Cough and Hemoptysis
Dr.Bilal Natiq NuamanLecturer at Ibn-Sina Medical College
C.A.B.M. ,F.I.B.M.S. ,D.I.M. ,M.B.Ch.B.
2013-2014
Cough
Definition:‘A Cough is a forced expulsive manoeuvre, usually against a closed glottis and which is associated with a characteristic sound’
Cough is the single most common respiratory complaint for which patients seek care
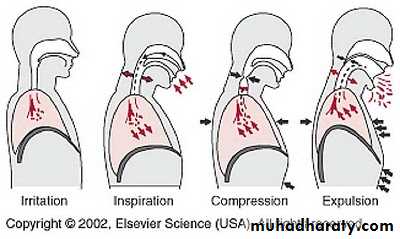
Phases of cough1. Inspiratory Phase
2. Compressive Phase3. Expiratory Phase
4. Relaxation Phase
Importance of Cough
1- Defense mechanism (physiological natural reflex )
Providing a normal protective mechanism for clearing the tracheobronchial tree free of secretions and foreign material.2-Complication of its force
excessive coughing can be exhausting; can be complicated by vomiting, syncope, muscular pain, or rib fractures; and can aggravate abdominal or inguinal hernias , urinary incontinence and Uterine prolapse .3-Symptom of disease (associated with many medical diseases and conditions)
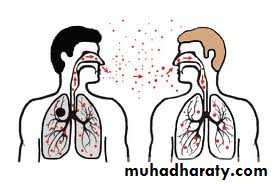
4- transmit infections to others by air droplets Diseases that are commonly spread by coughing or sneezing include:
Bacterial Meningitis
Chickenpox
Common cold
Influenza
Mumps
Strep throat
Tuberculosis
Measles
Rubella
Whooping cough
5-Impaired Cough in a person
(due to Altered conscious level- anesthesia, narcotics, sedatives, alcohol, coma, stroke, seizure, SLEEP,and Neuromuscular diseases)increase the risk for retained airway secretions and aspirated material, predisposing to infection, atelectasis, and respiratory compromise.
History
1-Onset and Duration :Acute : < 3weeks
Subacute :3-8 weeks
Chronic : > 8 weeks
2-Character :
Bovine with Hoarsness---- Left recurrent laryngeal nerve palsy causing left vocal cord paralysis due to CA LungBarking with Hoarsness and Stridor ----- Acute Epiglottitis, Laryngitis , CA Larynx
Wheezy ------COPD , Asthma
3-Timing and associated features :
Nocturnal ----- Asthma , CHFEarly Morning ----- Bronchiectasis , Chronic Bronchitis ,Asthma
Recumbent ------- Postnasal drip (PND) , CHF, Gastroesophageal reflux disease (GERD)
Change position (Standing) --------- Bronchiectasis
4-With or w/out Sputum :
Dry Cough ------ without sputum
Causes of dry cough (Asthma ,Viral infection of respiratory system, Interstitial Lung Disease)
Productive Cough ----- with sputum
Causes of Productive Cough (Respiratory Infections , COPD , Bronchiectasis)
5-With or w/out Blood :
Hemoptysis -------- With blood
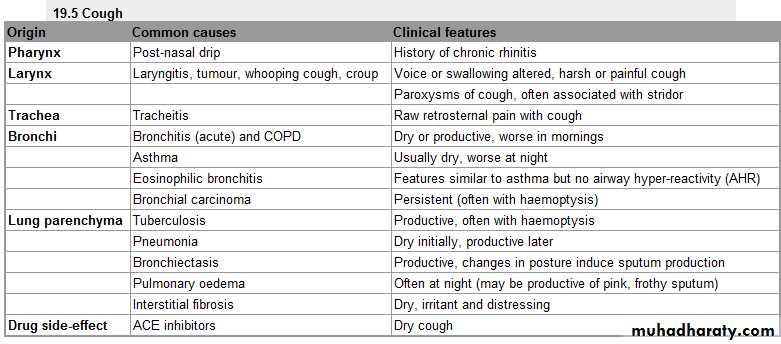
1-Types analysis Sputum
2-Amount of Sputum
How much sputum is coughed up each day ? Is it a small (a teaspoonful) or large (a teacupful) amount?Bronchiectasis-------- large amount of purulent sputum to be coughed up mainly in morning on changing posture with a long history .
