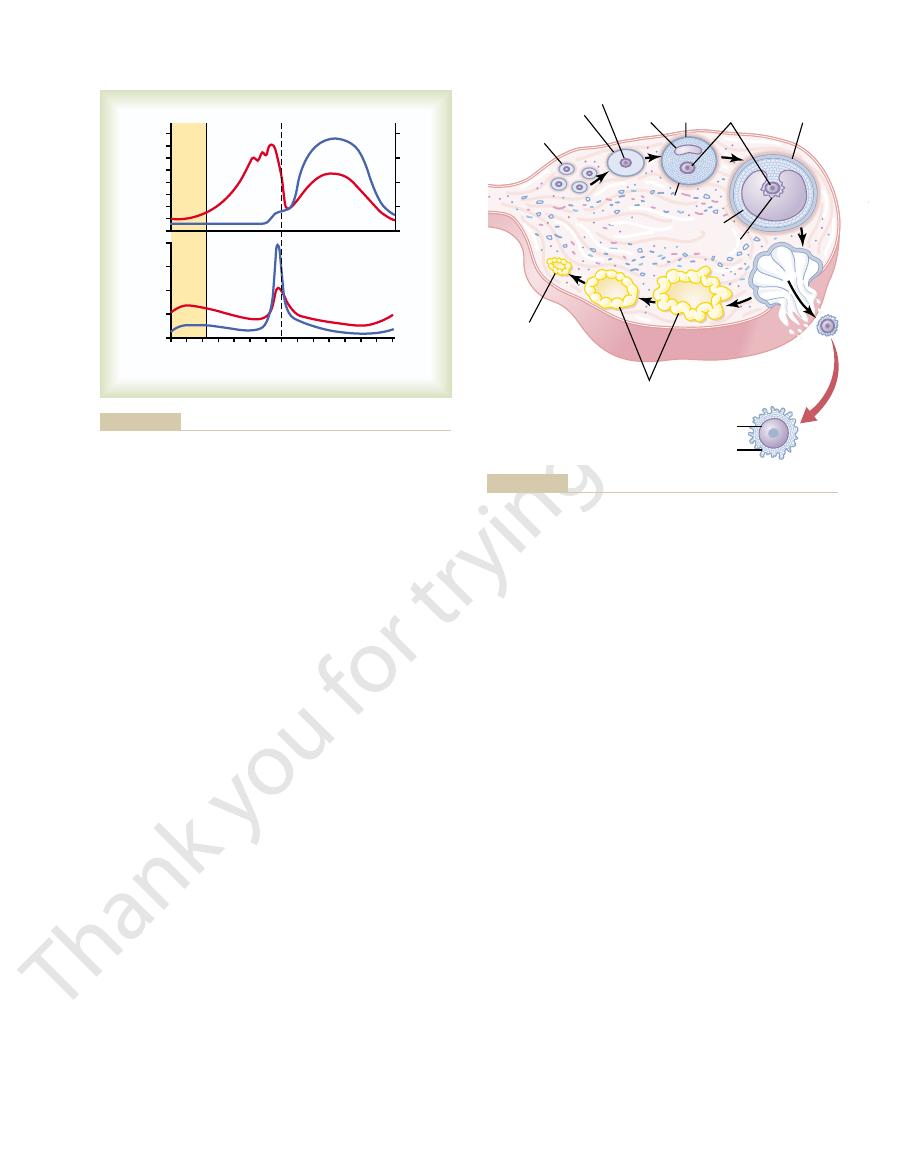
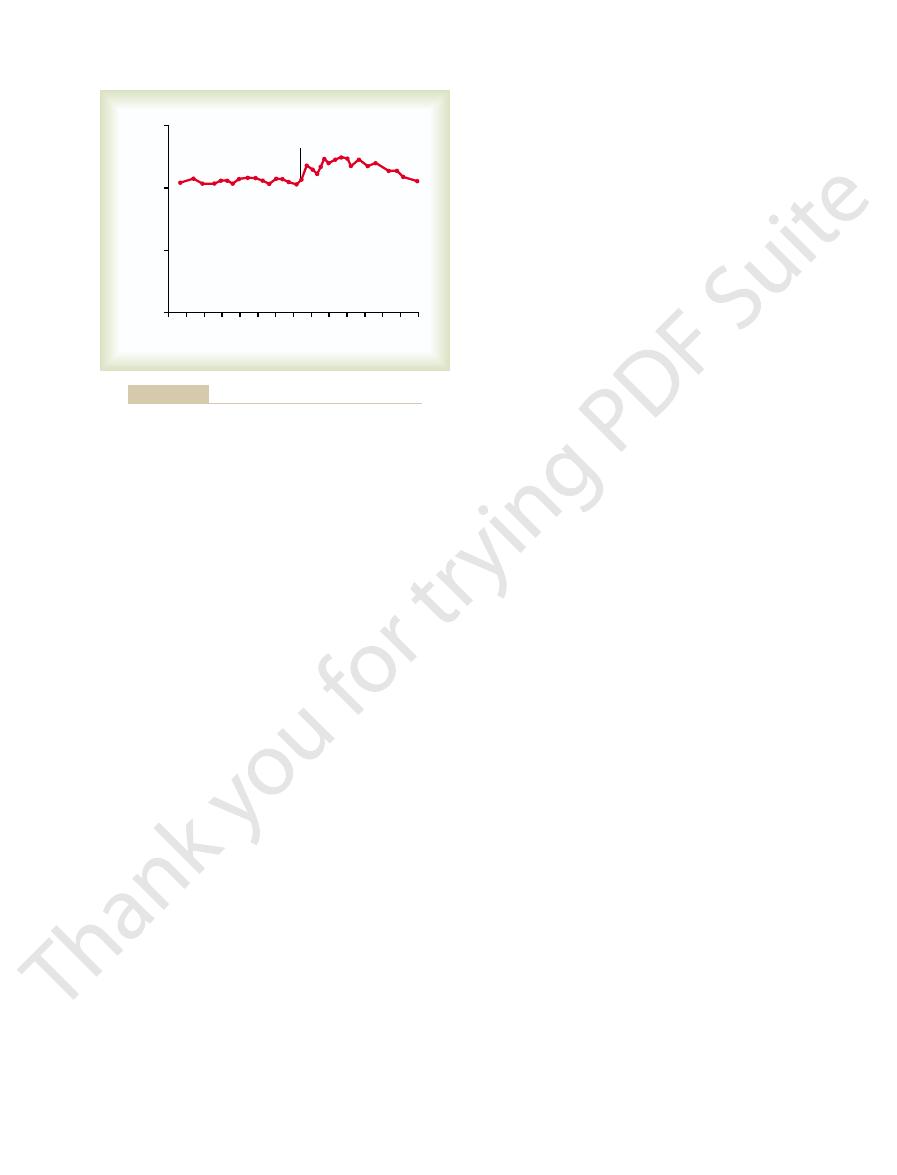
during different parts of the cycle. Figure 81–3 shows the approximate
female monthly sexual cycle; they are secreted at drastically differing rates
These various hormones are not secreted in constant amounts throughout the
progesterone,
3. The ovarian hormones,
2. The anterior pituitary sex hormones,
1. A hypothalamic releasing hormone,
of hormones, as follows:
The female hormonal system, like that of the male, consists of three hierarchies
Female Hormonal System
even these degenerate soon thereafter.
), only a few primordial follicles remain in the ovaries, and
). At the end of reproductive
each month; the remainder degenerate (become
age, 400 to 500 of the primordial follicles develop enough to expel their ova—one
During all the reproductive years of adult life, between about 13 and 46 years of
primary oocyte.
two more cell divisions before it can be fertilized by a sperm. At this time, the ovum
The ovum itself at this stage is still immature, requiring
primordial follicle.
The ovum surrounded by a single layer of granulosa cells is
granulosa cells.
the ovary) and causes them to take on epithelioid characteristics; they are then
lium and migrate into the substance of the ovarian cortex. Each ovum then collects
primordial ova
As the female fetus develops,
which embryologically is derived from the epithelium of the germinal ridges.
During fetal life, the outer surface of the ovary is covered by a
placenta, and fetal membranes—and eventually into a baby.
fertilized by a sperm, it implants in the uterus, where it develops into a fetus, a
ovum then passes through one of the fallopian tubes into the uterus; if it has been
the abdominal cavity near the open fimbriated ends of the two fallopian tubes. This
each monthly sexual cycle, a single ovum is expelled from an ovarian follicle into
Reproduction begins with the development of ova in the ovaries. In the middle of
ovaries, fallopian tubes, uterus,
tract, the most important of which are the
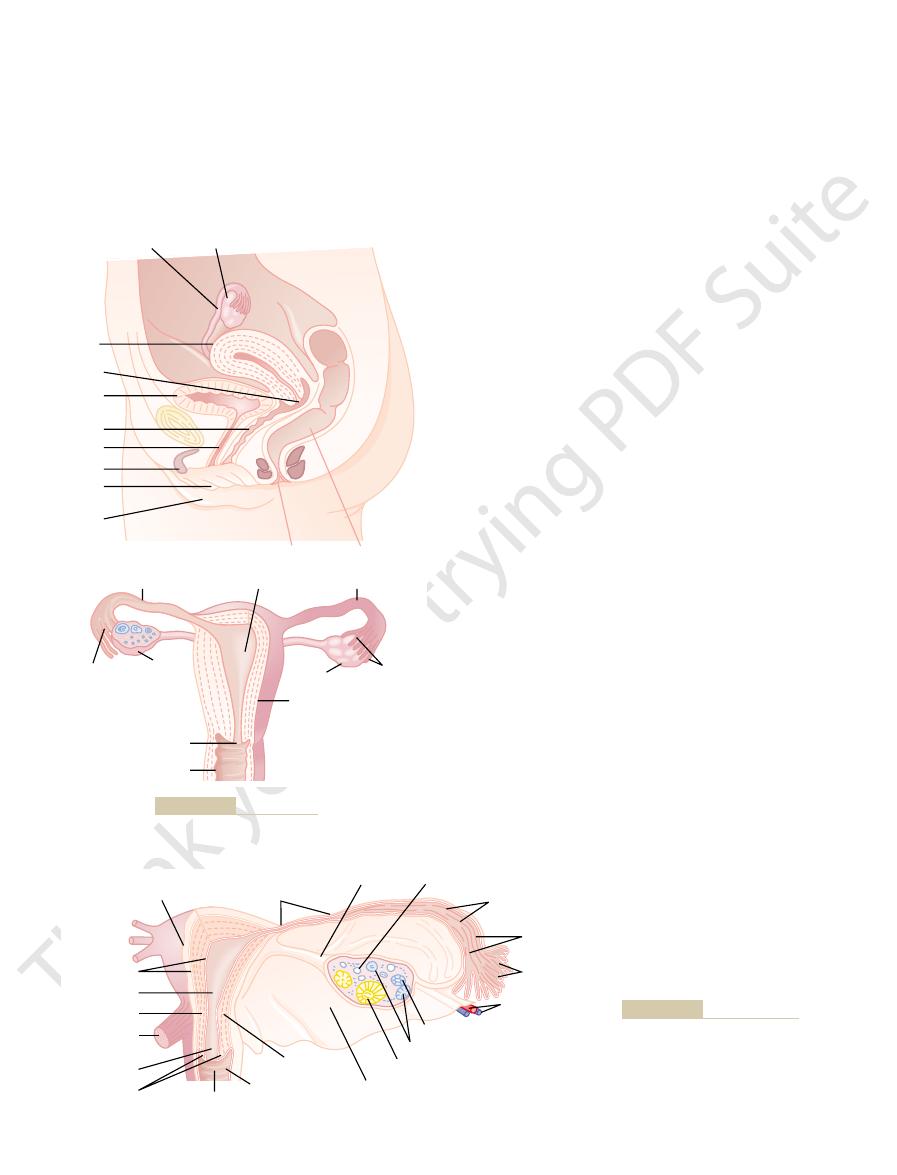
Figures 81–1 and 81–2 show the principal organs of the human female reproductive
Sexual Organs
nancy and childbirth.
