Pleural lesions
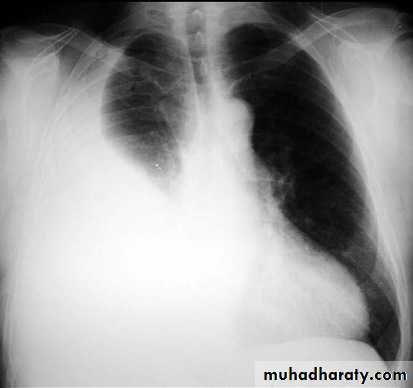
Pleural effusionPleural effusion tends to be used as a catch-all term denoting a collection of fluid within the pleural space. This can be further divided into exudates and transudates depending on the biochemical analysis of aspirated pleural fluid. Essentially it represents any pathological process which overwhelms the pleura's ability to reabsorb fluid.
Radiographic appearances
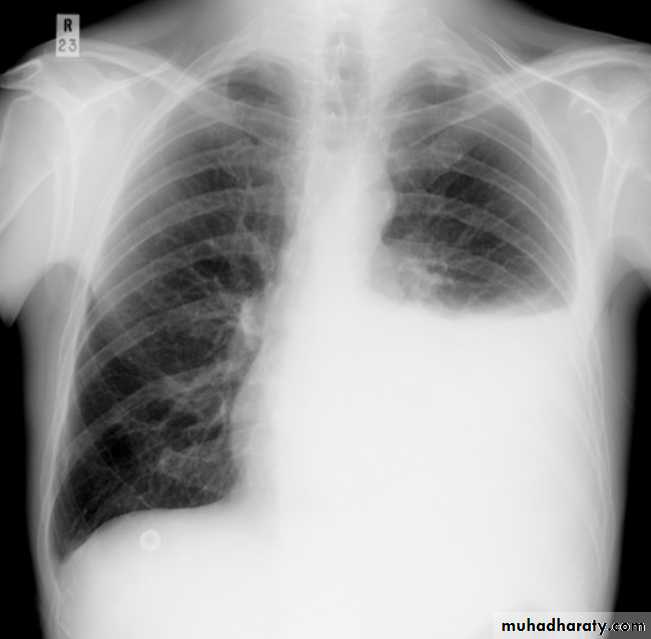
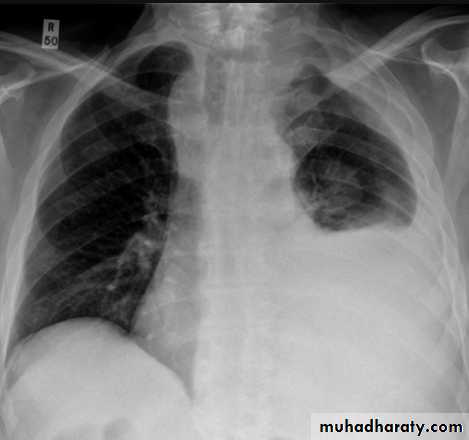
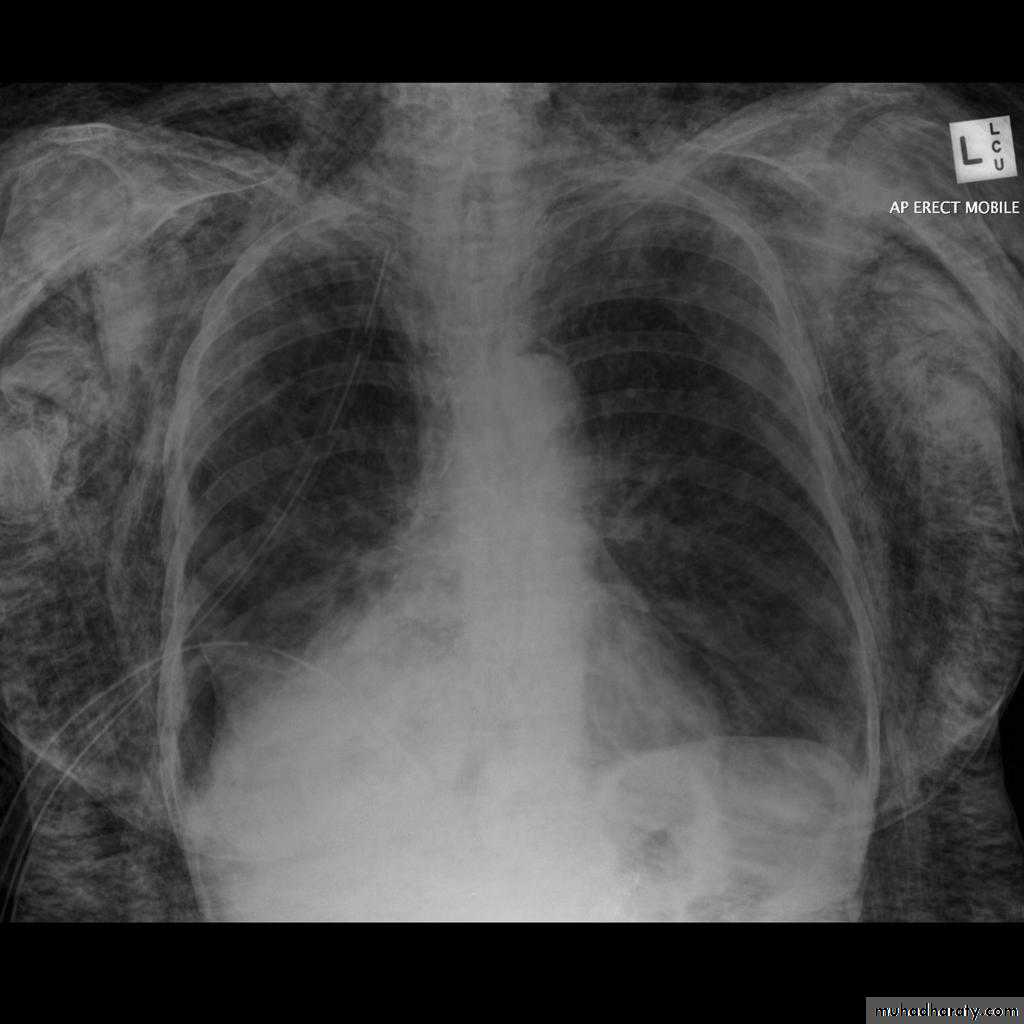
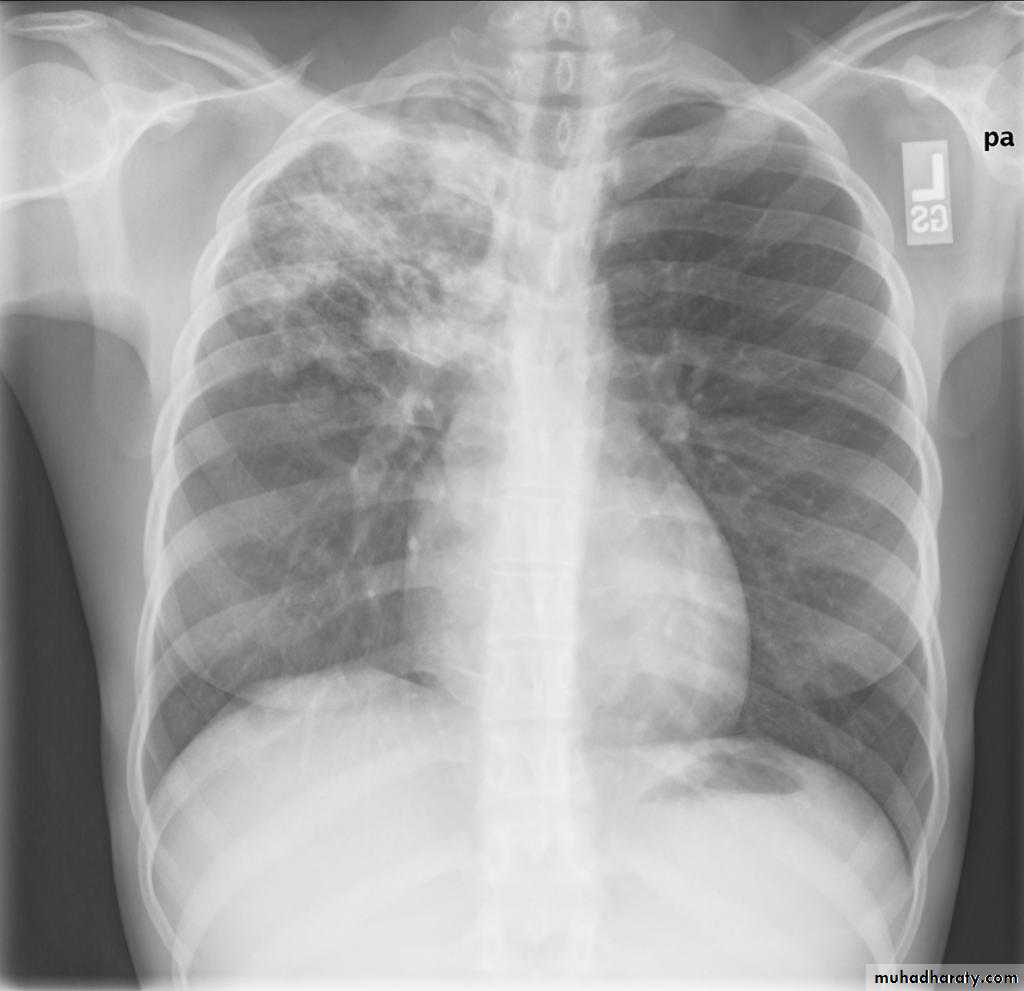
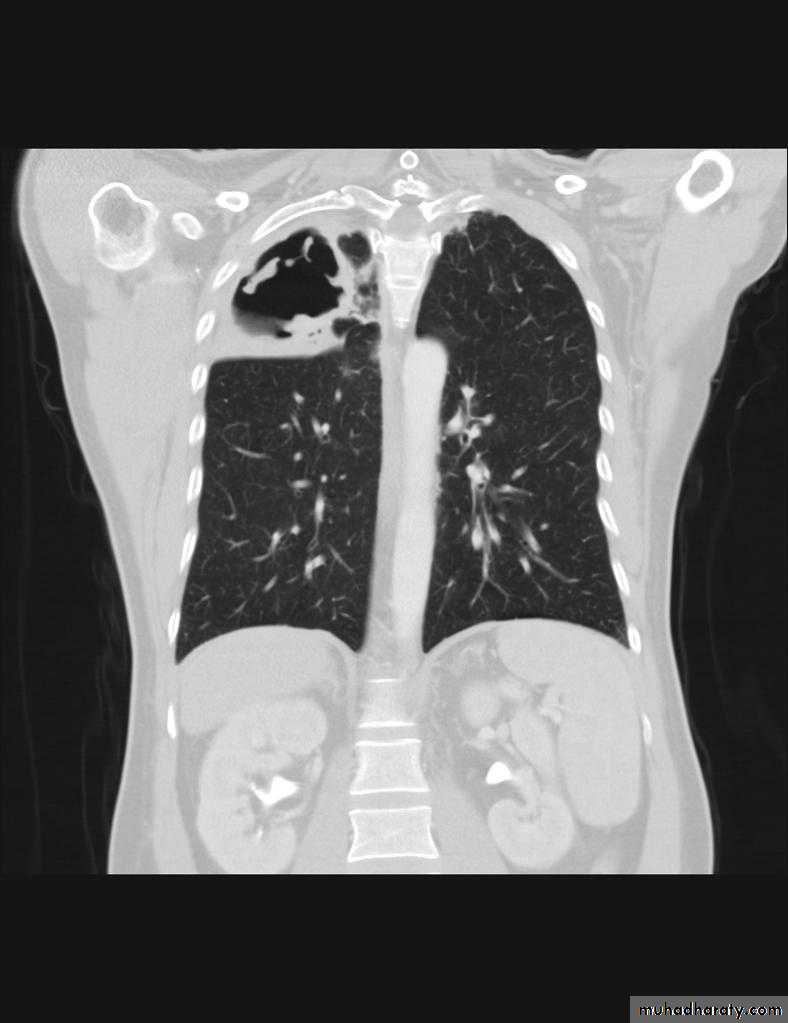
Plain radiographChest radiographs are the most commonly used examination to assess for presence of a pleural effusion, however it should be noted that on a routine erect chest x-ray as much as 250-600 ml of fluid is required before it becomes evident 6. A lateral decubitus film is most sensitive, able to identify even a small amount of fluid. At the other extreme, supine films can mask large quantities of fluid.
