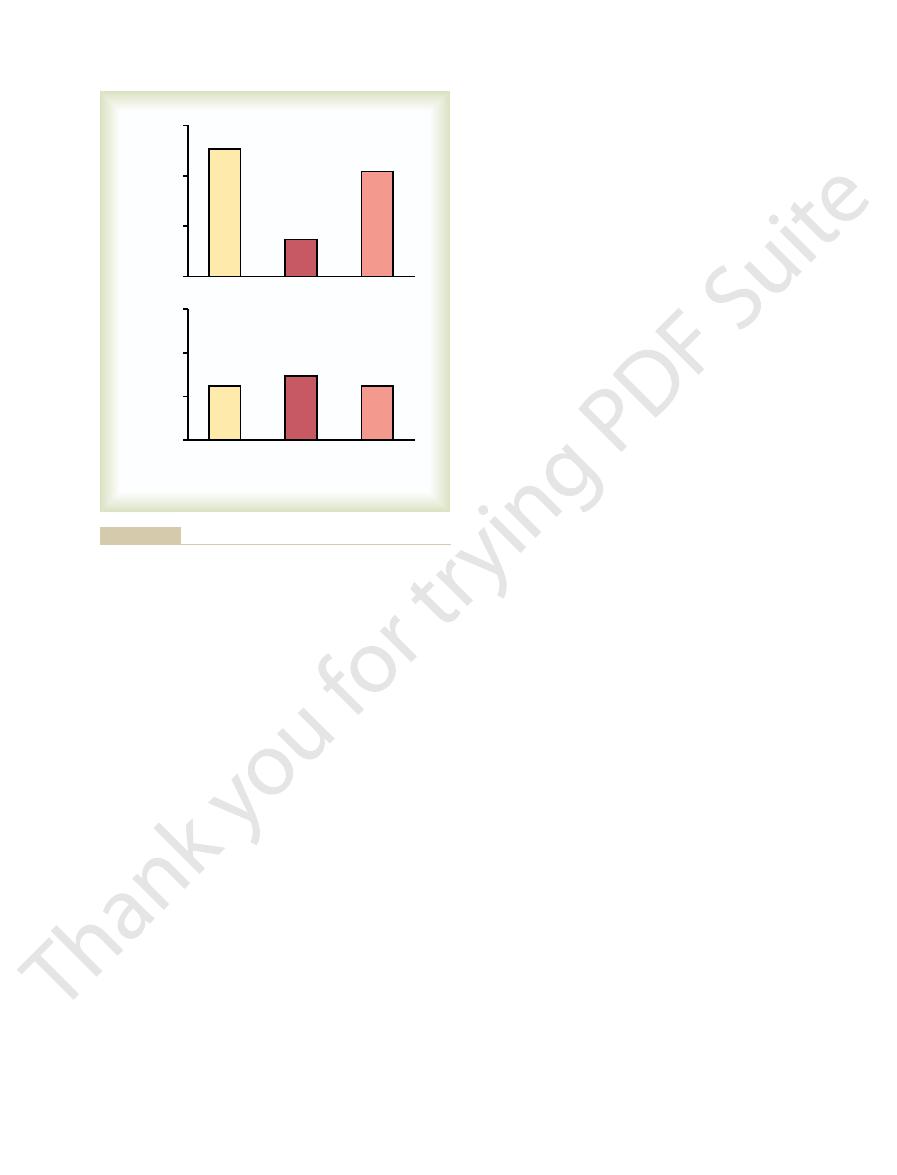
Figure 77–1 shows that the adrenal
Adrenocortical Hormones
Synthesis and Secretion of
which is the principal mineralocorticoid, and
aldosterone,
More than 30 steroids have been isolated from the adrenal cortex, but two
exhibit important effects that increase blood glucose concentration. They have
sium, in particular. The
the electrolytes (the “minerals”) of the extracellular fluids-sodium and potas-
The
chapter) and can result in masculinizing effects.
cortices, extreme quantities can be secreted (which is discussed later in the
mally of only slight importance, although in certain abnormalities of the adrenal
same effects in the body as the male sex hormone testosterone. They are nor-
androgenic hormones,
mones are secreted, especially
secreted by the adrenal cortex. In addition to these, small amounts of sex hor-
glucocorticoids,
adrenocortical hormones, the
Two major types of
molecular structures give them several different but very important functions.
and they all have similar chemical formulas. However, slight differences in their
These hormones are all synthesized from the steroid cholesterol,
corticosteroids.
The adrenal cortex secretes an entirely different group of hormones, called
These hormones and their effects are discussed in detail in Chapter 60 in rela-
effects as direct stimulation of the sympathetic nerves in all parts of the body.
to sympathetic stimulation. In turn, these hormones cause almost the same
sympathetic nervous system; it secretes the hor-
per cent of the gland, is functionally related to the
The adrenal medulla, the central 20
two distinct parts, the
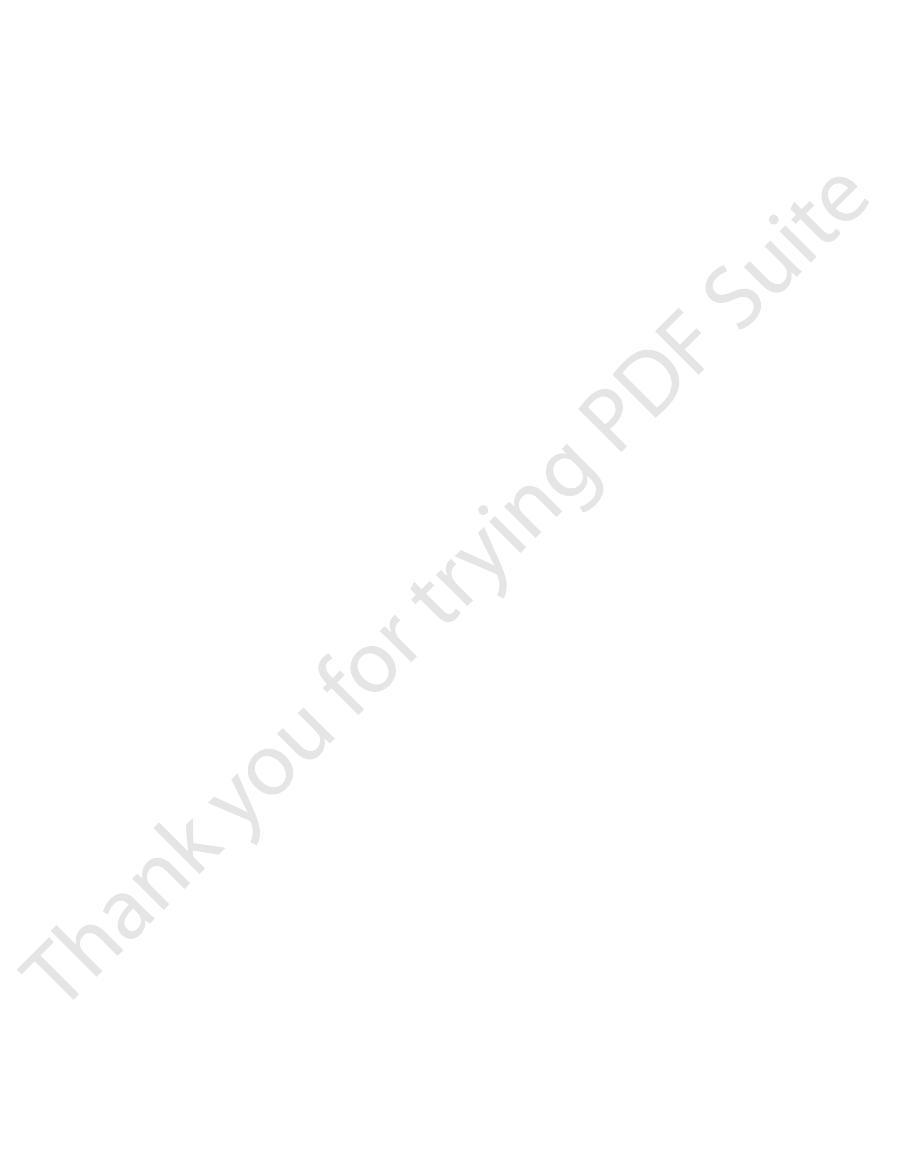
As shown in Figure 77–1, each gland is composed of
4 grams, lie at the superior poles of the two kidneys.
adrenal glands,
The two
C
H
A
P
T
E
R
7
7
944
Adrenocortical Hormones
each of which weighs about
adrenal medulla and the
adrenal cortex.
mones epinephrine and norepinephrine in response
tion to the sympathetic nervous system.
Corticosteroids Mineralocorticoids, Glucocorticoids, and Androgens.
mineralocorticoids and the
are
which exhibit about the
mineralocorticoids have gained this name because they especially affect
glucocorticoids have gained their name because they
additional effects on both protein and fat metabolism that are equally as impor-
tant to body function as their effects on carbohydrate metabolism.
are of exceptional importance to the normal endocrine function of the human
body:
cortisol, which
is the principal glucocorticoid.
The Adrenal Cortex Has Three Distinct Layers.
cortex is composed of three relatively distinct layers:
a thin layer of cells that lies just underneath the
the only ones in the adrenal gland capable of secreting significant amounts
of aldosterone because they contain the enzyme
is controlled mainly by the extracellular fluid concentrations of angiotensin
II and potassium, both of which stimulate aldosterone secretion.
cent of the adrenal cortex and secretes the glucocorticoids cortisol and
-Fluorocortisol (synthetic, slightly more potent
• Corticosterone (slight mineralocorticoid activity)
aldosterone, but very small quantities secreted)
• Desoxycorticosterone (1/30 as potent as
• Aldosterone (very potent, accounts for about 90 per
following as summarized in Table 77–1:
teroid hormones, including the synthetic ones, are the
therapy. Some of the more important of the corticos-
adrenal cortex. And several additional potent steroid
both, are normally secreted in small amounts by the
having glucocorticoid or mineralocorticoid activities, or
In addition to aldosterone and cortisol, other steroids
21. The mineralocorticoid aldosterone has an oxygen
Figure 77–2. Cortisol has a keto-oxygen on carbon
glucocorticoid hormones, respectively, are shown in
The chemical formulas of aldosterone and cortisol,
activity of only one of the enzymes in this pathway.
