Neoplasia
Dr. Nadwa S. M.Al-azowDefinition
A neoplasm( new growth) is defined as anabnormal mass of tissue, whose growth is uncoordinated with and exceeds that of the normal tissues.
The tumor arise from one clone that undergo genetic changes and uncontrolled proliferation
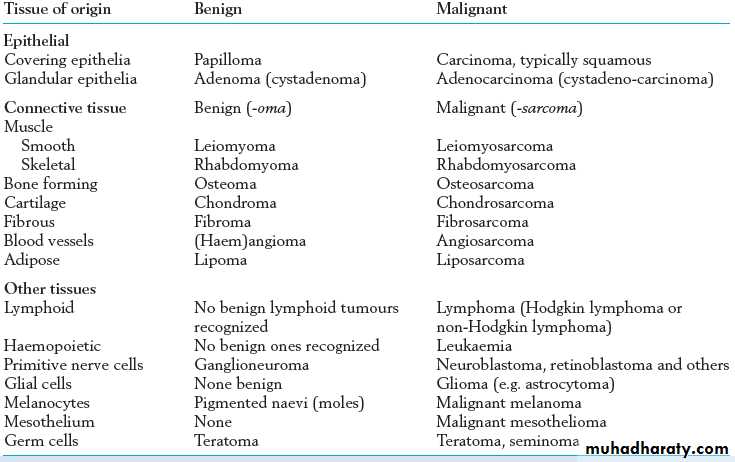
Classification of Tumours
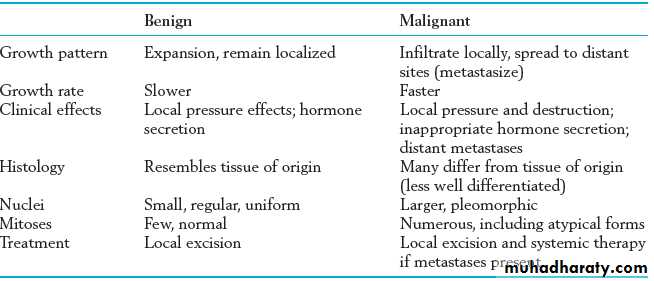
BenignMalignant
EpithelialMesenchymal
Epithelial
Mesenchymal
Benign Epithelial tumors
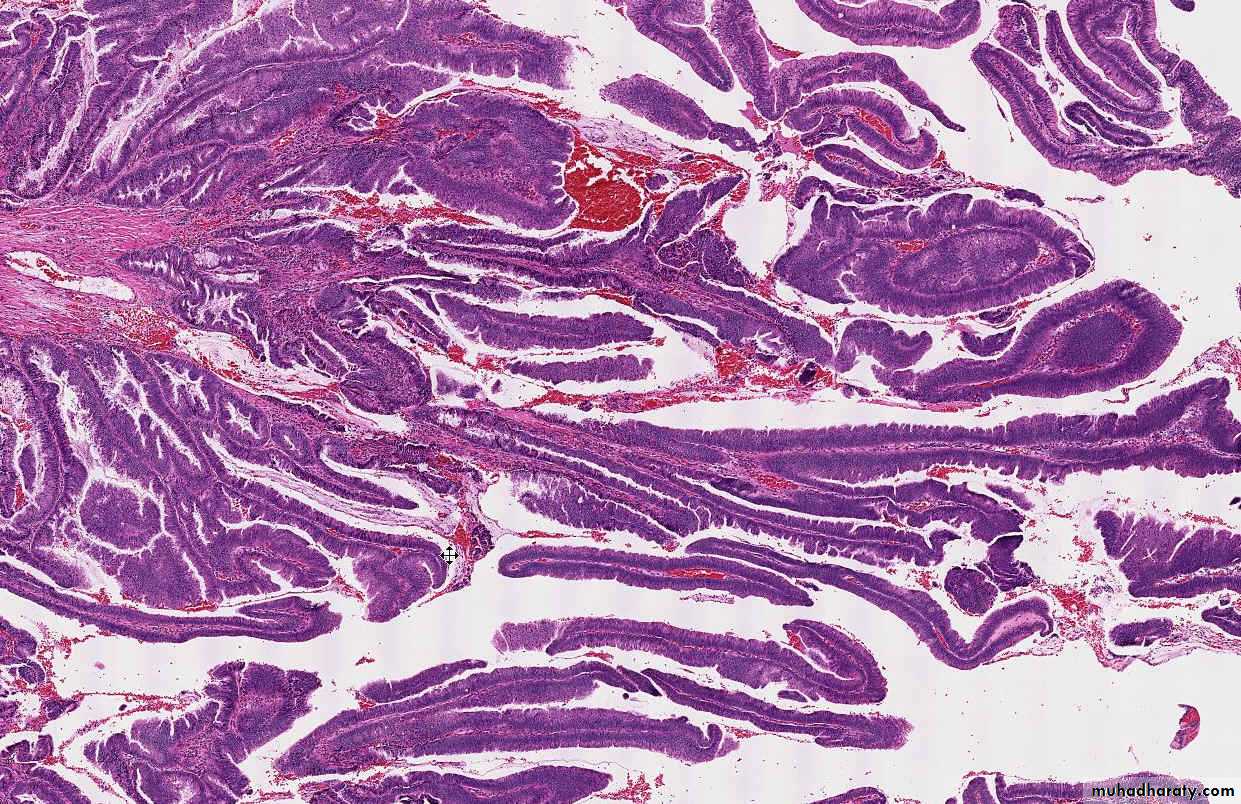
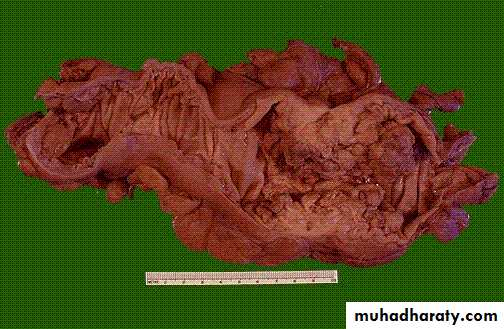
