SOURCES
Contemporary_Oral_and_Maxillofacial _ Surgery_4th_Ed_By_Peterson.Peterson's Principles of Oral and Maxillofacial Surgery 2nd Ed 2004.
Oral Surgery.Hand Book Local Anasthesia.
LOCAL ANEASTHESIADefinition of local anesthesia
L.A. defined as a loss of sensation in a circumscribed area of the body caused by a depression of excitation in nerve ending or an inhibition of the conduction process in peripheral nerves.Methods of inducing L.A.
In the “old days” the following were used for anesthesia.Alcohol
Drugs
Ice for numbing
Blow to the head
Strangulation
Methods of inducing L.A.
Mechanical traumaLow temperature
Anoxia
Chemical irritation
Neurolytic agents like alcohol
Chemical agents such as L.A.
Properties of ideal L.A.
Onset of anesthesia should be short while duration and effect of anesthesia should be long and powerfulL.A should not irritate tissues
L.A should not cause permanent damage to nerves
L.A should be effective even with lower doses
L.A should has lower systemic adverse effects
L.A should not be allergic
Properties of ideal L.A
L.A can be sterilized easily
L.A should be soluable within water
L.A should be cheap
L.A should be stabile
L.A should not get interaction with vasoconstrictors
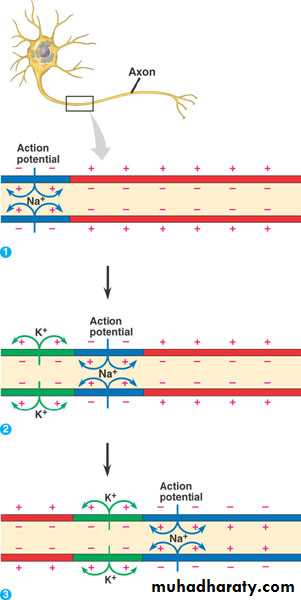
Neurophysiology
Electrochemistry of nerve conductionResting state
Depolarization
Re polarization
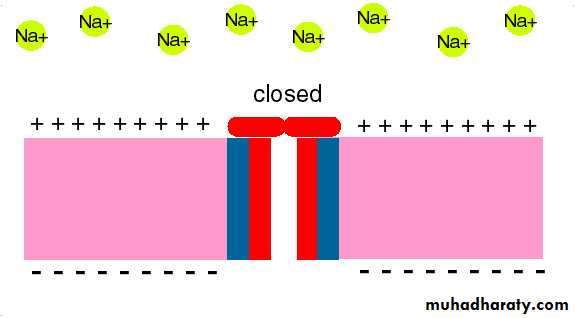
Mode of action of L.A.
Altering the basic resting potential
Altering the threshold potential(firing level)
Decreasing the rate of depolarization
Prolonging the rate of repolarization
What functions are lost with local anesthetics?
AnswerPain perception
Temperature
Touch sensation
Proprioception (reception of information about body position movements by the sensory systems )
Skeletal muscle tone
Factor affecting the local anesthetic action
1- PH value. Acidification of tissue decrease LA effectiveness Inadequate anesthesia result when local anesthetics are injected in to inflamed or infected areas since the inflammatory process produce acidic products.
2- Lipid solubility .↑ lipid solubility ↑ local anesthetic effect.
3- Protein binding . ↑ protein binding ↑LA duration .
4- Non nervous tissue diffusibility .
5-↑ Vasodilator activity ↓ LA solution activity.
Pharmacokinetic of local anesthetics
Administration.Distribution.
Metabolism.
Excretion.
Induction of L.A.
1-Diffusion2-Blocking process
Recovery of L.A.
note all LA readily cross the blood brain barrier & also readily cross the placenta & enter the circulatory system of developing fetus.
Administration
Oral rout
Topical routInjection
Distribution
The blood level of L.A. influenced byRate at which the drug is absorbed into CVS
Rate of distribution from vascular component into the tissue
Elimination by excretion
Continue
The rate at which the drug is removed from the blood mentioned as half lifeOne half life =50% reduction
Two half life=75% reduction
Three half life=87.5 reduction
Four half life=94% reduction
Five half life=97% reduction
Six half life= 98% reduction
Metabolism
Metabolism of L.A is important because the overall toxicity of the drug depend on the rate of absorption of the drug into the blood stream and its rate of metabolism and excretion.
