Spleen in surgery
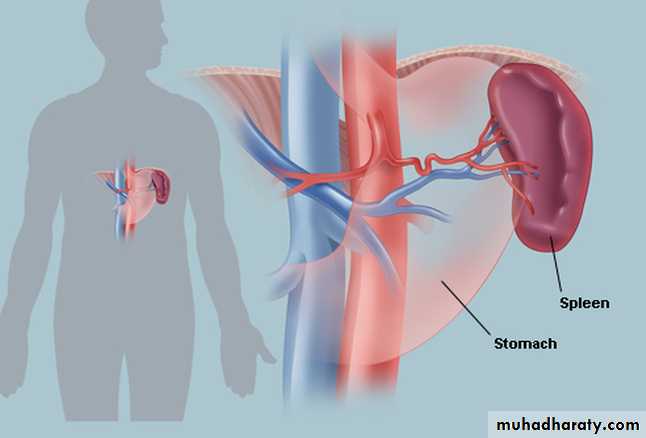
anatomyThe spleen is situated in the left upper quadrant tucked under and against the left dome of the diaphragm and overlain by the lower left 9th to 11th ribs.
It has to enlarge two to three times before becoming palpable.
Accessory spleens (splenunculi) are present in 10% of adults and are most commonly situated near the hilum but may occur in other sites They are important in relation to splenectomy for haematological disorders, because if left behind they may hypertrophy and cause recurrence of the disease.
embryology
Develops from mesenchymal cells in the dorsal mesogastrium during the fifth week of gestation.The peritoneum covering the spleen, except in the hilum.
Functions of the spleen
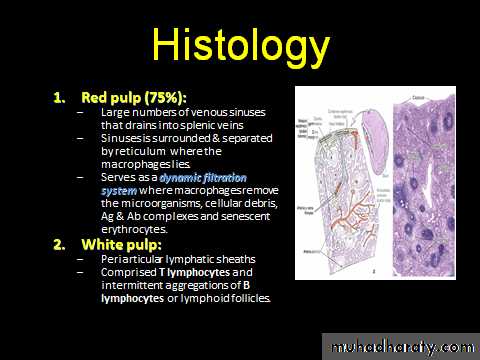
■ Immune■ Filter function
■ Pitting
■ Reservoir
■ Cytopoiesis
■ Splenectomy harms the patient
INVESTIGATION OF THE SPLEEN
Conditions that result in splenomegaly can be diagnosed on the basis of the history and examination findings andfrom laboratory examination.
In haemolytic anaemia, a full blood count, reticulocyte count and tests for haemolysis will determine the cause
of the anaemia.
Splenomegaly associated with portal hypertension caused by cirrhosis is diagnosed on the history, physical signs of liver dysfunction, abnormal tests of liver function and endoscopic evidence of oesophageal varices
Radiology of spleen
1: ultrasound
2: abdominal x-ray
3: CT scan of abdomin
4: MRI
5: nuclear scanning
6: angiography
Splenic artery angiography
Hypersplenism
This is a syndrome of splenomegaly combined with destruction of formed blood elements leading to one or more of the following:• anaemia;
• leukopenia < 4-5 x 109/L;
• thrombocytopenia < l00 X 109/L.
Hyposplenism
Hyposplenism is confirmed by the appearance of defective red cells in the peripheral circulation.
The most frequent cause is surgical splenectomy.
Causes of hyposplenism
SplenectomySplenic agenesis
Atrophy
Coeliac disease
Inflammatory
bowel disease and collagenous colitis
Systemic amyloidosis
Old age
Dermatitis herpetiformis
Sickle cell anaemia
Systemic lupus erythematosus
CONGENITAL ABNORMALITIES OF THE SPLEEN
1: agenesis of polysplenia2: splenuculai
3: hamartomas
4: non-parasitic cyst
5: wandering spleen
Splenunculi
Splenunculi are single or multiple accessory spleens that are found in approximately 10–30% of the population.
They are located near the hilum of the spleen in 50% of cases and are related to the splenic vessels or behind the tail of the pancreas in 30%.