Tumor arising from covering epithelia called papilloma like squamous papilloma arising from tissue that lined by stratified squamous epithelium like skin, esophagus….Or glandular epithelia called adenoma like thyroid or breast adenoma….
Malignant epithelial tumor
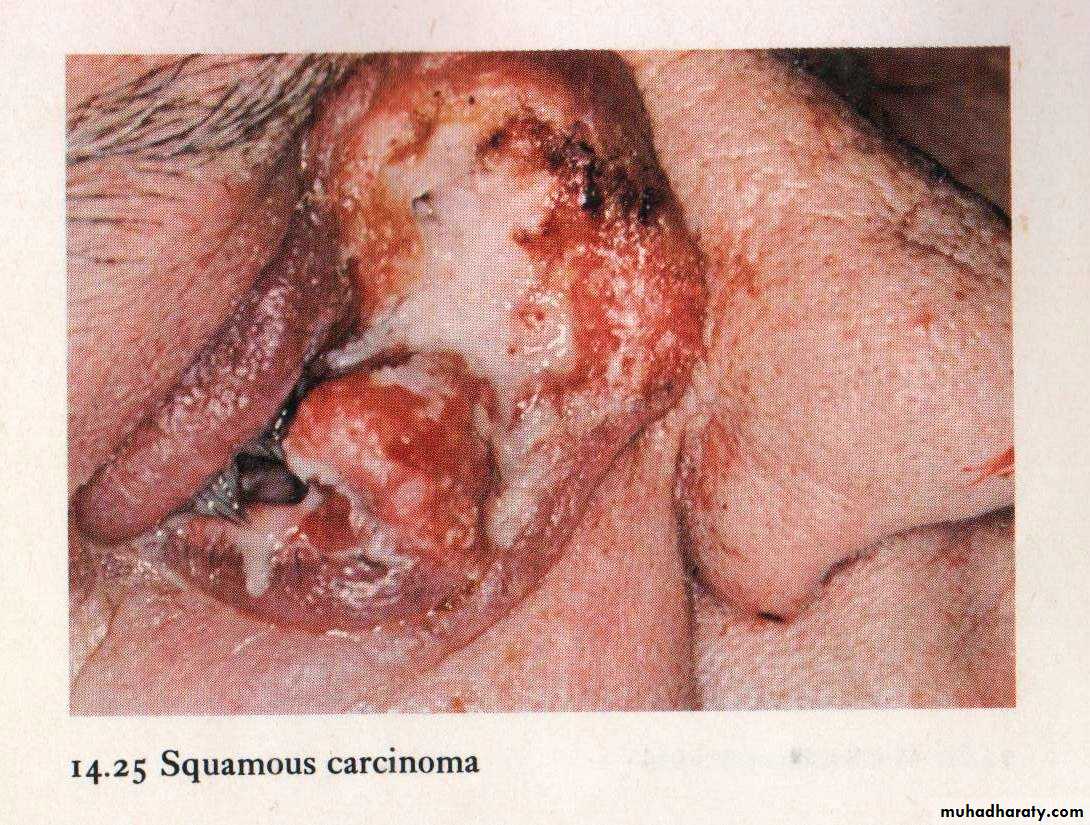
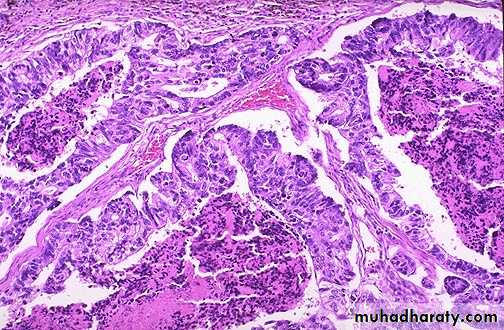
Squamouas carcinoma tumor arise from squamous epthelia with features of malignancyAdenocarcinoma malignant tumor arise from glandular epithelia
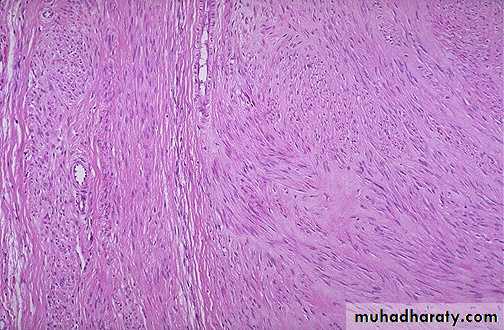
Benign Mesenchymal tumor
The nomenclature of these tumours is straightforward – the name consists of a prefix indicating the type of differentiation,for example lipo- (fat), chondro- (cartilage), haemangio-(blood vessel), with the suffix -oma denoting a benign tumour.
General features:
Most are slowly growing
encapsulated tumours
composed of the appropriate differentiated tissue
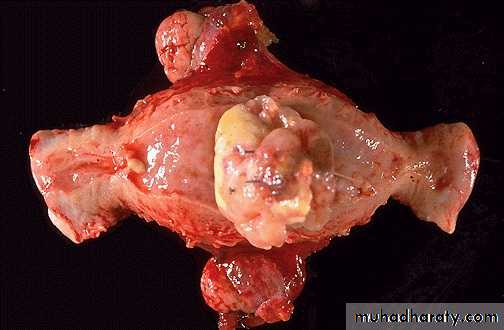
Malignant mesenchymal tumors
These are known as sarcomas . They arefar less common than carcinomas.
Most occur within the deep soft tissue of the limbs and trunk, although some arise within viscera.