Esters→ Hydrolysis in Plasma
Amides→ Liver
Excretion
Kidneys are the primary excretory organ for both local anesthetic drug and its metabolite.Summary
Clinical PharmacologyThe potency of Local Anesthetics, their onset and duration of action are primary determined by physicochemical properties of various agents and their inherent vasodilator activity of same local anesthetics.
Lipid solubility is the primary determinant of anaesthetic potency.
Protein binding influences the duration of action.
(acidity constant) of Local anaesthetics determines the onset of action.
The addition of vasoconstrictors, such as epinephrine or phenylephrine can prolong duration of action of local anaesthetics, decrease their absorption (and the peak plasma level) and enhance the blockade.
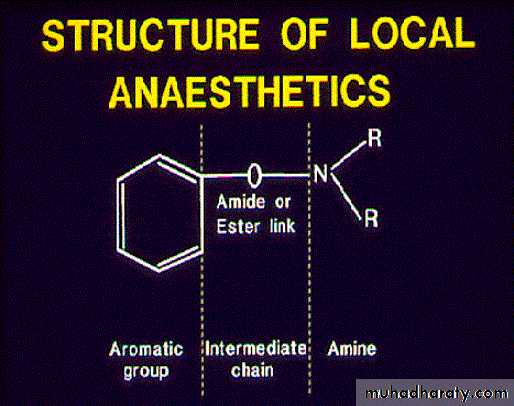
Chemistry
Three structural domains1) Aromatic or Lipophilic portion
-necessary for penetration lipid rich
nerve membranes
2) Amino end (hydrophilic end)
-confers water solubility
-ensures solubility of local in cartridge and prevent precipitation
3) Intermediate chain (-COO-) or (-NHCO-)
-provides spatial separation and divides local into esters or amidesLocal Anesthesia
EstersShort acting
Metabolized in the plasma and tissue fluids
Excreted in urine
Local Anesthesia
AmidesLonger acting
Metabolized by liver enzymes
Excreted in urine
Ester L.As are more allergic than amide L.As
Local Anesthesia
EstersCocaine.
Benzocaine.
Procaine.
Tetracaine.
Drug List
Local AnesthesiaAmides
Bupivacaine.
Articain.
Lidocaine (Xylocaine).
Mepivacaine.
Drug List
Properties of Local Anaesthetic Agents
• PROPERTIES• AMINOESTERS
• AMINOAMIDES
• Metabolism
• rapid by plasma cholinesterase
• slow, hepatic
• Systemic toxicity
• less likely
• more likely
• Allergic reaction
• possible - PABA derivatives form
• very rare
• Stability in solution
• breaks down in ampules (heat,sun)
• very stable chemically
• Onset of action
• slow as a general rule
• moderate to fast
• pKa's
• higher than PH = 7.4 (8.5-8.9)
• close to PH = 7.4 (7.6-8.1)
bupivacaine (Marcaine)
levobupivacaine
Lidocaine (Xylocaine)
lidocaine-prilocaine (EMLA)
mepivacaine (Carbocaine
Benzocaine
Chloroprocaine
Dyclonine
Procaine
tetracaine
Systemic action of L.A.
CNS→The primary action is depression
Anticonvulsant properties
Analgesia
Mood elevation
Preconvulsive signs and symptoms of CNS toxicity
Signs SymptomsSlurred speech Numbness of Tongue
and circumoral region
Shivering Warm flushed feeling of
skin
Tremor of muscle of face Pleasant dream like
and extremities state
Dizziness
Visual disturbanceTinnitus
Drowsiness
Disorientation
Signs Symptoms
Slurred speech Numbness of Tongue
and circumoral region
Shivering Warm flushed feeling of
skin
Tremor of muscle of face Pleasant dream like
and extremities state
Dizziness
Visual disturbanceTinnitus
Drowsiness
Disorientation
CVS
Direct action of L.A. on myocardium:
It will cause myocardial depression
↓ electrical excitability
↓ Conduction rate
↓ force of contraction
Continue
Direct action on peripheral vasculature
Cocaine is the only local anesthetic drug that cause vasoconstriction all others produce vasodilatation.
