بسم الله الرحمن الرحيم
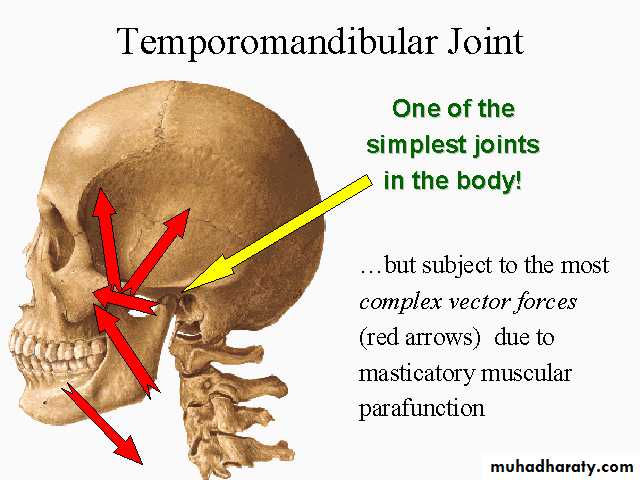
TEMPROMANDIBULAR JOINT DISORDERS
INTRODUCTIONIntro..
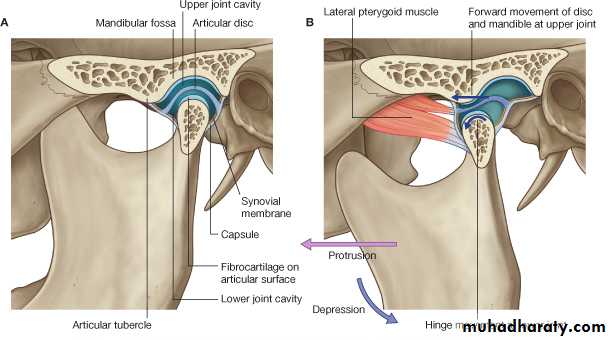
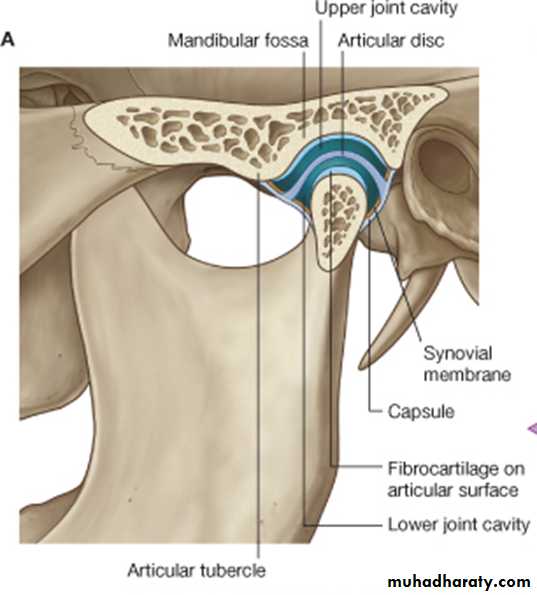
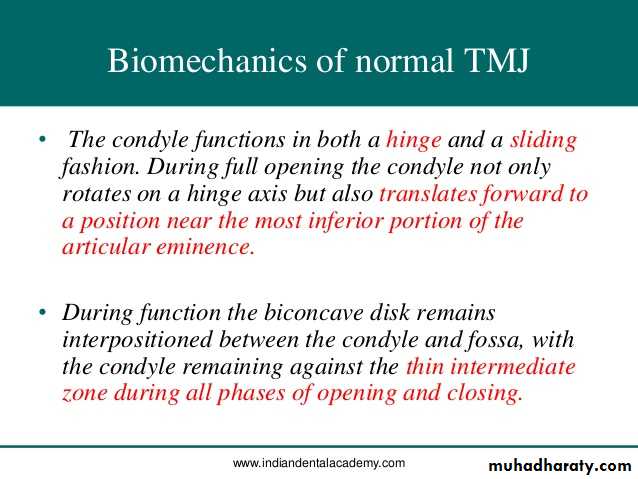
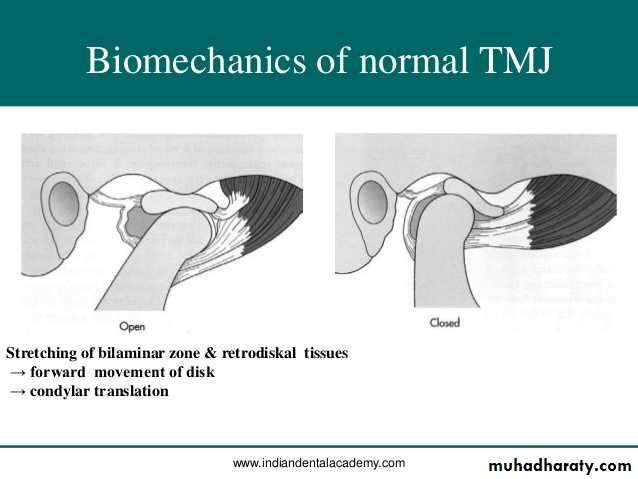
The TMJ is a synovial bilateral joint that permits the mandible to move as a unit with 2 functional patterns (gliding and hinge movements).Translatory movement – in the superior part of the joint as the disc and the condyle traverse anteriorly along the inclines of the anterior tubercle to provide an anterior and inferior movement of the mandible.
Mouth closed
Mouth open• Hinge movement – the inferior portion of the joint between the head of the condyle and the lower surface of the disc to permit opening of the mandible.
4 anatomical parts concerned with mandibular articulation:
Mandibular condyleMandibular fossa and articular eminence
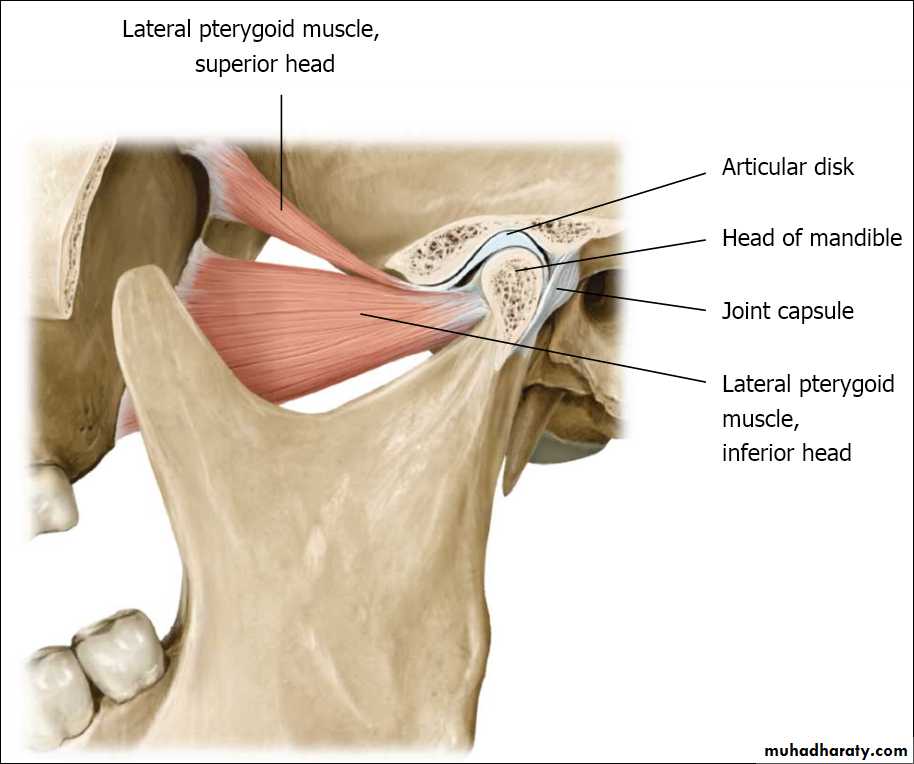
The articular disc
The articular capsule
The mandibular condyle articulates with the glenoid fossa and articular eminence of the temporal bone.