Rupture of a lung abscess ------ Sudden production of large amounts of purulent sputum on a single occasion .
Pulmonary Oedema ------ Large volumes of watery sputum with a pink tinge in an acutely dyspnic patient .
3-Colour of Sputum
Clear Sputum ------- COPD if there is no active infection.Yellow Sputum ------Acute lower respiratory tract infection(neutrophils) , and Asthma (eosinophils)
Green Sputum(purulent) ------- COPD ,Bronchiectasis (dead neutrophils)
Rusty Sputum ------ Pneumococcal Pneumonia
Black Sputum -------- Coal Dust Inhalation
4-Foul Smelling ------- Anaerobic bacterial infection , Bronchiectasis , Lung Abscess and Empyema .
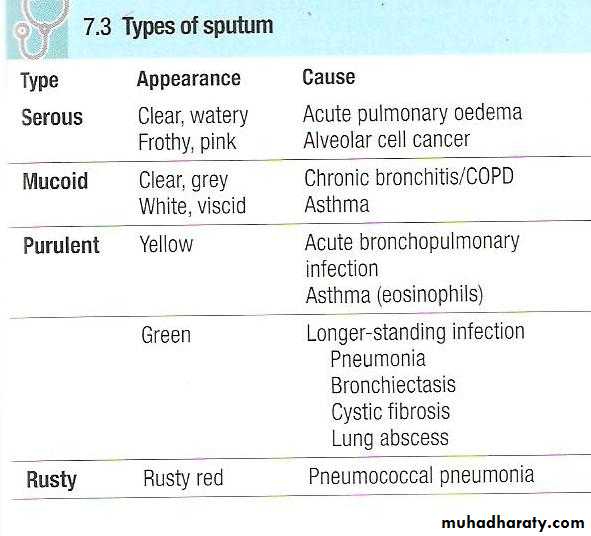
Classification of Cough
Acute Cough = < 3 Weeks DurationSubacute Cough 3-8 Weeks Duration
Chronic Cough > 8 Weeks DurationAcute Cough <3 weeks
Differential Diagnosis(CAUSES)Upper Respiratory Tract infections(URTI):
Viral syndromes, sinusitis , pertussis
URTI triggering exacerbations of Chronic Lung Disease eg Asthma/ COPD
Pneumonia
Left Ventricular Heart Failure
Foreign Body Aspiration
Red Flags in Acute Cough
THINK pneumonia, lung cancer, LVFGET a CHEST X-Ray
Symptoms
Haemoptysis
Breathlessness
Fever
Chest Pain
Weight Loss
Signs
TachypnoeaCyanosis
Dull chest
Bronchial Breathing
Crackles
Chronic Cough>8 weeks
Differential Diagnosis(CAUSES)SMOKER(Abnormal Chest X-ray)
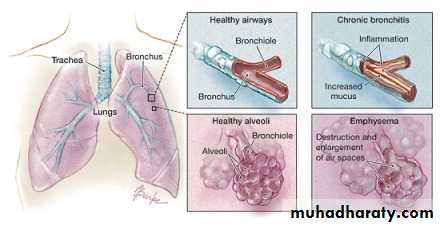
COPD :Chronic Bronchitis , Emphysema
CA Lung
NON-SMOKER(Normal Chest X-ray)