with preparation of the female body for pregnancy,
period of pregnancy itself. This chapter is concerned
body for conception and pregnancy, and (2) the
two major phases: (1) preparation of the female
Female reproductive functions can be divided into
Pregnancy and Female Hormones
Female Physiology Before
C
H
A
P
T
E
R
8
1
1011
and Chapter 82 presents the physiology of preg-
Physiologic Anatomy of the Female
and vagina.
germinal epithe-
lium,
differentiate from this germinal epithe-
around it a layer of spindle cells from the ovarian stroma (the supporting tissue of
called
called a
is called a
atretic
capability (at menopause
gonadotropin-releasing hormone
(GnRH)
follicle-stimulating hormone (FSH)
and luteinizing hormone (LH), both of which are secreted in response to
the release of GnRH from the hypothalamus
estrogen and
which are secreted by
the ovaries in response to the two female sex hormones from the anterior
pituitary gland
menarche.
strual cycle is called
puberty,
between the ages of 11 and 15 years. This period of
to onset of normal monthly sexual cycles beginning
secrete progressively more FSH and LH, which leads
secreted. At age 9 to 12 years, the pituitary begins to
inactive, which is the case throughout childhood,
In the absence of these hormones, the ovaries remain
The ovarian changes that occur during the sexual cycle
single fetus will begin to grow at a time. Second, the
from the ovaries each month, so that normally only a
cycle. First, only a
There are two significant results of the female sexual
associated with decreased fertility.
women, although abnormal cycle length is frequently
may be as short as 20 days or as long as 45 days in some
). The duration of the cycle averages 28 days. It
(or, less accurately, the
organs. This rhythmical pattern is called the
The normal reproductive years of the female are char-
Hormones
Function of the Gonadotropic
the male.
pulses averaging once every 90 minutes, as occurs in
during the monthly sexual cycle. It is secreted in short
1012
Unit XIV
Endocrinology and Reproduction
Monthly Ovarian Cycle;
acterized by monthly rhythmical changes in the rates
of secretion of the female hormones and correspon-
ding physical changes in the ovaries and other sexual
female
monthly sexual cycle
menstrual
cycle
single ovum is normally released
uterine endometrium is prepared in advance for
implantation of the fertilized ovum at the required
time of the month.
Gonadotropic Hormones and
Their Effects on the Ovaries
depend completely on the gonadotropic hormones
FSH and LH, secreted by the anterior pituitary gland.
when almost no pituitary gonadotropic hormones are
change is called
and the time of the first men-
Both FSH and LH are
small glycoproteins having molecular weights of about
30,000.
Cervix
Entrance to
uterine tube
Uterine tube
Uterine cavity
Uterine tube (sectioned)
Vagina
Uterine tube
Fimbriae
Uterus
Ovary
Ovary
Uterus
Urethra
Clitoris
Labium
minora
Labium
majora
Vagina
Cervix
Urinary
bladder
Ovary
Rectum
Anus
Female reproductive organs.
Figure 81–1
Ovarian ligament
Ovarian stroma
Perimetrium
Isthmus of uterine tube
Fimbriae
Ovarian vessels
Corpus albicans
Corpus luteum
Ovarian follicles
Broad ligament of uterus
Ampulla of
uterine tube
Mucosal folds
of uterine tube
Endometrium
Uterine cavity
Myometrium
Uterosacral
ligament
Cervical canal
Cervix
Vagina
Vaginal rugae
Isthmus of uterus
The amount of GnRH released from the hypothal-
Physiology of the Human Body,
(Redrawn from Guyton AC:
ovary, and a uterine tube.
Internal structures of the uterus,
Figure 81–2
6th ed. Philadelphia: Saunders
College Publishing, 1984.)
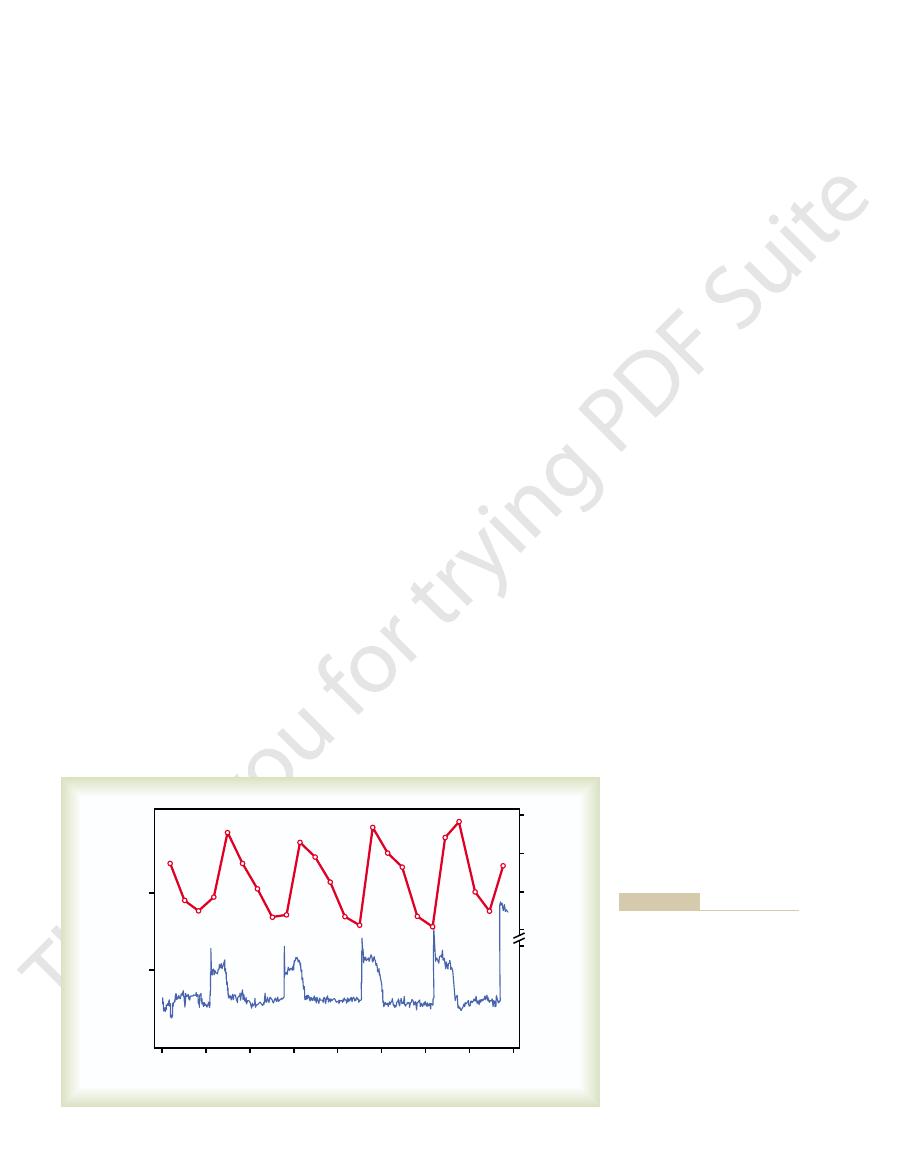
changing concentrations of the anterior pituitary
gonadotropic hormones FSH and LH (bottom two
curves) and of the ovarian hormones estradiol (estro-
gen) and progesterone (top two curves).
amus increases and decreases much less drastically
(discussed later). Accumulation of this fluid causes an
estrogen, one of the important female sex hormones
for a few days, the mass of granulosa cells secretes a
After the early proliferative phase of growth, lasting
the capsule of the developing follicle.
The outer layer, the
into two layers. In the
This is divided
several layers outside the granulosa cells, giving rise to
many more layers of these cells. In addition, spindle
rapid proliferation of the granulosa cells, giving rise to
to 12 primary follicles each month. The initial effect is
mones, especially FSH, cause accelerated growth of 6
that of LH and preceding it by a few days. These hor-
erately, with the increase in FSH slightly greater than
first few days of each monthly female sexual cycle,
Development of Antral and Vesicular Follicles.
primary follicles.
licles; these follicles are known as
diameter twofold to threefold. Then follows growth of
enlargement of the ovum itself, which increases in
The first stage of follicular growth is moderate
them, begin to grow.
ovaries, together with some of the follicles within
gland begin to be secreted in significant quantities, the
puberty, when FSH and LH from the anterior pituitary
the prophase stage of meiotic division. Then, after
Throughout childhood, the granulosa cells are
as shown in the figure.
primordial follicle,
losa cells; the ovum, with this granulosa cell sheath, is
growth in the ovaries. When a female child is born,
Figure 81–4 shows the progressive stages of follicular
Ovarian Follicle Growth—
that stimulate sex hormone synthesis, as explained in
cytoplasm, which causes the formation of
of the cells as well. Almost all these stimulatory
turn, the activated receptors increase the cells’ rates
receptors in the ovarian target cell membranes. In
which are explained in the following sections.
cyclical variations cause cyclical ovarian changes,
LH, as shown in the bottom of Figure 81–3. These
is a cyclical increase and decrease of both FSH and
During each month of the female sexual cycle, there
Female Physiology Before Pregnancy and Female Hormones
Chapter 81
1013
Both FSH and LH stimulate their ovarian target
cells by combining with highly specific FSH and LH
of secretion and usually the growth and proliferation
effects result from activation of the cyclic adenosine
monophosphate second messenger system in the cell
protein
kinase and multiple phosphorylations of key enzymes
Chapter 74.