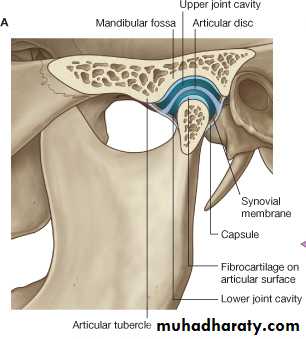
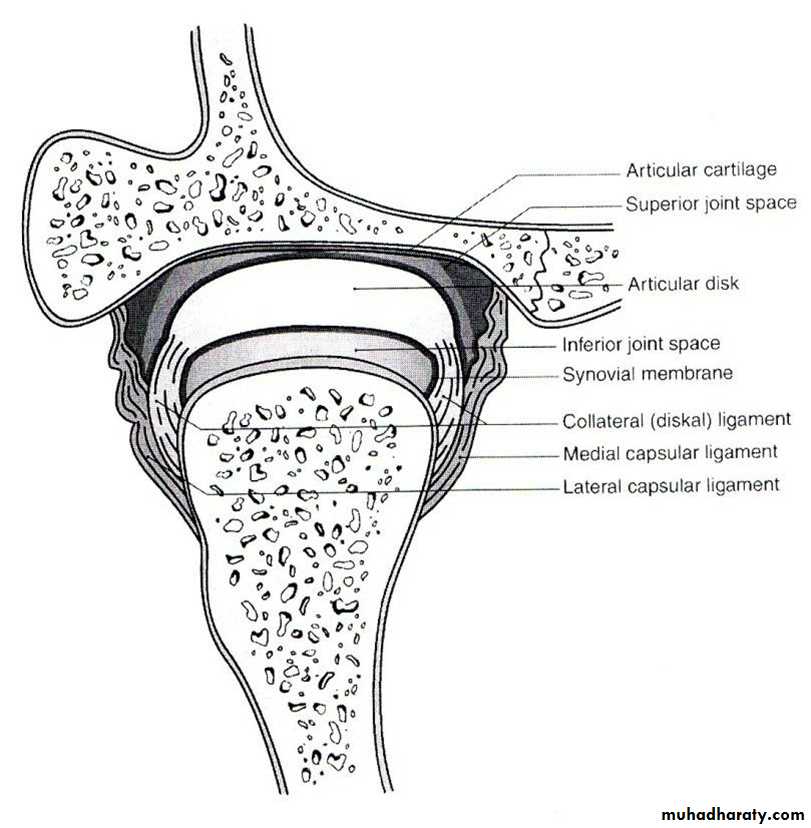
An articular disc separates the articular surfaces so that 2 cavities are present:
Upper compartment between the disc and temporal bone.
Lower compartment between the condyle and the disc
The joint capsule is attached below to the articular margin of the head of the condyle, and above to the margins of the glenoid fossa and articular eminence. The inner aspect of the capsule is lined by a synovial membrane.
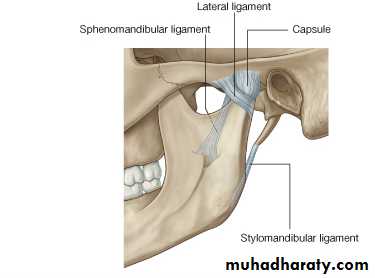
At the sides, the capsule is strengthened by collateral ligaments of which the lateral temporomandibular ligament is the strongest.
The lateral temporo-mandibular ligament is attached above to the zygoma, and below, it is attached to the lateral surfaces and posterior border of the neck of the mandible.
There are 2 accessory ligaments associated with the TMJ:
The stylomandibular ligament attaches to the styloid process and to the posterior border of the ramus.The sphenomandibular ligament extends between the spine of the sphenoid bone and the lingula of the mandible.
These ligaments limit the range of movement of the condyle preventing it from coming in contact with the tympanic plate behind and passing beyond the articular eminence in front.
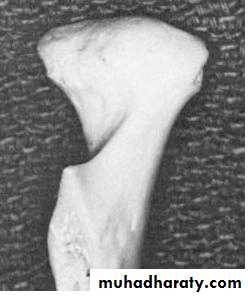
THE MANDIBULAR CONDYLE
It’s the articulating surface of the mandible.It is convex in all directions but wider
latero-medially than antero-posteriorly.
It has lateral and medial poles:
The medial pole is directed more posteriorly.
The long axis of the two poles deviate
• posteriorly and meets at the anterior
• border of the foramen magnum.
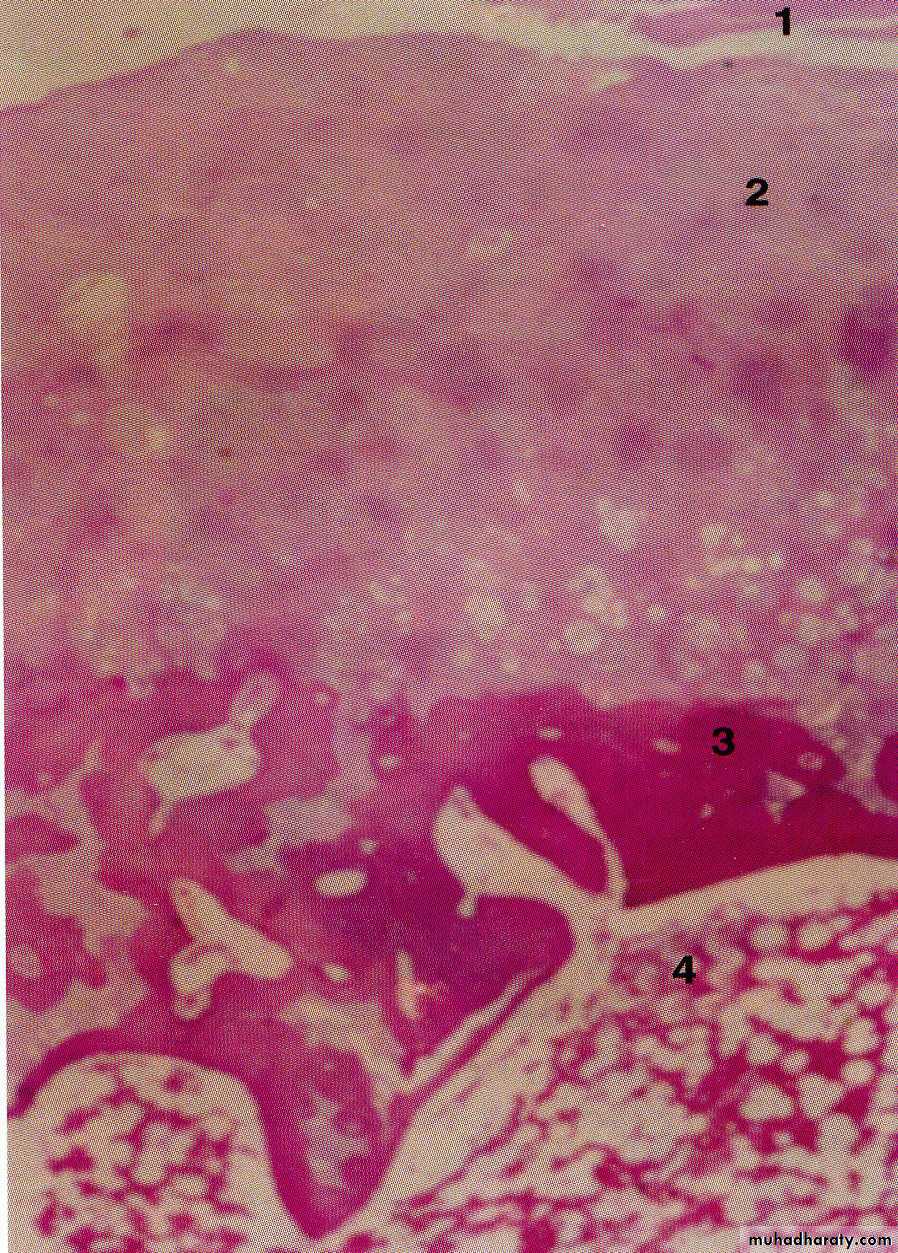
The fibrous articular covering of the condyle under the EM.