Leiomyosarcoma ,liposarcoma , Rhabdomyosarcoma…
Tumours of Haemopoietic and Lymphoid Tissues
Tumors that arise from stem cells of white blood cells in the bone marrow leukemia
malignant solid tumours of lymphocytic origin, most of which arise in lymph nodes, spleen, thymus or bone marrow Lymphomas
Tumors with mixed differentiation
mixed tumors: e.g. pleomorphic adenoma of salivary glandTeratoma
tumor comprised of cells from more than one germ layerarise from totipotent cells (usually gonads)
benign cystic teratoma of ovary is the most common teratoma
Aberrant differentiation (not true neoplasms)
Hamartoma: disorganized mass of tissue whose cell types are indiginous to the site of the lesion, e.g., lung
Choriostoma: ectopic focus of normal tissue (heterotopia), e.g., pancreas,
Misnomers
hepatoma: malignant liver tumor
melanoma: malignant skin tumor
seminoma: malignant testicular tumor
lymphoma: malignant tumor of lymphocytes
Differences between benign &malignant tumor
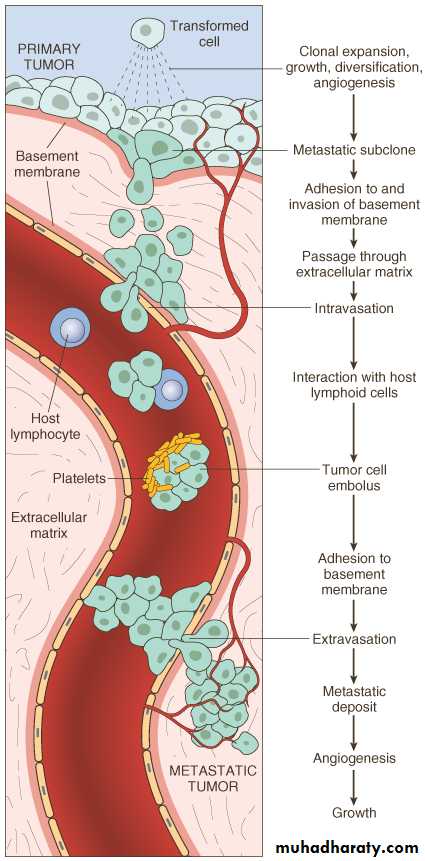
SPREAD OF MALIGNANT TUMOURSForms of tumour spread include:
• local spread• lymphatic spread
• blood (haematogenous spread)
transcoelomic spread
• intraepithelial spread