formed. For example, very large quantities of masculin-
catalyzed by a specific enzyme system. A change in even
of these organelles and some in the other. Each step is
mitochondria
in two of the organelles of the cell, the
tisol, and the androgens. Essentially all these steps occur
steroid products of the adrenal cortex: aldosterone, cor-
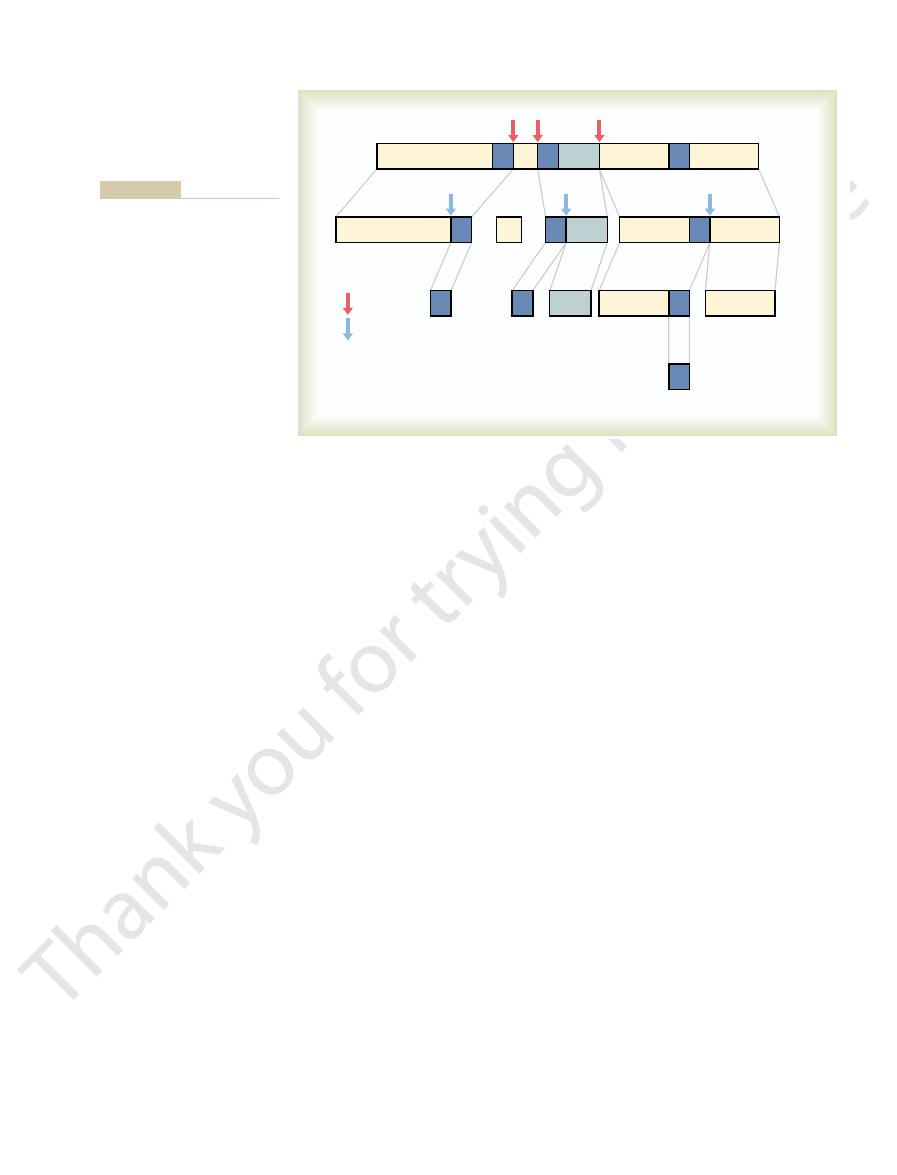
Figure 77–2 gives
pregnenolone.
secretion, increase the conversion of cholesterol to
tion, and angiotensin II, which stimulates aldosterone
example, both ACTH, which stimulates cortisol secre-
major hormone products aldosterone and cortisol. For
cortex, this initial step in steroid synthesis is stimulated
steroids (Figure 77–2). In all three zones of the adrenal
cholesterol desmolase
the mitochondria, where it is cleaved by the enzyme
Once the cholesterol enters the cell, it is delivered to
for LDL, as well as the activity of enzymes that liberate
ACTH, which stimulates adrenal steroid synthesis,
the amount available for steroid synthesis. For example,
Transport of cholesterol into the adrenal cells is reg-
hormones.
endocytosis,
the adrenocortical cell membranes. The coated pits are
high concentrations of cholesterol, diffuse from the
(LDL) in the circulating plasma. The LDLs, which have
de novo small amounts of cholesterol from acetate,
by the adrenal cortex, are synthesized from cholesterol.
All human steroid hormones, including those produced
as ACTH that increase secretion of cortisol and
no effect on the other two zones. Similarly, factors such
independent mechanisms. Factors such as angiotensin
mineralocorticoids.
androgen production, however, are not nearly as
involved. The mechanisms for controlling adrenal
released from the pituitary, may also be
hormone,
regulates secretion of these cells, although other
estrogens and some glucocorticoids. ACTH also
androstenedione,
cortex, secretes the adrenal androgens
zona reticularis,
3. The
adrenocorticotropic hormone (ACTH).
The secretion
estrogens.
corticosterone,
Chapter 77
Adrenocortical Hormones
945
as well as small amounts of
adrenal androgens and
of these cells is controlled in large part by
the hypothalamic-pituitary axis via
the deep layer of the
dehydroepiandrosterone (DHEA) and
as well as small amounts of
factors such as cortical androgen-stimulating
well understood as those for glucocorticoids and
Aldosterone and cortisol secretion are regulated by
II that specifically increase the output of aldosterone
and cause hypertrophy of the zona glomerulosa have
adrenal androgens and cause hypertrophy of the zona
fasciculata and zona reticularis have little or no effect
on the zona glomerulosa.
Adrenocortical Hormones Are Steroids Derived from Cholesterol.
Although the cells of the adrenal cortex can synthesize
approximately 80 per cent of the cholesterol used for
steroid synthesis is provided by low-density lipoproteins
plasma into the interstitial fluid and attach to specific
receptors contained in structures called coated pits on
then internalized by
forming vesicles that
eventually fuse with cell lysosomes and release choles-
terol that can be used to synthesize adrenal steroid
ulated by feedback mechanisms that can markedly alter
increases the number of adrenocortical cell receptors
cholesterol from LDL.
to form pregnenolone; this is the
rate-limiting step in the eventual formation of adrenal
by the different factors that control secretion of the
Synthetic Pathways for Adrenal Steroids.
the principal steps in the formation of the important
and
the endoplasmic reticulum, some steps occurring in one
a single enzyme in the schema can cause vastly differ-
ent types and relative proportions of hormones to be
izing sex hormones or other steroid compounds not
normally present in the blood can occur with altered
which are the most important mineralocorticoid and
number 3 and is hydroxylated at carbon numbers 11 and
atom bound at the number 18 carbon.
hormones not normally formed in the adrenal glands
have been synthesized and are used in various forms of
Mineralocorticoids
cent of all mineralocorticoid activity)
• 9
a
than aldosterone)
Cortisol
and
androgens
Magnified section
Zona glomerulosa
aldosterone
Zona fasciculata
Zona reticularis
Cortex
Medulla
(catecholamines)
adrenal cortex and secretion of catecholamines by the adrenal
Secretion of adrenocortical hormones by the different zones of the
Figure 77–1
medulla.

946
Unit XIV
Endocrinology and Reproduction
20 Lyase
20 Lyase
(P450 c11AS)
(P450 c11)
14
15
Cholesterol
desmolase
(P450 scc)
17
a
-Hydroxylase
(P450 c17)
3
b
-Hydroxysteroid
dehydrogenase
HO
C
O
CH
3
C
D
A
HO
3
2
1
10
19
11
12
13
18
17
16
21 20
22
23
24
26
27
25
4
6
9
7
8
5
B
17
a
-Hydroxylase
(P450 c17)
21
b
-Hydroxylase
(P450 c21)
O
C
O
CH
3
11
b
-Hydroxylase
O
C
O
CH
2
OH
Aldosterone
synthase
O
HO
C
O
CH
2
OH
17
,
(P450 c17)
17
,
(P450 c17)
HO
C
O
OH
OH
OH
OH
CH
3
O
C
O
CH
3
O
C
O
CH
2
OH
HO
O
O
O
O
HO
C
O
CH
2
OH
O
HO
HC
C
O
O
CH
2
OH
Pregnenolone
Progesterone
11-Deoxycorticosterone
Corticosterone
17-Hydroxypregnenolone
17-Hydroxyprogesterone
Dehydroepl-
androsterone
Androstenedione
11-Deoxycortisol
Cortisol
Aldosterone
Cholesterol
Pathways for synthesis of steroid hormones by the adrenal cortex. The enzymes are shown in italics.
Figure 77–2
tration of the extracellular fluid rises markedly, sodium
Without mineralocorticoids, potassium ion concen-
therapy or injection of mineralocorticoids.
Total loss of adreno-
Chloride Wasting and Hyperkalemia.
Aldosterone
Mineralocorticoids-
20 mg/day.
12 µg/100 ml, and the secretory rate averages 15 to
The concentration of cortisol in the blood averages
150 µg/day (0.15 mg/day).
100 ml, and the average secretory rate is approximately
The normal concentration of aldosterone in blood
inactive conjugates.
mones, and kidney diseases reduce the excretion of the
and excreted in the urine. Diseases of the liver markedly
plasma, and are therefore filtered readily by the kidneys
bound to plasma proteins, are highly soluble in the
the bile and then in the feces. The remaining conjugates
not have mineralocorticoid or glucocorticoid activity.
extent, sulfates. These substances are inactive and do
and, to a lesser
The
Adrenocortical Hormones Are Metabolized in the Liver.
tion of the adrenal hormones to the tissues.
episodic secretion of ACTH. This reservoir function
example, with cortisol during brief periods of stress and
in free hormone concentrations, as would occur, for
minutes. In both the combined and free forms, the hor-
so that about 40 per cent is in the free form; as a result,
culating aldosterone combines with the plasma proteins,
life of 60 to 90 minutes. Only about 60 per cent of cir-
the plasma; therefore, cortisol has a relatively long half-
lesser extent, to albumin. This high degree of binding to
and, to a
plasma binds to plasma proteins, especially a globulin
tant drug for stimulating specific glucocorticoid activity.
eralocorticoid activity, makes this an especially impor-
hormone dexamethasone, which has almost zero min-
The intense glucocorticoid activity of the synthetic
potent glucocorticoid effects.
mineralocorticoid effects, along with its much more
amount of mineralocorticoid activity, because some syn-
ties.
• Dexamethasone (synthetic, 30 times as potent as
• Methylprednisone (synthetic, five times as potent as
• Prednisone (synthetic, four times as potent as
• Cortisone (synthetic, almost as potent as cortisol)
glucocorticoid activity, but much less potent than
• Corticosterone (provides about 4 per cent of total
• Cortisol (very potent, accounts for about 95 per
• Cortisone (synthetic, slight mineralocorticoid
• Cortisol (very slight mineralocorticoid activity, but
Chapter 77
Adrenocortical Hormones
947
large quantity secreted)
activity)
Glucocorticoids
cent of all glucocorticoid activity)
cortisol)
cortisol)
cortisol)
cortisol)
It is clear from this list that some of these hormones
have both glucocorticoid and mineralocorticoid activi-
It is especially significant that cortisol has a small
dromes of excess cortisol secretion can cause significant
Adrenocortical Hormones Are Bound to Plasma Proteins.
Approximately 90 to 95 per cent of the cortisol in the
called cortisol-binding globulin or transcortin
plasma proteins slows the elimination of cortisol from
aldosterone has a relatively short half-life of about 20
mones are transported throughout the extracellular
fluid compartment.
Binding of adrenal steroids to the plasma proteins
may serve as a reservoir to lessen rapid fluctuations
may also help to ensure a relatively uniform distribu-
adrenal steroids are degraded mainly in the liver and
conjugated especially to glucuronic acid
About 25 per cent of these conjugates are excreted in
formed by the liver enter the circulation but are not
depress the rate of inactivation of adrenocortical hor-
is about 6 nanograms (6 billionths of a gram) per
Functions of the
Mineralocorticoid Deficiency Causes Severe Renal Sodium
cortical secretion usually causes death within 3 days to
2 weeks unless the person receives extensive salt
Table 77–1
-fluorocortisol
—
—
10
125
Dexamethasone
—
—
30
—
Methylprednisone
—
—
5
—
Prednisolone
—
—
4
0.8
Cortisone
—
—
1.0
1.0
Dehydroepiandrosterone
175
20
—
—
Deoxycorticosterone
0.006
0.2
0.2
100
Aldosterone
0.006
0.15
0.3
3000
Corticosterone
0.4
3
0.3
15.0
Cortisol
12
15
1
1
g/100 ml)
Secreted (mg/24 hr)
Activity
Activity
(free and bound,
Average Amount
Glucocorticoid
Mineralocorticoid
Average Plasma
Adrenal Steroid Hormones in Adults; Synthetic Steroids and Their Relative Glucocorticoid and Mineralocorticoid Activities
Concentration
Steroids
m
Adrenal Steroids
Synthetic Steroids
9
a
Glucocorticoid and mineralocorticoid activities of the steroids are relative to cortisol, with cortisol being 1.0.