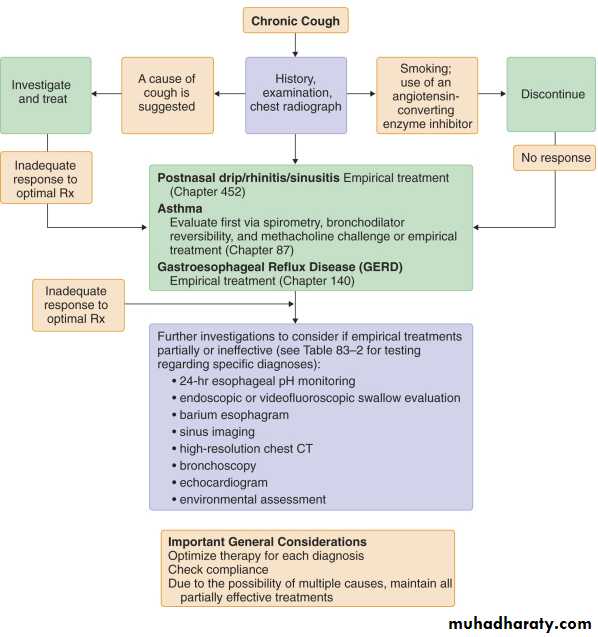
Drug(ACEI-Angiotensin Converting Enzyme Inhibitor-Captopril)
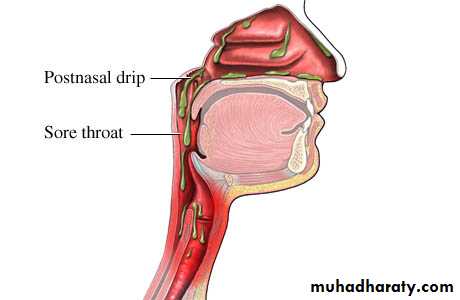
PND-Post Nasal Drip
Asthma-Cough Variant Asthma
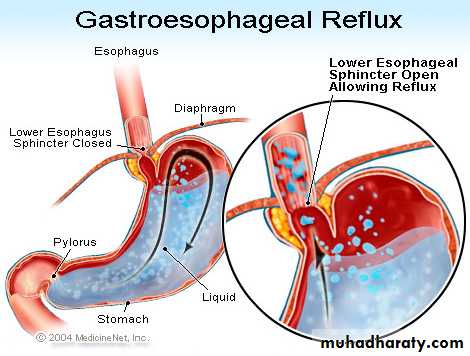
GERD-Gastroesophageal regurgitation disease
COPD
• Chronic Bronchitis :
defined clinically as Productive cough (cough with sputum expectoration ) in a chronic smoker for at least 3 months a year during a period of 2 consecutive years with exclusion of other causes of productive cough .
• Emphysema :
• defined pathologically as an abnormal permanent enlargement of air spaces distal to the terminal bronchioles, accompanied by the destruction of alveolar walls without obvious fibrosis.
Cough alone as a manifestation of asthma in the absence of wheezing, shortness of breath, and chest tightness is referred to as "cough-variant asthma
Clinical Diagnosis
Gold standard History (Episodic symptoms with specific aggravating factors, Family history)
Reversibility testing(Change in PFT before and after bronchodilation)
PEF monitoring(morning dipping of PEF serials)
Bronchoprovocation test (if normal pulmonary function test)
The best way to confirm asthma as a cause of cough is to demonstrate improvement in the cough with appropriate therapy for asthma
Post Nasal Drip refers to that sensation of having excess secretions (either thick or thin) drip down the back of your throat. Usually sinusitis, colds, allergies and other upper respiratory disorders are followed by post nasal drip.