The remainder are located in the mesocolon or the splenic ligaments.
Their significance lies in the fact that failure to identify and remove these at the time of splenectomy may give rise to persistent disease.
Splenunculi
Ectopic (wandering) spleen
Ectopic (wandering) spleen is rare and occurs more commonly in women (7 : 1). It is due to lax attachments of the spleen to the retroperitoneum and long splenic vessels, such that the spleen 'wanders' the quadrants of the abdomen.,It may present acutely with abdominal pain due to torsion that may progress to infarction with hypersplenism (due to congestion), or simply with an abdominal mass with or without associated pain.
The diagnosis is confirmed by CT or duplex ultrasonography.
Treatment of ectopic spleen is by splenopexy (viable spleen) or splenectomy when the spleen is infarcted.
Ectopic spleen
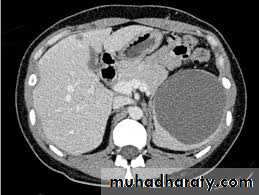
Ectopic spleen by CT
Splenic cysts
Splenic cysts are primary or secondary. Secondary cysts are more common and develop after splenic injuries, hence the name 'traumatic splenic pseudocysts' (no lining epithelium). Splenic traumatic pseudocysts may be totally asymptomatic but have a tendency to enlarge.The time interval between initial injury and presentation or diagnosis is extremely variable.
Some traumatic pseudocysts remain asymptomatic and are discovered accidentally during investigation by ultrasound.
Others develop abdominal pain and a palpable mass. Acute presentation with rupture is well treatment is only necessary for large symptomatic cysts after confirmation of the diagnosis by ultrasound or CT.
Spleen-preserving excision is possible unless the cyst is very large or presents acutely with rupture and bleeding documented.
.
• Surgicaltreatment is only necessary for large symptomatic cysts after confirmation of the diagnosis by ultrasound or CT.
• Spleen-preserving excision is possible unless the cyst is very large or presents acutely with rupture and bleeding
Splenic cyst
Splenic cyst
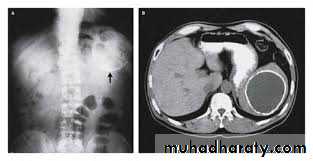
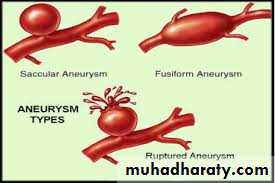
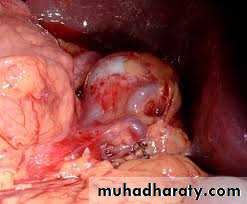
Splenic artery aneurysm
Aneurysms involving the splenic artery are estimated to occur at 0.04–1% of post-mortem examinations.They are twice as common in the female and are usually situated in the main arterial trunk. Although these are generally single, more than one aneurysm is found in a quarter of cases.
These may be a consequence of intra-abdominal sepsis and pancreatic necrosis in particular. They are more likely to be associated with arteriosclerosis in elderly patients.
The aneurysm is symptomless unless it ruptures and is more likely to be detected on a plain abdominal radiograph or ultrasound scan. It is unlikely to be palpable, although a bruit may be present.
Almost half the cases of rupture occur in patients younger than 45 years of age, and a quarter are in pregnant women, usually in the third trimester of pregnancy or at labour.
The treatment of choice previously consisted of splenectomy and removal of the diseased artery. Some surgeons advocate ligation of the proximal and distal ends of the sac to allow thrombosis of the aneurysm and partial or completelay.