“Follicular” Phase of the
Ovarian Cycle
each ovum is surrounded by a single layer of granu-
called a
believed to provide nourishment for the ovum and to
secrete an oocyte maturation-inhibiting factor that
keeps the ovum suspended in its primordial state in
additional layers of granulosa cells in some of the fol-
During the
the concentrations of both FSH and LH secreted by
the anterior pituitary gland increase slightly to mod-
cells derived from the ovary interstitium collect in
a second mass of cells called the theca.
theca interna, the cells take on
epithelioid characteristics similar to those of the gran-
ulosa cells and develop the ability to secrete additional
steroid sex hormones (estrogen and progesterone).
theca externa, develops into a
highly vascular connective tissue capsule that becomes
follicular fluid that contains a high concentration of
FSH and LH (ng/mL)
Estradiol (pg/mL)
0 2 4 6 8 10 12 14 16 18 20 22 24 26
FSH
LH
Progesterone
28
0
800
0
800
600
Menstruation
Ovulation
Estradiol
Ovulation
400
200
600
400
200
0
8
Days of female sexual cycle
Progesterone (ng/mL)
follicle-stimulating hormone; LH, luteinizing hormone.
ovarian hormones during the normal female sexual cycle. FSH,
Approximate plasma concentrations of the gonadotropins and
Figure 81–3
Ovum
Ovum
Antrum
Corona radiata
Corpus luteum
Ovulation
Degenerating
corpus luteum
Primordial
follicle
Preantral
follicle
Antral
follicle
Preovulatory
(mature) follicle
Zona pellucida
Theca
Granulosa cells
Corona radiata
Stages of follicular growth in the ovary, also showing formation of
Figure 81–4
the corpus luteum.
appearance.This process is called
They
lutein cells.
from the follicle, the remaining granulosa and theca
of the Ovarian Cycle
Phase
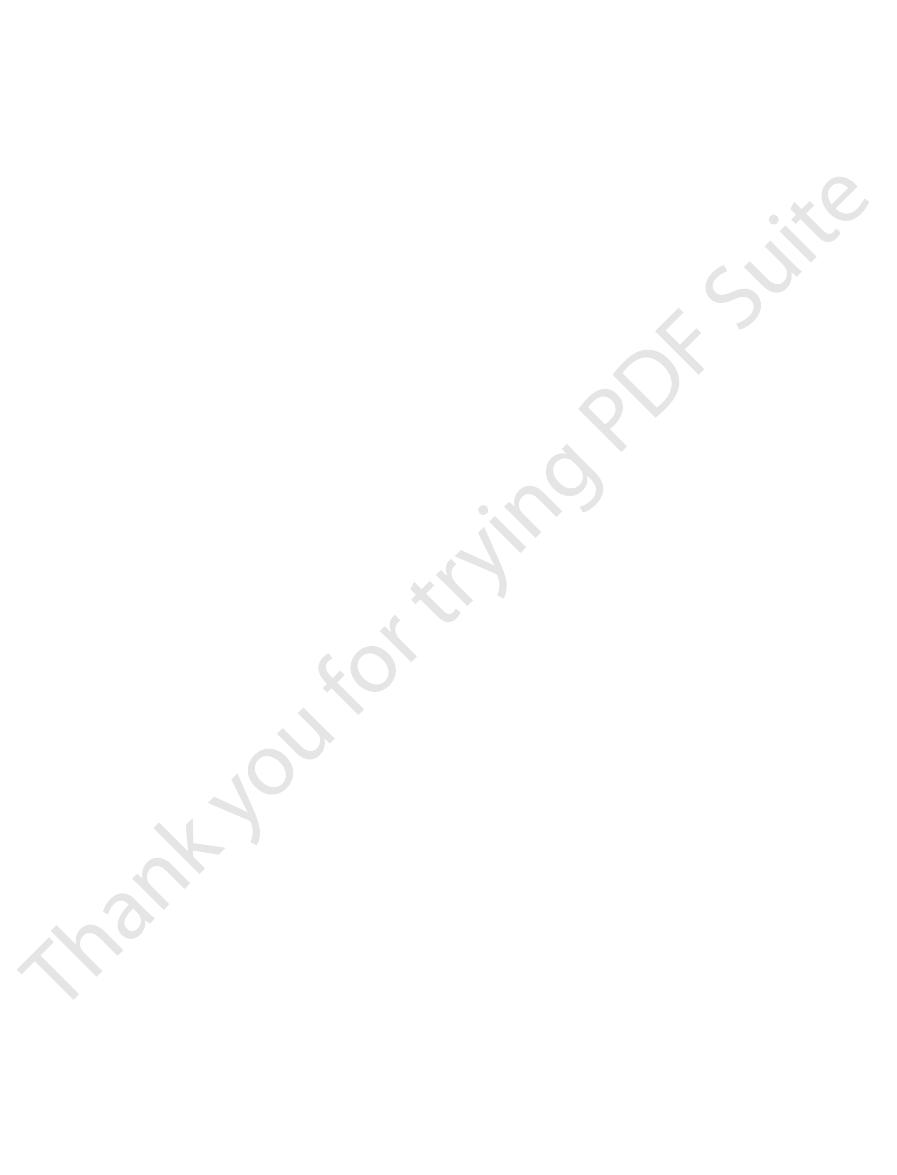
causes follicle rupture, with discharge of the ovum.
follicle swelling. Finally, the combination of follicle
transudation into the follicle, which contributes to
the follicular tissues. These two effects cause plasma
licle wall, and at the same time, prostaglandins (local
and degeneration of the stigma. (2) Simultaneously,
wall, resulting in further swelling of the entire follicle
from lysosomes, and these cause dissolution of the fol-
sary for ovulation: (1) The theca externa (the capsule
few hours, two events occur, both of which are neces-
steroid hormones that contain progesterone. Within a
gland. This LH causes rapid secretion of follicular
initiation of ovulation, showing the role of the large
Figure 81–5 gives a schema for the
ovulation will not take place.
occurs. Without the initial preovulatory surge of LH,
longed phase of excessive estrogen secretion, and (3)
follicle, (2) diminishing estrogen secretion after a pro-
fall about 1 day before ovulation, while increasing
fore, the rate of secretion of estrogen begins to
them mainly to progesterone-secreting cells. There-
effect on the granulosa and theca cells, converting
few days before ovulation. The LH also has a specific
the same time, and the FSH and LH act synergistically
ovulation. FSH also increases about 2-fold to 3-fold at
by the anterior pituitary gland increases markedly,
detail later in the chapter), the rate of secretion of LH
available, the follicle will not progress to the stage
hormone, even when large quantities of FSH are
for final follicular growth and ovulation. Without this
Surge of LH Is Necessary for Ovulation.
granulosa cells, called the
nate outward. This viscous fluid carries with it the
occupied the central portion of the follicle, to evagi-
widely, allowing a more viscous fluid, which has
stigma, and about 2 minutes later, the stigma ruptures
so, fluid begins to ooze from the follicle through the
protrudes like a nipple. In another 30 minutes or
in the center of the follicular capsule, called the
outer wall of the follicle swells rapidly, and a small area
menstruation. Shortly before ovulation, the protruding
female sexual cycle occurs 14 days after the onset of
mature follicle.
nancy. The single follicle reaches a diameter of 1 to 1.5
enough each month to ovulate; this usually prevents
This process of atresia is important, because it nor-
involute.
grow because of its intrinsic positive feedback effects,
follicles. Therefore, the largest follicle continues to
FSH secretion by the anterior pituitary gland, in this
postulated to be the following: The large amounts of
The cause of the atresia is unknown, but it has been
atretic.
begins to outgrow all the others; the remaining 5 to 11
Only One Follicle Fully Matures Each Month, and the Remain-
of granulosa cells located at one pole of the follicle.
enlarges, the ovum itself remains embedded in a mass
fold, or a mass increase of 1000-fold. As the follicle
fold, giving a total ovum diameter increase up to 10-
growth occurs almost explosively. The ovum itself
Once the antral follicles begin to grow, their
in follicular secretion. (3) The increasing estrogens
LH receptors on the original granulosa cells, thus
granulosa cells even more sensitive to FSH. (2) The
causes a positive feedback effect, because it makes the
to form increasing numbers of FSH receptors; this
ated growth is caused by the following: (1) Estrogen is
This acceler-
vesicular follicles.
Then greatly accelerated growth occurs, leading to still
the antral stage is stimulated mainly by FSH alone.
The early growth of the primary follicle up to
shown in Figure 81–4.
to appear within the mass of granulosa cells, as
1014
Unit XIV
Endocrinology and Reproduction
antrum
larger follicles called
secreted into the follicle and causes the granulosa cells
pituitary FSH and the estrogens combine to promote
allowing LH stimulation to occur in addition to FSH
stimulation and creating an even more rapid increase
from the follicle plus the increasing LH from the ante-
rior pituitary gland act together to cause proliferation
of the follicular thecal cells and increase their secre-
tion as well.
also enlarges in diameter another threefold to four-
der Undergo Atresia.
After a week or more of growth—
but before ovulation occurs—one of the follicles
developing follicles involute (a process called atresia),
and these follicles are said to become
estrogen from the most rapidly growing follicle act on
the hypothalamus to depress further enhancement of
way blocking further growth of the less well developed
while all the other follicles stop growing and actually
mally allows only one of the follicles to grow large
more than one child from developing with each preg-
centimeters at the time of ovulation and is called the
Ovulation
Ovulation in a woman who has a normal 28-day
stigma,
ovum surrounded by a mass of several thousand small
corona radiata.
LH is necessary
of ovulation.
About 2 days before ovulation (for reasons that are
not completely understood but are discussed in more
rising 6- to 10-fold and peaking about 16 hours before
to cause rapid swelling of the follicle during the last
amounts of progesterone begin to be secreted.
It is in this environment of (1) rapid growth of the
initiation of secretion of progesterone that ovulation
Initiation of Ovulation.
quantity of LH secreted by the anterior pituitary
of the follicle) begins to release proteolytic enzymes
licular capsular wall and consequent weakening of the
there is rapid growth of new blood vessels into the fol-
hormones that cause vasodilation) are secreted into
swelling and simultaneous degeneration of the stigma
Corpus Luteum—“Luteal”
During the first few hours after expulsion of the ovum
interna cells change rapidly into
enlarge in diameter two or more times and become
filled with lipid inclusions that give them a yellowish
luteinization, and the

follows.
and menstruation begins. A new ovarian cycle then
hormones estrogen and progesterone decrease greatly,
corpus luteum degenerates, whereupon the ovarian
progesterone and estrogen. After another 2 weeks, the
large quantities of both the major female hormones,
After ovulation, the secretory cells of the ovulating
14th day of the cycle. During growth of the follicles,
licles finally becomes “mature” and ovulates on the
cles to begin to grow in the ovaries. One of these fol-
About every 28 days, gonadotropic hormones from the
explained later.
this time also leads to menstruation by the uterus, as
of new follicles, beginning a new ovarian cycle. The
FSH and LH again. FSH and LH initiate the growth
terone, and inhibin by the corpus luteum removes the
sudden cessation of secretion of estrogen, proges-
2 days before menstruation begins. At this time, the
around the 26th day of the normal female sexual cycle,
almost exactly 12 days of corpus luteum life, which is
Final involution normally occurs at the end of
causes the corpus luteum to degenerate completely, a
FSH and LH result, and loss of these hormones finally
cially FSH secretion. Low blood concentrations of both
inhibits secretion by the anterior pituitary gland, espe-
by the Sertoli cells of the male testes. This hormone
In addition, the lutein cells secrete small amounts of
luteal phase of the ovarian cycle, have strong feedback
lesser extent, secreted by the corpus luteum during the
pregnancy.
which is secreted by the placenta, can
chorionic
pregnancy in Chapter 82 that another hormone with
in about 12 days. We shall see in the discussion of
secretion, followed by (4) degeneration. All this occurs
sequence of (1) proliferation, (2) enlargement, and (3)
to cause luteinization, the newly formed lutein cells
The corpus luteum is a highly secretory organ, secret-
tion-inhibiting factor,
local hormone in the follicular fluid, called
of the ovum from the follicle. A yet uncharacterized
“yellowing.” Luteinization also depends on extrusion
this function gives LH its name—“luteinizing,” for
on LH secreted by the anterior pituitary gland. In fact,
The change of granulosa and
during the ensuing few weeks, this is replaced
about 12 days after ovulation, becoming the
function as well as its yellowish, lipid characteristic
of development 7 to 8 days after ovulation. Then it
about 1.5 centimeters in diameter, reaching this stage
In the normal female, the corpus luteum grows to
hormones.
sex hormones. However, most of these hormones are
estrogen). The theca cells form mainly the androgens
The granulosa cells in the corpus luteum develop
which is shown in Figure 81–4. A well-developed
Female Physiology Before Pregnancy and Female Hormones
Chapter 81
1015
total mass of cells together is called the corpus luteum,
vascular supply also grows into the corpus luteum.
extensive intracellular smooth endoplasmic reticula
that form large amounts of the female sex hormones
progesterone and estrogen (more progesterone than
androstenedione and testosterone rather than female
also converted by the granulosa cells into the female
begins to involute and eventually loses its secretory
corpus
albicans;
by connective tissue and over months is absorbed.