Clinical Presentation:
• Dripping sensation , Tickle in the throat , Nasal congestion , Mucus in oropharynx , Cobblestone appearence of oropharynx
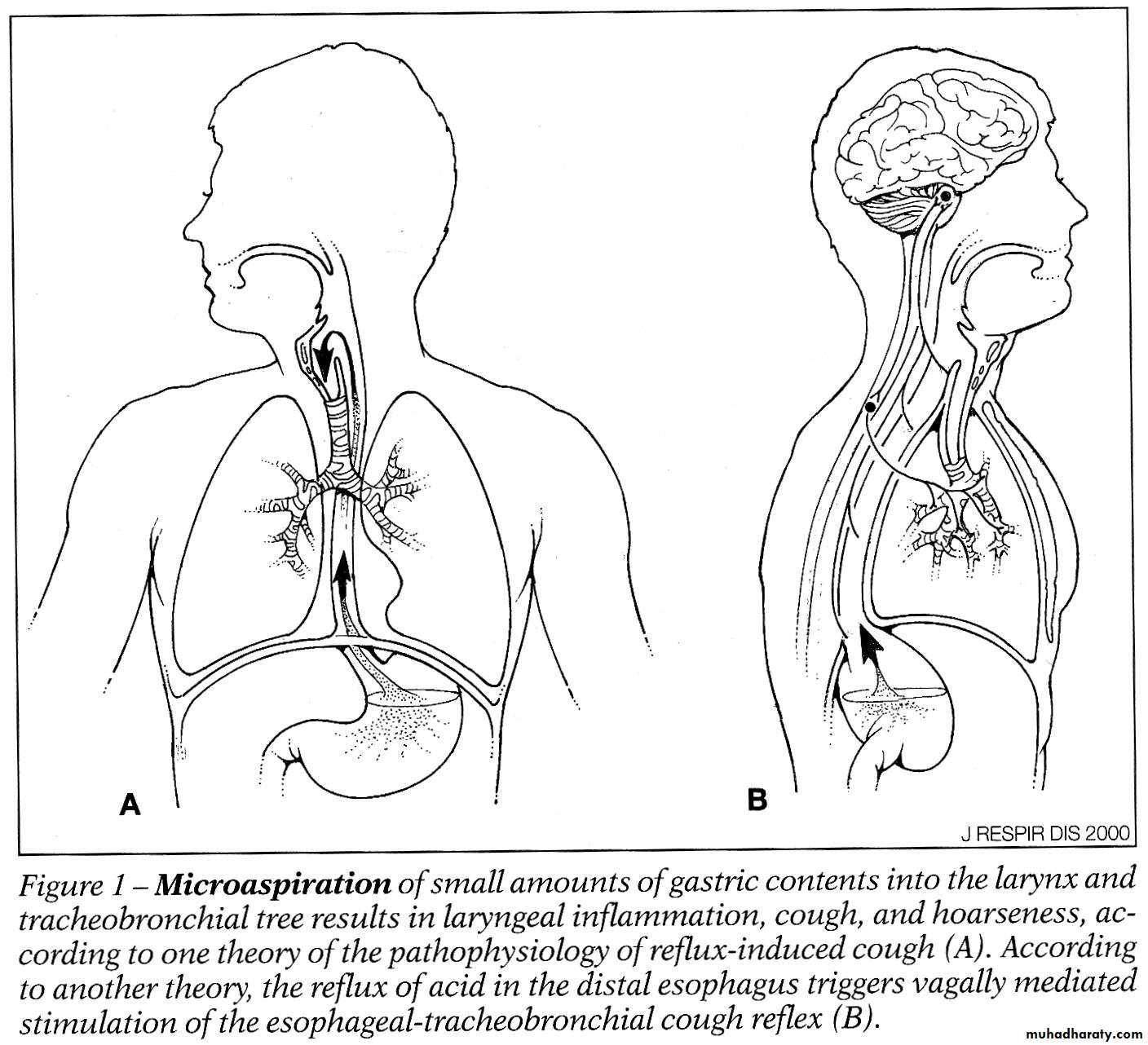
Gastroesophageal reflux disease (GERD) refers to acid reflux, or backward flow, of stomach acid and other contents into the esophagus. If stomach acid moves backward up the esophagus, reflexes result in spasm of the airways that can cause shortness of breath and coughing. In some individuals, no sensation of heartburn is felt and their only symptom may be cough.