CXR (lateral decubitus)
A lateral decubitus film (obtained with the patient lying on their side, effusion side down, with a cross table shoot through technique) can visualise small amounts of fluid layering against the dependent parietal pleura.
CXR (erect)
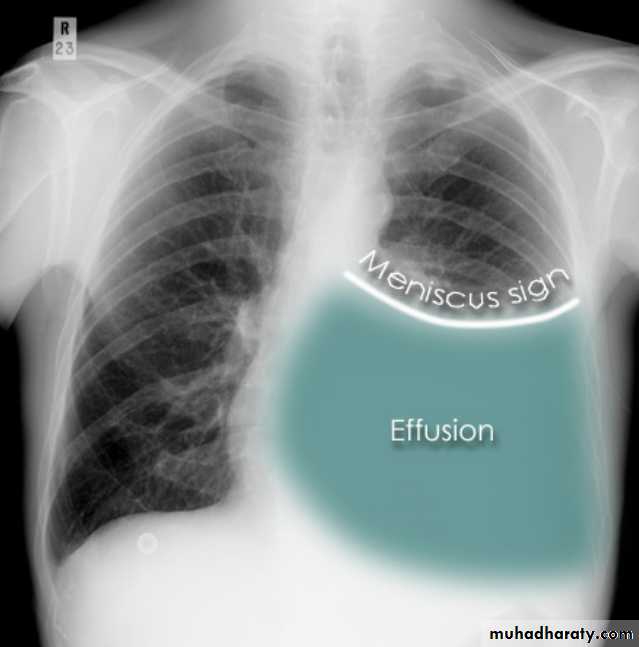
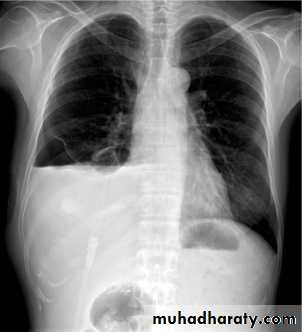
Both PA and AP erect films are insensitive to small amounts of fluid. Features include:
blunting of the costophrenic angle
blunting of the cardiophrenic angle
fluid within the horizontal or oblique fissures
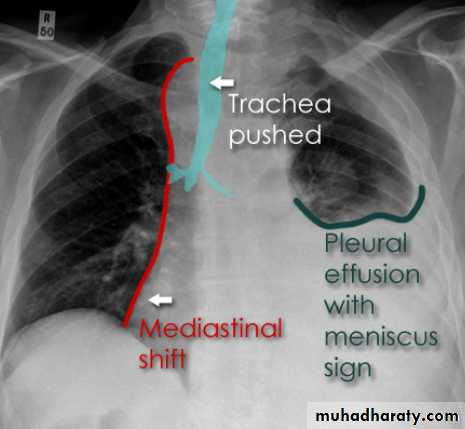
eventually a meniscus will be seen, on frontal films seen laterally and gently sloping medially (note:
A subpulmonic effusion (infrapulmonary effusion) may be seen when there is previously established pulmonary disease, but can also be encountered in normal lungs , They are more common on the right, and usually unilateral
with large volume effusions, mediastinal shift occurs away from the effusion (note: if coexistent collapse dominates then mediastinal shift may occur towards the effusion)
An empyema can resemble a pleural effusion
and can mimic a peripheral pulmonary abscess, although a number of features usually enable distinction between the two Features that help distinguish a pleural effusion from an empyema include:Shape and location
Empyemas usually:
form an obtuse angle with the chest wall
unilateral or markedly asymmetric whereas pleural effusions are (if of any significant size) usually bilateral and similar in size .
lenticular in shape (bi-convex), whereas pleural effusions are crescentic in shape (i.e concave towards the lung)
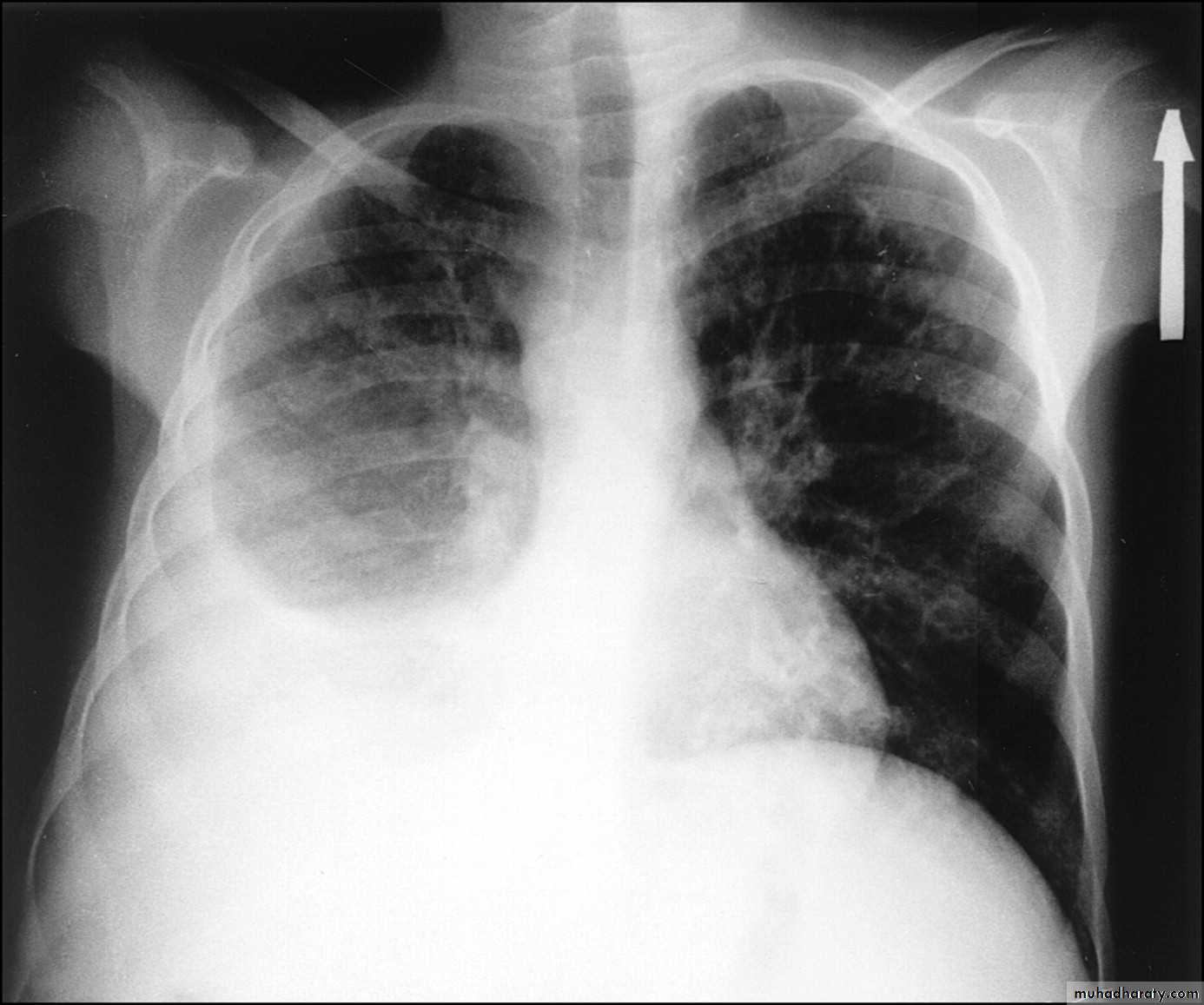
Pneumothorax
Pneumothorax refers to the presence of gas (air) in the pleural space. When this collection of gas is constantly enlarging with resulting compression of mediastinal structures it can be life-threatening and is known as a tension pneumothoraxIt is useful to divide pneumo thoraces into three categories :