Luteinizing Function of LH.
theca interna cells into lutein cells is dependent mainly
luteiniza-
seems to hold the luteinization
process in check until after ovulation.
Secretion by the Corpus Luteum: An Additional Function of LH.
ing large amounts of both progesterone and estrogen.
Once LH (mainly that secreted during the ovulatory
surge) has acted on the granulosa and theca cells
seem to be programmed to go through a preordained
almost exactly the same properties as LH,
gonadotropin,
act on the corpus luteum to prolong its life—usually
maintaining it for at least the first 2 to 4 months of
Involution of the Corpus Luteum and Onset of the Next Ovarian
Cycle.
Estrogen in particular and progesterone to a
effects on the anterior pituitary gland to maintain low
secretory rates of both FSH and LH.
the hormone inhibin, the same as the inhibin secreted
process called involution of the corpus luteum.
feedback inhibition of the anterior pituitary gland,
allowing it to begin secreting increasing amounts of
paucity of secretion of progesterone and estrogen at
Summary
anterior pituitary gland cause about 8 to 12 new folli-
mainly estrogen is secreted.
follicle develop into a corpus luteum that secretes
Weakened follicle wall
Luteinizing hormone
Follicle rupture
Evagination of ovum
Follicular steroid hormones
(progesterone)
Proteolytic enzymes
(collagenase)
Follicular hyperemia
and
prostaglandin secretion
Degeneration
of stigma
Plasma transudation
into follicle
Follicle swelling
Figure 81–5
Postulated mechanism of ovulation.
fates, and about one fifth of these conjugated products
The liver
period of 30 minutes or so.
esterone-binding globulins. The binding between these
Estrogens and Progesterone Are Transported in the Blood Bound
the plasma of the male by the testes.
into the circulating blood at this time. Also, about one
cells. During the luteal phase of the cycle, far too much
these two initial hormones can leave the ovaries,
during the follicular phase of the ovarian cycle, before
sex hormone testosterone are synthesized first; then,
During synthesis, mainly progesterone and the male
combine to form the appropriate steroid nucleus.
acetyl coenzyme A, multiple molecules of which can
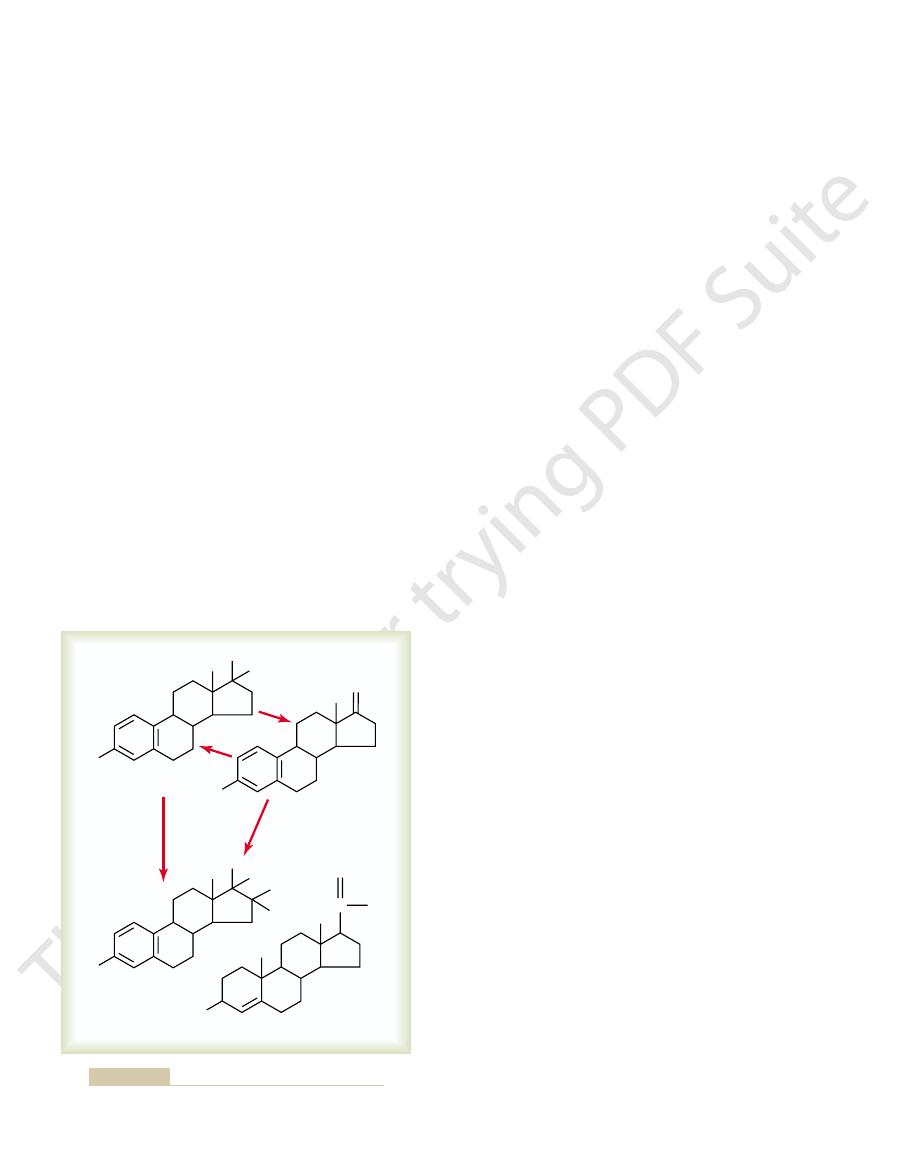
in Figure 81–6 that they are all steroids. They are
pregnancy, especially after the fourth month of
As we shall see in Chapter 82, large amounts of
half of each ovarian cycle, when it is secreted by the
In the normal nonpregnant female, progesterone is
effects. Yet, for practical purposes, it is usually reason-
-hydroxyprogesterone, are secreted
progestin, 17-
is progesterone. However, small amounts of another
the estrogenic effects of estrone are not negligible.
estradiol is considered the major estrogen, although
that of the other two together. For this reason,
ing these relative potencies, one can see that the total
that of estrone and 80 times that of estriol. Consider-
The estrogenic potency of
occurring mainly in the liver.
from both estradiol and estrone, with the conversion
a weak estrogen; it is an oxidative product derived
adrenal cortices and by ovarian thecal cells. Estriol is
are also secreted, but most of this is formed in the
-estradiol. Small amounts of estrone
in Figure 81–6. The principal estrogen secreted by
estrone,
placenta, as discussed in Chapter 82.
pregnancy,
the adrenal cortices. During
ovaries, although minute amounts are also secreted by
female, estro-
prepare the uterus for pregnancy and the breasts for
of the female. The progestins function mainly to
The estro-
progesterone.
progestins.
The two types of ovarian sex hormones are the
and Progesterone
Hormones—Estradiol
1016
Unit XIV
Endocrinology and Reproduction
Functions of the Ovarian
estro-
gens and the
By far the most important of
the estrogens is the hormone estradiol, and by far the
most important progestin is
gens mainly promote proliferation and growth of spe-
cific cells in the body that are responsible for the
development of most secondary sexual characteristics
lactation.
Chemistry of the Sex Hormones
Estrogens.
In the normal nonpregnant
gens are secreted in significant quantities only by the
tremendous
quantities of estrogens are also secreted by the
Only three estrogens are present in significant quan-
tities in the plasma of the human female:
b-estradiol,
and estriol, the formulas for which are shown
the ovaries is
b
peripheral tissues from androgens secreted by the
b-estradiol is 12 times
estrogenic effect of
b-estradiol is usually many times
b-
Progestins.
By far the most important of the progestins
a
along with progesterone and have essentially the same
able to consider progesterone the only important
progestin.
secreted in significant amounts only during the latter
corpus luteum.
progesterone are also secreted by the placenta during
gestation.
Synthesis of the Estrogens and Progestins.
Note from the
chemical formulas of the estrogens and progesterone
synthesized in the ovaries mainly from cholesterol
derived from the blood but also to a slight extent from
almost all the testosterone and much of the proges-
terone are converted into estrogens by the granulosa
progesterone is formed for all of it to be converted,
which accounts for the large secretion of progesterone
fifteenth as much testosterone is secreted into the
plasma of the female by the ovaries as is secreted into
to Plasma Proteins.
Both estrogens and progesterone
are transported in the blood bound mainly with
plasma albumin and with specific estrogen- and prog-
hormones and the plasma proteins is loose enough
that they are rapidly released to the tissues over a
Functions of the Liver in Estrogen Degradation.
conjugates the estrogens to form glucuronides and sul-
HO
b
-Estradiol
Estrone
Progesterone
H
OH
CH
3
HO
O
CH
3
HO
H
OH
H
OH
CH
3
O
C
CH
3
CH
3
O
CH
3
Estriol
Chemical formulas of the principal female hormones.
Figure 81–6

estrogens are administered. This mainly results from
a slight increase in total body protein, which is evi-
prevent the osteoporotic effects.
vertebrae, a large share of postmenopausal women are
and lead to bone fracture, especially fracture of the
Chapter 79. Because this can greatly weaken the bones
osteoporosis,
In some women, this effect is extremely severe, and the
decreased deposition of bone calcium and phosphate.
the bones, (2) decreased bone matrix, and (3)
deficiency leads to (1) increased osteoclastic activity in
estrogens are secreted by the ovaries. This estrogen
After menopause, almost no
ciency in Old Age.
normal time.
several years earlier than growth of the male. A female
male. As a result, growth of the female usually ceases
bones. This effect of estrogen in the female is much
another potent effect on skeletal growth: They cause
rapid for several years. However, estrogens have
her reproductive years, her growth in height becomes
late bone growth. At puberty, when the female enters
Effect of Estrogens on the Skeleton.
the breasts into milk-producing organs.
However, they do not complete the job of converting
breasts and of the milk-producing apparatus. They
In summary, the estrogens initiate growth of the
determinative growth and function of these structures.
extent under the influence of estrogens alone, but it
system, and (3) deposition of fat in the breasts. The
tissues of the breasts, (2) growth of an extensive ductile
the influence of appropriate hormones, the masculine
of females and males are exactly alike. In fact, under
The primordial breasts
Effect of Estrogens on the Breasts.