Local tissue toxicity
Skeletal muscles are subjected to the action of local anesthetic drugs more than other tissues intraoral and intramuscular injection of lidocaine,atricaine, mepivicaine, prilocaine, bupivacaine and etidocaine will produce skeletal muscle alteration.Respiratory system
At a non overdose Local anesthetic drugs have a direct relaxant action on bronchial smooth muscleAt overdose level they may produce respiratory arrest as a result of generalized CNS depression
Vasoconstrictors
for local anesthetic agentsLocal Anesthetics
VasodilatationVasodilatation
Procain (highest vasodilatation effect)
Prilocain, mepivacain
Vasodilatator effect of local anesthetics…
Increases absorbtion of anesthetic solution leading rapid move away of solution from injection area
Decreases depth and duration of anesthesia
Increases the plasma level of L.A that may cause possible TOXICITY
Causes increased bleeding due to increased vasodilatation
Vasoconstrictor (vasopressor)
agents acts oppositeto local anesthetics
by constricting vessels
Why adding vasoconstrictors to L.A. (Advantages of vasoconstrictors)
↓ blood flow to the site of administrationAbsorption of L.A. to the CVS is slowed resulting in lower level of anesthetic drug in the blood
Minimize the risk of toxicity by lowering the blood level of L.A. drug
↑ duration of action
↓bleeding at side of administration
Classification of vasoconstrictors according to chemical structure
Catecholamine's Noncatecholamines
Epinephrine Amphetamine
Nor epinephrine Methamphetamine
Levonordefrin Ephedrine
Isoproterenol Mephentermine
Dopamine Hydroxyamphetamine
Metaraminol
Methoxamine
phenylephrine
Classification of vasoconstrictors according to mode of action
Direct acting Indirect acting Mixed actingEpinephrine Tyramine Metaraminol
Norepinephrine Amphetamine Ephedrine
Levonordefrin Methamphetamine
Isoproterenol Hydroxyamphytamine
Dopamine
Methoxamine
Phenylephrine
Dilutions of vasoconstrictors
The most common dilutions of vasoconstrictors used in dentistry are:
1:50000
1:80000
1:10000
1:100000
1:200000
1:300000
1:400000
Epinephrine
NorepinephrinePharmacology of vasoconstrictors
EPINEPHRINE:Mode of action:
Act directly on α and β receptors but more predominate on β receptor
Systemic action:
1-Myocardium:
Adrenaline stimulate β1 receptors of the myocardium
↑ cardiac output and heart rate
Continue
2-Pacemaker cells:
↑ incidence of dysarthmias
3-coronory arteries:
↑ coronary arteries blood flow4- BP:
In small doses ↑ systolic BP, ↓ Diastolic BPIn larger doses ↑ diastolic BP
Continue
Cardiovascular dynamic:↑ Systolic and diastolic pressure
↑ Cardiac output
↑ Heart rate
↑ strength of contraction
Continue
5- Vasculature:Adrenaline produce constriction of vasculatures which supplying skin, mucous membrane and kidneys
While its effect on vessels supplying skeletal muscle in small doses it produce dilatation while in larger doses produce vasoconstriction
6-Hemostasis:
Adrenaline is used frequently as vasoconstrictor during surgical procedures
7- Respiratory system:
It’s a potent dilator of bronchiole smooth muscle
Continue
8- CNS:
In normal therapeutic doses it have no effect on CNS while in an excessive dose it stimulate CNS
↑ fear, anxiety, restlessness, headache, tremor, weakness and dizziness.
Side effects of overdose:
Cardiac dysarthmiaVentricular fibrillation
Dramatic increase in both systolic and diastolic BP
Angina episode
Clinical applications
Management of acute allergic reactionManagement of bronchospasm
Management of cardiac arrest
For haemostatic
Increase depth of anesthesia
Increase duration of anesthesia
To produce mydriasis
Availability in dentistry
Epinephrine dilution LA
1:50,000 Lidocaine
1:80,000 Lidocaine
1:100,000 Lidocaine
Atricaine
1:200,000 Atricaine
Bupivacaine
Etidocaine
Lidocaine
Mepivacaine
Prilocaine
1:300,000 Lidocaine
NOREPINEPHRINE (NORADRENALINE, LEVARTERENOL)
Released from similar source like epinephrineEffectiveness is one fourth of epinephrine
It has intensive adrenargic stimulative effect which may cause possible tissue necrosis. (especially within palatinal region in the mouth)
Its use with L.A is controversial.
SYSTEMIC EFFECTS OF NOREPINEPHRINE
Cardiovascular systemIncreases systolic and diastolic blood pressure
Decreases heart rate
Increases volume of heart
It has no bronchodilatator effect
Increases metabolism but less effective than epinephrine
It causes vasoconstriction
Selection of vasoconstrictors
1-length of dental procedure.
2-Requirement of haemostatic.3-Medical status of patient.