primary spontaneous: no underlying lung disease marfan syndrum , Elher danus syndrome alpha-1 antitrypsin deficiency
secondary spontaneous: underlying lung disease is present
iatrogenic/traumatic
Radiographic features
Chest radiograph
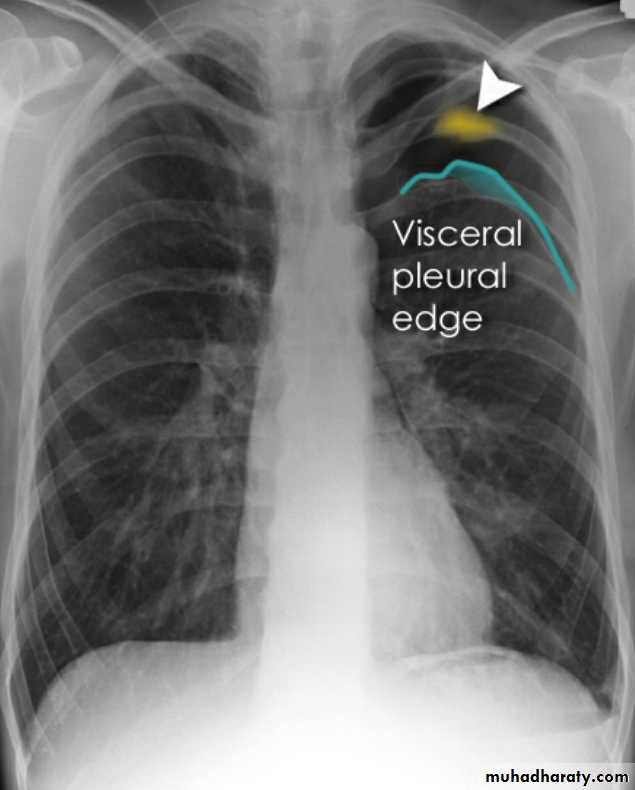
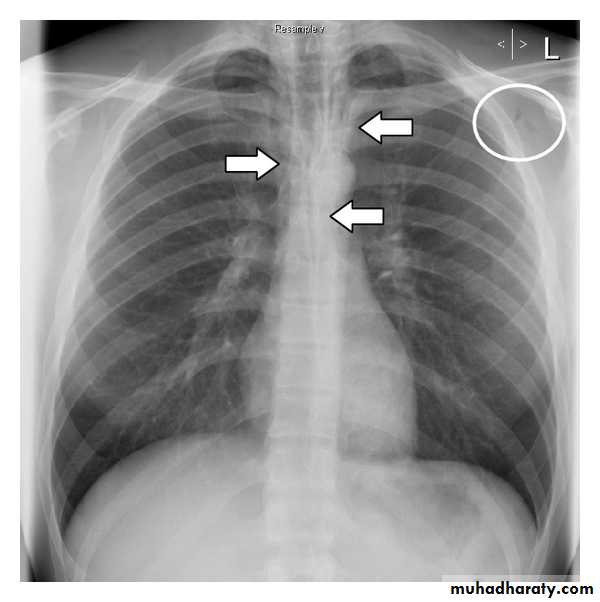
A pneumothorax is, when looked for, usually relatively easily appreciated. Typically they demonstrate:
visible visceral pleural edge see as a very thin, sharp white line
no lung markings are seen peripheral to this line
the peripheral space is radiolucent compared to adjacent lung
the lung may completely collapse
the mediastinum should not shift away from the pneumothorax unless a tension pneumothorax is present
A tension pneumothorax
A tension pneumothorax occurs when intrapleural air accumulates progressively in such a way as to exert positive pressure on mediastinal and intrathoracic structures. It is a life threatening occurrence requiring rapid recognition and treatment is required if cardiorespiratory arrest is to be avoided.Radiographic features
A pneumothorax will have the same features as a run-of-the-mill pneumothorax with a number of additional features, helpful in identifying tension. These additional signs indicate over expansion of the hemithorax:
ipsilateral increased intercostal spaces
shift of the mediastinum to the contralateral side
depression of the hemidiaphragm
tension pneumothorax
Hydro pnuemothorax
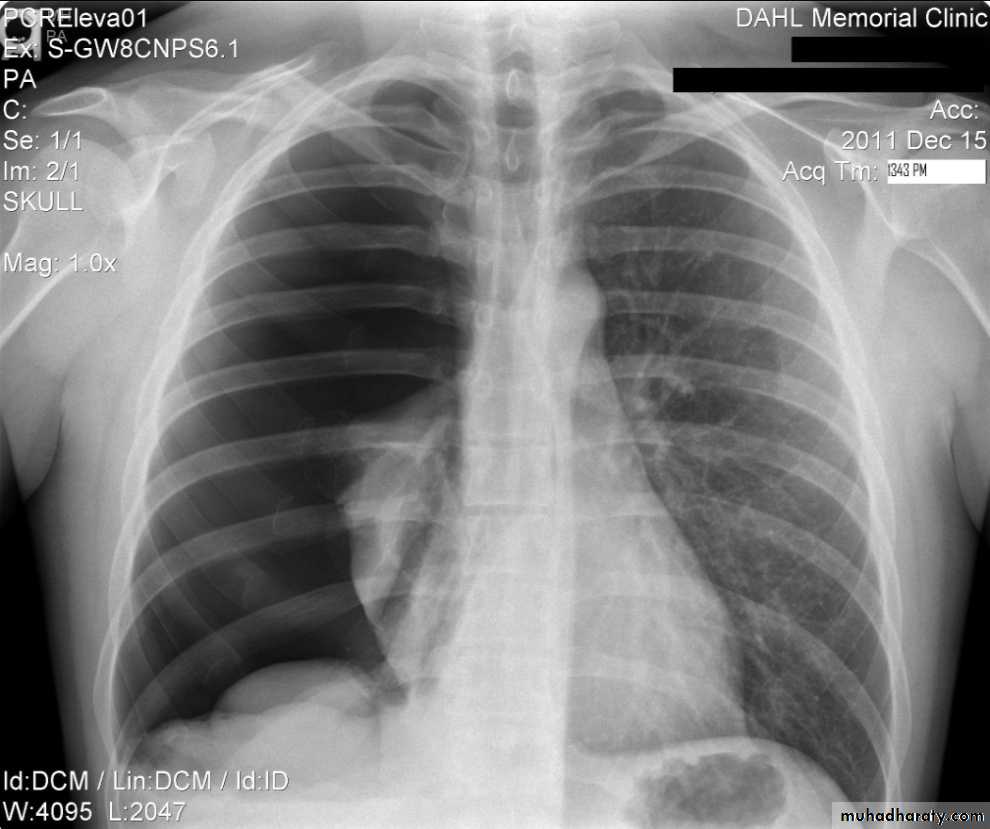
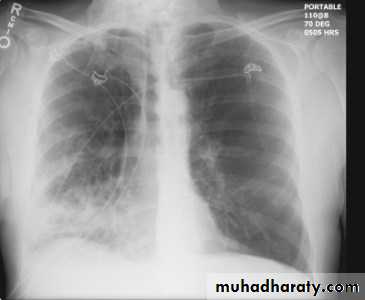
Hydropneumothorax is a term given to the concurrent presence of a pneumothorax as well as a hydrothorax (i.e. air and fluid) in the pleural space.Plain radiographs
On an erect chest radiograph, recognition of hydropneumothorax can be rather easy - and is clasically shown as an air-fluid level. On the supine radiograph, this may be more challenging where a sharp pleural line is bordered by increased opacity lateral to it within the pleural space may sometimes suggest towards the diagnosis 3,