Embolisation or endovascular stenting following selective splenic artery angiography can be considered
Splenic artery aneurism
Splenic artery aneurism
Splenic abscess
Epid : rare 0.05-0.7% , high mortalityEtiology :
- Hematogenic Spread >>
- Infected Trauma
- Infected spleenic infarction
- Alcoholism,DM,Immunosupressan, drug abuser >>
Pathophysiology
- Hematogenous embolization
- Spread from altered splenic architecture
- Contiguous spread
Clinical features
FeverAbdominal Pain(maximum in the left hypochondria )
Shoulder pain (Involvement of the diaphragmatic pleura )
Pleuritic chest pain
General malaise
Dyspeptic symptoms
imagings
Plain photo
US
CT
MRI
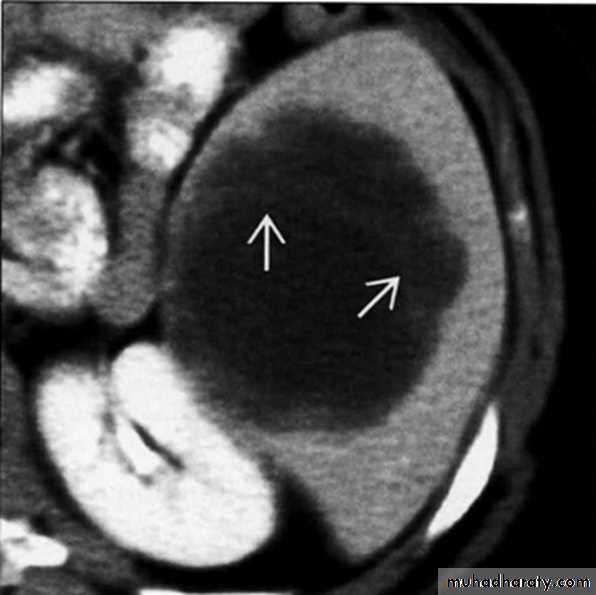
Pyogenic splenic abscess on axial CECT.Note thin septations within abscess (arrows)
Treatment and complications
Splenectomy for most cases؟؟Percutaneous drainage
Complications
Spontaneous rupturePeritonitis
sepsis
Tumor
BenignHemangiomas
Lymphangioma
Hamartoma
Primary cyst \ echinoccocus cyst
Malignants
Lymphomas or myeloprolifrative diseases
Rare site for solid tumors but more common in lung and breast tumors
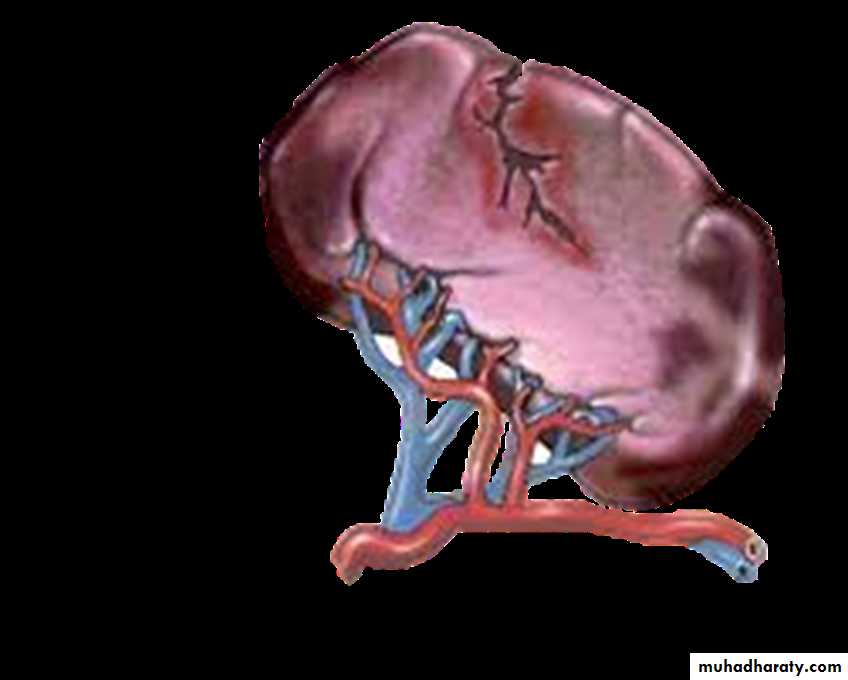
Splenic Trauma/Injury
The spleen is the intra-abdominal organ most frequently injured in blunt trauma.