• Fibrous layer• Cartilage
• Bone
• Bone marrow
MANDIBULAR (GLENOID) FOSSA AND ARTICULAR EMINENCE
Glenoid fossa:
Posteriorly limited by the
• squamotympanic fissure.
Anterioly bounded by the
• articular eminence.
Roof: thin layer of compact
• bone separating the middle
• cranial fossa.
Articular eminence:
Composed of: Spongy bone
• covered by thin layer of compact
• bone.
Chondroid tissues commonly seen
• in the eminence.
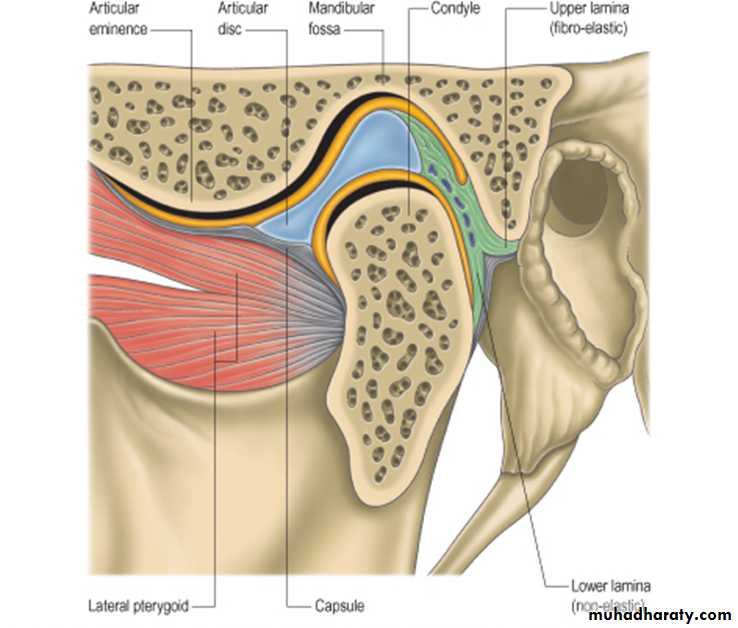
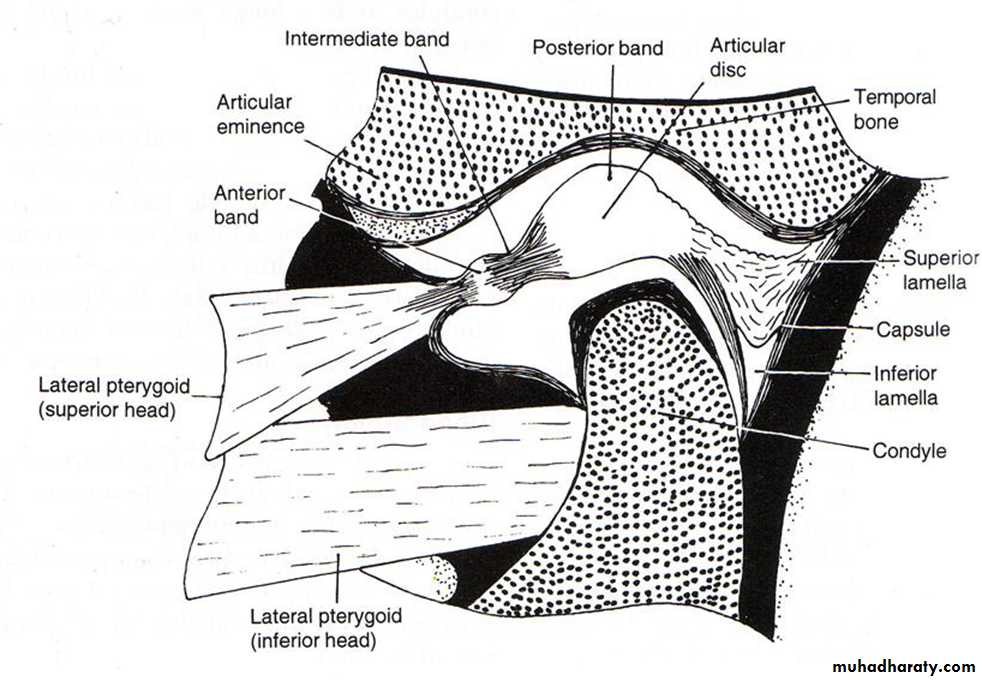
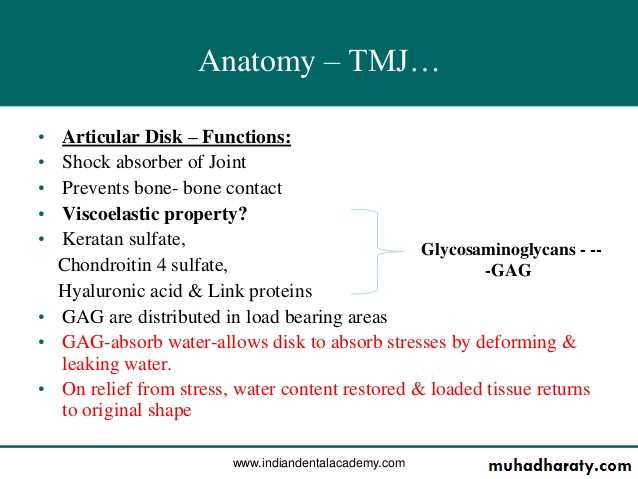
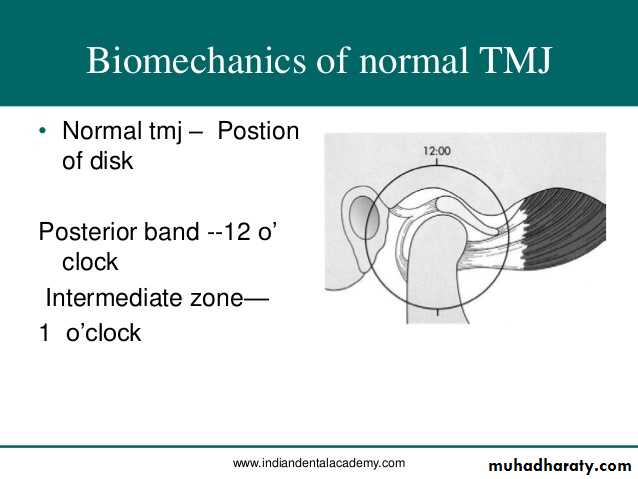
Interarticular disc (Meniscus)
Disk is fibrous, avascular, non inverted plateShape is oval, biconcave in sagittal section. It is thin in central part and
thick at posterior borders.
Attachment: Medial and lateral
poles of the condyle by medialand lateral ligaments.
Divide the joint into: Upper
(larger) compartment andlower (smaller) compartment.
Anterior border divides into upper and lower lamellae that run forward.
The upper lamella fuses with the anterior slope of the articular eminence.The lower lamella attaches to the front of the neck of the condyle.
Fibers of the superior head of the lateral pterygoid muscle is attached to the anterior border.
Posterior border divides into upper and lower lamellae
The upper lamella is fibrous and elastic and fuses with the capsule and is inserted in the squamotympanic fissure.The lower lamella, non elastic, attaches to the back of the condyle.
ARTICULATING CAPSULE AND LIGAMENTS AND SYNOVIAL MEMBRANE
The whole TMJ is enclosed in a fibrous capsule.It is attached to:
Articular tubercle (in front)
Lips of squamous tympanic fissure
• (posteriorly)
Borders of articulating glenoid fossa
Neck of the mandible. (below)
It is lined by synovial membrane.