Hydropnemothorax
Subcutaneous Emphysema
Subcutaneous emphysema, strictly speaking, refers to air in the subcutaneous tissues. But the term is generally used to describe any soft tissue emphysema of the body wall or limbs, since the air often dissects into the deeper soft tissue and musculature along fascial planes .Radiographic appearance
Plain film
If affecting the anterior chest wall, subcutaneous emphysema can outline the pectoralis major muscle, giving rise to the ginkgo leaf sign , dissecting air along tissue fat planes appears as multiple lines of lucency.
Subcutaneous Emphysema
Pneumomediastinum is the presence of extraluminal gas within the mediastinum. Gas may originate from the lungs, trachea, central bronchi, oesophagus, and track from the mediastinum to the neck or abdomen
Radiographic features
Small amounts of air appear as linear or curvilinear lucencies outlining mediastinal contours such as:
subcutaneous emphysema
air anterior to pericardium: pneumopericardium
air around pulmonary artery and main branches: ring around artery sign
air outlining major aortic branches: tubular artery sign
air outlining bronchial wall: double bronchial wall sign
continuous diaphragm sign: due to air trapped posterior to pericardium
air between parietal pleura and diaphragm: extrapleural sign
Chronic obstructive pulmonary disease (COPD)
represents a spectrum of obstructive airway diseases. It includes two key components which are chronic bronchitis-small airways disease and emphysemaChronic bronchitis (CB)
Chronic bronchitis (CB) is often defined as the presence of productive cough for 3 months in two successive years in a patient in whom other causes of chronic cough, such as tuberculosis, lung cancer and heart failure, have been excluded . It can be an important pathological compotent of chronic obstructive pulmonary disease . (often considered as a distinct phenotype of COPD)
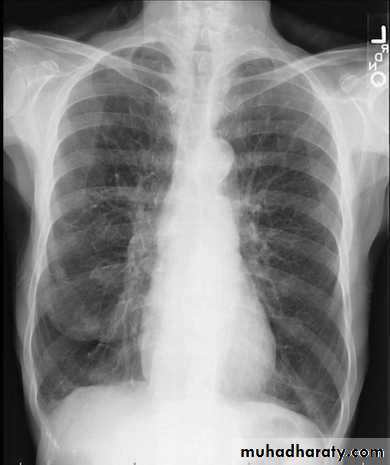