These cilia always beat toward the uterus, which helps
Also, activity of the cilia is considerably enhanced.
epithelial cells that line the fallopian tubes to increase.
especially important, they cause the number of ciliated
similar to that on the uterine endometrium.They cause
The estrogens’
Effect of Estrogens on the Fallopian Tubes.
cycle.
the implanted ovum. These effects are discussed later
glands, which will later aid in providing nutrition to
under the influence of estrogens. Estrogens cause
the uterus increases twofold to threefold, but more
During the first few years after puberty, the size of
is the prepubertal cuboidal cell epithelium. Vaginal
from a cuboidal into a stratified type, which is consid-
In addition, estrogens change the vaginal epithelium
times in size. Also, the external genitalia enlarge, with
lopian tubes, uterus, and vagina all increase several
those of a child to those of an adult. The ovaries, fal-
more. At this time, the female sex organs change from
in minute quantities, but at puberty, the quantity
During childhood, estrogens are secreted only
Functions of the Estrogens
fore, one can estimate the rate of progesterone
esterone is excreted in the urine in this form. There-
The major end product of progesterone degradation
estrogens, the liver is especially important for this
steroids that have no progestational effect. As with the
tion, almost all the progesterone is degraded to other
Within a few minutes after secre-
activity of estrogens in the body, sometimes causing
totally impotent estrogen estriol. Therefore, dimin-
excreted in the urine. Also, the liver converts the
is excreted in the bile; most of the remainder is
Female Physiology Before Pregnancy and Female Hormones
Chapter 81
1017
potent estrogens estradiol and estrone into the almost
ished liver function actually increases
the
hyperestrinism.
Fate of Progesterone.
metabolic degradation.
is pregnanediol. About 10 per cent of the original prog-
formation in the body from the rate of this excretion.
—
Their Effects on the Primary and
Secondary Female Sex Characteristics
A primary function of the estrogens is to cause cellu-
lar proliferation and growth of the tissues of the sex
organs and other tissues related to reproduction.
Effect of Estrogens on the Uterus and External Female Sex
Organs.
secreted in the female under the influence of the
pituitary gonadotropic hormones increases 20-fold or
deposition of fat in the mons pubis and labia majora
and enlargement of the labia minora.
erably more resistant to trauma and infection than
infections in children can often be cured by the admin-
istration of estrogens simply because of the resulting
increased resistance of the vaginal epithelium.
important than the increase in uterus size are the
changes that take place in the uterine endometrium
marked proliferation of the endometrial stroma
and greatly increased development of the endometrial
in the chapter in connection with the endometrial
effect on the mucosal lining of the fallopian tubes is
the glandular tissues of this lining to proliferate;
propel the fertilized ovum in that direction.
breast during the first 2 decades of life can develop
sufficiently to produce milk in the same manner as the
female breast.
Estrogens cause (1) development of the stromal
lobules and alveoli of the breast develop to a slight
is progesterone and prolactin that cause the ultimate
are also responsible for the characteristic growth
and external appearance of the mature female breast.
Estrogens inhibit
osteoclastic activity in the bones and therefore stimu-
uniting of the epiphyses with the shafts of the long
stronger than the similar effect of testosterone in the
eunuch who is devoid of estrogen production usually
grows several inches taller than a normal mature
female because her epiphyses do not unite at the
Osteoporosis of the Bones Caused by Estrogen
Defi
resulting condition is
described in
treated prophylactically with estrogen replacement to
Effect of Estrogens on Protein Deposition.
Estrogens cause
denced by a slight positive nitrogen balance when
the growth-promoting effect of estrogen on the sexual
cycle, the stromal cells and the epithelial cells
estrogens,
only a thin layer of endometrial stroma remains, and
desquamated by menstruation. After menstruation,
monthly cycle, most of the endometrium has been
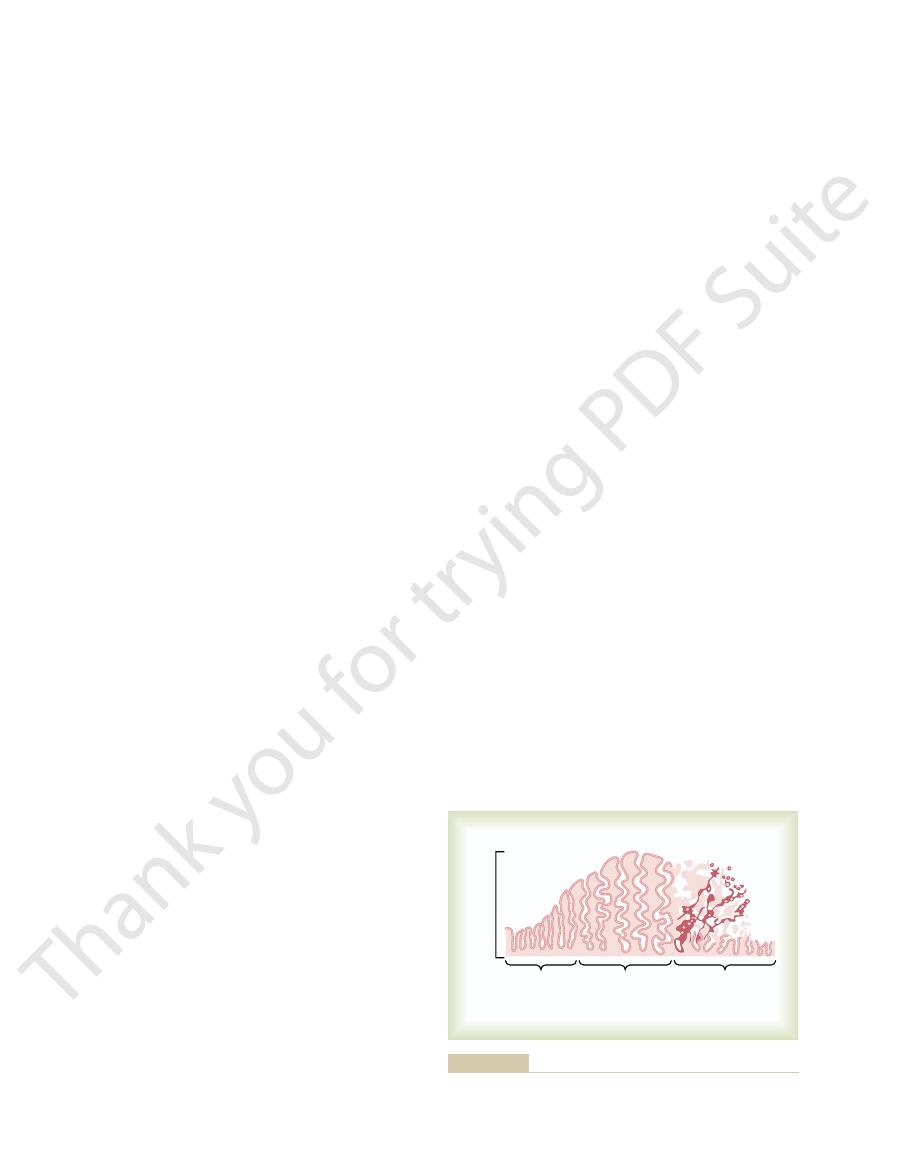
cycle are shown in Figure 81–7.
The various phases of this endometrial
mation of the endometrium, which is known as
tory changes in the endometrium; and (3) desqua-
the uterine endometrium; (2) development of secre-
ates through the following stages: (1) proliferation of
endometrial cycle in the lining of the uterus that oper-
Associated with the monthly cyclical production
increased fluid in the subcutaneous tissue.
the lobules and alveoli, but part also results from
Progesterone also causes the breasts to swell. Part
milk; as discussed in Chapter 82, milk is secreted only
enlarge, and become secretory in nature. However,
the breasts, causing the alveolar cells to proliferate,
Effect of Progesterone on the Breasts.
necessary for nutrition of the fertilized, dividing ovum
lining of the fallopian tubes. These secretions are
Effect of Progesterone on the Fallopian Tubes.
of uterine contractions, thereby helping to prevent
progesterone decreases the frequency and intensity
with the endometrial cycle of the uterus.
ovum. This function is discussed later in connection
the latter half of the monthly female sexual cycle, thus
secretory changes in the uterine endometrium
Functions of Progesterone
body fluid retention, as discussed in Chapter 82.
nificance, but during pregnancy, the tremendous for-
sodium and water retention by the kidney tubules. This
terone and some other adrenocortical hormones, cause
hormones has been pointed out. Estrogens, like aldos-
The chemical
the skin to become more vascular; this is often associ-
of a child or a castrated female. Also, estrogens cause
but even so, the skin of a woman is thicker than that
responsible for this.
puberty. Androgens formed in increased quantities by
greatly affect hair distribution. However, hair does
characteristic of the feminine figure.
deposition of fat in the buttocks and thighs, which is
breasts and subcutaneous tissues, estrogens cause the
more protein. In addition to deposition of fat in the
greater than that in the male body, which contains
fat in the subcutaneous tissues. As a result, the per-
They also cause deposition of increased quantities of
increase caused by the male sex hormone testosterone.
slightly, but only about one third as much as the
erful as that caused by estrogens.
The enhanced protein deposition caused by testos-
organs, the bones, and a few other tissues of the body.
1018
Unit XIV
Endocrinology and Reproduction
terone is much more general and many times as pow-
Effect of Estrogens on Body Metabolism and Fat Deposition.
Estrogens increase the whole-body metabolic rate
centage of body fat in the female body is considerably
Effect of Estrogens on Hair Distribution.
Estrogens do not
develop in the pubic region and in the axillae after
the female adrenal glands after puberty are mainly
Effect of Estrogens on the Skin.
Estrogens cause the skin
to develop a texture that is soft and usually smooth,
ated with increased warmth of the skin and also pro-
motes greater bleeding of cut surfaces than is observed
in men.
Effect of Estrogens on Electrolyte Balance.
similarity of estrogenic hormones to adrenocortical
effect of estrogens is normally slight and rarely of sig-
mation of estrogens by the placenta may contribute to
Effect of Progesterone on the Uterus.
By far the most
important function of progesterone is to promote
during
preparing the uterus for implantation of the fertilized
In addition to this effect on the endometrium,
expulsion of the implanted ovum.
Progesterone
also promotes increased secretion by the mucosal
as it traverses the fallopian tube before implantation.
Progesterone
promotes development of the lobules and alveoli of
progesterone does not cause the alveoli to secrete
after the prepared breast is further stimulated by pro-
lactin from the anterior pituitary gland.
of this swelling is due to the secretory development in
Monthly Endometrial Cycle
and Menstruation
of estrogens and progesterone by the ovaries is an
menstruation.
Proliferative Phase (Estrogen Phase) of the Endometrial Cycle,
Occurring Before Ovulation.
At the beginning of each
the only epithelial cells that are left are those located
in the remaining deeper portions of the glands and
crypts of the endometrium. Under the influence of
secreted in increasing quantities by the
ovary during the first part of the monthly ovarian
(11 days)
Endometrial
thickness
Proliferative
phase
Secretory
phase
(12 days)
Menstrual
phase
(5 days)
Phases of endometrial growth and menstruation during each
Figure 81–7
monthly female sexual cycle.