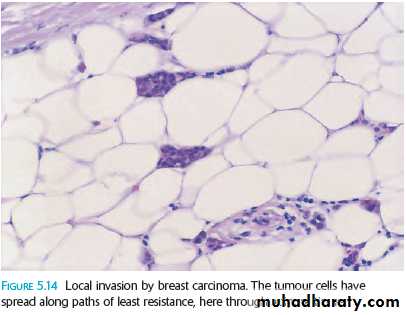
Local Spread
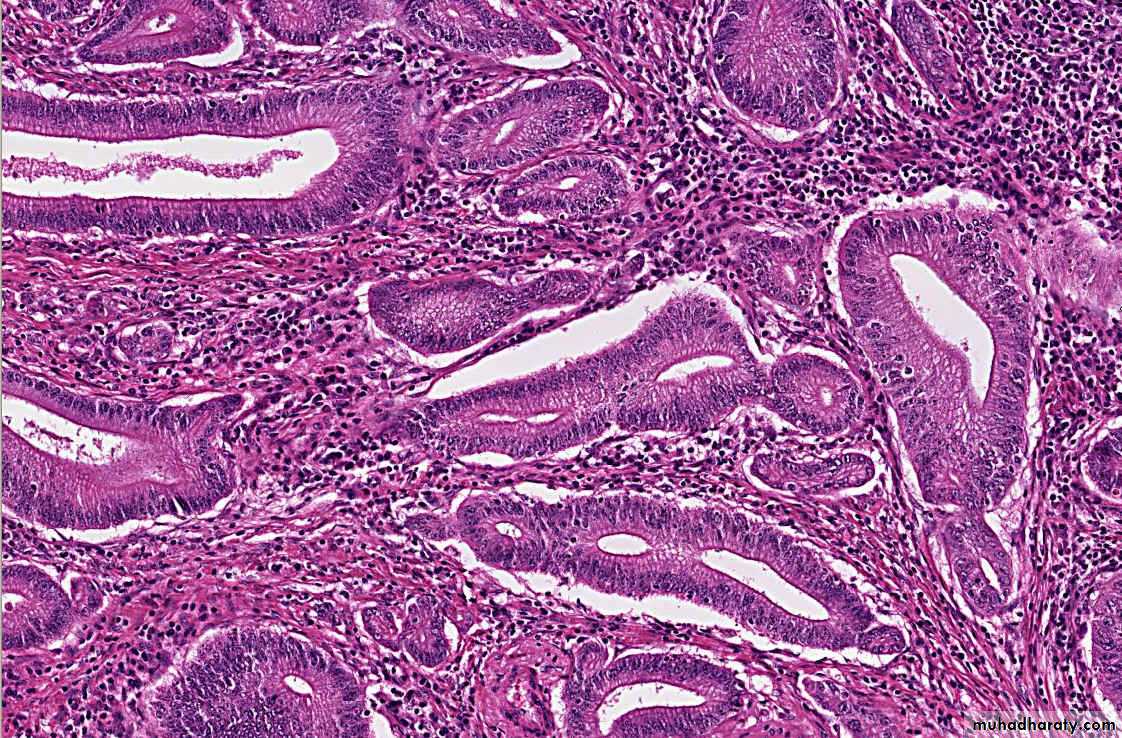
Malignant cells have the ability to emerge themselves between adjacent normal cells and invade the surrounding tissues ( first loose connective tissue).For epithelial tumors the first step should break the basement membrane
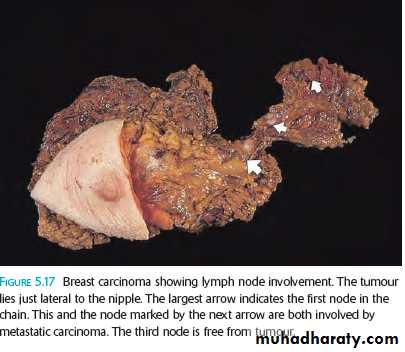
Lymphatic Spread
This is the principal mode by which carcinomas spread.The very thin walls of lymphatics are readily penetrated by tumour cell , which is carried along in the lymph to the first lymph node in the lymph node chain
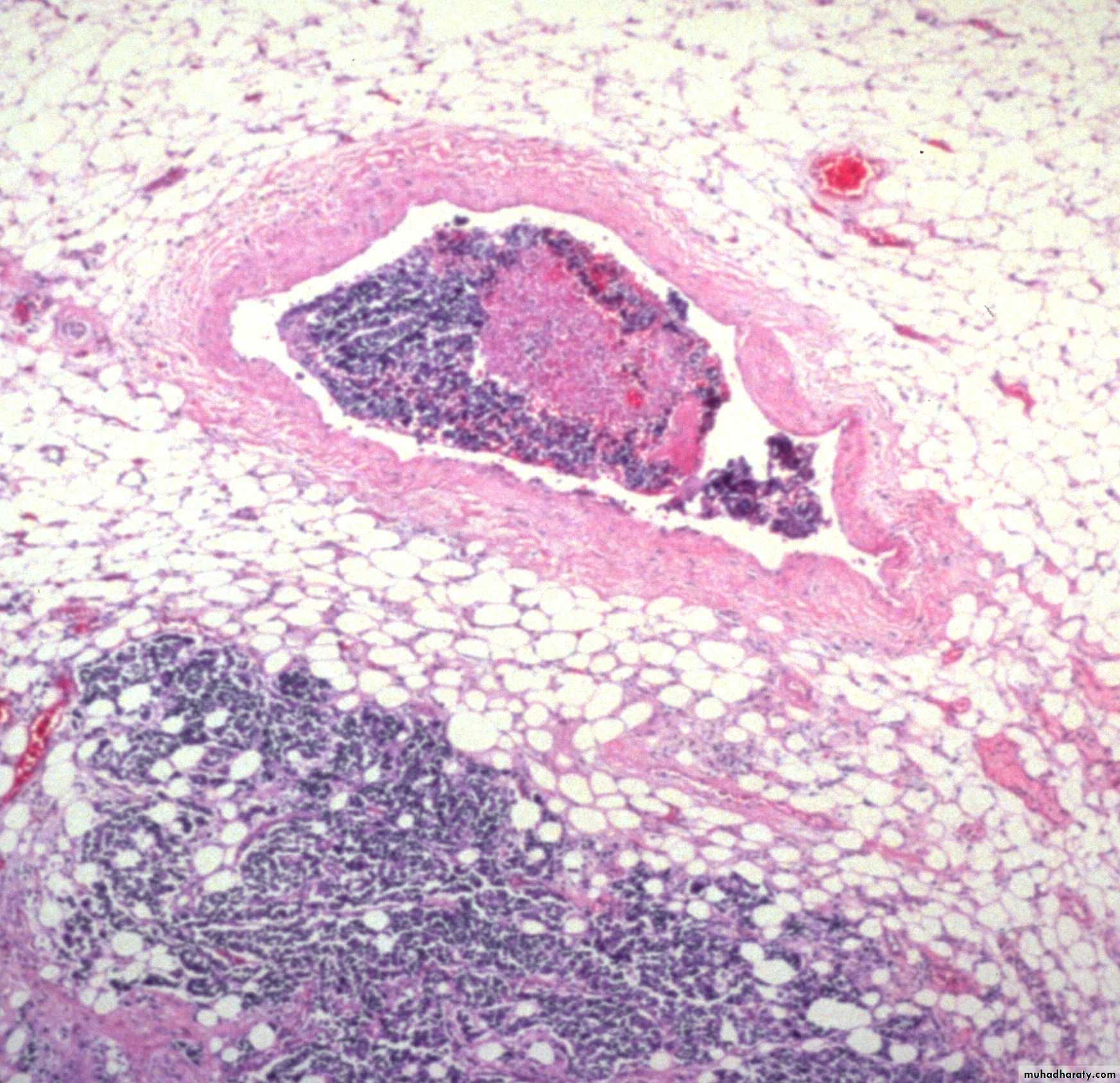
Blood (Haematogenous) Spread
Tumour cells are able to invade thin walled veins and grow along the venous system or embolize into the blood stream.The site of initial metastasis (first-pass organ)
depends on the venous drainage of the location of the
tumour.
Lung , liver and brain are the main organs of hematogenous spread for cancers.
Blood spread is main way for Sarcoma and later for carcinomaTranscoelomic Spread
It means spread across body cavities, the
peritoneal, pleural and pericardial spaces.