findings of chronic bronchitis on chest radiography
are nonspecific and include 1.increased bronchovascular markings and2.cardiomegaly other added radiological signs
* direct signs
3.thickened peripheral airways - may only be seen in the proximal portion
*indirect signs - many of these features may be non specific on their own
1.air trapping
2.subsegmental atelectasis
3.Dirty lung appearance
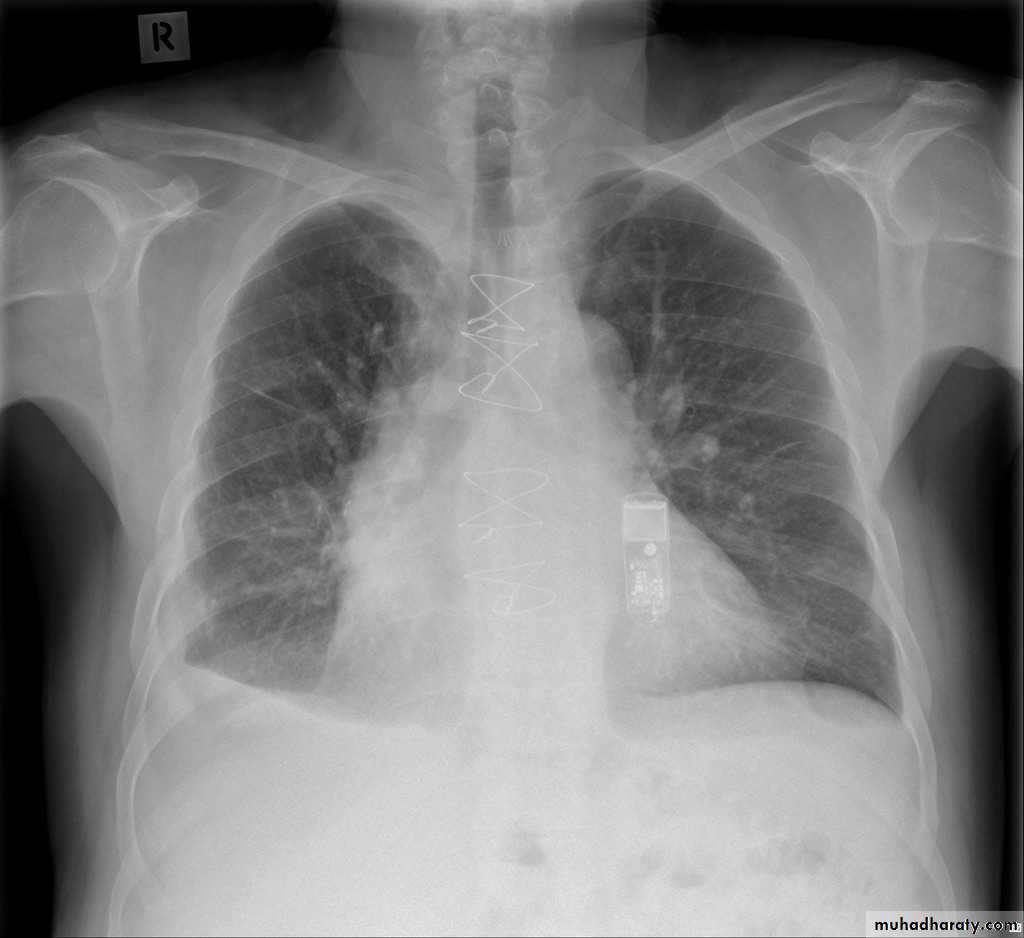
Pulmonary emphysema
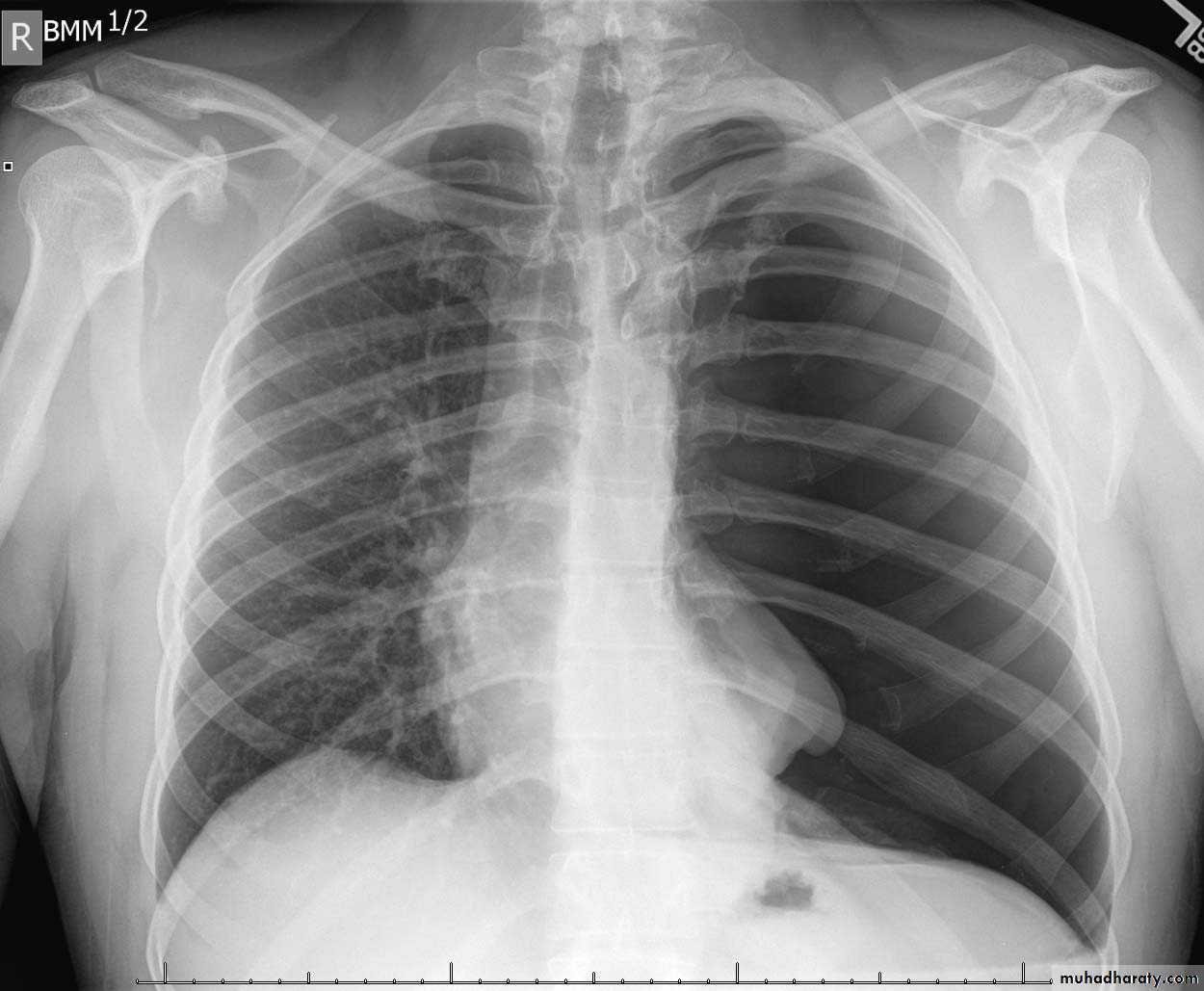
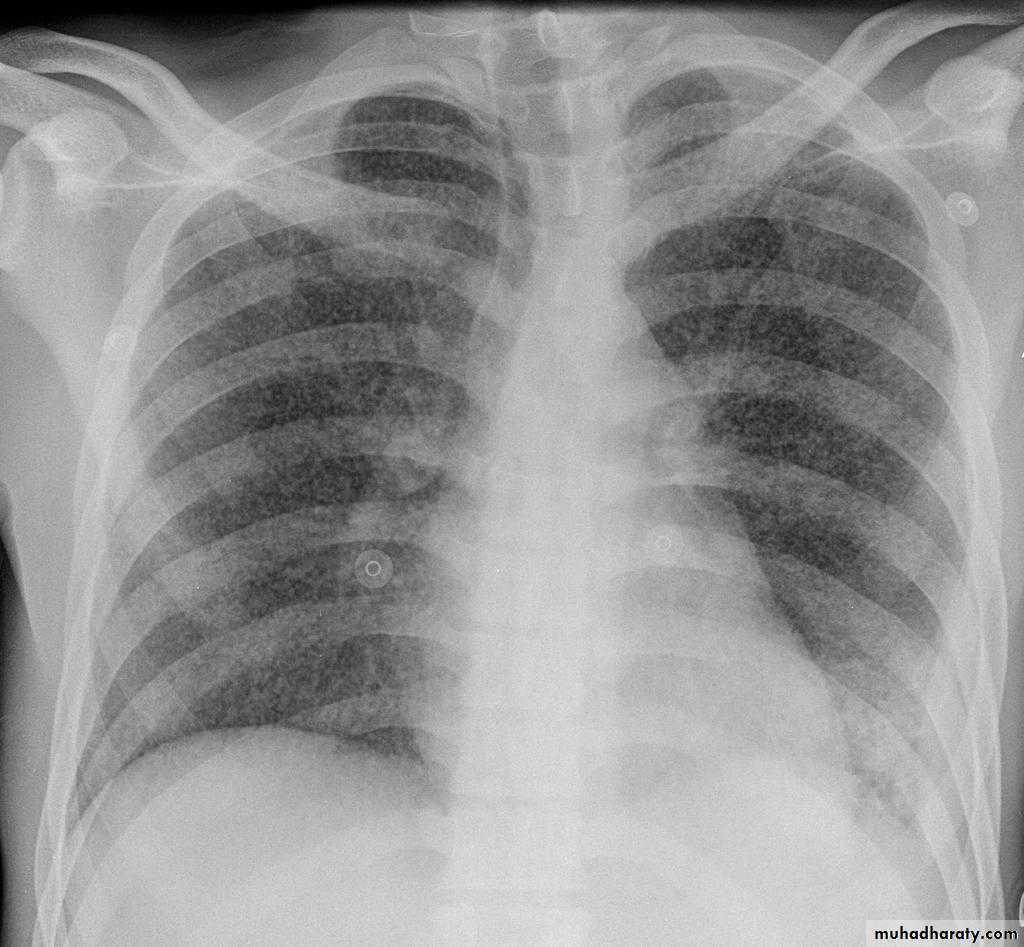
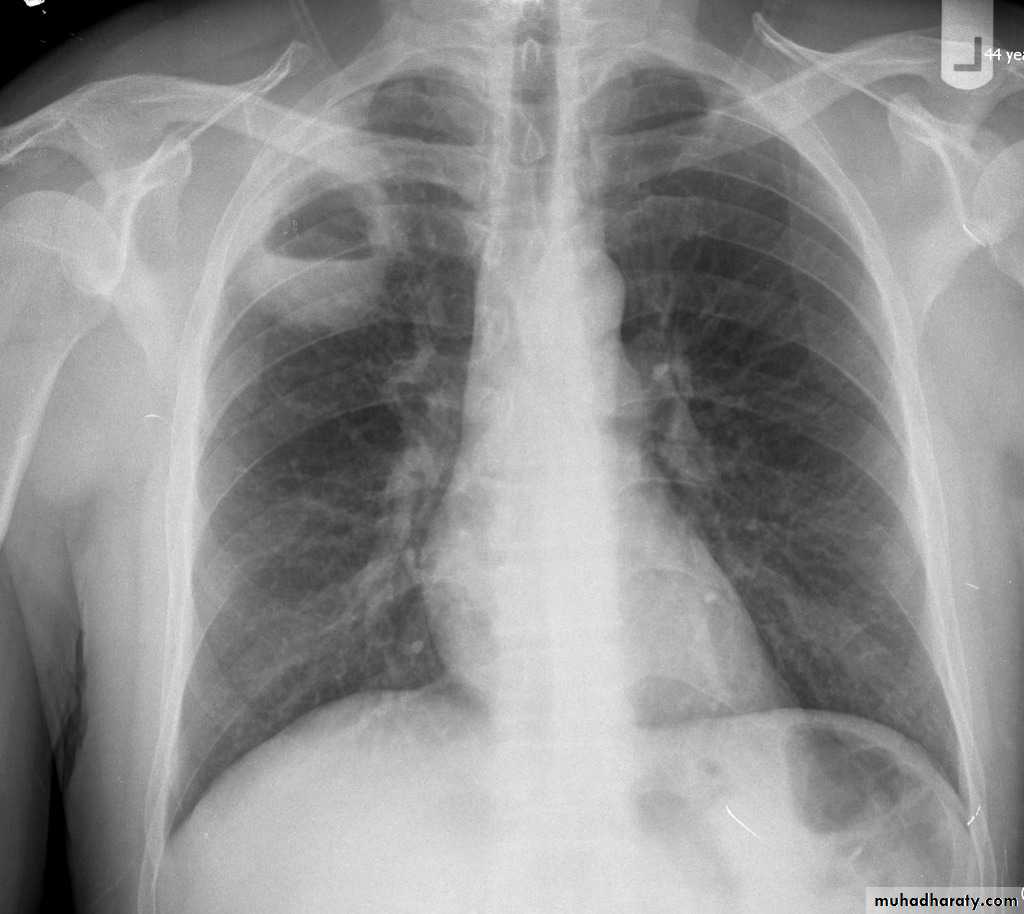
Pulmonary emphysema is defined as the "abnormal permanent enlargement of the airspaces distal to the terminal bronchioles accompanied by destruction of the alveolar wall and without obvious fibrosis". Emphysema is one of the entities grouped together as chronic obstructive pulmonary diseaseRadiographic features
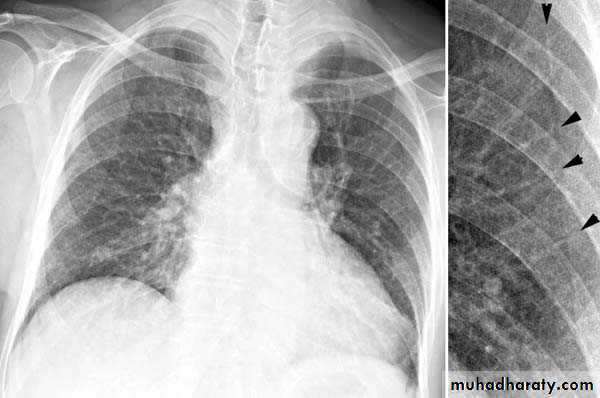
Plain film
Except in the case of very advanced disease with bulla formation, chest radiography does not image emphysema directly, but rather infers the diagnosis due to associated features :
hyperinflation:
1.flattened hemidiaphragm(s): most reliable sign
2.ncreased and usually irregular radiolucency of the lungs
3.increased retrosternal airspace
4.increased antero-posterior diameter of chest
5.widely spaced ribs
6.sternal bowing
7.tenting of the diaphragm
8.saber-sheath trachea
9.vascular changes paucity of blood vessels ( absent pulmonary markings in outer 1/3 of the lung fields )
10 .pulmonary arterial hypertension
pruning of peripheral vessels
increased calibre of central arteries
right ventricular enlargement
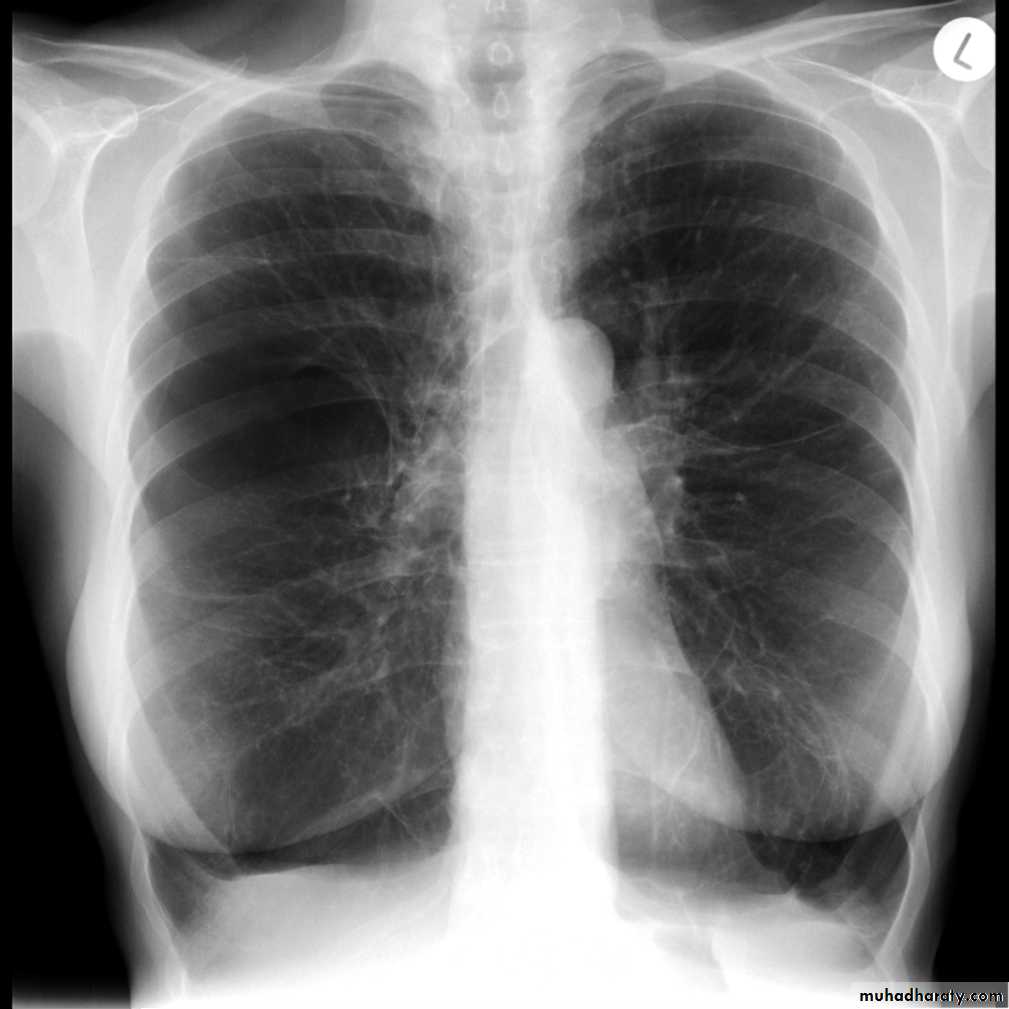
Emphyzema
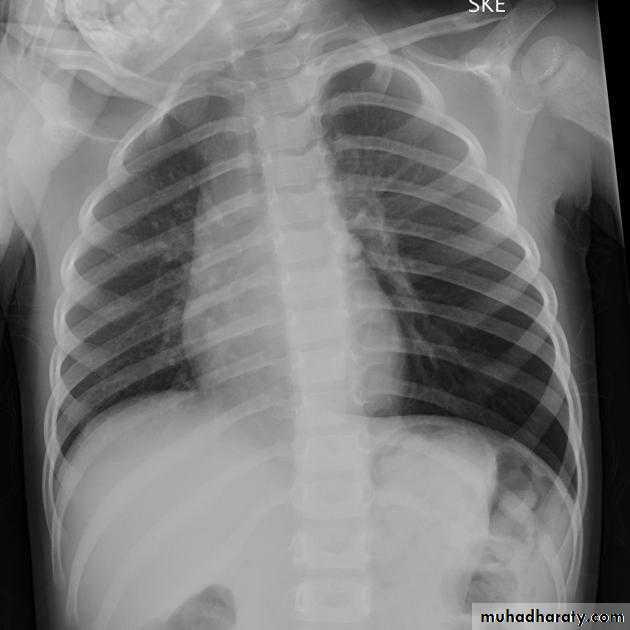
Unilateral obstructive emphysemaunilateral emphysema or atelectasis are the most common findings; only uncommonly will a radio-opaque foreign body be demonstrated ,Aspirated foreign bodies have a predominance for the right tracheo bronchial tree.