mechanism that causes the cyclical variations.
cycle, we can attempt to explain the basic rhythmical
Now that we have presented the major cyclical
Hormones
Hypothalamic-Pituitary
denuded. This is of extreme protective value.
struation, even though the endometrial surfaces are
of these leukocytes and possibly other factors, the
necrosis causes this outflow of leukocytes. As a result
along with the necrotic material and blood. It is prob-
tion, tremendous numbers of leukocytes are released
of blood ceases because, by this time, the endometrium
Within 4 to 7 days after menstruation starts, the loss
clinical evidence of uterine pathology.
ting. The presence of clots during menstruation is often
bleeding occurs from the uterine surface, the quantity
with the necrotic endometrial material. If excessive
serous fluid are lost. The menstrual fluid is normally
During normal menstruation, approximately 40
uterine contents.
together, initiate uterine contractions that expel the
substances in the decaying desquamate, all acting
desquamated tissue and blood in the uterine cavity,
the endometrium have desquamated. The mass of
onset of menstruation, all the superficial layers of
of the hemorrhages until, about 48 hours after the
hours. Gradually, the necrotic outer layers of the
vascular layer of the endometrium, and the hemor-
blood vessels. As a result, blood at first seeps into the
initiate necrosis in the endometrium, especially of the
endometrium, and the loss of hormonal stimulation
The vasospasm, the decrease in nutrients to the
time.
effect of involution, such as release of a vasoconstric-
become vasospastic, presumably because of some
onset of menstruation, the tortuous blood vessels
thickness. Then, during the 24 hours preceding the
two hormones, followed rapidly by involution of the
end of the monthly ovarian cycle. The first effect is
gens and progesterone, especially progesterone, at the
Menstruation follows.
low levels of secretion, as shown in Figure 81–3.
in the ovary suddenly involutes, and the ovarian
before the end of the monthly cycle, the corpus luteum
If the ovum is not fertilized, about 2 days
nutrients available to the early implanting embryo.
stored substances, thus making great quantities of
the implanting ovum (in the blastocyst stage) begin to
endometrium, the trophoblastic cells on the surface of
dividing ovum. Then, once the ovum implants in the
called “uterine milk,” provide nutrition for the early
to 9 days after ovulation), the uterine secretions,
ovum during the latter half of the monthly cycle. From
fertilized
The whole purpose of all these endometrial changes
6 millimeters.
ovulation, the endometrium has a thickness of 5 to
the peak of the secretory phase, about 1 week after
with the blood vessels becoming highly tortuous. At
in proportion to the developing secretory activity,
deposits increase greatly in the stromal cells; and the
plasm of the stromal cells increases; lipid and glycogen
mulates in the glandular epithelial cells. Also, the cyto-
in tortuosity; an excess of secretory substances accu-
development of the endometrium. The glands increase
endometrium during this phase of the cycle, whereas
large quantities by the corpus luteum. The estrogens
half of the monthly cycle, after ovulation has occurred,
Secretory Phase (Progestational Phase) of the Endometrial
uterus.
the cervical canal, forming channels that help guide
vical region, secrete a thin, stringy mucus. The mucus
The endometrial glands, especially those of the cer-
metrium. At the time of ovulation, the endometrium is
greatly in thickness, owing to increasing numbers of
Then, during the next week and a half—that is,
proliferate rapidly. The endometrial surface is re-
Female Physiology Before Pregnancy and Female Hormones
Chapter 81
1019
epithelialized within 4 to 7 days after the beginning of
menstruation.
before ovulation occurs—the endometrium increases
stromal cells and to progressive growth of the endome-
trial glands and new blood vessels into the endo-
3 to 5 millimeters thick.
strings actually align themselves along the length of
sperm in the proper direction from the vagina into the
Cycle, Occurring After Ovulation.
During most of the latter
progesterone and estrogen together are secreted in
cause slight additional cellular proliferation in the
progesterone causes marked swelling and secretory
blood supply to the endometrium further increases
is to produce a highly secretory endometrium that con-
tains large amounts of stored nutrients to provide
appropriate conditions for implantation of a
the time a fertilized ovum enters the uterine cavity
from the fallopian tube (which occurs 3 to 4 days
after ovulation) until the time the ovum implants (7
digest the endometrium and absorb the endometrial
Menstruation.
hormones (estrogens and progesterone) decrease to
Menstruation is caused by the reduction of estro-
decreased stimulation of the endometrial cells by these
endometrium itself to about 65 per cent of its previous
leading to the mucosal layers of the endometrium
tor material—possibly one of the vasoconstrictor types
of prostaglandins that are present in abundance at this
rhagic areas grow rapidly over a period of 24 to 36
endometrium separate from the uterus at the sites
plus contractile effects of prostaglandins or other
milliliters of blood and an additional 35 milliliters of
nonclotting because a fibrinolysin is released along
of fibrinolysin may not be sufficient to prevent clot-
has become re-epithelialized.
Leukorrhea During Menstruation.
During menstrua-
able that some substance liberated by the endometrial
uterus is highly resistant to infection during men-
Regulation of the Female
Monthly Rhythm—Interplay
Between the Ovarian and
changes that occur during the monthly female sexual
LH at the end of the monthly female sexual cycle.
extent, LH by the anterior pituitary gland. Therefore,
male—inhibiting the secretion of FSH and, to a lesser
Sertoli cells secrete inhibin in the male testes. This
involved, especially
gen and progesterone, other hormones seem to be
frequency of the GnRH pulses.
decrease secretion of GnRH, especially by altering the
the anterior pituitary gland directly, but they also
These feedback effects seem to operate mainly on
estrogen is multiplied, even though progesterone by
when progesterone is available, the inhibitory effect of
inhibit the production of both LH and FSH. Also,
and FSH Secretion
and Progesterone in Decreasing Both LH
Negative Feedback Effects of Estrogen
release and the frequency of the pulses, thus providing
ronal centers in the higher brain’s “limbic” system (the
secrete GnRH in moderate amounts. Multiple neu-
female sexual activity, although neurons located in the
in the arcuate nuclei of this area. Therefore, it is
primarily in the mediobasal hypothalamus, especially
The neuronal
This is shown by the upper curve in Figure 81–8.
tent output of LH secretion about every 90 minutes.
The pulsatile release of GnRH also causes intermit-
reasons unknown, the pulsatile nature of GnRH
by the anterior pituitary gland is lost. Therefore, for
pulses, its ability to cause the release of LH and FSH
occur every 1 to 2 hours. The lower curve in Figure
Stimulates Pulsatile Release of LH from the Anterior Pituitary
Glu-His-Trp-Ser-Tyr-Gly-Leu-Arg-Pro-Gly-NH
is important. This hormone has been purified
case of the gonadotropins, one releasing hormone,
the hypothalamic-hypophysial portal system. In the
hormones” formed in the hypothalamus and then
anterior pituitary hormones is controlled by “releasing
As pointed out in Chapter 74, secretion of most of the
Causes the Anterior Pituitary Gland to Secrete
The Hypothalamus Secretes GnRH, Which
1020
Unit XIV
Endocrinology and Reproduction
LH and FSH
transported to the anterior pituitary gland by way of
GnRH,
and has been found to be a decapeptide with the
following formula:
2
Intermittent, Pulsatile Secretion of GnRH by the Hypothalamus
Gland.
Experiments have demonstrated that the hypo-
thalamus does not secrete GnRH continuously but
instead secretes it in pulses lasting 5 to 25 minutes that
81–8 shows the electrical pulsatile signals in the hypo-
thalamus that cause the hypothalamic pulsatile output
of GnRH.
It is intriguing that when GnRH is infused continu-
ously so that it is available all the time rather than in
release is essential to its function.
Hypothalamic Centers for Release of GnRH.
activity that causes pulsatile release of GnRH occurs
believed that these arcuate nuclei control most
preoptic area of the anterior hypothalamus also
system for psychic control) transmit signals into the
arcuate nuclei to modify both the intensity of GnRH
a partial explanation of why psychic factors often
modify female sexual function.
Estrogen in small amounts has a strong effect to
itself has little effect.
operate to a lesser extent on the hypothalamus to
Hormone Inhibin from the Corpus Luteum Inhibits FSH and LH
Secretion.
In addition to the feedback effects of estro-
inhibin, which is secreted along
with the steroid sex hormones by the granulosa cells
of the ovarian corpus luteum in the same way that
hormone has the same effect in the female as in the
it is believed that inhibin might be especially impor-
tant in causing the decrease in secretion of FSH and
0
120
240
360
480
MUA
LH
1000
2000
0
40
60
80
100
Minutes
Multi-unit electrical activity (MUA)
(spikes/min)
Luteinizing hormone (LH)
(ng/mL)
hormone secretion. Neuroen-
correlates of pulsatile luteinizing
al: Central electrophysiologic
hypothalamus. (Data from Wilson
recording of multi-unit electrical
ovariectomized rhesus monkey.
peripheral circulation of a
luteinizing hormone (LH) in the
Figure 81–8
Upper curve: Pulsatile change in
p e n t o b a r b i t a l - a n e s t h e t i z e d
Lower curve: Minute-by-minute
activity (MUA) in the mediobasal
RC, Kesner JS, Kaufman JM, et
docrinology 39:256, 1984.)
means the beginning of the cycle of
menarche
means the onset of adult sexual life, and
months to years before menopause, presumably
usually anovulatory, as are the cycles occurring several
The first few cycles after the onset of puberty are
itself, although it can alter its rhythm.
terone is not required for maintenance of the cycle
rhythm continues. Therefore, it is likely that proges-
Second, the cycle is shortened by several days, but the
of progesterone during the latter portion of the cycle.
of the corpus luteum, so there is almost no secretion
First, lack of ovulation causes failure of development
continue, but they are altered in the following ways:
said to be “anovulatory.” The phases of the sexual cycle
magnitude, ovulation will not occur, and the cycle is
Anovulatory Cycles—Sexual Cycles at Puberty
luteum. Thus, the hormonal system begins its new
ever the cause of this preovulatory LH and FSH surge,
the secretion of LH and, to a lesser extent, FSH. What-
as explained earlier, which leads to a terrific surge in
feedback stimulatory effect on the anterior pituitary,
to an abrupt halt. It is believed that the high level of
cycle, the decline in secretion of FSH and LH comes
3. Preovulatory Surge of LH and FSH Causes Ovulation.
FSH. This is the preovulatory surge of LH and FSH,
increase in the secretion of LH and, to a lesser extent,
pituitary gland. Then there is a sudden, marked
feedback effect, mainly of estrogen, on the anterior
new female monthly sexual cycle.
in the secretion of estrogen, reaching a peak estrogen
tion increases slightly as well. These hormones initiate
then, several days after menstruation begins, LH secre-
of FSH begins to increase again, as much as twofold;
the time that menstruation begins, pituitary secretion
these hormones. Therefore, a day or so later, at about
to a low ebb. This releases the hypothalamus and
terone, and inhibin from the corpus luteum decreases
total involution, and the secretion of estrogen, proges-
struation, the corpus luteum has regressed to almost
Two to 3 days before men-
tion. These effects are shown in Figure 81–3.
hypothalamus, causing the suppression of both FSH
esterone and estrogen, as well as the hormone inhibin.
the beginning of menstruation. During this time, the
of the cycle to explain is the events that occur during
The easiest part
Depression of the Pituitary Gonadotropins.
1. Postovulatory Secretion of the Ovarian Hormones, and
events.
rhythm of the female sexual cycle. It seems to operate
of the female hormonal system, we can attempt to
Now, after discussing much of the known information
Feedback Oscillation of the
ovulation will not occur.
Without this normal preovulatory surge of LH,
latory LH surge, and it has been suggested that this
of the female monthly cycle. (2) The granulosa cells of
extent, FSH; this is in sharp contrast to its normal neg-
of stimulating pituitary secretion of LH and, to a lesser
positive feedback effect
point in the cycle has a peculiar
follows: (1) It has been suggested that estrogen at this
known. However, several possible explanations are as
The cause of this abrupt surge in LH secretion is not
tion of LH causes ovulation to occur.
increases about twofold. The greatly increased secre-
abruptly sixfold to eightfold, and secretion of FSH
slightly suppressed. Then secretion of LH increases
estrogens. During this period, secretions of both FSH
cles, as well as rapidly accelerating secretion of ovarian
the latter part of the first half of the ovarian cycle will
The figure shows a much smaller preovulatory surge
ovulation. This effect is demonstrated in Figure 81–3.