Splenic injury
Mechanism of injury
1: Blunt abdominal traumafrom compression or deceleration
(motor vehicle accidents, falls ,direct blow to abdomen,with haematological abnormalities)
2:Penetrating trauma rare
Presentations
Clinical symptoms vary1:Patient may present with left upper abdominal or flank pain
2:Reffered pain to left shoulder (kehr sign)
3:Some may be asymptomatic
signs
Physical examination is insensitive and non specific.
Patient may have signs of left upper quadrant tenderness or signs of generalized peritoneal irritation.
May present with tachycardia ,Tachypnea, anxiety , Hypotension (shock)
diagosis
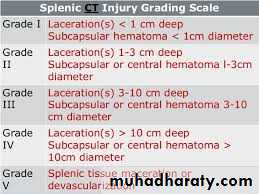
The diagnosis is confirmed by ultrsound - CT (hemodynamic stability) or exploratory laparotomy (hemodynamic instability)Nonopertative Treatment
1:Hemodynamic stability.2:Normal abdominal examination.
3:Absence of contrast extravasation on CT.
4:Absence of other clear indications for exploratory laparotomy or associated injuries requiring surgical intervention.
5:Absence of associated health conditions that carry an increased risk for bleeding (coagulopathy, hepatic failure, use of anticoagulants, specific coagulation factor deficiency)
6:Injury grade I to III.
Surgical treatment of a splenic injury depends on its severit the presence of shock, and
associated injuries.1: splenectomy
2: partial splenctomy
3: preserving the spleen
SPLENOMEGALY
1: infections2: blood diseases
3: metabolic
4: circulatory
5: collagen diseases
6: splenic cysts
7: neoplasia
Indications of SPLENECTOMY
• trauma resulting from an accident or during a surgical procedure, as for example during mobilisation of the oesophagus, stomach, distal pancreas or splenic flexure of the colon;• removal en bloc with the stomach as part of a radical gastrectomy or with the pancreas as part of a distal or total pancreatectomy;
• to reduce anaemia or thrombocytopenia in spherocytosis, idiopathic thrombocytopenic purpura or hypersplenism;
• in association with shunt or variceal surgery for portal hypertension
Preoperative preparation
Surgical approachOpen splenectomy
Laparoscopic splenectomy
Postoperative complications
1: early complications
A: bleeding: slipped ligatures or from oozing of raw areas and sites of splenic adhesions.
B: atelectasis, pneumonia and pleural effusion
C: thrombosis and hypercoagulable state
D: acute gastric dilation and hematemesis
E: injury to surrounding organs like stomach,colon and pancreas.
F: portal vein thrombosis.
Postoperative complications
2: late comlications:A: risk of thrombosis and pulmonary embolism
B: late recurrence of disease may complicate splenectomy like anaemia and thrombocytopenia, due to enlarged messed splenuculi .
C:Post-splenectomy septicaemia may result from Streptococcus pneumoniae, Neisseria meningitides, Haemophilus influenzae and Escherichia coli.
D: the most important complication is overwhelming(opprotunist) postsplenectomy infection(OPSI).
Opportunist post-splenectomy infection (OPSI)
Published guidelines emphasise that most infections after splenectomy could be avoided through measures that include offering patients appropriate and timely immunization, antibiotic prophylaxis, education and prompt treatment of infection.vaccinations
It is thought that children who have undergone splenectomy before the age of 5 years should be treated with a daily dose of penicillin until the age of 10 years.Prophylaxis in older children should be continued at least until the age of 16 years, but its use is less well defined in adults.
Furthermore, compliance is problematic in the long term but, as the risk of overwhelming sepsis is greatest within the first 2–3 years after splenectomy, it seems reasonable to give prophylaxis during this time.
vaccinnization
If elective splenectomy is planned, consideration should be given to vaccinating against pneumococcus, meningococcus (both repeated every 5 years) and H. influenzae (repeated every 10 years).
Such vaccinations should be administered at least 2 weeks before elective surgery and as soon as possible after recovery from surgery but before discharge from hospital in all other cases.