Pulmonary bullae are focal regions of emphysema with no discenible wall which measure more than 1cm in diameter
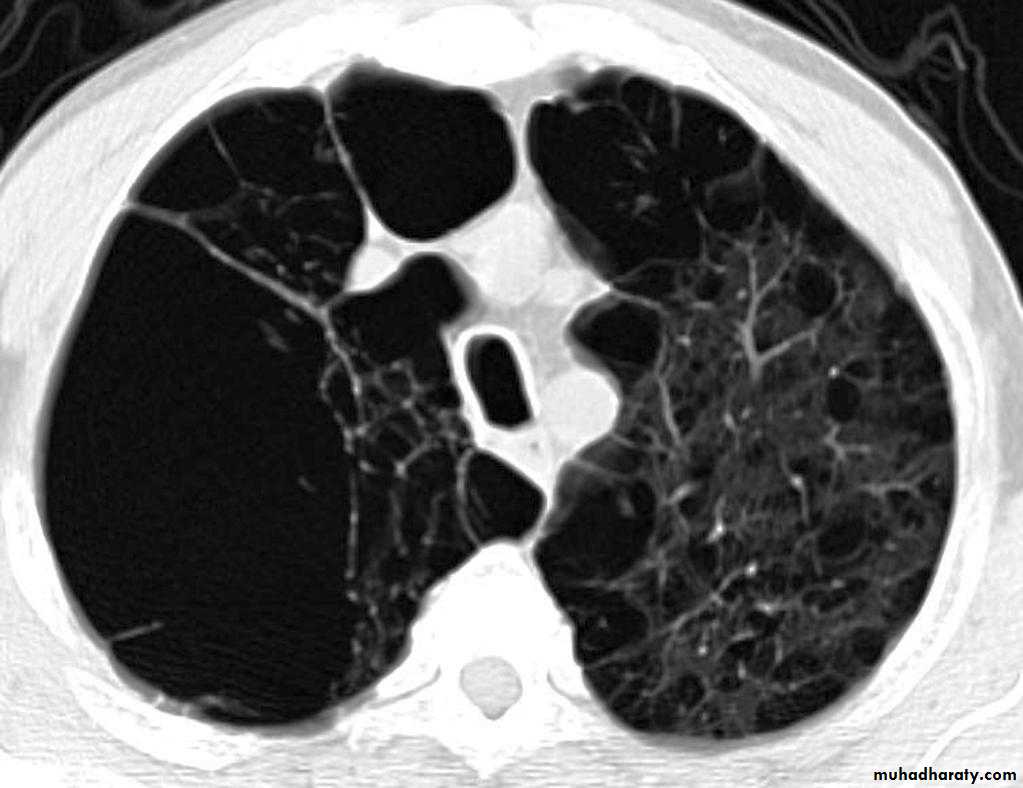
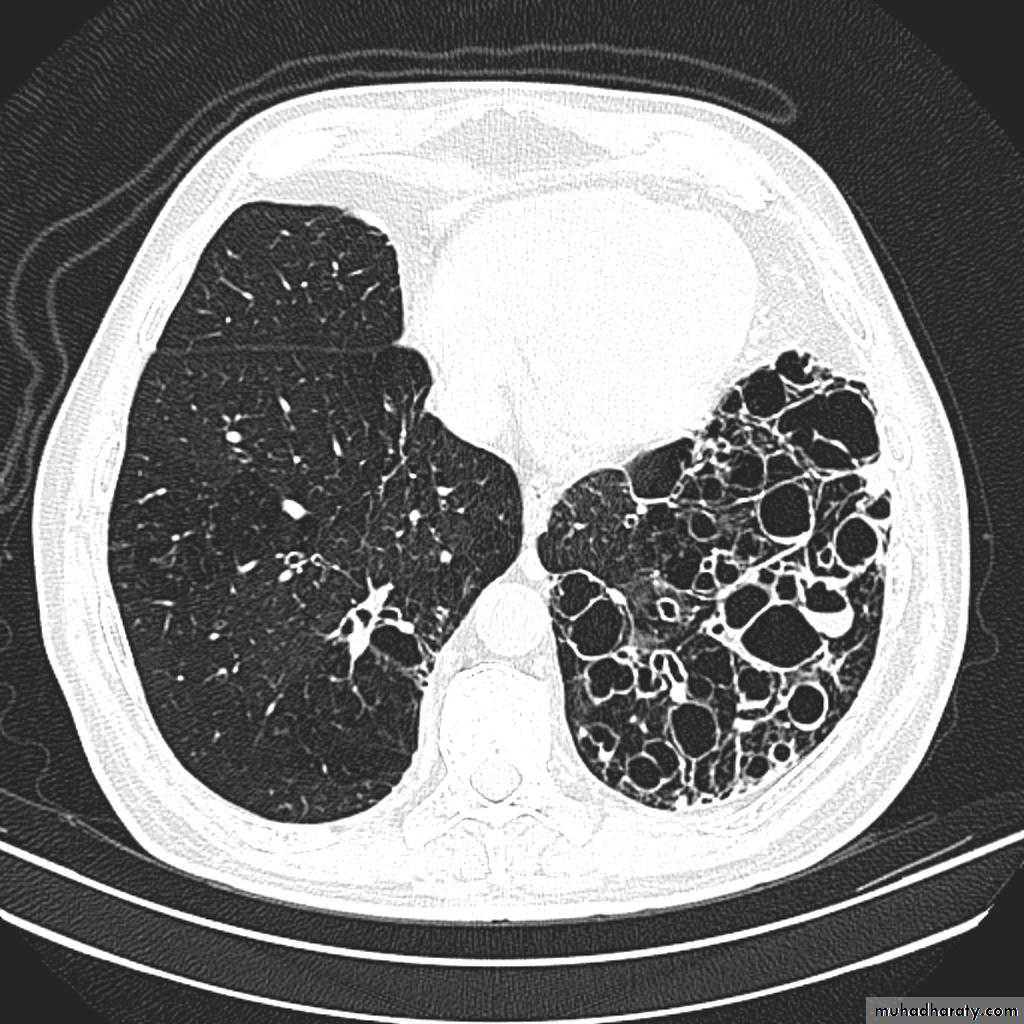
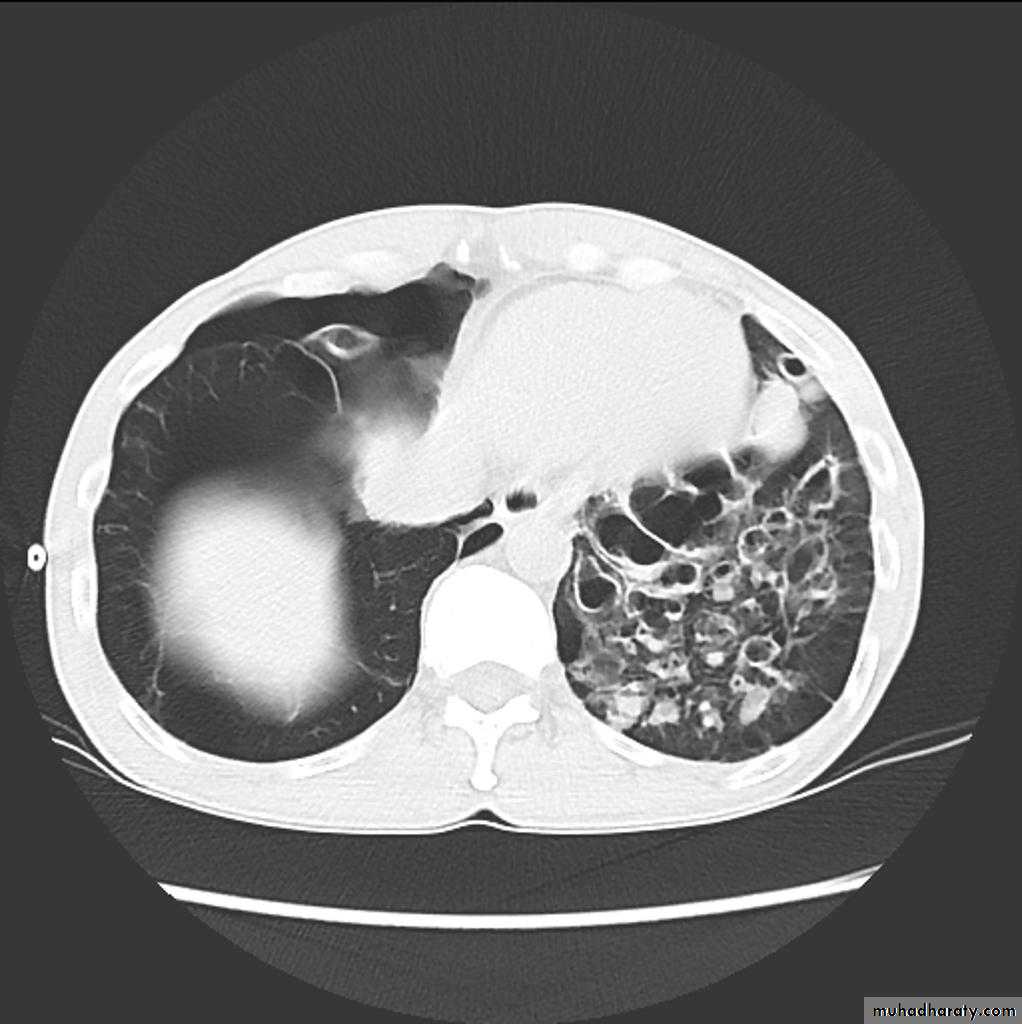
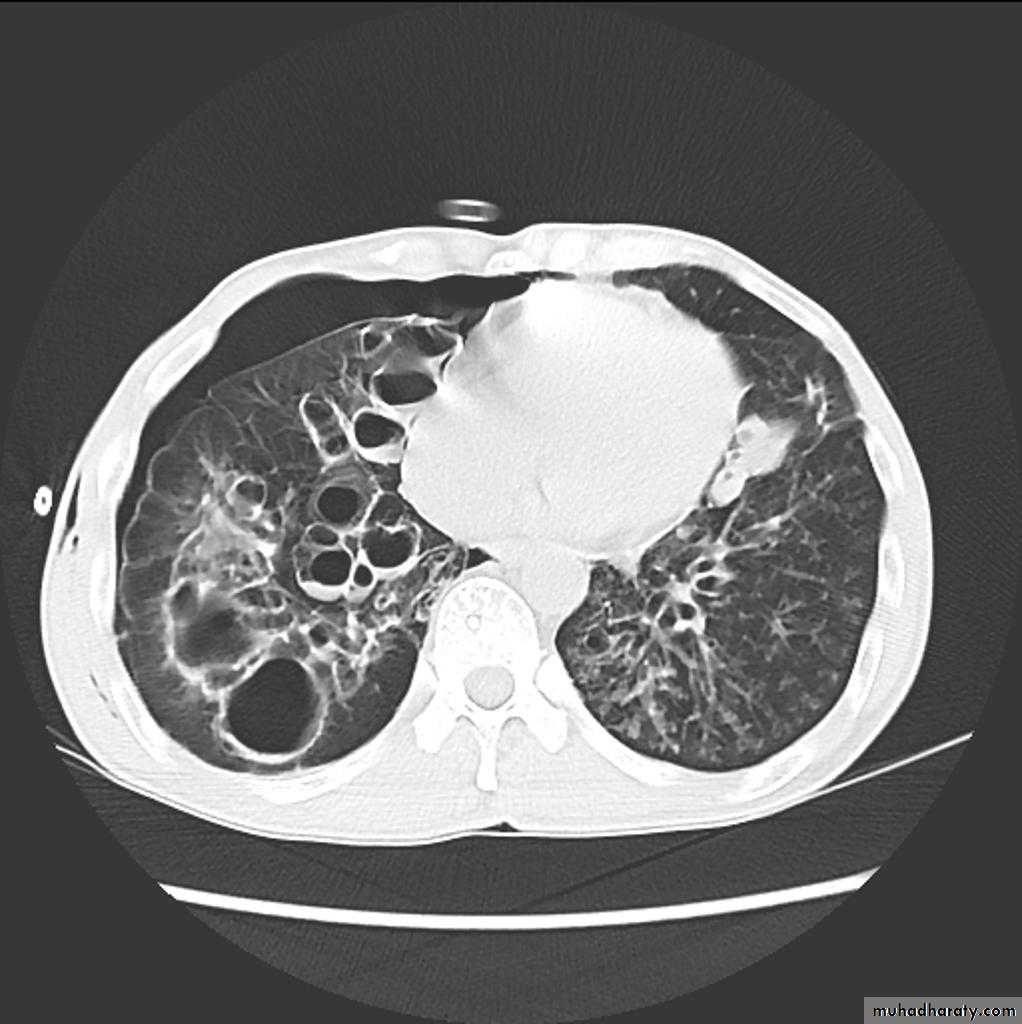
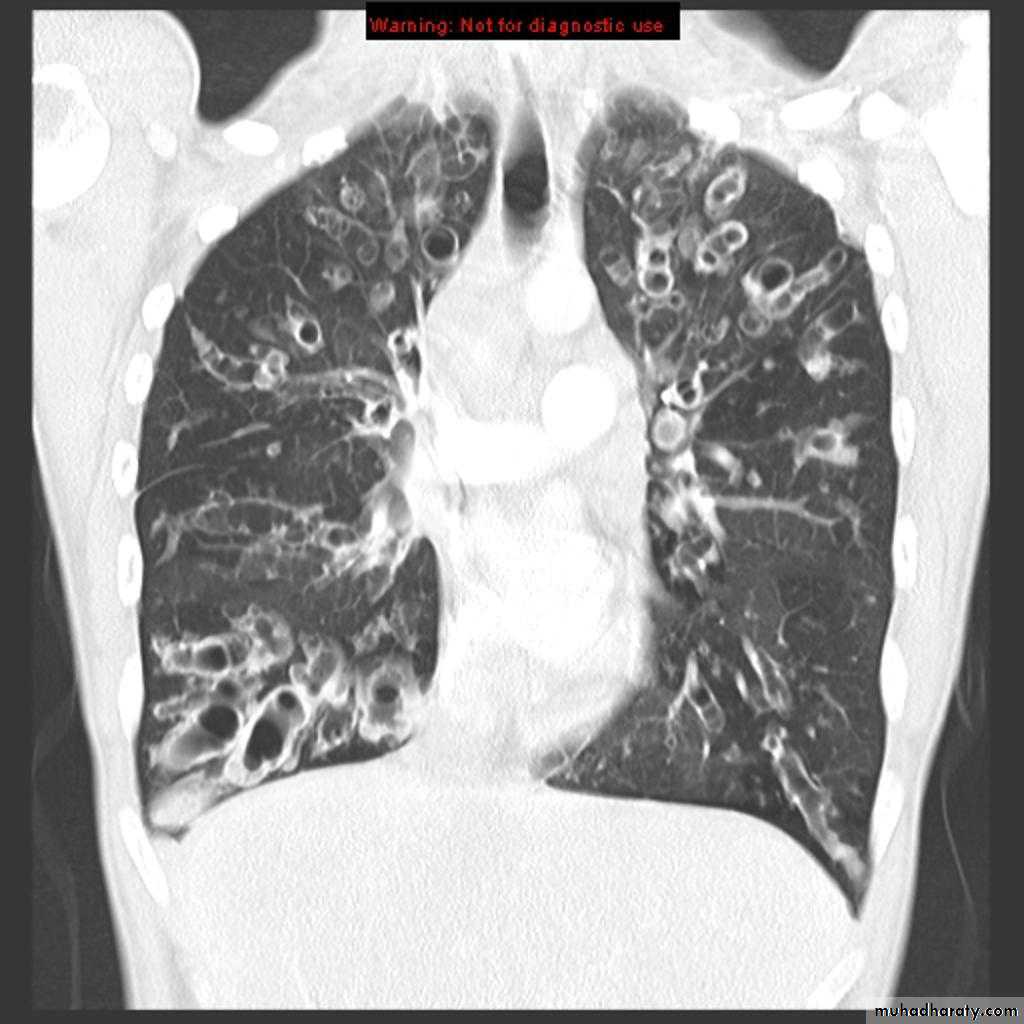
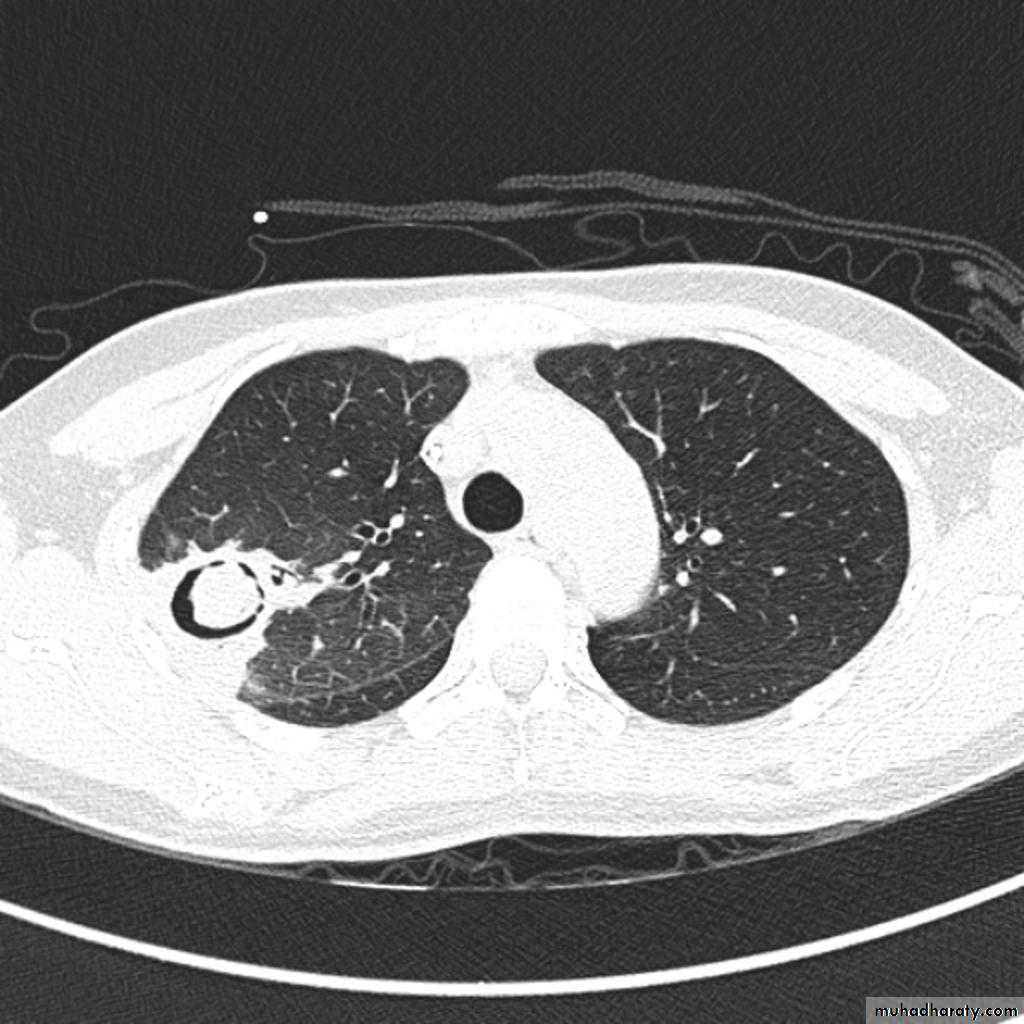
Bronchiactasis
Bronchiectasis refers to abnormal dilatation of the bronchial tree and is seen in a variety of clinical settings. CT is the most accurate modality for diagnosis. It is largely considered irreversibleCauses of bronchiactasias very important to consider
post-infective (most common)necrotising bacterial pneumonia, e.g Staph. aureus, Klebsiella, B. pertussis
granulomatous disease, e.g tuberculosis, MAIC, histoplasmosis
allergic bronchopulmonary aspergillosis (ABPA)
congenital
congenital cystic bronchiectasis
cystic fibrosis (CF)
ciliary dysfunction syndromes, e.g. Kartagener syndrome
bronchial obstruction
malignancy, e.g. bronchogenic carcinoma
inhaled foreign bodies
chronic aspiration lung changes
Plain radiograph
Chest x-rays are usually abnormal
1. Tram-track opacities are seen in cylindrical bronchiectasis, and
2. air-fluid levels may be seen in cystic bronchiectasis.
Honey comb shadow
3.Overall there appears to be an increase in bronchovascular markings, and bronchi seen end on may appear as ring shadows .
4.Pulmonary vasculature appears ill-defined, thought to represent peri bronchovascular fibrosis .
TB of the lung
Tuberculosis encompasses an enormously wide disease spectrum affecting multiple organs and body systems predominantly caused by the organism Mycobacterium tuberculosisPulmonary manifestations of tuberculosis are varied and depend in part whether the infection is primary or post-primary. The lungs are the most common site of primary infection by tuberculosis and are a major source of spread of the disease .
Have 2 categories
Primary
Post primary TB
Primary pulmonary TB
Radiographic featuresprimary pulmonary tuberculosis
1.the initial focus of infection can be located anywhere within the lung and has non-specific appearances ranging from too small to be detectable, to patchy areas or consolidation or even lobar consolidation in RT upper or RT middle lobe . Radiographic evidence of parenchymal infection is seen in 70% of children and 90% of adults called Ghon lesion , +/- ipsilateral hilar or paratracheal Lymph adenopathy usually right sided
( Ghon focus + LAP ) called primary complex.
2.Later In most cases, the infection becomes localized and a caseating granuloma resolve eventually calcifies with or without calcification of the regional LN , Calcification of nodes is seen in 35% of cases . When a calcified node and a calcified Ghon lesion are present, the combination is known as a Ranke complex.