This return to normal of salt and water excretion by
water to normal despite the excess aldosterone (Figure
sure also increases 15 to 25 mm Hg, and this elevated
increases 5 to 15 per cent above normal, arterial pres-
respectively. Thus, after the extracellular fluid volume
pressure diuresis,
water, called
explained in Chapter 19. The rise in arterial pressure
also leads to an increase in arterial pressure, as
secreted. An aldosterone-mediated increase in extra-
powerful sodium-retaining hormones, only transient
Even though aldosterone is one of the body’s most
retained sodium, but without much change in sodium
intake, if water is available. Therefore, the extracellu-
Also, small increases in extracellular fluid sodium
absorption of almost equivalent amounts of water.
sorbed by the tubules, there is simultaneous osmotic
lents. The reason for this is that when sodium is reab-
by the kidneys, the concentration of sodium in the
Excess Aldosterone Increases Extracellular Fluid Volume and
of all the sodium in the body. At the same time, potas-
urine a day, an amount equal to one tenth to one fifth
Conversely, total lack of aldosterone secretion can
fold. Therefore, the net effect of excess aldosterone
time, potassium loss into the urine increases several-
to as little as a few milliequivalents a day. At the same
potassium excretion in the urine.
lecting ducts. Therefore, aldosterone causes sodium to
and, to a lesser extent, in the distal tubules and col-
Aldosterone Increases Renal Tubular Reabsorption of Sodium
nearly 2000 times that of aldosterone.
of cortisol, but the plasma concentration of cortisol is
of mineralocorticoid activity. Aldosterone’s mineralo-
the adrenal cortex, also provides a significant amount
tions, but cortisol, the major glucocorticoid secreted by
discussed later in the chapter.
life’s intermittent physical and mental “stresses,” as
The glucocorticoids are equally necessary, however,
“lifesaving” portion of the adrenocortical hormones.
fore, the mineralocorticoids are said to be the acute
aldosterone or some other mineralocorticoid. There-
shocklike state, followed by death. This entire
diminished cardiac output, which progresses to a
become greatly reduced. The person soon develops
and chloride are rapidly lost from the body, and the
948
Unit XIV
Endocrinology and Reproduction
total extracellular fluid volume and blood volume
sequence can be prevented by the administration of
allowing the person to resist the destructive effects of
Aldosterone Is the Major Mineralocorticoid Secreted by the
Adrenals.
Aldosterone exerts nearly 90 per cent of the
mineralocorticoid activity of the adrenocortical secre-
corticoid activity is about 3000 times greater than that
Renal and Circulatory Effects
of Aldosterone
and Secretion of Potassium.
It will be recalled from
Chapter 27 that aldosterone increases absorption
of sodium and simultaneously increases secretion
of potassium by the renal tubular epithelial cells-
especially in the principal cells of the collecting tubules
be conserved in the extracellular fluid while increasing
A high concentration of aldosterone in the plasma
can transiently decrease the sodium loss into the urine
in the plasma is to increase the total quantity of
sodium in the extracellular fluid while decreasing the
potassium.
cause transient loss of 10 to 20 grams of sodium in the
sium is conserved tenaciously in the extracellular fluid.
Arterial Pressure but Has Only a Small Effect on Plasma Sodium
Concentration.
Although aldosterone has a potent
effect in decreasing the rate of sodium ion excretion
extracellular fluid often rises only a few milliequiva-
concentration stimulate thirst and increased water
lar fluid volume increases almost as much as the
concentration.
sodium retention occurs when excess amounts are
cellular fluid volume lasting more than 1 to 2 days
then increases kidney excretion of both salt and
pressure natriuresis and
blood pressure returns the renal output of salt and
77–3).
the kidneys as a result of pressure natriuresis and
110
2
2
4
6
8
10 12
4
14
100
400
300
200
-
-
0
Urinary sodium
excretion (mEq/day)
100
90
120
Extracellular fluid
volume (% Normal)
100
80
120
Mean arterial
pressure (mm Hg)
Time (days)
Aldosterone
arterial pressure in aldosterone “escape.” Hypertension 6 (suppl
Granger JP, Smith MJ Jr, Premen N: Role of hemodynamics and
sodium excretion returned to normal. (Drawn from data in Hall JE,
second day of infusion as arterial pressure increased and urinary
20 times normal, note the “escape” from sodium retention on the
fluid volume, and sodium excretion in dogs. Although aldosterone
Effect of aldosterone infusion on arterial pressure, extracellular
Figure 77–3
was infused at a rate that raised plasma concentrations to about
I):I-183–I-192, 1984.)
from the tubular lumen into the cell; then the sodium
equally important, are epithelial sodium channel pro-
renal tubular cells. Additional proteins, perhaps
potassium adenosine triphosphatase,
and hydrogen transport through the cell membrane.
acting together, are required for sodium, potassium,
and (2) membrane transport proteins that, all
ribosomes, it causes protein formation. The proteins
cytoplasm, where, operating in conjunction with the
Fourth, the messenger RNA diffuses back into the
one or more types of messenger RNA related to the
ing one or more specific portions of the DNA to form
where it may undergo further alterations, finally induc-
product of this complex diffuses into the nucleus,
Third, the aldosterone-receptor complex or a
terone combines with a highly specific cytoplasmic
Second, in the cytoplasm of the tubular cells, aldos-
of the tubular epithelial cells.
membranes, aldosterone diffuses readily to the interior
First, because of its lipid solubility in the cellular
following.
However, the cellular sequence of events that leads
effects of mineralocorticoids on the body, the basic
Aldosterone Action
loss of salt from the body.
chloride and water then lead to diarrhea, with further
anions and water as well. The unabsorbed sodium
poor, leading to failure to absorb chloride and other
absence of aldosterone, sodium absorption can be
prevents loss of sodium in the stools. Conversely, in the
tion by the intestines, especially in the colon, which
environments, and the effect on the salivary glands is
secretion of potassium by the ducts. The effect on the
bicarbonate ions are secreted. Aldosterone greatly
excretory ducts, is reabsorbed, whereas potassium and
much of the sodium chloride, on passing through the
that contains large quantities of sodium chloride, but
tubules. Both these glands form a primary secretion
Potassium Transport in Sweat Glands,
Aldosterone Stimulates Sodium and
cellular fluid, causing a mild degree of alkalosis.
of the cortical collecting tubules. This
Excess Aldosterone Increases Tubular Hydrogen Ion Secretion,
of potassium lead inevitably to heart failure.
becomes evident; progressively higher concentrations
normal, serious cardiac toxicity, including weakness of
above normal.When it rises to 60 to 100 per cent above
Conversely, when aldosterone is deficient, the extra-
vents transmission of normal action potentials.
muscle fiber membranes (see Chapter 5), which pre-
muscle weakness often develops. This is caused by
tration falls below about one-half normal, severe
When the potassium ion concen-
4.5 mEq/L to as low as 2 mEq/L. This condition is
concentration, sometimes from the normal value of
as occurs with some types of adrenal tumors, may
body. Therefore, excessive secretion of aldosterone,
Toxicity.
ness; Too Little Aldosterone Causes Hyperkalemia and Cardiac
Excess Aldosterone Causes Hypokalemia and Muscle Weak-
stop secreting aldosterone.
Without therapy, this usually causes death
tory shock.
dehydration and low blood volume, leading to
fluid volume. The result is severe extracellular fluid
zero, large amounts of salt are lost in the urine, not
Conversely, when aldosterone secretion becomes
person remains exposed to high levels of aldosterone.
developed hypertension, which lasts as long as the
aldosterone. In the meantime, however, the person has
rate of gain of salt and water by the body is zero, and
Thereafter, the
aldosterone escape.
Chapter 77
Adrenocortical Hormones
949
diuresis is called
balance is maintained between salt and water intake
and output by the kidneys despite continued excess
only diminishing the amount of sodium chloride in the
extracellular fluid but also decreasing the extracellular
circula-
within a few days after the adrenal glands suddenly
Excess aldosterone not only causes loss of
potassium ions from the extracellular fluid into the
urine but also stimulates transport of potassium
from the extracellular fluid into most cells of the
cause a serious decrease in the plasma potassium
called hypokalemia.
alteration of the electrical excitability of the nerve and
cellular fluid potassium ion concentration can rise far
heart contraction and development of arrhythmia,
and Causes Mild Alkalosis.
Aldosterone not only causes
potassium to be secreted into the tubules in exchange
for sodium reabsorption in the principal cells of the
renal collecting tubules but also causes secretion of
hydrogen ions in exchange for sodium in the interca-
lated cells
decreases the hydrogen ion concentration in the extra-
Salivary Glands, and Intestinal
Epithelial Cells
Aldosterone has almost the same effects on sweat
glands and salivary glands as it has on the renal
increases the reabsorption of sodium chloride and the
sweat glands is important to conserve body salt in hot
necessary to conserve salt when excessive quantities of
saliva are lost.
Aldosterone also greatly enhances sodium absorp-
Cellular Mechanism of
Although for many years we have known the overall
action of aldosterone on the tubular cells to increase
transport of sodium is still not fully understood.
to increased sodium reabsorption seems to be the
receptor protein, a protein that has a stereomolecular
configuration that allows only aldosterone or very
similar compounds to combine with it.
process of sodium and potassium transport.