Laterally, the capsule is reinforced by TMJ ligaments.
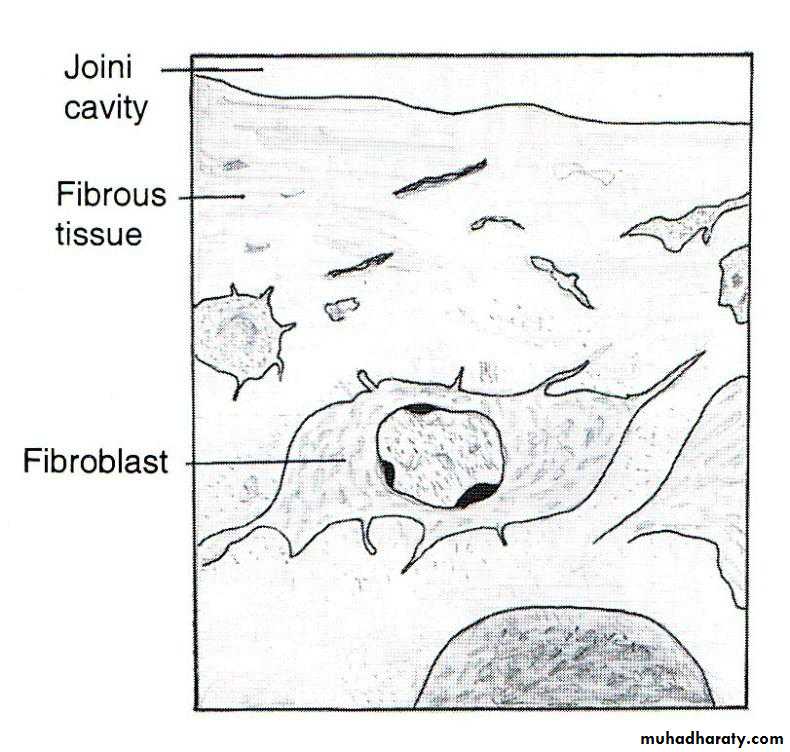
HISTOLOGY OF CAPSULE
Consists of 2 layers:Outer fibrous capsule – strengthen laterally to form the temporomandibular ligament.
Inner synovial layer – composed of thin connective tissue layer lined with:
Synovial cells
Type A : secretes hyaluronic acid
Type B : produces protein rich secretion.
Synovial membrane is very rich in blood supply and contains lymphatic vessels.
Synovial fluid
It is clear, straw-colored viscous fluid.
It diffuses out from the rich cappillary network of the synovial membrane.
Contains:
Hyaluronic acid which is highly viscous
May also contain some free cells mostly macrophages.
Functions:
Lubricant for articulating surfaces.
Carry nutrients to the avascular tissue of the joint.
Clear the tissue debris caused by normal wear and tear of the articulating surfaces.
Blood supply
4 arteries supply the joint:Superficial temporal
Deep auricular
Anterior tympanic
Ascending pharyngeal
Branches from the 4 approach the joint and penetrate the capsule.
Nerve supply
Branches from the mandibular nerve
Auriculotemporal nerve
Masseteric nerve
Deep temporal nerves
Supply all surfaces of the head, fossa, capsule and part of the disk.
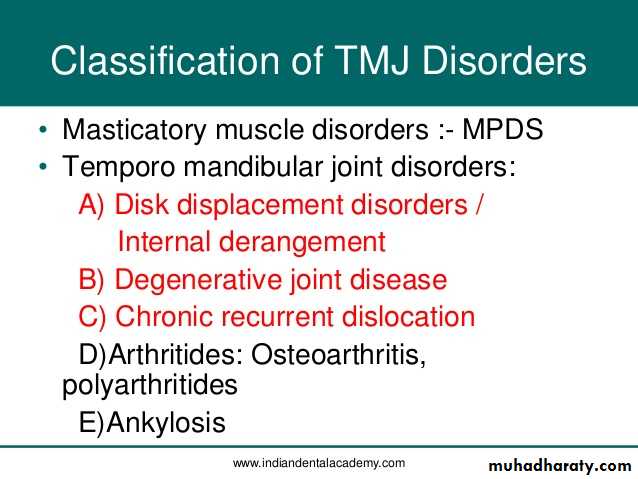
INTERNAL DERANGEMENT OF TMJ
Myofascial pain dysfunction syndromeDefinition
MPDS is a pain disorder, in which unilateral pain is referred from the trigger points in myofascial structures, to the muscles of the head and neck.MPDS is the most common cause of masticatory pain & limited function for which patient seeks dental consultation & the source of the pain treatment
Laskin (1969)- Myofascial Pain Dysfunction Syndrome.
He implicated psychophysiologic theory stating that psychological stress leads to myospasm & advised tranquilizers, muscle relaxants.Etiology
Tooth muscle theory- occlusal interference cause an altered proprioceptive feedback, leading to incoordination & spasm of muscles of mastication.
Prosthetic problems- faulty prosthesis, over closure, bilateral loss of molar teeth, increased vertical dimensions.
Malocclusion-
Oral habits (clenching, grinding of teeth), BRUXISM, anxiety.Psychophysiological theory- masticatory muscle spasm causes MPDS, degenerative arthritis & contracture arthritis.
Okeson, Jeffrey P. (2003). Textbook of Management of temporomandibular disorders and occlusion (5th ed.)
Clinical characteristics
Laskin’s Cardinal symptoms of MPDS :-• Pain or discomfort anywhere about the head or neck.
• Limitation of motion of the jaw.
• Joint noises– clicking, poping.
• Tenderness on palpation of the muscles of mastication.
• Negative characteristics:-
• Absence of clinical, radiographic or biochemical evidence of organic changes in TMJ.
• Lack of tenderness in TMJ area when palpated via external auditory meatus.