3. Pleural effusions are more frequent in adults .
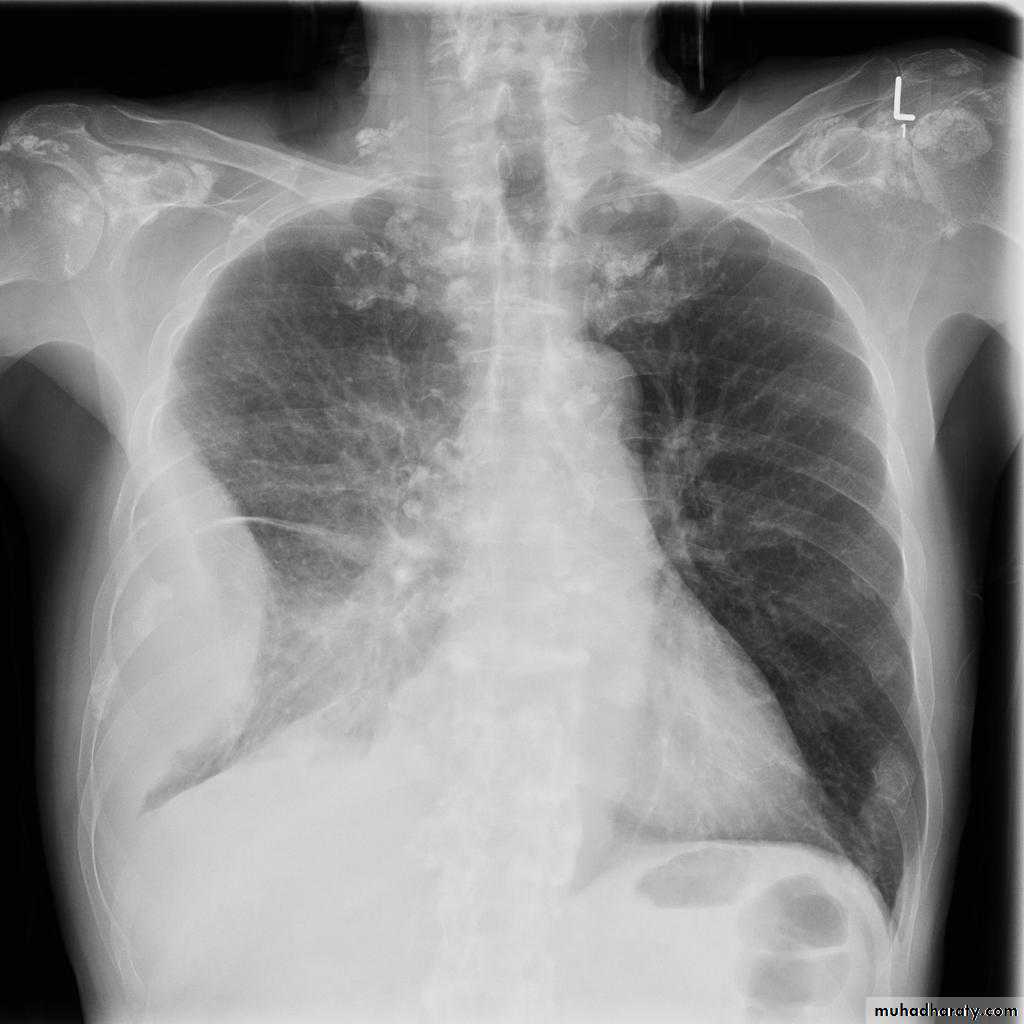
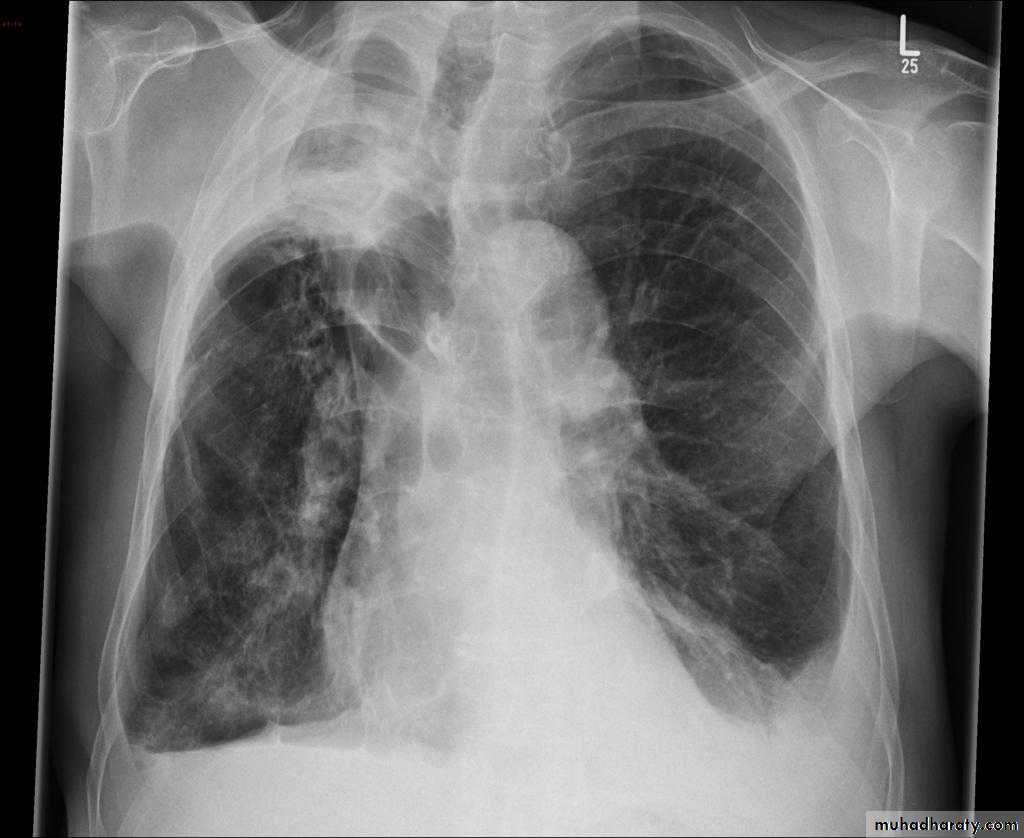
Post primary TB radiographic appearance
Post-primary pulmonary tuberculosis, also known as reactivation tuberculosis or secondary tuberculosis occurs years later, frequently in the setting of a decreased immune status. In the majority of cases, post-primary TB within the lungs develops in either :
* posterior segments of the upper lobes
*superior segments of the lower lobes
Typical appearance of post-primary TB
1.patchy consolidation or poorly defined linear and nodular opacities in both apices , upper zone in one lung , & lower zone in other lung ( ulternating lesion ) .2. Post-primary infections are far more likely to cavitate with multiple abscess formation & air fluid level more develop in the posterior segments of the upper lobes.
3. Tuberculomas seen in post-primary TB and appear as a well defined rounded mass typically located in the upper lobes .
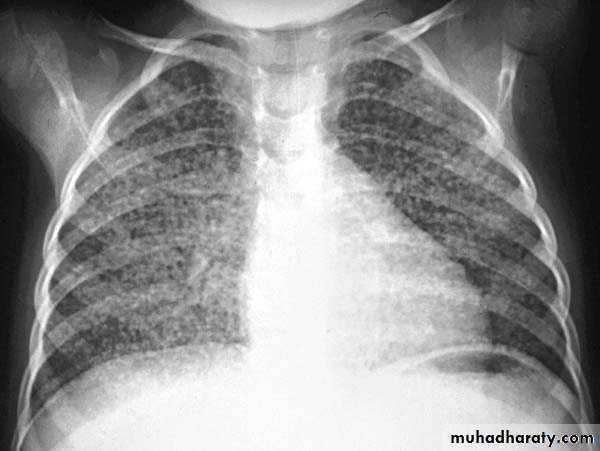
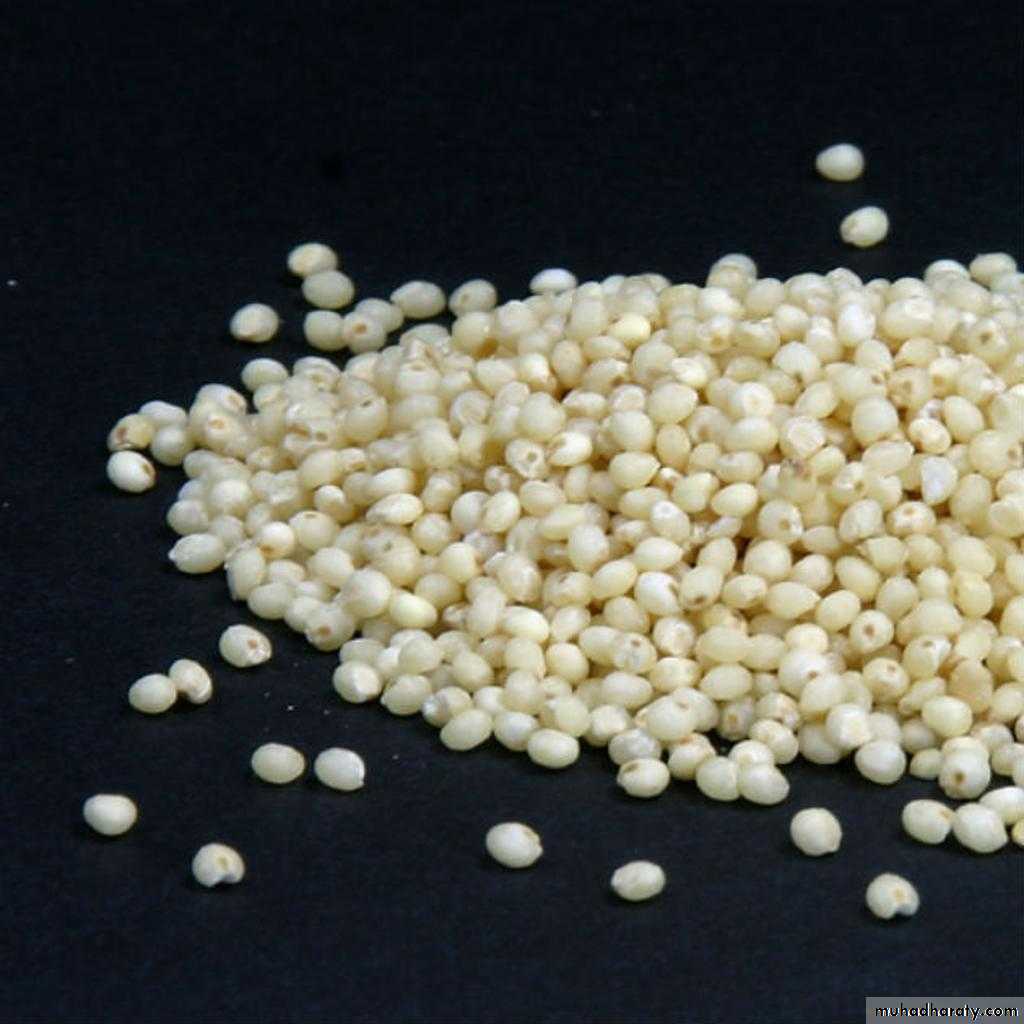
4. Miliary tuberculosis is uncommon but carries a poor prognosis. It represents haematogenous dissemination of an uncontrolled tuberculous infection. It is seen both in primary and post-primary tuberculosis. Although implants are seen throughout the body, the lungs are usually the easiest location to the image. Miliary deposits appear as 1-3 mm diameter nodules . are uniform in size and uniformly distributed
TB abscess
Complications
Recognized complications include:1.colonisation of cavities by fungus, e.g. aspergilloma
2.bronchiectasis
3.arterial pseudoaneurysms
bronchial artery pseudo aneurysm
pulmonary artery pseudo aneurysm / Rasmussen aneurysm
4.empyema
5.fibrothorax
6.bronchopleural fistula
Aspergiloma