formed are a mixture of (1) one or more enzymes
One of the enzymes especially increased is sodium-
which serves as
the principal part of the pump for sodium and potas-
sium exchange at the basolateral membranes of the
teins inserted into the luminal membrane of the same
tubular cells that allows rapid diffusion of sodium ions
remain considerably deranged. Furthermore, the
for utilization of proteins, carbohydrates, and fats
is far from normal. Instead, its metabolic systems
an acutely adrenalectomized animal, the animal still
Glucocorticoids
aldosterone is required, but total absence of ACTH
anterior pituitary gland, it is usually enough to permit
there is even a small amount of ACTH secreted by the
double aldosterone secretion. In the case of ACTH, if
tion, which occurs on rare occasions, can perhaps
tion are usually minor. Nevertheless, a 10 to 20 per cent
per se and of ACTH in controlling aldosterone secre-
By contrast, the effects of sodium ion concentration
fold. Note that blocking angiotensin II formation
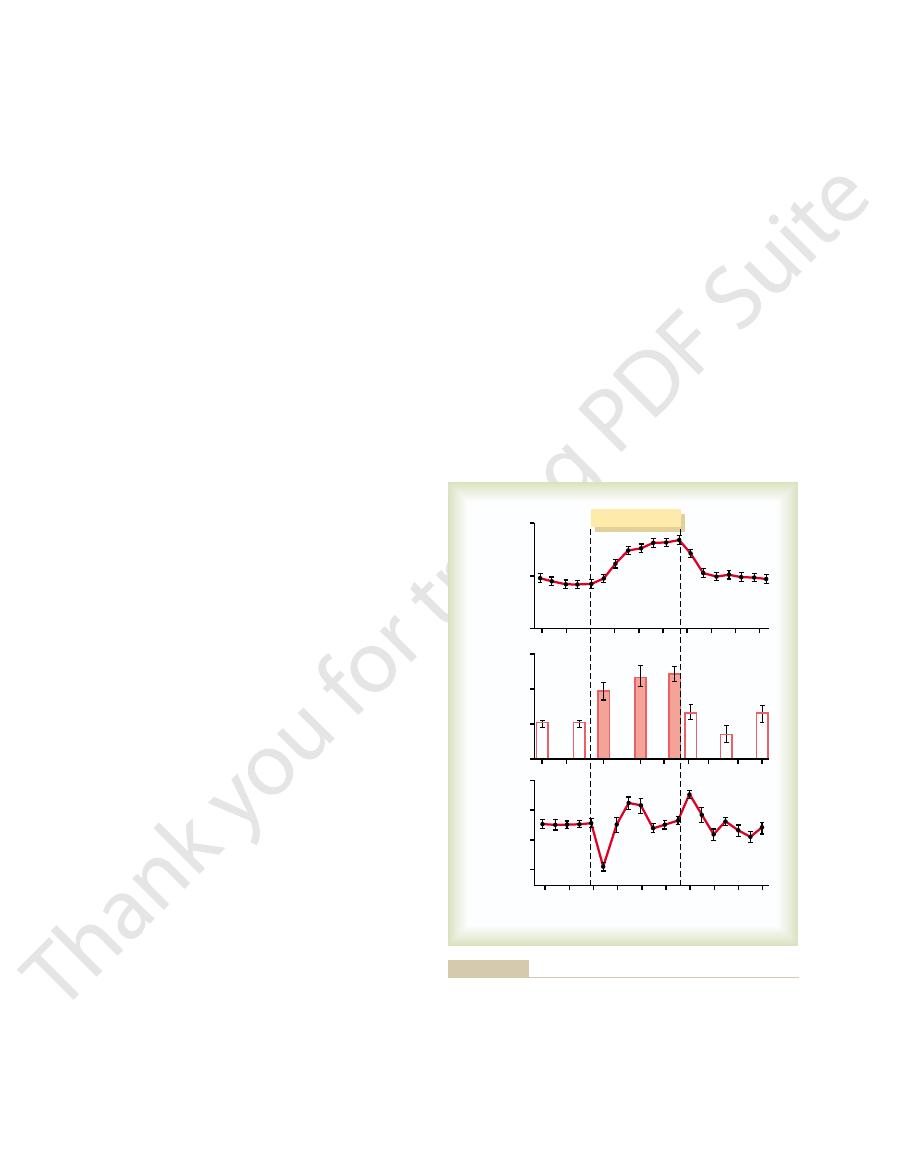
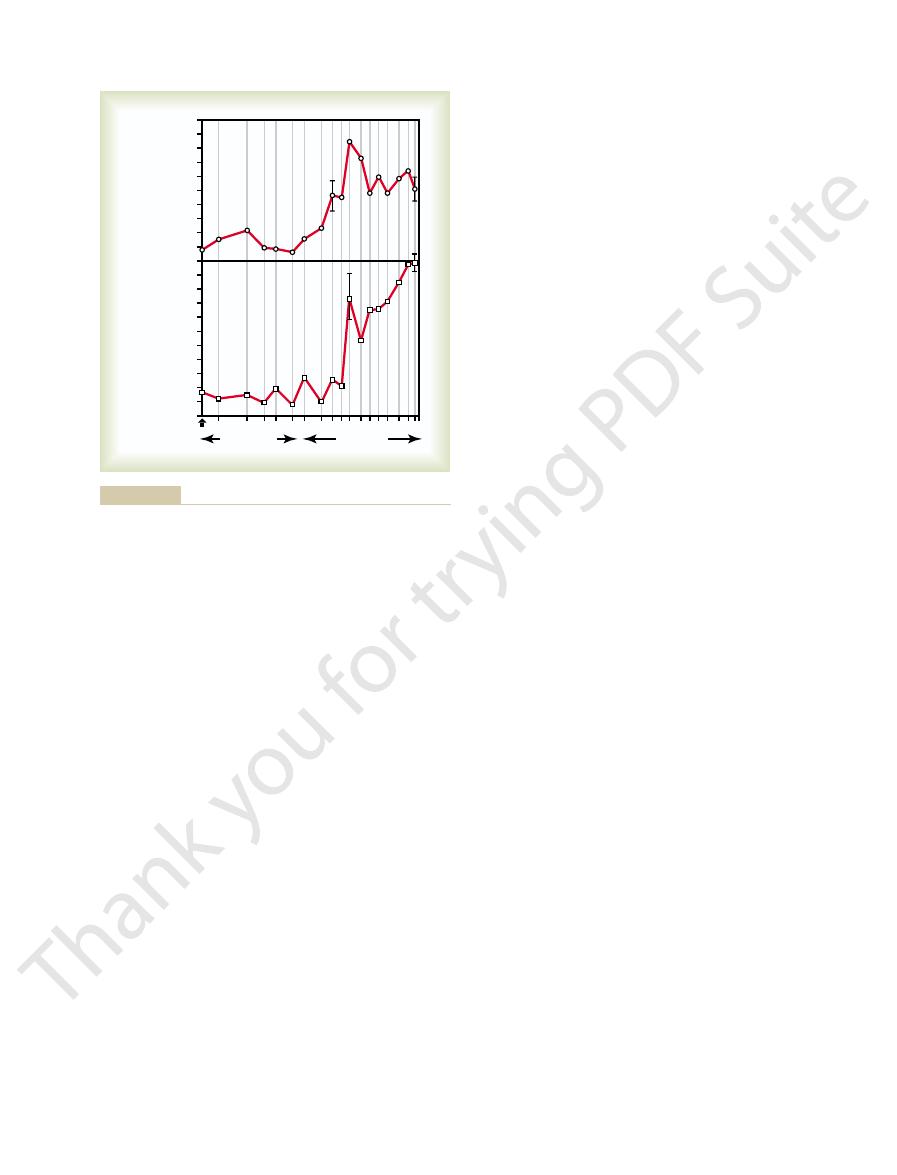
Figure 77–4 shows the effects on plasma aldosterone
functions.
maintaining life, and the reader is referred again to
These feedback control mechanisms are essential for
angiotensin system toward its normal level of activity.
volume and arterial pressure, thus returning the renin-
increase in aldosterone secretion. In turn, the aldos-
kidneys or to sodium loss, can cause a severalfold
Likewise, activation of the renin-angiotensin system,
potent in regulating aldosterone secretion. A small
Of these factors,
4. ACTH from the anterior pituitary gland is
3. Increased sodium ion concentration in the
2. Increased activity of the renin-angiotensin system
1. Increased potassium ion concentration in the
their importance, they are as follows:
regulation of aldosterone. In the probable order of
Four factors are known to play essential roles in the
ciculata and zona reticularis.
The regulation of aldosterone secretion by the zona
referred. However, it is important to list here some of
detail in Chapters 28 and 29, to which the reader is
of all these other factors. This subject is presented in
blood volume, arterial pressure, and many special
electrolyte concentrations, extracellular fluid volume,
The regulation of aldosterone secretion is so deeply
Regulation of Aldosterone Secretion
terone has not been determined, nor is the physiolog-
messenger system. However, the precise structure of
teins. In other cell types, aldosterone has been shown
less than two minutes, a time period that is far too
For example, aldosterone has been shown to increase
that are coupled to second messenger systems, similar
These nongenomic actions are believed to be medi-
in a few seconds or minutes.
teins, but also rapid
effects that have a latency of 60 to 90 minutes and
aldosterone, elicit not only slowly developing
Recent studies suggest that many steroids, including
of Aldosterone and Other
Possible Nongenomic Actions
several hours.
increase; the effect reaches maximum only after
RNA appears in the cells, and about 45 minutes is
transport. About 30 minutes is required before new
on sodium transport; rather, this effect must await the
Thus, aldosterone does not have an immediate effect
950
Unit XIV
Endocrinology and Reproduction
is pumped the rest of the way by the sodium-potassium
pump located in the basolateral membranes of the cell.
sequence of events that leads to the formation of the
specific intracellular substances required for sodium
required before the rate of sodium transport begins to
Steroid Hormones
genomic
require gene transcription and synthesis of new pro-
nongenomic effects that take place
ated by binding of steroids to cell membrane receptors
to those used for peptide hormone signal transduction.
formation of cAMP in vascular smooth muscle cells
and in epithelial cells of the renal collecting tubules in
short for gene transcription and synthesis of new pro-
to rapidly stimulate the phosphatidylinositol second
receptors responsible for the rapid effects of aldos-
ical significance of these nongenomic actions of
steroids well understood.
intertwined with the regulation of extracellular fluid
aspects of renal function that it is difficult to discuss
the regulation of aldosterone secretion independently
the more important points of aldosterone secretion
control.
glomerulosa cells is almost entirely independent of the
regulation of cortisol and androgens by the zona fas-
extracellular fluid greatly increases aldosterone
secretion.
(increased levels of angiotensin II) also greatly
increases aldosterone secretion.
extracellular fluid very slightly decreases
aldosterone secretion.
necessary for aldosterone secretion but has little
effect in controlling the rate of secretion.
potassium ion concentration
and the renin-angiotensin system are by far the most
percentage increase in potassium concentration can
cause a severalfold increase in aldosterone secretion.
usually in response to diminished blood flow to the
terone acts on the kidneys (1) to help them excrete the
excess potassium ions and (2) to increase the blood
Chapters 27 and 29 for a full understanding of their
concentration caused by blocking the formation of
angiotensin II with an angiotensin-converting enzyme
inhibitor after several weeks of a low-sodium diet that
increases plasma aldosterone concentration several-
markedly decreases plasma aldosterone concentration
without significantly changing cortisol concentration;
this indicates the important role of angiotensin II in
stimulating aldosterone secretion when sodium intake
and extracellular fluid volume are reduced.
decrease in extracellular fluid sodium ion concentra-
the adrenal glands to secrete whatever amount of
can significantly reduce aldosterone secretion.
Functions of the
Even though mineralocorticoids can save the life of
adrenal diabetes.
The increase in blood glucose concentration is occa-
hormone.
insulin’s actions on the tissues. In this way, excess
ticoids to mobilize lipids from fat depots, may impair
levels of fatty acids, caused by the effect of glucocor-
and utilization. One possible explanation is that high
tissues, especially skeletal muscle and adipose tissue,
For reasons that are not entirely clear, high levels
plasma glucose as they are under normal conditions.
insulin, however, are not as effective in maintaining
secretion of insulin. The increased plasma levels of
rise. The rise in blood glucose in turn stimulates
by the cells.
NADH must be oxidized to allow glycolysis, this effect
. Because
dinucleotide (NADH) to form NAD
delays the rate of glucose utilization. A suggested
into the cells and its final degradation, cortisol directly
decrease is unknown, most physiologists believe that
by most cells in the body. Although the cause of this
glucose in times of need, such as between meals.
mones, such as epinephrine and glucagon, to mobilize
This effect of cortisol allows other glycolytic hor-
marked increase in glycogen storage in the liver cells.
of glucose.
result, more amino acids become available in the
As a
the extrahepatic tissues mainly from muscle.
required for gluconeogenesis.
RNAs that in turn lead to the array of enzymes
renal tubular cells, with formation of messenger
activate DNA transcription in the liver cell nuclei
This
amino acids into glucose in the liver cells.
This results mainly from two effects of cortisol.
some other substances) by the liver, often increasing
Effects of Cortisol on
corticosterone.
addition to this, a small but significant amount of glu-
hydrocortisone.
sections.
eralocorticoids. They are explained in the following
tract infections can lead to death. Therefore, the glu-
mental stress, and minor illnesses such as respiratory
Chapter 77
Adrenocortical Hormones
951
animal cannot resist different types of physical or even
cocorticoids have functions just as important to the
long-continued life of the animal as those of the min-
At least 95 per cent of the glucocorticoid activity of
the adrenocortical secretions results from the secre-
tion of cortisol, known also as
In
cocorticoid activity is provided by
Carbohydrate Metabolism
Stimulation of Gluconeogenesis.