For reasons not completely understood, the anterior
Ovulation—The Preovulatory LH Surge
Positive Feedback Effect of Estrogen Before
Female Physiology Before Pregnancy and Female Hormones
Chapter 81
1021
pituitary gland secretes greatly increased amounts of
LH for 1 to 2 days beginning 24 to 48 hours before
of FSH as well.
Experiments have shown that infusion of estrogen
into a female above a critical rate for 2 to 3 days during
cause rapidly accelerating growth of the ovarian folli-
and LH by the anterior pituitary gland are at first
ative feedback effect that occurs during the remainder
the follicles begin to secrete small but increasing quan-
tities of progesterone a day or so before the preovu-
might be the factor that stimulates the excess LH
secretion.
Hypothalamic-Pituitary-Ovarian
System
about the interrelations of the different components
explain the feedback oscillation that controls the
in approximately the following sequence of three
the postovulatory phase—between ovulation and
corpus luteum secretes large quantities of both prog-
All these hormones together have a combined nega-
tive feedback effect on the anterior pituitary gland and
and LH secretion and decreasing them to their lowest
levels about 3 to 4 days before the onset of menstrua-
2. Follicular Growth Phase.
anterior pituitary from the negative feedback effect of
new ovarian follicle growth and a progressive increase
secretion at about 12.5 to 13 days after the onset of the
During the first 11 to 12 days of this follicle growth,
the rates of pituitary secretion of the gonadotropins
FSH and LH decrease slightly because of the negative
which is followed by ovulation.
At
about 11.5 to 12 days after the onset of the monthly
estrogens at this time (or the beginning of proges-
terone secretion by the follicles) causes a positive
the great excess of LH leads to both ovulation and sub-
sequent development of and secretion by the corpus
round of secretions until the next ovulation.
If the preovulatory surge of LH is not of sufficient
because the LH surge is not potent enough at these
times to cause ovulation.
Puberty and Menarche
Puberty

menopausal women can likely avoid severe symptoms.
toms, and by gradually decreasing the dose, post-
treatment. If counseling fails, daily administration of
out the body. These symptoms are of sufficient magni-
(6) occasionally various psychotic states, and (7)
of dyspnea, (3) irritability, (4) fatigue, (5) anxiety,
by extreme flushing of the skin, (2) psychic sensations
of the body, including (1) “hot flushes” characterized
devoid of these hormones. The loss of estrogens often
At the time of menopause, a woman must readjust
the ovaries falls virtually to zero.
licles become atretic, the production of estrogens by
tinuous quantities, but as the remaining primordial fol-
Figure 81–9, the gonadotropins FSH and LH (mainly
gonadotropins FSH and LH. Instead, as shown in
production falls below a critical value, the estrogens
primordial follicles approaches zero. When estrogen
and, as shown in Figure 81–10, the production of
degenerate. At about age 45 years, only a few primor-
follicles and ovulate, and hundreds of thousands of ova
ovaries. Throughout a woman’s reproductive life,
The cause of menopause is “burning out” of the
menopause.
cycle ceases and the female sex hormones diminish to
shown in Figure 81–10. The period during which the
months to a few years, the cycle ceases altogether, as
irregular, and ovulation often fails to occur.After a few
At age 40 to 50 years, the sexual cycle usually becomes
secretion beyond menopause.
and, finally, (5) almost no estrogen or progesterone
estrogen secretion toward the end of reproductive life,
of reproductive life, (4) the progressive decrease in
during the monthly sexual cycle, (3) the further
gen secretion at puberty, (2) the cyclical variation
Figure 81–10 shows (1) the increasing levels of estro-
where in the brain, perhaps somewhere in the limbic
fore, it is now believed that the onset of puberty is
area of brain to cause the secretion is lacking. There-
hormone, but the appropriate signal from some other
during childhood. Experiments have shown that
male, and for reasons not understood, the hypothala-
priately stimulated. However, as is also true in the
In the female, as in the male, the infantile pituitary
11 and 16 years in girls (average, 13 years).
life, as shown in Figure 81–9, and usually culminating
by the pituitary, beginning in about the eighth year of
menstruation. The period of puberty is caused by a
1022
Unit XIV
Endocrinology and Reproduction
gradual increase in gonadotropic hormone secretion
in the onset of puberty and menstruation between ages
gland and ovaries are capable of full function if appro-
mus does not secrete significant quantities of GnRH
the hypothalamus itself is capable of secreting this
initiated by some maturation process that occurs else-
system.
increase in estrogen secretion during the first few years
Menopause
almost none is called
about 400 of the primordial follicles grow into mature
dial follicles remain to be stimulated by FSH and LH,
estrogens by the ovaries decreases as the number of
can no longer inhibit the production of the
FSH) are produced after menopause in large and con-
her life from one that has been physiologically stimu-
lated by estrogen and progesterone production to one
causes marked physiological changes in the function
decreased strength and calcification of bones through-
tude in about 15 per cent of women to warrant
estrogen in small quantities usually reverses the symp-
0
80
70
60
50
40
30
20
Female
Male
Puberty
Menopause
10
0
60
50
40
30
20
10
Age (yr)
Total urinary gonadotropins
(rat units/24 hr)
cially abrupt increase in gonadotropic hormones at menopause in
Total rates of secretion of gonadotropic hormones throughout the
Figure 81–9
sexual lives of female and male human beings, showing an espe-
the female.
0
12
13
40
50
60
0
400
300
300
100
Age (yr)
Estrogens excreted in urine
(
m
g/24 hr)
Puberty
Menopause
Estrogen secretion throughout the sexual life of the female human
Figure 81–10
being.
emission and ejaculation in the male, and it may help
The female orgasm is analogous to
initiated that cause the female orgasm, also called
conditioning signals from the cerebrum, reflexes are
maximum intensity, and especially when the local
When local sexual stimulation reaches
climaxes.
by a dry vagina. A massaging sensation constitutes
than an irritative sensation, which may be provoked
glands. This lubrication is necessary during intercourse
lubrication during sexual intercourse, although much
the introitus. This mucus is responsible for much of the
Bartholin’s glands located beneath the labia minora
stimulation for ejaculation to occur.
that the introitus tightens around the penis; this aids
polypeptide (VIP) at the nerve endings. This allows
of acetylcholine, nitric oxide, and vasoactive intestinal
of the erectile tissue, probably resulting from release
stimulation, parasympathetic signals dilate the arteries
the external genitalia. In the early phases of sexual
penis. This erectile tissue, like that of the penis, is
female sexual organs.
transmitted to the cerebrum. Also, local reflexes inte-
these signals have entered the spinal cord, they are
through the pudendal nerve and sacral plexus. Once
As in the male, the sexual sensory signals are trans-
tiating sexual sensations.
The glans of the
other perineal regions can create sexual sensations.
and other types of stimulation of the vulva, vagina, and
reaching a peak near the time of ovulation, probably
Desire also changes during the monthly sexual cycle,
ological drive, although sexual desire does increase in
woman’s background training as well as on her physi-
female sexual act. Such desire is based largely on a
desire, and this aids greatly in the performance of the
Thinking sexual thoughts can lead to female sexual
sexual act, successful performance of the female sexual
exists.
bleeding from this endometrium. In fact, bleeding is
which exert the usual estrogenic effects, including
These tumors secrete large quantities of estrogens,
occurring more often after menopause than before.
can develop in an ovary,
feminizing tumor develops.
hormones. Consequently, hypersecretion of feminizing
pituitary, and this limits the production of ovarian
ovarian hormones by the ovaries is a rare clinical entity,
of the preovulatory surge of LH, which is necessary for
frequently associated with failure of ovulation, presum-
altogether (amenorrhea). Prolonged ovarian cycles are
between menstrual periods, or menstruation may cease
not occur normally. Instead, several months may elapse
the ovarian cycle often does
small quantities of estrogens as a result of other factors,
order to cause rhythmical sexual cycles. Consequently,
cussion of menopause, the quantity of estrogens pro-
Irregularity of Menses, and Amenorrhea Caused by
menopause.
thinner. The same changes occur in women after
and become pendulous, and the pubic hair becomes
becomes thin and easily damaged. The breasts atrophy
vagina becomes smaller, and the vaginal epithelium
that the uterus becomes almost infantile in size, the
removed, the sexual organs regress to some extent so
When the ovaries of a fully developed woman are
early as they do in a normal woman. Consequently, the
organs remain infantile. Especially characteristic of
sexual characteristics do not appear, and the sexual
occurs. In this condition, the usual secondary
eunuchism
they become nonfunctional before puberty,
cells. When ovaries are absent from birth or when
can result from poorly formed ovaries, lack of ovaries,
Abnormalities of Secretion
Female Physiology Before Pregnancy and Female Hormones
Chapter 81
1023
by the Ovaries
Hypogonadism.
Less than normal secretion by the ovaries
or genetically abnormal ovaries that secrete the wrong
hormones because of missing enzymes in the secretory
female
this condition is prolonged growth of the long bones
because the epiphyses do not unite with the shafts as
female eunuch is essentially as tall as or perhaps even
slightly taller than her male counterpart of similar
genetic background.
Hypogonadism.
As pointed out in the preceding dis-
duced by the ovaries must rise above a critical value in
in hypogonadism or when the gonads are secreting
such as hypothyroidism,
ably because of insufficient secretion of LH at the time
ovulation.
Hypersecretion by the Ovaries.
Extreme hypersecretion of
because excessive secretion of estrogens automatically
decreases the production of gonadotropins by the
hormones is usually recognized clinically only when a
A rare granulosa cell tumor
hypertrophy of the uterine endometrium and irregular
often the first and only indication that such a tumor
Female Sexual Act
Stimulation of the Female Sexual Act.
As is true in the male
act depends on both psychic stimulation and local
sexual stimulation.
proportion to the level of sex hormones secreted.
because of the high levels of estrogen secretion during
the preovulatory period.
Local sexual stimulation in women occurs in more
or less the same manner as in men because massage
clitoris is especially sensitive for ini-
mitted to the sacral segments of the spinal cord
grated in the sacral and lumbar spinal cord are at least
partly responsible for some of the reactions in the
Female Erection and Lubrication.