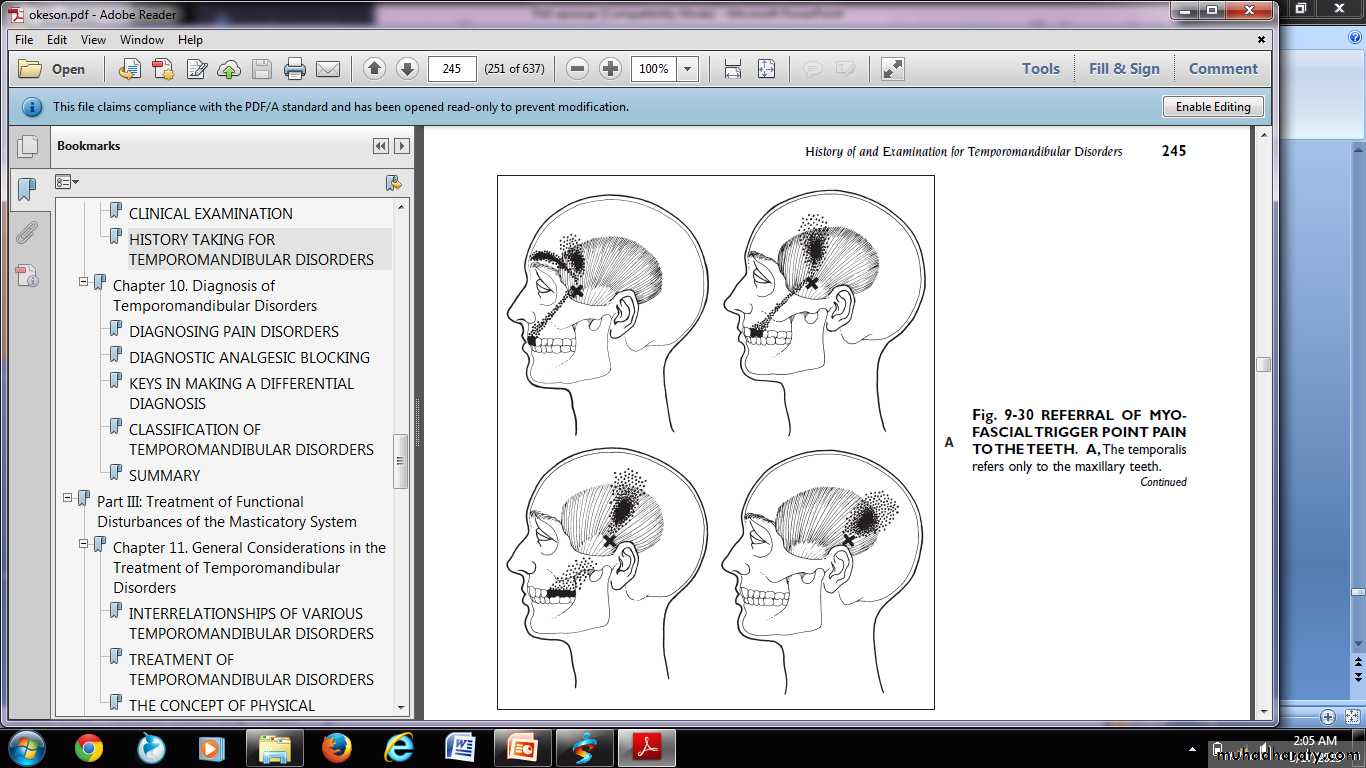
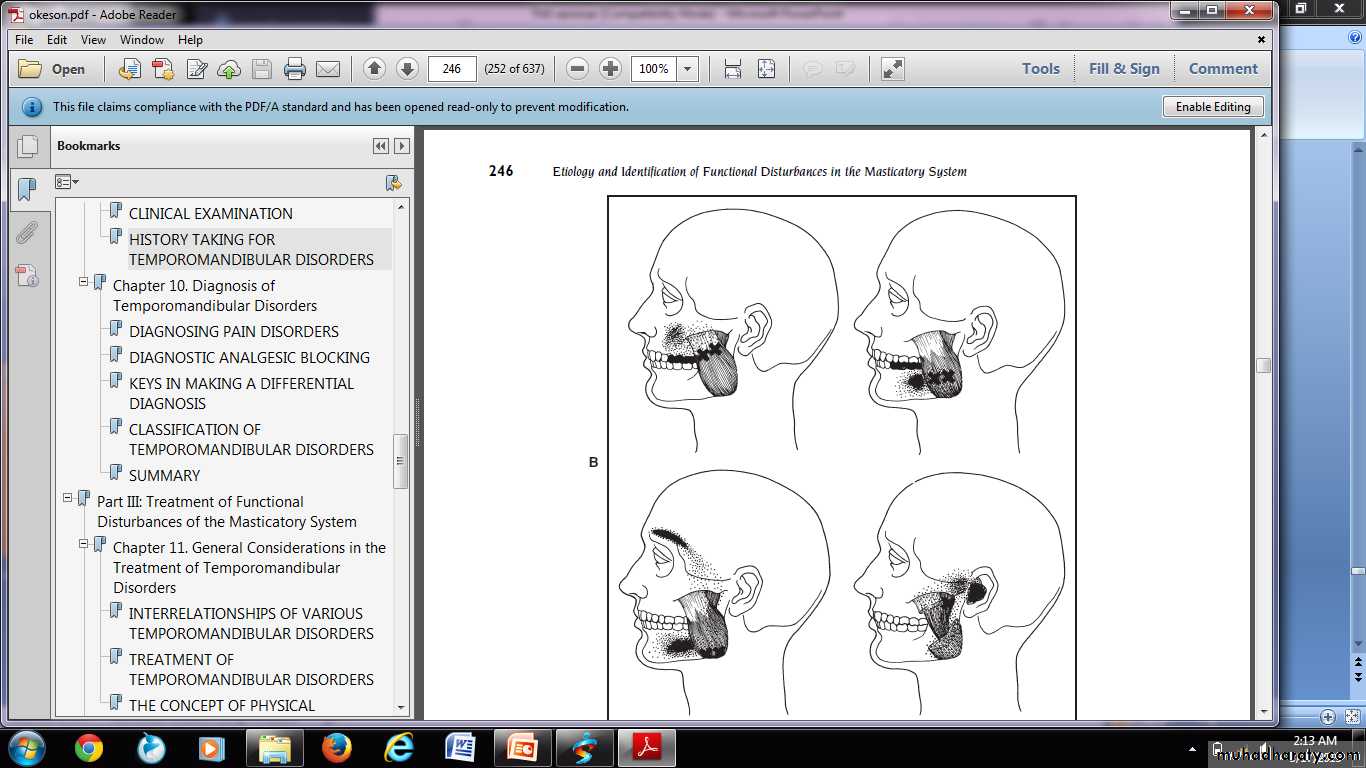
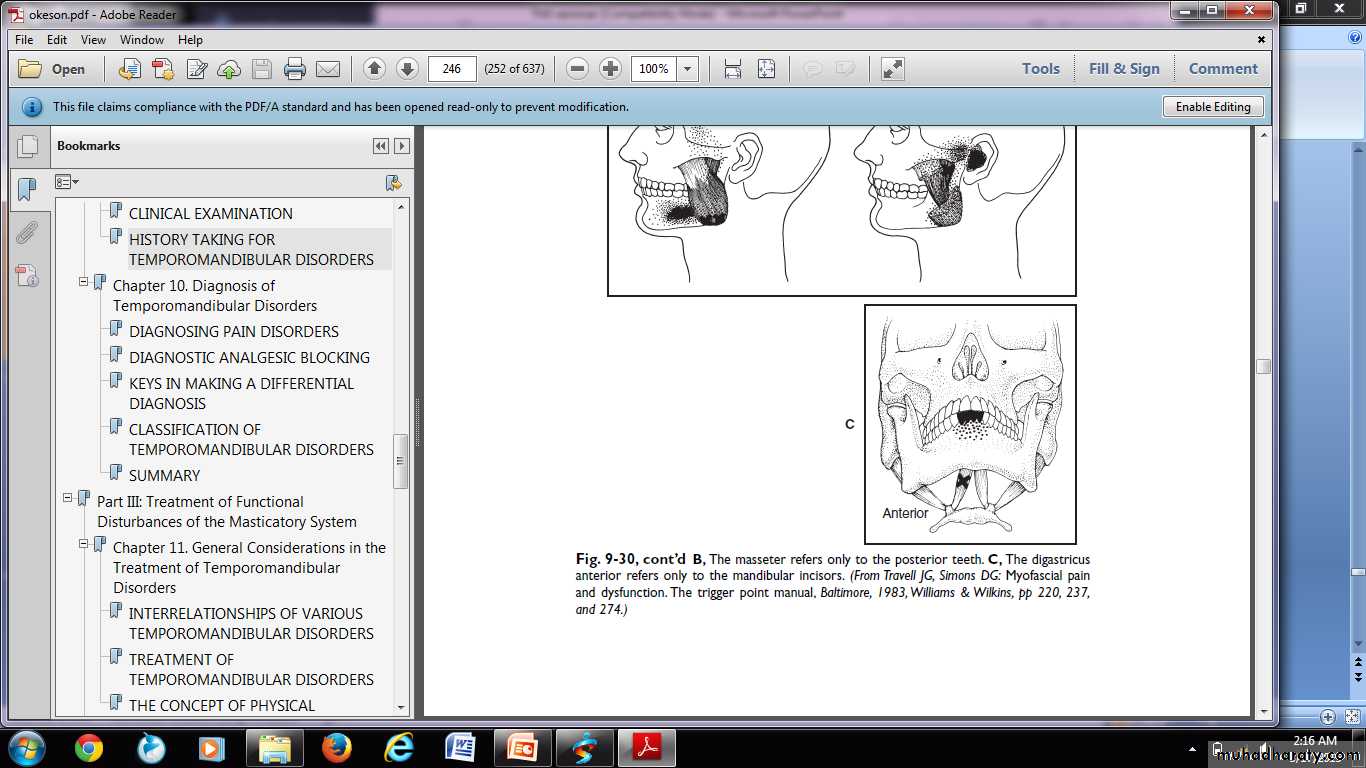
Zone of reference
Referral of myofascial trigger point pain of temporalis muscles refers only to the maxillary teeth.