By far the best-known
metabolic effect of cortisol and other glucocorticoids
on metabolism is their ability to stimulate gluconeo-
genesis (formation of carbohydrate from proteins and
the rate of gluconeogenesis as much as 6- to 10-fold.
1. Cortisol increases the enzymes required to convert
results from the effect of the glucocorticoids to
in the same way that aldosterone functions in the
2. Cortisol causes mobilization of amino acids from
plasma to enter into the gluconeogenesis process
of the liver and thereby to promote the formation
One of the effects of increased gluconeogenesis is a
Decreased Glucose Utilization by Cells.
Cortisol also causes
a moderate decrease in the rate of glucose utilization
somewhere between the point of entry of glucose
mechanism is based on the observation that glucocor-
ticoids depress the oxidation of nicotinamide-adenine
+
could account for the diminished utilization of glucose
Elevated Blood Glucose Concentration and “Adrenal Diabetes.”
Both the increased rate of gluconeogenesis and the
moderate reduction in the rate of glucose utilization
by the cells cause the blood glucose concentrations to
of glucocorticoid reduce the sensitivity of many
to the stimulatory effects of insulin on glucose uptake
secretion of glucocorticoids may produce disturbances
of carbohydrate metabolism very similar to those
found in patients with excess levels of growth
sionally great enough (50 per cent or more above
normal) that the condition is called
Administration of insulin lowers the blood glucose
concentration only a moderate amount in adrenal
diabetes-not nearly as much as it does in pancreatic
Control
ACE inhibitor
0.0
3.0
2.0
1.0
+
Ang II infusion
ACE
inhibitor
Plasma cortisol
(
m
g/100 ml)
20
50
40
30
Plasma aldosterone
(n
g/100 ml)
Coleman TG: Chronic blockade of angiotensin II formation during
tion. (Drawn from data in Hall JE, Guyton AC, Smith MJ Jr,
Ang II in stimulating aldosterone secretion during sodium deple-
with little effect on cortisol, demonstrating the important role of
ing Ang II formation reduced plasma aldosterone concentration
restore plasma Ang II levels after ACE inhibition. Note that block-
converting enzyme (ACE) inhibitor for 7 days to block formation
Effects of treating sodium-depleted dogs with an angiotensin-
Figure 77–4
of angiotensin II (Ang II) and of infusing exogenous Ang II to
sodium deprivation. Am J Physiol 237:F424, 1979.)
cortical secretion of cortisol. This is demonstrated
in ACTH secretion by the anterior pituitary gland,
genic, causes an immediate and marked increase
Almost any type of stress, whether physical or neuro-
Cortisol is Important in Resisting
results from excess stimulation of food intake, with fat
unknown, it has been suggested that this obesity
and a rounded “moon face.” Although the cause is
head regions of the body, giving a buffalo-like torso
obesity, with excess deposition of fat in the chest and
mobilization from adipose tissue, many people with
in insulin, as we discuss in Chapter 78. Nevertheless,
tisol mechanism, however, requires several hours to
acids in times of starvation or other stresses. This cor-
cells, helps shift the metabolic systems of the cells from
The increased mobilization of fats by cortisol, com-
the fat cells begin to release fatty acids.
nance of triglycerides in these cells, and in its absence
glucose, is required for both deposition and mainte-
-glycerophosphate, which is derived from
diminished transport of glucose into the fat cells.
However, part of the effect probably results from
The mechanism by which cortisol promotes fatty
cells.
lization for energy. Cortisol also seems to have a direct
fatty acids in the plasma, which also increases their uti-
adipose tissue. This increases the concentration of free
muscle, it promotes mobilization of fatty acids from
Effects of Cortisol on Fat Metabolism
the hepatic effects.
gluconeogenesis. Thus, it is possible that many of the
version of amino acids to glucose-that is, enhanced
plasma proteins by the liver, and (4) increased con-
synthesis in the liver, (3) increased formation of
of amino acids by the liver, (2) increased protein
The increased plasma concentration of amino acids
cortisol mobilizes amino acids from the nonhep-
fore,
increase the plasma amino acid concentration. There-
existing proteins, and these diffuse out of the cells to
thesis of protein.Yet, catabolism of proteins in the cells
The decreased transport of amino acids into extra-
cells.
Acids into Extrahepatic Cells, and Enhanced Transport into
Increased Blood Amino Acids, Diminished Transport of Amino
liver enzymes required for protein synthesis.
occurs elsewhere in the body. It is believed that this
then released into the blood) are also increased. These
the liver proteins become enhanced. Furthermore, the
tally with the reduced proteins elsewhere in the body,
rise from the squatting position. And the immunity
In the presence of great excesses of cortisol, the
lymphoid tissue.
in many extrahepatic tissues, especially in muscle and
formation of RNA and subsequent protein synthesis
the major cause, because cortisol also depresses the
hepatic tissues, as discussed later; this probably is not
of protein already in the cells. Both these effects may
cells except those of the liver. This is caused by both
Effects of Cortisol on
952
Unit XIV
Endocrinology and Reproduction
diabetes-because the tissues are resistant to the effects
of insulin.
Protein Metabolism
Reduction in Cellular Protein.
One of the principal effects
of cortisol on the metabolic systems of the body is
reduction of the protein stores in essentially all body
decreased protein synthesis and increased catabolism
result from decreased amino acid transport into extra-
muscles can become so weak that the person cannot
functions of the lymphoid tissue can be decreased to a
small fraction of normal.
Cortisol Increases Liver and Plasma Proteins.
Coinciden-
plasma proteins (which are produced by the liver and
increases are exceptions to the protein depletion that
difference results from a possible effect of cortisol to
enhance amino acid transport into liver cells (but
not into most other cells) and to enhance the
Hepatic Cells.
Studies in isolated tissues have demon-
strated that cortisol depresses amino acid transport
into muscle cells and perhaps into other extrahepatic
hepatic cells decreases their intracellular amino acid
concentrations and consequently decreases the syn-
continues to release amino acids from the already
atic tissues and in doing so diminishes the tissue stores
of protein.
and enhanced transport of amino acids into the
hepatic cells by cortisol could also account for
enhanced utilization of amino acids by the liver to
cause such effects as (1) increased rate of deamination
effects of cortisol on the metabolic systems of the body
result mainly from this ability of cortisol to mobilize
amino acids from the peripheral tissues while at the
same time increasing the liver enzymes required for
Mobilization of Fatty Acids.
In much the same manner
that cortisol promotes amino acid mobilization from
effect to enhance the oxidation of fatty acids in the
acid mobilization is not completely understood.
Recall that
a
bined with increased oxidation of fatty acids in the
utilization of glucose for energy to utilization of fatty
become fully developed-not nearly so rapid or so pow-
erful an effect as a similar shift elicited by a decrease
the increased use of fatty acids for metabolic energy is
an important factor for long-term conservation of
body glucose and glycogen.
Obesity Caused by Excess Cortisol.
Despite the fact that
cortisol can cause a moderate degree of fatty acid
excess cortisol secretion develop a peculiar type of
being generated in some tissues of the body more
rapidly than it is mobilized and oxidized.
Stress and Inflammation
followed within minutes by greatly increased adreno-
decreased quantity.
stored in the lysosomes, are released in greatly
cells to cause inflammation, which are mainly
lysosomes to rupture. Therefore, most of the
effects, because it is much more difficult than
This
Cortisol stabilizes the lysosomal membranes.
ing Lysosomes and by Other Effects.
Cortisol Prevents the Development of Inflammation by Stabiliz-
explained further as follows.
increased rapidity of healing. These effects are
even begins, or (2) if inflammation has already begun,
injected into a person, the cortisol has two basic
When large amounts of cortisol are secreted or
healing process.
the area by leukocytes; and (5) after days or weeks,
ability, followed by clotting of the tissue fluid, thus
some of the released products from the tissues, an
enzymes, prostaglandins, and leukotrienes; (2) an
chemicals such as histamine, bradykinin, proteolytic
There are five main stages of inflammation: (1)
process, discussed in more detail in Chapter 33.
once it has begun. Before attempting to explain the
aging than the trauma or disease itself. The adminis-
rheumatoid arthritis, the inflammation is more dam-
become “inflamed.” In some conditions, such as in
with bacteria, or in other ways, they almost always
When tissues are damaged by trauma, by infection
of Cortisol
Anti-inflammatory Effects of High Levels
tial to life.
released. This preferential effect of cortisol in
neurons, until almost all other proteins have been
the basic functional proteins of the cells, such as
But all this is mainly supposition. It is supported
of new cells.
pyrimidines, and creatine phosphate, which are neces-
other essential intracellular substances such as purines,
Also, the amino acids are perhaps used to synthesize
new proteins that are essential to the lives of the cells.
Indeed, it has been shown in a few instances that
ing glucose, needed by the different tissues of the body.
energy and for synthesis of other compounds, includ-
stores, making them immediately available both for
why this is of significant benefit to the animal. One
increases greatly in stressful situations, we are not sure
8. Almost any debilitating disease
7. Restraining an animal so that it cannot move
6. Injection of necrotizing substances beneath the
5. Surgery
4. Injection of norepinephrine and other
3. Intense heat or cold
2. Infection
1. Trauma of almost any type
fracture of two leg bones.
dramatically by the experiment shown in Figure 77–5,
Chapter 77
Adrenocortical Hormones
953
in which corticosteroid formation and secretion
increased sixfold in a rat within 4 to 20 minutes after
Some of the different types of stress that increase
cortisol release are the following:
sympathomimetic drugs
skin
Even though we know that cortisol secretion often
possibility is that the glucocorticoids cause rapid mobi-
lization of amino acids and fats from their cellular
damaged tissues that are momentarily depleted of pro-
teins can use the newly available amino acids to form
sary for maintenance of cellular life and reproduction
only by the fact that cortisol usually does not mobilize
the muscle contractile proteins and the proteins of
mobilizing labile proteins could make amino acids
available to needy cells to synthesize substances essen-
tration of large amounts of cortisol can usually block
this inflammation or even reverse many of its effects
way in which cortisol functions to block inflammation,
let us review the basic steps in the inflammation
release from the damaged tissue cells of chemical
substances that activate the inflammation process-
increase in blood flow in the inflamed area caused by
effect called erythema; (3) leakage of large quantities
of almost pure plasma out of the capillaries into the
damaged areas because of increased capillary perme-
causing a nonpitting type of edema; (4) infiltration of
ingrowth of fibrous tissue that often helps in the
anti-
inflammatory effects: (1) it can block the early stages
of the inflammation process before inflammation
it causes rapid resolution of the inflammation and
Cortisol has the fol-
lowing effects in preventing inflammation:
1.
is one of its most important anti-inflammatory
normal for the membranes of the intracellular
proteolytic enzymes that are released by damaged
15
30
45 60 90 2
3 4 5 6 8 101215 20 25 30
Seconds
Minutes
-
0
45
40
35
30
25
20
15
10
5
55
50
45
40
35
30
25
20
15
10
5
Plasma corticosterone
concentration
(mg/100 ml)
Adrenal cortisone
concentration
(mg/g)
Dear, and Lipscomb.)
terone is secreted in place of cortisol.) (Courtesy Drs. Guillemin,
fracture of the tibia and fibula at time zero. (In the rat, corticos-
Rapid reaction of the adrenal cortex of a rat to stress caused by
Figure 77–5

that mediate their multiple physiologic effects. Thus,
many genes to alter synthesis of mRNA for the proteins
coid response elements.
factors,
scription. Other proteins in the cell, called
coid response elements,
specific regulatory DNA sequences, called
cortisol binds with its protein receptor in the cytoplasm,
diffuse through the cell membrane. Once inside the cell,
cells. Because cortisol is lipid soluble, it can easily
Cortisol, like other steroid hormones, exerts its effects
Cortisol Action
Cellular Mechanism of
no cortisol, anemia often results.
results, and conversely, when the adrenal glands secrete
secreted by the adrenal glands, polycythemia often
by mechanisms that are unclear. When excess cortisol is
transplanted hearts, kidneys, and other tissues.
been arrested. Conversely, this ability of cortisol and
that would otherwise not be lethal, such as fulminating
invaders of the body is decreased. This occasionally can
As a result, the level of immunity for almost all foreign
of both T cells and antibodies from the lymphoid tissue.
throughout the body, which in turn decreases the output
Likewise, the administration of large doses of cortisol
phocytopenia or eosinopenia is an important diagnostic
marked within a few hours. Indeed, a finding of lym-
phocytes in the blood; this effect begins within a few
anaphylaxis, which otherwise kills many people, as
instance, cortisol effectively prevents shock or death in
release of inflammatory products, can be lifesaving. For
effects of allergic reactions, administration of cortisol,
However, because the inflammatory response is respon-
secondary effects of the allergic reaction still occur.
body is not affected by cortisol, and even some of the
The basic allergic reaction between antigen and anti-
Cortisol Blocks the Inflammatory Response to Allergic Reactions.