Located around the
introitus and extending into the clitoris is erectile
tissue almost identical to the erectile tissue of the
controlled by the parasympathetic nerves that pass
through the nervi erigentes from the sacral plexus to
rapid accumulation of blood in the erectile tissue so
the male greatly in his attainment of sufficient sexual
Parasympathetic signals also pass to the bilateral
and cause them to secrete mucus immediately inside
is also provided by mucus secreted by the vaginal
epithelium and a small amount from the male urethral
to establish a satisfactory massaging sensation rather
the optimal stimulus for evoking the appropriate
reflexes that culminate in both the male and female
Female Orgasm.
sensations are supported by appropriate psychic
the female climax.
hyposecretion of gonadotropic hormones, in which
sterility is failure to ovulate. This can result from
the ova themselves.
organs, in which case it must be assumed that the infer-
10 per cent of women are infertile. Occasionally, no
Abnormal Conditions That Cause Female Sterility.
to occur and a new cycle to begin.
occur. Then the drug is stopped, allowing menstruation
begun in the early stages of the monthly cycle and con-
The drug is usually
odrel, ethynodiol,
norethindrone, norethyn-
Two of the most commonly used synthetic estrogens
destructive propensity of the liver, thus allowing oral
testinal tract into the portal circulation. However,
and synthetic progestins. The main reason for using syn-
Therefore, almost all “pills” used for the control of fer-
terone, especially the 19-norsteroids, along with small
cause abnormal menstrual bleeding patterns. However,
effects. For instance, too much of either hormone can
suppress ovulation but do not cause other, unwanted
The problem in devising methods for the hormonal
anterior pituitary that leads to the LH surge. The admin-
by the ovarian follicles, and this might be the necessary
gested that immediately before the surge occurs, there
fully understood. However, experimental work has sug-
Why the administration of estrogen or progesterone
surge of LH secretion by the pituitary gland, which is
The reason for this is that appropriate administration of
the first half of the monthly cycle, can inhibit ovulation.
progesterone, if given in appropriate quantities during
regular.
used only when the periodicity of the menstrual cycle is
conception. But such a method of contraception can be
the 7th day of the cycle. Therefore, it is usually stated
cycle is 21 days, ovulation usually occurs within 1 day of
the 26th day of the cycle. Finally, if the periodicity of the
cycle is 40 days, ovulation usually occurs within 1 day of
day of the cycle. If, in contrast, the periodicity of the
days, ovulation usually occurs within 1 day of the 14th
strual cycle is regular, with an exact periodicity of 28
always between 13 and 15 days. Therefore, if the men-
time of ovulation. Yet the interval from ovulation until
course near the time of ovulation. The difficulty with
days.
female fertility during each month is short, about 4 to 5
up to a few hours after ovulation. Thus, the period of
fore, for fertilization to take place, intercourse must
in the female reproductive tract for up to 5 days. There-
tilization is to take place. A few sperm can remain fertile
fore, sperm must be available soon after ovulation if fer-
from the ovary probably no longer than 24 hours. There-
The ovum remains
Female Fertility
terized by relaxed peacefulness, an effect called
culmination of the sexual act, this gives way during the
intense muscle tension throughout the body. But after
fertilization, the intense sexual sensations that develop
achieve. Whether this occurs in the human female is
of the fallopian tube in the cow in about 5 minutes, a
lated to cause increased transport of the sperm. A few
cal contractions of the uterus, which have been postu-
the pituitary. The oxytocin causes increased rhythmi-
the posterior pituitary gland to secrete oxytocin; this
Second, in many lower animals, copulation causes
minutes, thus allowing easy transport of the sperm.
subject is scanty, however. Also, the orgasm seems to
the uterus toward the ovum; information on this
the male. It is possible that these reflexes increase
female contract rhythmically, which results from spinal
First, during the orgasm, the perineal muscles of the
this are as follows.
function of the female orgasm. Possible reasons for
by artificial methods, thus indicating an important
promote fertilization of the ovum. Indeed, the human
1024
Unit XIV
Endocrinology and Reproduction
female is known to be somewhat more fertile when
inseminated by normal sexual intercourse rather than
cord reflexes similar to those that cause ejaculation in
uterine and fallopian tube motility during the orgasm,
thus helping to transport the sperm upward through
cause dilation of the cervical canal for up to 30
effect is probably mediated through the brain amyg-
daloid nuclei and then through the hypothalamus to
sperm have been shown to traverse the entire length
rate at least 10 times as fast as that which the swim-
ming motions of the sperm themselves could possibly
unknown.
In addition to the possible effects of the orgasm on
during the orgasm also pass to the cerebrum and cause
succeeding minutes to a sense of satisfaction charac-
resolution.
Fertile Period of Each Sexual Cycle.
viable and capable of being fertilized after it is expelled
occur sometime between 4 and 5 days before ovulation
Rhythm Method of Contraception.
One of the commonly
practiced methods of contraception is to avoid inter-
this method of contraception is predicting the exact
the next succeeding onset of menstruation is almost
that avoidance of intercourse for 4 days before the cal-
culated day of ovulation and 3 days afterward prevents
Hormonal Suppression of Fertility—“The Pill.”
It has long
been known that administration of either estrogen or
either of these hormones can prevent the preovulatory
essential in causing ovulation.
prevents the preovulatory surge of LH secretion is not
is probably a sudden depression of estrogen secretion
signal that causes the subsequent feedback effect on the
istration of sex hormones (estrogens or progesterone)
could prevent the initial ovarian hormonal depression
that might be the initiating signal for ovulation.
suppression of ovulation has been in developing appro-
priate combinations of estrogens and progestins that
use of certain synthetic progestins in place of proges-
amounts of estrogens usually prevents ovulation yet
allows an almost normal pattern of menstruation.
tility consist of some combination of synthetic estrogens
thetic estrogens and progestins is that the natural hor-
mones are almost entirely destroyed by the liver within
a short time after they are absorbed from the gastroin-
many of the synthetic hormones can resist this
administration.
are ethinyl estradiol and mestranol. Among the most
commonly used progestins are
and norgestrel.
tinued beyond the time that ovulation would normally
About 5 to
abnormality can be discovered in the female genital
tility is due to either abnormal physiological function of
the genital system or abnormal genetic development of
Probably by far the most common cause of female
case the intensity of the hormonal stimuli is simply
of female infertility. JAMA 290:1767, 2003.
Smith S, Pfeifer SM, Collins JA: Diagnosis and management
practice. N Engl J Med 348:618, 2003.
Riggs BL, Hartmann LC: Selective estrogen-receptor mod-
resorption. J Clin Invest 106:1203, 2000.
Riggs BL: The mechanisms of estrogen regulation of bone
in estrogen action. Annu Rev Physiol 63:165, 2001.
Pettersson K, Gustafsson JA: Role of estrogen receptor beta
tives. N Engl J Med 349:1443, 2003.
Petitti DB: Combination estrogen-progestin oral contracep-
Physiol Rev 80:1, 2000.
Niswender GD, Juengel JL, Silva PJ, et al: Mechanisms con-
gen action. Physiol Rev 81:1535, 2001.
Nilsson S, Makela S, Treuter E, et al: Mechanisms of estro-
291:1610, 2004.
gen for treatment of hot flashes: scientific review. JAMA
Nelson HD: Commonly used types of postmenopausal estro-
16:251, 2001.
membrane, cytosolic, and nuclear effects. News Physiol Sci
Nadal A, Diaz M, Valverde MA: The estrogen trinity:
replacement therapy. N Engl J Med 345:34, 2001.
Manson JE, Martin KA: Postmenopausal hormone-
regulate bone mass. J Clin Invest 111:1641, 2003.
Lorenzo J: A new hypothesis for how sex steroid hormones
Hamilton-Fairley D, Taylor A: Anovulation. BMJ 327:546,
duction and actions of estrogens. N Engl J Med 346:340,
Gruber CJ, Tschugguel W, Schneeberger C, Huber JC: Pro-
Compston JE: Sex steroids and bone. Physiol Rev 81:419,
therapy. Lancet 360:942, 2002.
Beral V, Banks E, Reeves G: Evidence from randomised
menopausal? JAMA 289:895, 2003.
Bastian LA, Smith CM, Nanda K: Is this woman peri-
porosis. JAMA 285:1415, 2001.
Altkorn D, Vokes T: Treatment of postmenopausal osteo-
low-grade infection or inflammation, or abnormal hor-
“threads.” Abnormalities of the cervix itself, such as
of ovulation, the hormonal environment of estrogen
mal mucus by the uterine cervix. Ordinarily, at the time
infertility.
of gonococcal infection, but with modern therapy,
the past, such inflammation occurred mainly as a result
causes fibrosis in the tubes, thereby occluding them. In
that is,
ingitis,
lopian tubes, either at the fimbriated ends or elsewhere
abdominal cavity. Often, endometriosis occludes the fal-
pelvis, and this fibrosis sometimes so enshrouds
ovaries. Endometriosis causes fibrosis throughout the
cavity surrounding the uterus, fallopian tubes, and
endometriosis,
with this hormone.
simultaneously; this results in multiple births, an effect
erful stimulator of ovulation. However, excess use of
This hormone, although secreted by the placenta, has
man chorionic gonadotropin,
illustrated in Figure 81–11.
temperature chart, showing the point of ovulation, is
rise coming abruptly at the time of ovulation. Such a
the body temperature about 0.5°F, with the temperature
progesterone during the latter half of the cycle raises
body temperature throughout the cycle. Secretion of
metabolism, during the latter half of the sexual cycle;
surge in pregnanediol, the end product of progesterone
effects, the cycle can be assumed to be anovulatory.
of anovulatory cycles. In the absence of progestational
body, because the normal increase in progesterone
determine whether ovulation occurs. These methods are
sterile women, special methods are often used to
outsides of the ovaries, making ovulation difficult.
instance, thick ovarian capsules occasionally exist on the
abnormal ovaries that do not allow ovulation. For
insufficient to cause ovulation, or it can result from
Female Physiology Before Pregnancy and Female Hormones
Chapter 81
1025
Because of the high incidence of anovulation in
based mainly on the effects of progesterone on the
secretion usually does not occur during the latter half
One of these tests is simply to analyze the urine for a
the lack of this substance indicates failure of ovulation.
Another common test is for the woman to chart her
Lack of ovulation caused by hyposecretion of the
pituitary gonadotropic hormones can sometimes be
treated by appropriately timed administration of hu-
a hormone (discussed in
Chapter 82) that is extracted from the human placenta.
almost the same effects as LH and is therefore a pow-
this hormone can cause ovulation from many follicles
that has caused as many as eight babies (mostly
stillborn) to be born to mothers treated for infertility
One of the most common causes of female sterility is
a common condition in which endome-
trial tissue almost identical to that of the normal uterine
endometrium grows and even menstruates in the pelvic
the ovaries that an ovum cannot be released into the
along their extent.
Another common cause of female infertility is salp-
inflammation of the fallopian tubes; this
this is becoming a less prevalent cause of female
Still another cause of infertility is secretion of abnor-
causes the secretion of mucus with special charac-
teristics that allow rapid mobility of sperm into the
uterus and actually guide the sperm up along mucous
monal stimulation of the cervix can lead to a viscous
mucous plug that prevents fertilization.
References
trials on the long-term effects of hormone replacement
2001.
2002.
2003.
trolling the function and life span of the corpus luteum.
ulators—mechanisms of action and application to clinical
0 2
4 6
8 10 12 14 16 18 20 22 24 26 28
0
99
°
98
°
97
°
Day of cycle
Body temperature (
°
F)
Ovulation
Elevation in body temperature shortly after ovulation.
Figure 81–11

molecular specificity. Physiol Rev 82:923, 2002.
hormone receptor interactions: physiological flexibility by
Vasudevan N, Ogawa S, Pfaff D: Estrogen and thyroid
local regulation of the growth plate. Endocr Rev 24:782,
van der Eerden BC, Karperien M, Wit JM: Systemic and
the brain: where will it end? Endocrinology 145:1069,
Toran-Allerand CD: A plethora of estrogen receptors in
of the onset of puberty in primates. Endocr Rev 22:111,
Terasawa E, Fernandez DL: Neurobiological mechanisms
1026
Unit XIV
Endocrinology and Reproduction
2001.
2004.
2003.