The masseter refers only to the posterior teeth.
The digastric anterior refers only to the mandibular incisors.Trigger points
Trigger points exist as a localized tender areas within taut bands of skeletal muscles & stimulated by macro & microtraumatic episodes, they refer a characteristic pain pattern to a distant group of muscles, i.e. zone of reference.Palpation of trigger points gives a positive ‘jump sign’.
Associated symptoms
History of the patientMode of onset, duration, frequency & quality of pain. Site & reference point of pain.
Time of the day, at which pain is most pronounced.
Occupation.
Sleeping habits.
Parafunctional habits.
H/O previous trauma, prolonged dental work etc.
Family or emotional problems.
Associated symptoms.
Aggravating & relieving factors.
Physical examination
Articular / joint examinationDental examination
Muscular examination
Cervical examination
Neelima Malik, Textbook Of Oral & Maxillofacial Surgery, 2nd Edi
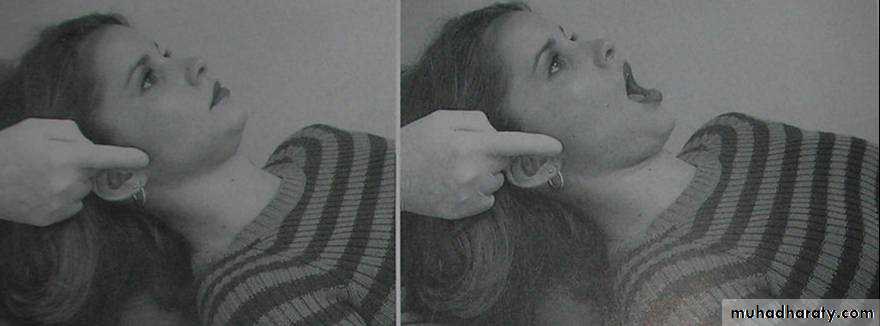
Clinical examination of TMJ
TMJ pain-
Determined by digital palpation of the joints – when mandible is in both stationary as well as dynamic movement
Finger tips placed – lateral aspect of both the joints – feel for the lateral poles passing downwards & forwards across articular eminence on repeated opening & closing.
A medial force is then applied to – record symptoms if any in static position & then on opening & closing.
Also, on maximal opening – fingers are rotated slightly posteriorly to apply force on the posterior aspect of the condyle (to evaluate posterior capsulitis & retrodiscitis)
Temporalis muscle
Palpation of the posterior, middle, and anterior regions and tendon of the Temporalis.I / o- The finger is moved up the anterior border of the ramus until the coronoid process and the attachment of the tendon of the temporalis are felt.
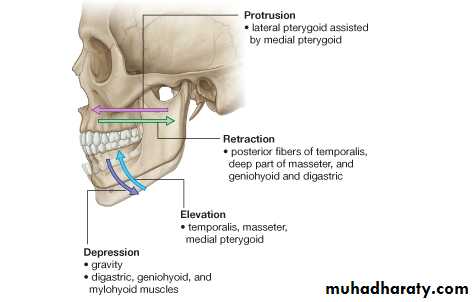
Functional manipulation of inferior lateral pterygoid.
The patient is asked to protrude against resistance provided by the examiner.Functional manipulation of the superior lateral Pterygoid is achieved by asking the patient to bite on at tongue blade bilaterally.
Medial pterygoid
Tell patient to open mouth wide, protrude against resistance, clench the teeth together, and then bite on a separator when these function causes pain then medial pterygoid muscle is involved.Sternocleidomastoid
Palpation of the sternocleidomastoid muscle high near the mastoid process & low near the clavicle.TMJ Range of Motion:-
• 1. Amount of oral opening and the excursions.• 2. Extent of movement
• i) ROM – Range of motion
• i) AROM – Active range of motion
• iii) PROM – Passive range of motion
• Grading of click or crepitation- noises evaluation.
• Auscultation (stethoscopic evaluation), if needed.
1. Amount of oral opening and excursions.
Opening path & amount of deviation should be noted.Early opening deviation is due to spasm lateral pterygoid muscle of same side.
Normal range of protrusive movement- 10mm
Lateral excursions- normal- 10mmPain or inflammation indicates one of the following conditions
Joint inflammation,
muscle dysfunction.
Anteriorly displaced disc etc
Neelima Malik, Textbook Of Oral & Maxillofacial Surgery, 2nd Edi
• Normal vertical ROM in adults is-40- 50 mm
Hypomobility without pain gives indication for pathology.
Measurement of maximum pain free motion is noted.
Limited AROM with pain indicates structural restrictions by muscular problems.
Neelima Malik, Textbook Of Oral & Maxillofacial Surgery, 2nd EdiC and S Curves
A ‘C-pattern’ of motion occurs if the hypo mobility is due to internal derangement• The mandible deviates toward the involved side in the midrange of opening before returning to normal.
An ‘S-pattern’ of movement while opening the mouth may indicate a muscle imbalance.
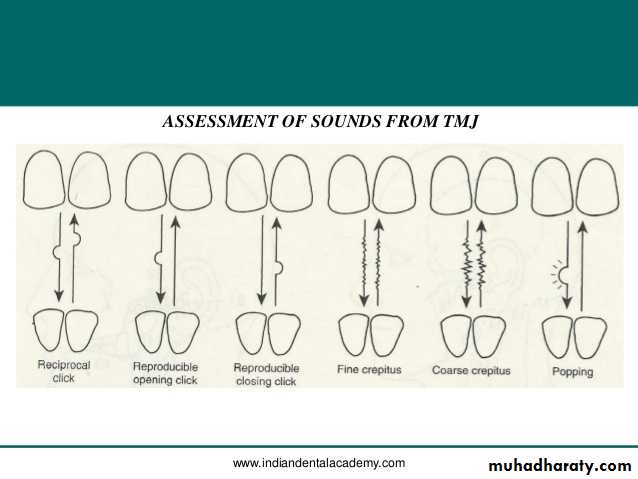
3. Timing of the click
Noted whether it is coming during opening, closing or both should be ascertained.Distinct sound click
Crepitus
Multiple scraping, grating noises
These sound can be heard by stethoscope.
Neelima Malik, Textbook Of Oral & Maxillofacial Surgery, 2nd EdiLaskin and Block, (1986)
• Phase I therapy psychophysiologic discussion.• Home therapy (diet & exercise)
• Muscle relaxant & NSAIDs (2-4 wks)- 50% resolution
Phase Il therapy
Home therapy and medications + bite appliance
(2 to 4 wks) 20% to 25%resolution.
Phase lll
Physiotherapy (ultrasound,
electrogalvanic stimulation) or relaxation therapy (yoga, biofeedback)
(4 to 6 weeks) 10% to 15% resolution.
Phase lV
Psychologic counselling pain clinic
Medications
• NSAIDs to reduce inflammation & pain in muscles & joint.• Aspirin : 2 tabs 0.3 to 0.6gm/ 4 hourly.(ECOSPIRIN)
• Piroxicam: cap. 10 to 20mg /once daily.(FELDENE)
• Ibuprofen : 200 to 600mg/3 times a day.(BRUFEN)
• Pentazocine: 30 mg i.v./i.m./s.c. every 3– 4 hrs max.- 360mg. (TALWIN, TALACEN)
• Muscle relaxant-
• Methocarbamol : muscle relaxant- 1500mg/ 4 times a day for 2-3 days,1000mg i.v./ 8 hrly (ROBAXIN)
• Metaxalone- (SKELAXIN)
• Chlorzoxazone - (FLEXON MR)- 400 mg, 325mg, 250 mg
• Antidepressant-
• Diazepam- (VALIUM, CALMPOSE) & chlordiazepoxide (sedative)
• 5 to 10mg /2 to 3 times a day.(LIBRIUM)
• Amitriptyline: - 25mg/ 3- 4 times a day or at bedtime.(ELAVIL, VANATRIP).