Other Effects of Cortisol
often be a lifesaving measure.
ing effects of the inflammatory response, this alone can
basic disease condition, merely preventing the damag-
the inflammation begins to subside within 24 hours.
tered to patients with these diseases, almost invariably
When cortisol or other glucocorticoids are adminis-
disease.
characterized by severe local inflammation, and the
and acute glomerulonephritis. All these diseases are
eases, such as rheumatoid arthritis, rheumatic fever,
anti-inflammatory effect occurs, this effect of cortisol
products.
lular energy; or perhaps it depends on some effect of
able in critical metabolic systems; perhaps it results
the damaged tissues; perhaps it results from the
cortisol are secreted. Perhaps this results from the
undefined, factors that allow the body to resist many
enhanced. This probably results from the same, mainly
inflammation. But in addition, the rate of healing is
within hours to a few days. The immediate effect is to
inflammation has become well established, the admin-
membranes and other effects of cortisol is unclear.
ing all aspects of the inflammatory process. How much
Thus, cortisol has an almost global effect in reduc-
hypothalamic temperature control system. The
cells,
process.
turn, reduced amounts of T cells and antibodies
The T lymphocytes are especially suppressed. In
lymphocyte reproduction to decrease markedly.
Cortisol suppresses the immune system, causing
permeability, and mobility of white blood cells.
otherwise would increase vasodilation, capillary
These effects probably result from
damaged cells.
prevents loss of plasma into the tissues.
reduced release of proteolytic enzymes. This
capillaries,
954
Unit XIV
Endocrinology and Reproduction
2. Cortisol decreases the permeability of the
probably as a secondary effect of the
3. Cortisol decreases both migration of white blood
cells into the inflamed area and phagocytosis of the
the fact that cortisol diminishes the formation
of prostaglandins and leukotrienes that
4.
in the inflamed area lessen the tissue reactions
that would otherwise promote the inflammation
5. Cortisol attenuates fever mainly because it reduces
the release of interleukin-1 from the white blood
which is one of the principal excitants to the
decreased temperature in turn reduces the degree
of vasodilation.
of this results from the simple effect of cortisol in
stabilizing lysosomal and cell membranes versus its
effect to reduce the formation of prostaglandins and
leukotrienes from arachidonic acid in damaged cell
Cortisol Causes Resolution of Inflammation.
Even after
istration of cortisol can often reduce inflammation
block most of the factors that are promoting the
other types of physical stress when large quantities of
mobilization of amino acids and use of these to repair
increased glucogenesis that makes extra glucose avail-
from increased amounts of fatty acids available for cel-
cortisol for inactivating or removing inflammatory
Regardless of the precise mechanisms by which the
plays a major role in combating certain types of dis-
harmful effects on the body are caused mainly by
the inflammation itself and not by other aspects of the
And even though the cortisol does not correct the
sible for many of the serious and sometimes lethal
followed by its effect in reducing inflammation and the
explained in Chapter 34.
Effect on Blood Cells and on Immunity in Infectious Diseases.
Cortisol decreases the number of eosinophils and lym-
minutes after the injection of cortisol and becomes
criterion for overproduction of cortisol by the adrenal
gland.
causes significant atrophy of all the lymphoid tissue
lead to fulminating infection and death from diseases
tuberculosis in a person whose disease had previously
other glucocorticoids to suppress immunity makes them
useful drugs in preventing immunological rejection of
Cortisol increases the production of red blood cells
by first interacting with intracellular receptors in target
and the hormone-receptor complex then interacts with
glucocorti-
to induce or repress gene tran-
transcription
are also necessary for the hormone-receptor
complex to interact appropriately with the glucocorti-
Glucocorticoids increase or decrease transcription of
most of the metabolic effects of cortisol are not
at times when the body is not experiencing stress.
There is also direct feedback of the cortisol to both
the damaging nature of the stressful state.
release of cortisol, and the cortisol in turn initiates a
tation of the hypothalamus by different types of stress.
cortisol secretion. The key to this control is the exci-
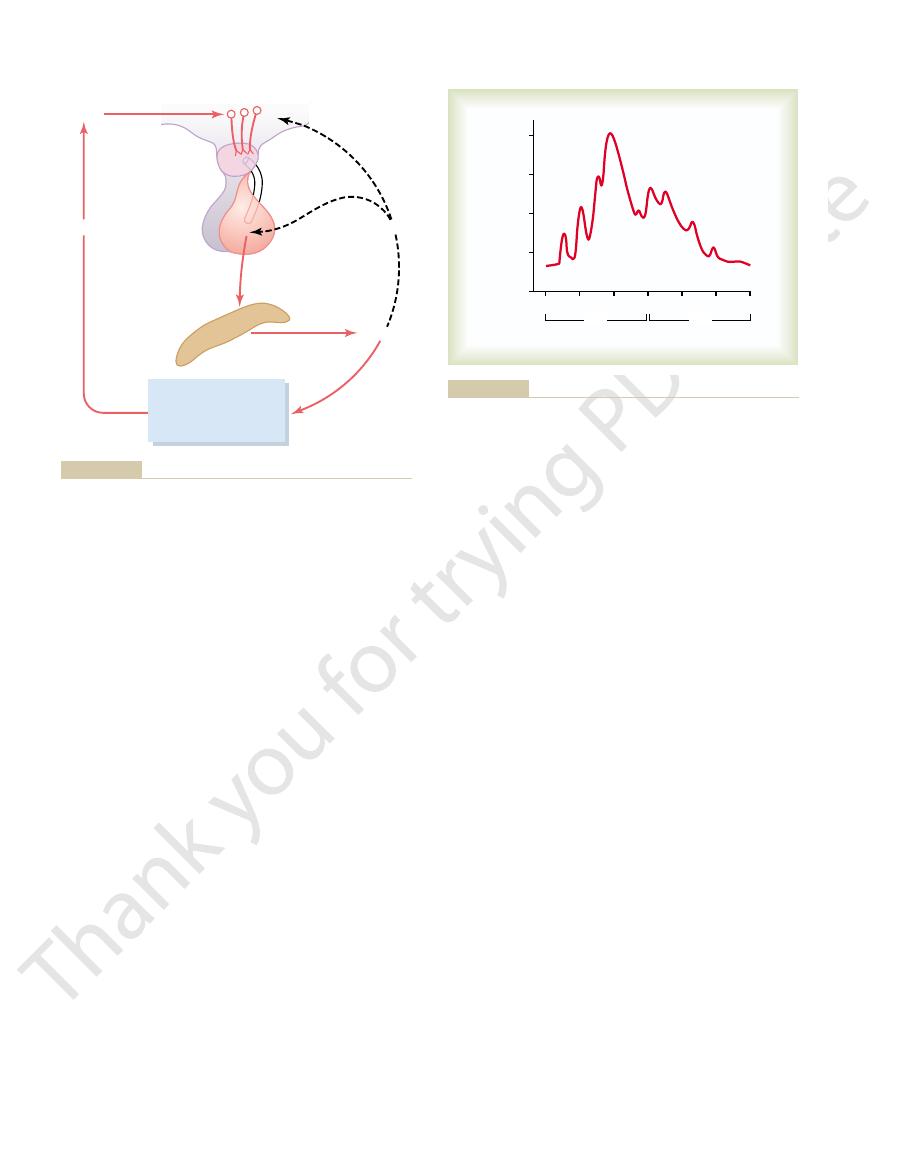
Figure 77–6 shows the overall system for control of
Summary of the Cortisol Control System
feedbacks automatically reduce the ACTH toward
the cortisol concentration becomes too great, the
the plasma concentration of cortisol. That is, whenever
of ACTH. Both of these feedbacks help regulate
Anterior Pituitary to Decrease ACTH Secretion.
Inhibitory Effect of Cortisol on the Hypothalamus and on the
hypothalamus.
region of the amygdala and hippocampus, both of
increased activity in the limbic system, especially in the
ACTH secretion. This is believed to result from
secreted into the hypophysial portal system. Within
hypothalamus, as shown in Figure 77–6. Here CRF is
responses after trauma shown in Figure 77–5.
tion as much as 20-fold. This effect was demonstrated
quently cortisol as well, often increasing cortisol secre-
to greatly enhanced secretion of ACTH and conse-
As pointed out earlier in the chapter, almost any type
Adrenocortical Secretion
Physiologic Stress Increases ACTH and
and zona reticularis, where cortisol and the androgens
adrenocortical cells, especially in the zona fasciculata
cortex by ACTH not only increases secretory activity
to be formed. Long-term stimulation of the adrenal
adrenocortical hormones, which explains why ACTH
initial conversion is the “rate-limiting” step for all the
This
initial conversion of cholesterol to pregnenolone.
protein kinase A,
The most important of all the ACTH-stimulated
This is another example of cAMP as a
that cause formation of the adrenocortical hormones.
The cAMP in turn activates the intracellular enzymes
plasm, reaching its maximal effect in about 3 minutes.
in the cell cyto-
in the cell membrane. This
principal effect of ACTH on the adrenocortical cells is
The
regions of the brain, including the hypothalamus, and
most conditions that cause high ACTH secretory rates
quantities of ACTH in the absence of CRF. Instead,
The anterior pituitary gland can secrete only minute
tricular nucleus of the hypothalamus. This nucleus in
posed of 41 amino acids. The cell bodies of the neurons
it induces ACTH secretion. CRF is a peptide com-
and then carried to the anterior pituitary gland, where
(CRF). It is secreted into the
also controls ACTH secretion. This is called
from the hypothalamus, an important releasing factor
total molecule.
chain length of 24 amino acids, has all the effects of the
polypeptide, a digested product of ACTH having a
tide, having a chain length of 39 amino acids. A smaller
form from the anterior pituitary. It is a large polypep-
ACTH has been isolated in pure
Chemistry of ACTH.
of adrenal androgens.
pituitary gland. This hormone, also called
almost entirely by ACTH secreted by the anterior
cortisol. Instead, secretion of cortisol is controlled
on the adrenocortical cells, almost no stimuli have
secretion by the zona glomerulosa, which is controlled
from the Pituitary Gland
by Adrenocorticotropic Hormone
Regulation of Cortisol Secretion
port that may contribute to their therapeutic benefits.
especially at high concentrations, may also have some
develop. Recent evidence suggests that glucocorticoids,
be synthesized, and up to several hours or days to fully
Chapter 77
Adrenocortical Hormones
955
immediate but require 45 to 60 minutes for proteins to
rapid nongenomic effects on cell membrane ion trans-
ACTH Stimulates Cortisol Secretion.