Diagnostic tests:
24-hour esophageal pH probe (best)
OGD – Esophagogastrodudenoscope
Therapeutic trial: gastric acid suppression with proton pump inhibitor (e.g. omeprazole) for ≥ 2 months, combined with diet and lifestyle modification
ACE-Inhibitors and Chronic Cough
Incidence: 5-20%Onset: one week to six months
Mechanism
Bradykinin increase because it is Usually metabolized by ACE
Treatment: switch to Angiotensin II Receptor Blockers (ARBs)
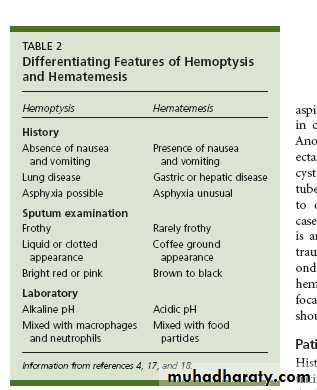
Hemoptysis
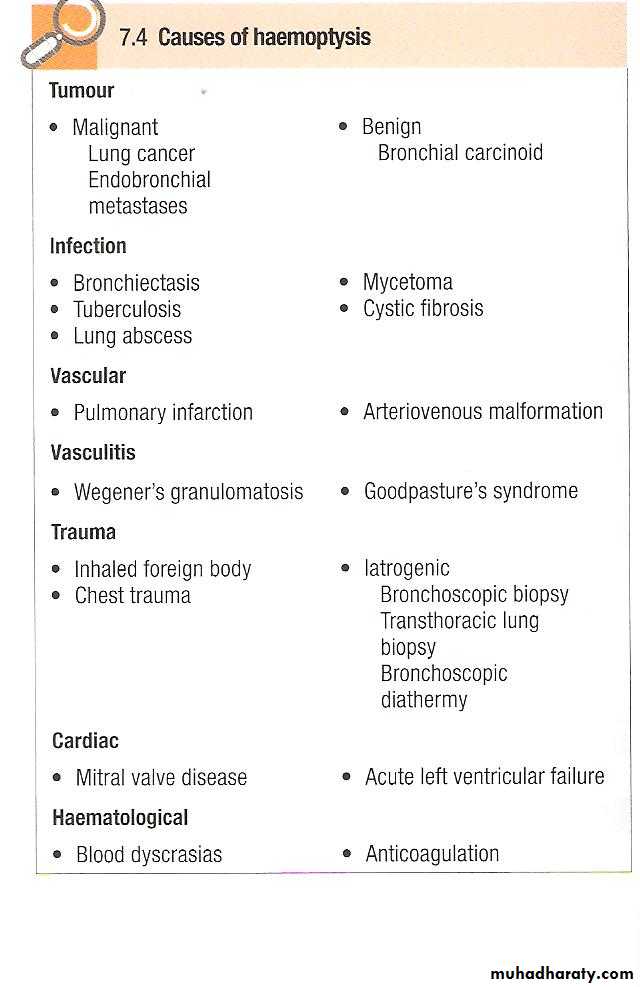
Coughing up blood, irrespective of the amount, is an alarming symptom and patients nearly always seek medical advice. A history should be taken to establish that it is true haemoptysis and not haematemesis, or gum or nose bleeding.Haemoptysis must always be assumed to have a serious cause until this is excluded .
A history of repeated small haemoptysis is highly suggestive of bronchial carcinoma.
Fever, night sweats and weight loss suggest tuberculosis. Pneumococcal pneumonia often causes 'rusty'-coloured sputum but can cause frank haemoptysis, as can all suppurative pneumonic infections including lung abscess. Bronchiectasis can cause catastrophic bronchial haemorrhage,, pulmonary thromboembolism is a common cause of haemoptysis and should always be considered.
Physical examination may reveal additional clues.
Finger clubbing suggests bronchial carcinoma or bronchiectasis;other signs of malignancy, such as cachexia, hepatomegaly and lymphadenopathy, should also be sought.
Fever, pleural rub or signs of consolidation occur in pneumonia or pulmonary infarction; a minority of patients with pulmonary infarction also have unilateral leg swelling or pain suggestive of deep venous thrombosis.
Rashes, haematuria and digital infarcts suggest an underlying systemic disease such as a vasculitis, which may be associated with haemoptysis.
In the vast majority of cases the haemoptysis itself is not life-threatening and a logical sequence of investigations should be followed: chest X-ray, which may give evidence of a localised lesion including pulmonary infarction, tumour (malignant or benign), pneumonia, mycetoma or tuberculosis
full blood count and clotting screen
bronchoscopy after acute bleeding has settled, which may reveal a central bronchial carcinoma (not visible on the chest X-ray) and permit biopsy and tissue diagnosis
CTPA, which may reveal underlying pulmonary thromboembolic disease or alternative causes of haemoptysis not seen on the chest X-ray (e.g. pulmonary arteriovenous malformation or small or hidden tumours).
Massive Hemoptysis:
It is coughing of about 600ml blood/24 h
Questions??