Trigger Point Injection
A trigger point is located, trapped between the fingers, and injected (with a short 27-gauge needle).
0.5% bupivacaine with epinephrine.
Blocks are given at 48-hour to weekly intervals into nerve distributions and particularly into zones of muscular trigger foci.Okeson, Jeffrey P. (2003). Textbook of Management of temporomandibular disorders and occlusion (5th ed.)
Physiotherapeutic modalities
• Heat application.Ultrasound
Heat lamp
Diathermy.
• Cryotherapy.
• Ice pack
• Vapo- coolant spray
• Ice massage
• Cold whirlpool
• Transcutaneous Electronic Nerve Stimulator (TENS).
• Active stretch exercises.
Mujakperuo HR, Watson M, (2010). "Pharmacological interventions for pain in patients with temporomandibular disorders". The Cochrane Database of Systematic Reviews
Phonophoresis
The use of ultrasound to enhance the delivery of topically applied medicationsHydrocortisone- 10%
Ketoprofen- 10%
Dexamethazone
1 MHz frequency with transducer having an affective radiating Intensity of 1.5 W/ cm² in continuous mode to insure reaching the deep tissues .
Parafunctional Behaviors
Gum/candy chewing (chewing limited to 15 – 20 minutes/day!) – including chewing on one sideClenching/bruxing/grinding
Leaning on chin/jaw
Biting nails, pencils, cheeks
Sleep position
Caffeine use
Musical instruments
Mouth breathing
Phone cradling
TMJ Dysfunction Syndrome (TMD)
Myofacial Pain Dysfunction Syndrome (MPDS)
• Prevention:
• Eliminate oral habits such as teeth grinding and yawing widely.
• Dental treatment (orthodontic treatment, prosthetic restoration, orthognathic surgery and TMJ surgery).
• Seek effective treatment for diseases such as osteoarthritis and fibromyalgia.
• Early Diagnosis and therapy.
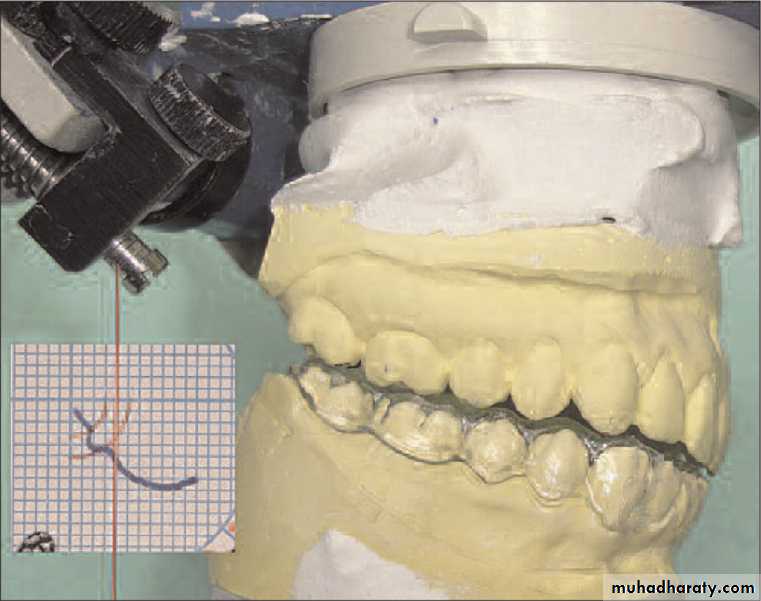
Usefulness of occlusal splints
Dentists often use occlusal splints in the management of occlusodontic problems.Proper design and placement of occlusal splints requires that they respond to precise indications and that practitioners fabricate and maintain them with care to assure that patients benefit from them.
Splints help practitioners adjust the relationship between the jaws either by suppressing blockage of teeth to relax muscles or by repositioning the condyles in the articular fossas to recapture discs or to reduce painful excess intra-articular pressure derived from degenerative diseases.
1 – THE MUSCLE RECONDITIONING SPLINT
2 – THE ANTERIOR STOP
3 – THE ARTICULAR REPOSITIONING SPLINT
4 – THE DECOMPRESSION SPLINT
5 – THE STABILIZING SPLINT
6 – THE NOCTURNAL PROTECTION SPLINT
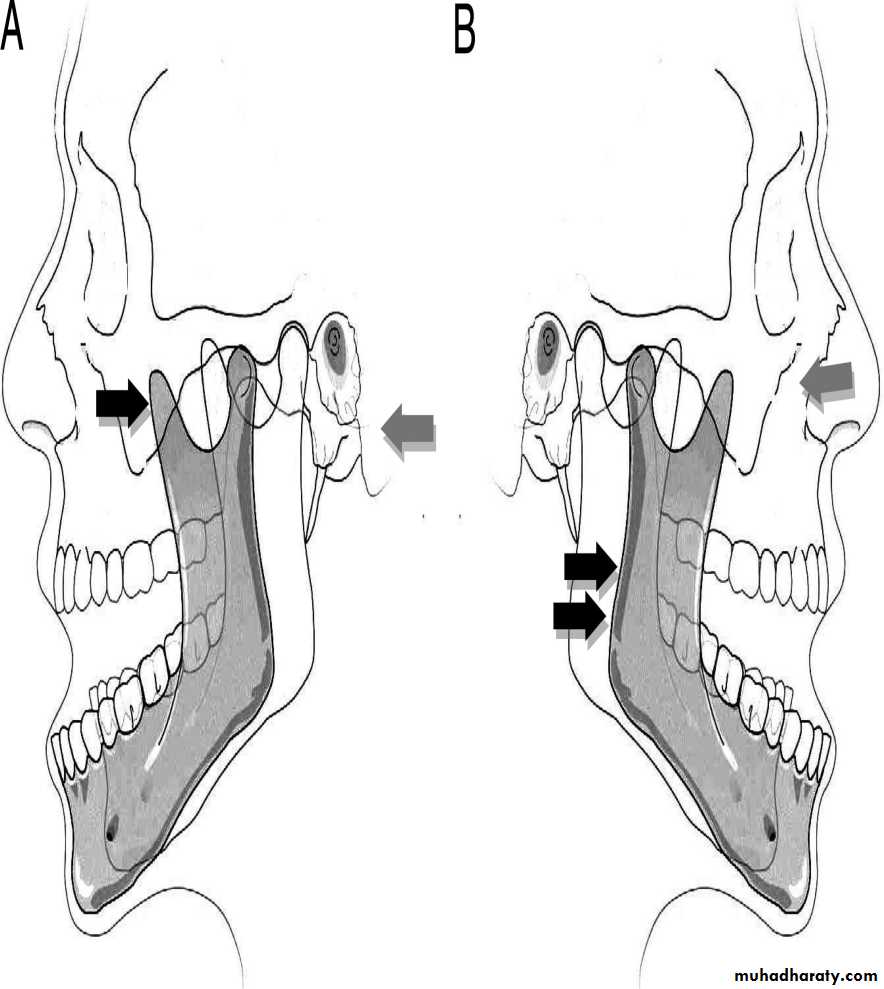
Tmj dislocation
Temporomandibular joint (TMJ) subluxation and dislocation are uncommon but very unpleasant and distressing conditions to patients.Subluxation of the TMJ is an excessively abnormal condylar excursion secondary to flaccidity and laxity of the capsule.