Unlike aldosterone
mainly by potassium and angiotensin acting directly
direct control effects on the adrenal cells that secrete
corticotropin
or adrenocorticotropin, also enhances the production
ACTH Secretion Is Controlled by Corticotropin-Releasing Factor
from the Hypothalamus.
In the same way that other pitu-
itary hormones are controlled by releasing factors
corti-
cotropin-releasing factor
primary capillary plexus of the hypophysial portal
system in the median eminence of the hypothalamus
that secrete CRF are located mainly in the paraven-
turn receives many nervous connections from the
limbic system and lower brain stem.
initiate this secretion by signals that begin in the basal
are then transmitted by CRF to the anterior pituitary
gland.
ACTH Activates Adrenocortical Cells to Produce Steroids by
Increasing Cyclic Adenosine Monophosphate (cAMP).
to activate adenylyl cyclase
then induces the formation of cAMP
second messen-
ger signal system.
steps for controlling adrenocortical secretion is acti-
vation of the enzyme
which causes
normally is necessary for any adrenocortical hormones
but also causes hypertrophy and proliferation of the
are secreted.
of physical or mental stress can lead within minutes
by the rapid and strong adrenocortical secretory
Pain stimuli caused by physical stress or tissue
damage are transmitted first upward through the brain
stem and eventually to the median eminence of the
minutes the entire control sequence leads to large
quantities of cortisol in the blood.
Mental stress can cause an equally rapid increase in
which then transmit signals to the posterior medial
Cortisol has
direct negative feedback effects on (1) the hypothala-
mus to decrease the formation of CRF and (2) the
anterior pituitary gland to decrease the formation
a normal control level.
Stress stimuli activate the entire system to cause rapid
series of metabolic effects directed toward relieving
the hypothalamus and the anterior pituitary gland to
decrease the concentration of cortisol in the plasma
pituitary lobes. This lobe secretes an especially large
developed, lying between the anterior and posterior
the pituitary gland, called the
In some lower animals, an intermediate “lobe” of
genetically dark skins than in light-skinned people.
skin. The effect is much greater in people who have
it to the epidermis. Injection of MSH into a person
dermis and epidermis of the skin, MSH stimulates
-MSH, but not ACTH. As
-, and
hypothalamus, the expression of PC2 leads to the
-lipotropin. In the
-endorphin, and
peptide, ACTH,
ing in the production of N-terminal peptide, joining
(PC1), but not PC2, result-
the tissue. Thus, pituitary corticotroph cells express
form a series of smaller peptides. The precise type
tissue. In all of these cell types, POMC is processed to
the hypothalamus, cells of the dermis, and lymphoid
pituitary, POMC neurons in the arcuate nucleus of
tissues, including the corticotroph cells of the anterior
The POMC gene is actively transcribed in several
disease, formation of some of the other POMC-
tion of ACTH is high, as may occur in Addison’s
effect on the human body, but when the rate of secre-
conditions, none of these hormones is secreted in
, and a few others (Figure 77–8)
as several other peptides, including
which is the precursor of ACTH as well
RNA molecule that causes ACTH synthesis initially
ical structures are secreted simultaneously. The reason
gland, several other hormones that have similar chem-
When ACTH is secreted by the anterior pituitary
Hormone, Lipotropin, and Endorphin
Synthesis and Secretion of ACTH in
measurements are made.
expressed in terms of the time in the cycle at which the
changes correspondingly. Therefore, measurements of
When a person changes daily sleeping habits, the cycle
results from a 24-hour cyclical alteration in the signals
g/dl around midnight. This effect
77–7; the plasma cortisol level ranges between a high of
morning but low in the late evening, as shown in Figure
rates of CRF, ACTH, and cortisol are high in the early
The secretory
times of chronic stress.
day (Figure 77–7) or prolonged cortisol secretion in
feedback of cortisol, causing either periodic exacerba-
However, the stress stimuli are the prepotent ones;
956
Unit XIV
Endocrinology and Reproduction
they can always break through this direct inhibitory
tions of cortisol secretion at multiple times during the
Circadian Rhythm of Glucocorticoid Secretion.
about 20
mg/dl an hour before arising in the morning
and a low of about 5
m
from the hypothalamus that cause cortisol secretion.
blood cortisol levels are meaningful only when
Association with Melanocyte-Stimulating
for this is that the gene that is transcribed to form the
causes the formation of a considerably larger protein,
a preprohormone called proopiomelanocortin
(POMC),
melanocyte-
stimulating hormone (MSH),
b-lipotropin, b-endor-
phin
. Under normal
enough quantity by the pituitary to have a significant
derived hormones may also be increased.
of POMC-derived products from a particular tissue
depends on the type of processing enzymes present in
prohormone convertase 1
b
b
production of
a-, b
g
discussed in Chapter 71,
a-MSH formed by neurons of
the hypothalamus plays a major role in appetite
regulation.
In melanocytes located in abundance between the
formation of the black pigment melanin and disperses
over 8 to 10 days can greatly increase darkening of the
pars intermedia, is highly
Portal
vessel
(CRF)
1 Gluconeogenesis
2 Protein mobilization
3 Fat mobilization
4 Stabilizes lysosomes
Inhibits
Cortisol
ACTH
Adrenal
cortex
Relieves
Stress
Excites
Hypothalamus
Median
eminence
adrenocorticotropic hormone; CRF, corticotropin-releasing factor.
Mechanism for regulation of glucocorticoid secretion. ACTH,
Figure 77–6
AM
PM
12:00 4:00
8:00 12:00 4:00
8:00 12:00
0
20
15
10
5
Cortisol concentration
(
m
g/dl)
Noon
or so after awaking in the morning.
oscillations in secretion as well as a daily secretory surge an hour
Typical pattern of cortisol concentration during the day. Note the
Figure 77–7
many other metabolic functions of the body. This
proteins and fats from the tissues, thereby depressing
quantities of glucose by gluconeogenesis. Furthermore,
it impossible for a person with Addison’s disease to
Glucocorticoid Deficiency.
in shock, death usually occurring in the untreated
markedly, cardiac output decreases, and the patient dies
volume falls, red blood cell concentration rises
As the extracellular fluid becomes depleted, plasma
volume. Furthermore, hyponatremia, hyperkalemia, and
and water to be lost into urine in great profusion. The
tion and consequently allows sodium ions, chloride ions,
Mineralocorticoid Deficiency.
turbances in Addison’s disease are as follows.
or invasion of the adrenal cortices by cancer. The dis-
tices. Adrenal gland hypofunction is also frequently
the adrenal cortices. In about 80 per cent of the cases,
cortices to produce adrenocortical hormones, and this
Addison’s disease results from failure of the adrenal
Adrenocortical Secretion
Abnormalities of
androgenic activity. The physiologic effects of andro-
hormone, which probably accounts for much of their
gens are converted to testosterone, the primary male sex
In extra-adrenal tissues, some of the adrenal andro-
results from the action of these hormones.
before puberty but also throughout life. Much of the
androgens also exert mild effects in the female, not only
hood secretion of adrenal androgens. The adrenal
effects in humans. It is possible that part of the early
Normally, the adrenal androgens have only weak
in minute quantities.
estrogens, which are female sex hormones, are secreted
cussed more fully in Chapter 83. Also, progesterone and
the adrenal cortex, especially during fetal life, as dis-
Adrenal Androgens
ACTH normally is more important than MSH in
small, whereas those of ACTH are large, it is likely that
MSH. Furthermore, because the quantities of pure
about 1/30 as much melanocyte-stimulating effect as
ACTH, because it contains an MSH sequence, has
winter.
instance, some arctic animals develop darkened fur in
or in response to other environmental factors. For
amount of MSH. Furthermore, this secretion is inde-
Chapter 77
Adrenocortical Hormones
957
pendently controlled by the hypothalamus in response
to the amount of light to which the animal is exposed
the summer and yet have entirely white fur in the
MSH secreted in the human being are extremely
determining the amount of melanin in the skin.
Several moderately active male sex hormones called
adrenal androgens (the most important of which is
dehydroepiandrosterone) are continually secreted by
development of the male sex organs results from child-
growth of the pubic and axillary hair in the female
gens are discussed in Chapter 80 in relation to male
sexual function.
Hypoadrenalism-Addison’s Disease
in turn is most frequently caused by primary atrophy of
the atrophy is caused by autoimmunity against the cor-
caused by tuberculous destruction of the adrenal glands
Lack of aldosterone secre-
tion greatly decreases renal tubular sodium reabsorp-
net result is a greatly decreased extracellular fluid
mild acidosis develop because of failure of potassium
and hydrogen ions to be secreted in exchange for
sodium reabsorption.
patient 4 days to 2 weeks after cessation of mineralo-
corticoid secretion.
Loss of cortisol secretion makes
maintain normal blood glucose concentration between
meals because he or she cannot synthesize significant
lack of cortisol reduces the mobilization of both
N-Terminal protein
Proopiomelanocortin
COOH
NH
2
ACTH
Joining
protein
g
-MSH
a
-MSH
b
-MSH
g
-Lipotropin
CLIP
PCI
PC2
b
-Lipotropin
b
-Endorphin
CLIP, corticotropin-like intermedi-
hormone (MSH), but not ACTH.
mus leads to the production of
-lipotropin. Expres-
terminal peptide, joining peptide,
PC1, resulting in formation of N-
The anterior pituitary expresses
tides produced in various tissues.
enzymes results in different pep-
cific expression of these two
PC 2 (blue arrows). Tissue spe-
vertase 1 (PC1, red arrows) and
processing by prohormone con-
Proopiomelanocortin (POMC)
Figure 77–8
ACTH, and
b
sion of PC2 within the hypothala-
a-,
b-, and g-melanocyte stimulating
ate peptide.

patients die of infections. Even the protein collagen
a suppressed immune system, so that many of these
the muscles in particular causes severe weakness. The
teins also remain unaffected. The loss of protein from
the body with the exception of the liver; the plasma pro-
are often profound in Cushing’s syndrome, causing
The effects of glucocorticoids on protein catabolism
tissues.
as twice normal. This results mainly from enhanced glu-
times to values as high as 200 mg/dl after meals-as much
cause increased blood glucose concentration, some-
dance of cortisol secreted in Cushing’s syndrome can
The abun-
About 80 per cent of patients have hypertension, pre-
with Cushing’s syndrome to the left in Figure 77–8.
“moon face,” as demonstrated in the untreated patient
acne and hirsutism (excess growth of facial hair). The
potency of some of the hormones sometimes causes
matous appearance of the face, and the androgenic
The excess secretion of steroids also leads to an ede-
upper abdominal regions, giving rise to a buffalo torso.
mobilization of fat from the lower part of the body, with
A special characteristic of Cushing’s syndrome is
symptoms of Cushing’s syndrome.
longed periods for therapeutic purposes. For example,
Cushing’s syndrome can also occur when large
the differential diagnosis of Cushing’s syndrome.