When the condyle head excurses anterior to the eminence upon wide opening, it can return to the fossa by self-manipulation or non-surgical conservative reduction.
Surgery is recommended if a complete dislocation, so-called open lock, occurs as a chronic or recurrent protracted condition that cannot be reduced voluntarily. A range of surgical procedures can be performed to limit condylar hypermobility including soft tissue tethering, removal of mechanical blockade and augmentation of articular eminence using different kinds of grafts.
The clinican aims to direct a downwards and backwards force to the mandible. This is achieved by placing the clinican’s thumbs on the outer aspect of the occlusal surface of the mandibular molars bilaterally, and then pushing gently, with increasing pressure downwards. At the same time, with the fingers, gentle upwards pressure is placed on the chin . The patient’s mandible should be at the level of, or below the clinican’s elbow to allow for adequate but gentle pressure. The effort required is such as to overcome the muscular spasm and guide the condyle down along the front of the articular eminence and back into the glenoid fossa
arthritis
Infectious arthritisinfection of the temporomandibular joint (TMJ) may result from direct extension of adjacent infection or hematogenous spread of bloodborne organisms
The area is inflamed, and jaw movement is limited and painful. Local signs of infection associated with evidence of a systemic disease or with an adjacent infection suggest the diagnosis.
Treatment includes antibiotics, proper hydration, pain control, and motion restriction.
Parenteral penicillin G is the drug of choice until a specific bacteriologic diagnosis can be made on the basis of culture and sensitivity testing.
Suppurative infections are aspirated or incised. Once the infection is controlled, jaw-opening exercises help prevent scarring and limitation of motion.
Traumatic arthritis
Rarely, acute injury (eg, due to difficult tooth extraction or endotracheal intubation) may lead to arthritis of the TMJ.
Pain, tenderness, and limitation of motion occur.
Diagnosis is based primarily on history.
X-ray results are negative except when intra-articular edema or hemorrhage widens the joint space.
Treatment includes NSAIDs, application of heat, a soft diet, and restriction of jaw movement.
Osteoarthritis
The TMJ may be affected, usually in people > 50 yr. Occasionally, patients complain of stiffness, grating, or mild pain.Crepitus results from a hole worn through the disk, causing bone to grate on bone. Joint involvement is generally bilateral.
X-rays or CT may show flattening of the condyle, suggestive of dysfunctional change.
Treatment is symptomatic. A mouth guard worn during the night or day may help alleviate pain and reduce grating sounds in patients with missing teeth (which can cause their jaws to come closer together when biting).
Rheumatoid arthritis
The TMJ is affected in > 17% of adults and children with RA, but it is usually among the last joints involved.Pain, swelling, and limited movement are the most common findings. In children, destruction of the condyle results in mandibular growth disturbance and facial deformity. Ankylosis may follow.
X-rays of the TMJ are usually negative in early stages but later show bone destruction, which may result in an anterior open-bite deformity.
Treatment is similar to that of RA in other joints In the acute stage, NSAIDs may be given, and jaw function should be restricted. A mouth guard or splint worn at night is often helpful. When symptoms subside, mild jaw exercises help prevent excessive loss of motion. Surgery is necessary if ankylosis develops .
Internal Tempromandibular Joint Derangement
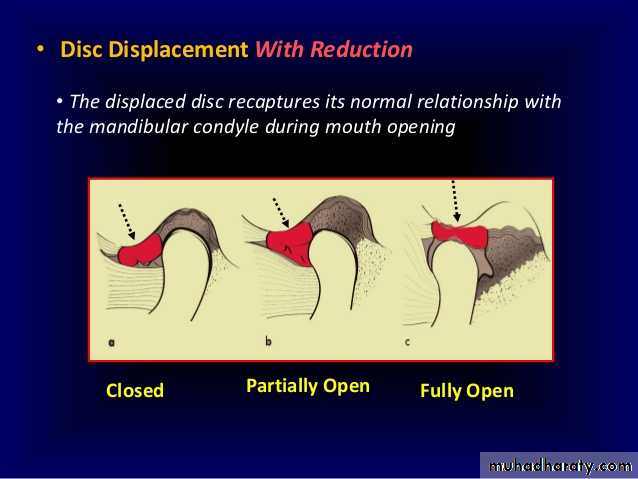
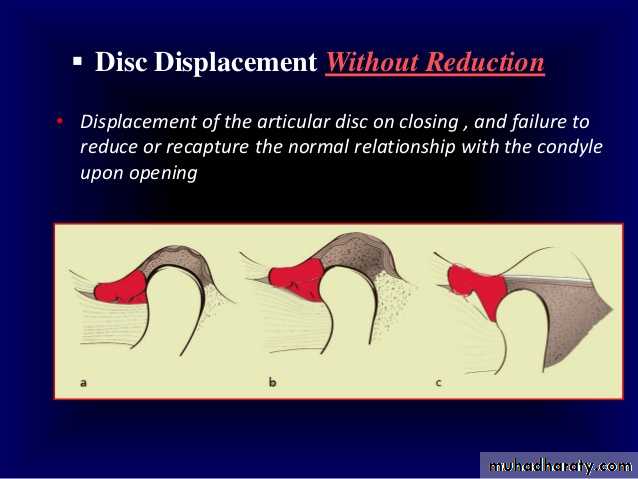
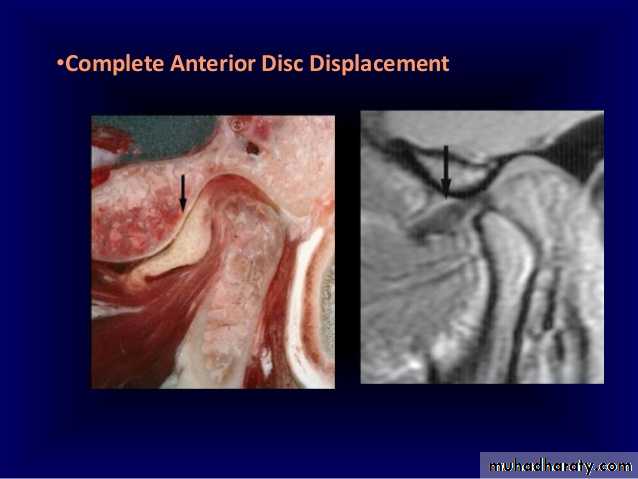
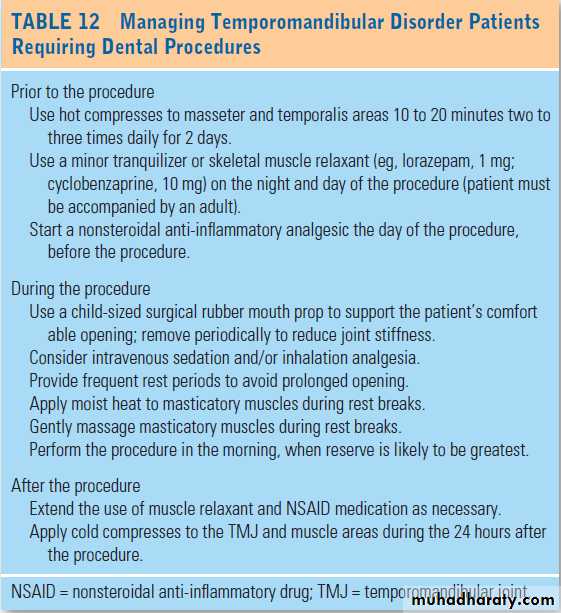
Key PointsThe articular disk is pulled out of place anteriorly due to abnormal jaw mechanics; it may remain displaced (without reduction) or return (with reduction).
Disk displacement with reduction typically causes clicking and pain with chewing.
Disk displacement without reduction does not cause clicking but reduces maximum jaw opening to ≤ 30 mm.
Surrounding tissues may become painfully inflamed (capsulitis).
Analgesics, repositioning splints, and passive jaw-motion exercisers often help, but surgery is occasionally required.