Therefore, it is usually considered to be a first step in
dexamethasone with suppressed ACTH secretion.
some ACTH-secreting pituitary tumors respond to
can sometimes give an incorrect diagnosis, because
ACTH. The dexamethasone test, although widely used,
primary adrenal overproduction of cortisol (ACTH-
suppress ACTH secretion. In contrast, patients with
tion of ACTH due to an ACTH-secreting pituitary
Cushing’s syndrome. In patients who have overproduc-
ACTH-independent
ACTH-dependent
a synthetic glucocorticoid, can be used to distinguish
Administration of large doses of dexamethasone,
levels due to cortisol feedback inhibition of ACTH
drome and is usually associated with reduced ACTH
about 20 to 25 per cent of clinical cases of Cushing’s syn-
levels of ACTH as well as cortisol. Primary overpro-
Cushing’s syndrome and is characterized by high plasma
Excess ACTH secretion is the most common cause of
Cushing’s disease.
pituitary, this is referred to as
ondary to excess secretion of ACTH by the anterior
the adrenal cortex. When Cushing’s syndrome is sec-
such as an abdominal carcinoma; and (4) adenomas of
secretion” of ACTH by a tumor elsewhere in the body,
which stimulates excess ACTH release; (3) “ectopic
adrenal hyperplasia and excess cortisol secretion; (2)
that secrete large amounts of ACTH, which then causes
causes, including (1) adenomas of the anterior pituitary
effects. Hypercortisolism can occur from multiple
ascribable to abnormal amounts of cortisol, but excess
Most of the abnormalities of Cushing’s syndrome are
Cushing’s syndrome.
addisonian crisis.
This critical need for extra glucocorticoids and the
stresses, such as surgical operations, supervene, a person
whenever different types of trauma, disease, or other
glucocorticoids does not increase during stress. Yet
stress. In a person with Addison’s disease, the output of
As noted earlier in the chapter, great
coids are administered daily.
circulatory shock. Yet such a person can live for years if
Treatment of People with Addison’s Disease.
the same way that MSH does.
stimulate formation of melanin by the melanocytes in
MSH. Probably the tremendous amounts of ACTH
allowing tremendous rates of ACTH secretion as well
anterior pituitary gland is also depressed, therefore
the following: When cortisol secretion is depressed, the
The cause of the melanin deposition is believed to be
thin skin of the nipples.
areas, such as the mucous membranes of the lips and the
blotches, and it is deposited especially in the thin skin
of the mucous membranes and skin. This melanin is not
people with Addison’s disease is melanin pigmentation
the deteriorating effects of different types of stress, and
a person with Addison’s disease highly susceptible to
are weak, indicating that glucocorticoids are needed to
and other nutrients are available, the person’s muscles
cocorticoid lack. Even when excess quantities of glucose
958
Unit XIV
Endocrinology and Reproduction
sluggishness of energy mobilization when cortisol is not
available is one of the major detrimental effects of glu-
maintain other metabolic functions of the tissues in
addition to energy metabolism.
Lack of adequate glucocorticoid secretion also makes
even a mild respiratory infection can cause death.
Melanin Pigmentation.
Another characteristic of most
always deposited evenly but occasionally is deposited in
normal negative feedback to the hypothalamus and
as simultaneous secretion of increased amounts of
cause most of the pigmenting effect because they can
An untreated
person with total adrenal destruction dies within a few
days to a few weeks because of weakness and usually
small quantities of mineralocorticoids and glucocorti-
Addisonian Crisis.
quantities of glucocorticoids are occasionally secreted
in response to different types of physical or mental
is likely to have an acute need for excessive amounts of
glucocorticoids and often must be given 10 or more
times the normal quantities of glucocorticoids to
prevent death.
associated severe debility in times of stress is called an
Hyperadrenalism-Cushing’s
Syndrome
Hypersecretion by the adrenal cortex causes a complex
cascade of hormone effects called
secretion of androgens may also cause important
abnormal function of the hypothalamus that causes high
levels of corticotropin-releasing hormone (CRH),
duction of cortisol by the adrenal glands accounts for
secretion by the anterior pituitary gland.
between
and
adenoma or to hypothalamic-pituitary dysfunction,
even large doses of dexamethasone usually do not
independent) usually have low or undetectable levels of
amounts of glucocorticoids are administered over pro-
patients with chronic inflammation associated with dis-
eases such as rheumatoid arthritis are often treated with
glucocorticoids and may develop some of the clinical
concomitant extra deposition of fat in the thoracic and
appearance of the face is frequently described as a
sumably because of the slight mineralocorticoid effects
of cortisol.
Effects on Carbohydrate and Protein Metabolism.
coneogenesis and decreased glucose utilization by the
greatly decreased tissue proteins almost everywhere in
loss of protein synthesis in the lymphoid tissues leads to
fibers in the subcutaneous tissue are diminished so that

finding can be used in diagnosing the disease.
gens) in the urine may be 10 to 15 times normal. This
the adult male. In adrenogenital syndrome, the excre-
of the testosterone secreted by the testes. It is often dif-
adrenogenital syndrome. In the adult male, the viriliz-
in Figure 77–9, which depicts a 4-year-old boy with
rapid development of the male sexual organs, as shown
In the prepubertal male, a virilizing adrenal tumor
to give typical masculine characteristics.
growth of the clitoris to resemble a penis, and deposi-
masculine distribution of hair on the body and the pubis,
baldness if she also has the genetic trait for baldness,
growth of a beard, a much deeper voice, occasionally
female, she develops virile characteristics, including
ing effects throughout the body. If this occurs in a
most of the adrenal tissue when hyperplasia is the cause.
from the aldosteronism. Treatment of primary aldos-
nism is a decreased plasma renin concentration. This
the nerve fibers, as explained in Chapter 5.
paralysis caused by the hypokalemia. The paralysis is
almost always, hypertension. Especially interesting in
not more than a 4 to 6 mEq/L increase), and,
in extracellular fluid volume and blood volume, very
important effects are hypokalemia, slight increase
discussed in detail earlier in the chapter. The most
than cortisol. The effects of the excess aldosterone are
nism” or “Conn’s syndrome.” Also, in a few instances,
the resulting condition is called “primary aldostero-
to make up for any insufficiency that develops.
lectomy, followed by administration of adrenal steroids
cannot easily be decreased, the only satisfactory treat-
used when surgery is not feasible. If ACTH secretion
GABA-transaminase inhibitors,
that inhibit ACTH secretion, such as
aminoglutethimide,
metyrapone, ketoconazole,
by radiation. Drugs that block steroidogenesis, such as
small tumors in the pituitary that oversecrete ACTH
this is possible. Hypertrophied pituitary glands or even
is the cause or decreasing the secretion of ACTH, if
Treatment of Cushing’s
Treatment of Cushing’s Syndrome.
consequent weakness of the bones.
apart. In addition, severely diminished protein deposi-
the subcutaneous tissues tear easily, resulting in devel-
Chapter 77
Adrenocortical Hormones
959
opment of large purplish striae where they have torn
tion in the bones often causes severe osteoporosis with
syndrome consists of removing an adrenal tumor if this
can sometimes be surgically removed or destroyed
and
or
serotonin antago-
nists and
can also be
ment is usually bilateral partial (or even total) adrena-
Primary Aldosteronism
(Conn’s Syndrome)
Occasionally a small tumor of the zona glomerulosa
cells occurs and secretes large amounts of aldosterone;
hyperplastic adrenal cortices secrete aldosterone rather
slight increase in plasma sodium concentration (usually
primary aldosteronism are occasional periods of muscle
caused by a depressant effect of low extracellular potas-
sium concentration on action potential transmission by
One of the diagnostic criteria of primary aldostero-
results from feedback suppression of renin secretion
caused by the excess aldosterone or by the excess extra-
cellular fluid volume and arterial pressure resulting
teronism is usually surgical removal of the tumor or of
Adrenogenital Syndrome
An occasional adrenocortical tumor secretes excessive
quantities of androgens that cause intense masculiniz-
tion of proteins in the skin and especially in the muscles
causes the same characteristics as in the female plus
ing characteristics of adrenogenital syndrome are
usually obscured by the normal virilizing characteristics
ficult to make a diagnosis of adrenogenital syndrome in
tion of 17-ketosteroids (which are derived from andro-
(Courtesy Dr. Leonard Posey.)
) subtotal adrenalectomy.
drome before (
A person with Cushing’s syn-
Figure 77–9
left) and after
(right
genesis to genetics. Trends Endocrinol Metab 14:310,
Stowasser M, Gordon RD: Primary aldosteronism: from
epithelia. Am J Physiol Renal Physiol 282:F559, 2002.
Stockand JD: New ideas about aldosterone signaling in
hormone biosynthesis. Annu Rev Physiol 63:193, 2001.
Stocco DM: StAR protein and the regulation of steroid
89:3677, 2004.
Stewart PM: Adrenal replacement therapy: time for an
N Engl J Med 349:776, 2003.
Speiser PW, White PC: Congenital adrenal hyperplasia.
Physiol Rev 84:489, 2004.
Spat A, Hunyady L: Control of aldosterone secretion: a
282:G742, 2002.
receptors. Am J Physiol Gastrointest Liver Physiol
Sheppard KE: Nuclear receptors. II. Intestinal corticosteroid
the Cushing syndrome. Ann Intern Med 138:980, 2003.
Raff H, Findling JW: A physiologic approach to diagnosis of
sion. J Clin Invest 113:1075, 2004.
O’Shaughnessy KM, Karet FE: Salt handling and hyperten-
action. News Physiol Sci 19:51, 2004.
Oberleithner H: Unorthodox sites and modes of aldosterone
Endocrinol 211:75, 2003
New MI: Inborn errors of adrenal steroidogenesis. Mol Cell
83:965, 2003.
action: Controversies, questions, and answers. Physiol Rev
HC, Rossol-Haseroth K, Wehling M: Nongenomic steroid
Lösel RM, Falkenstein E, Feuring M, Schultz M, Tillmann
phia: WB Saunders Co, 2003.
Williams Textbook of Endocrinology, 10th ed. Philadel-
Larsen PR, Kronenberg HM, Melmed S, Polonsky KS:
“escape.” Hypertension 6 :I183, 1984.
Hall JE, Granger JP, Smith MJ Jr, Premen AJ: Role of renal
F181, 2001.
alocorticoid selectivity. Am J Physiol Renal Physiol 280:
Farman N, Rafestin-Oblin ME: Multiple aspects of miner-
hyperfiltration. Hypertension 43:41, 2004.
de Paula RB, da Silva AA, Hall JE: Aldosterone antagonism
nisms for gene repression. Endocr Rev 24:488, 2003.
factor-kappa B or activator protein-1: molecular mecha-
De Bosscher K, Vanden Berghe W, Haegeman G: The inter-
acutely ill patients. N Engl J Med 348:727, 2003.
Cooper MS, Stewart PM: Corticosteroid insufficiency in
drome. Lancet 357:783, 2001.
Boscaro M, Barzon L, Fallo F, Sonino N: Cushing’s syn-
hormone by swift action. News Physiol Sci 19:97, 2004.
Boldyreff B, Wehling M: Aldosterone: refreshing a slow
Science Limited, 2002.
ed. Philadelphia: Mosby, Elsevier
Endocrinology, 3
Besser GM,
Thorner MO:
Comprehensive Clinical
Metab 88:5593, 2003.
syndrome: a consensus statement. J Clin Endocrinol
A, Boscaro M: Diagnosis and complications of Cushing’s
Newell-Price J, Nieman LK, Sonino N, Vance ML, Giustina
Grossman AB, Kola B, Lacroix A, Mancini T, Mantero F,
F, Chrousos GP, Fava GA, Findling JW, Gaillard RC,
Arnaldi G, Angeli A, Atkinson AB, Bertagna X, Cavagnini
960
Unit XIV
Endocrinology and Reproduction
References
rd
play between the glucocorticoid receptor and nuclear
attenuates obesity-induced hypertension and glomerular
hemodynamics and arterial pressure in aldosterone
model for convergence in cellular signaling pathways
inward look to the medulla? J Clin Endocrinol Metab
2003.
Leonard Posey.)
Adrenogenital syndrome in a 4-year-old boy. (Courtesy Dr.
Figure 77–10