e.g: Gastric carcinoma can spread in a similar fashion, to involve the peritoneal cavity, often seeding in the ovaries. known as Krukenberg’s tumours
Intraepithelial Spread
This is the process by which tumour cells can infiltrate between the cells of a normal epithelium, without invading the underlying stroma.It is best seen in Paget’s disease of the nipple in which the cells of ductal carcinoma in situ of breast grow into the nipple skin giving an appearance resembling eczema.
MECHANISMS OF TUMOUR SPREAD
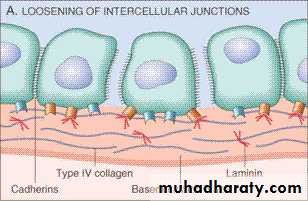
I/ Direct Spread and InvasivenessReduction in Cell: Cell Adhesion
(low production of c-cadherin by malignant cells
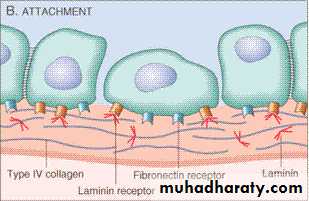
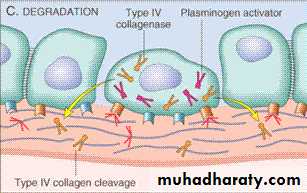
Invasion of Basement Membrane and Stroma
1.cancer cells have altered integrin molecule expression
2. production of proteolytic enzymes by cancer
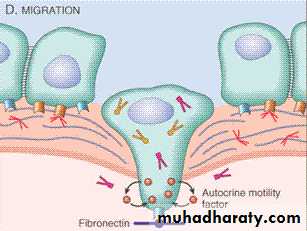
Tumour Cell Motility
The cells extrude pseudopodia at the front and attach to stromal proteins(cytoskeleton)
II/ Angiogenesis
(New blood vessels formation occur normally during tissue healing and chronic inflammation)In recent years they found it is important step in tumor growth and metastasis , which involve:
proteolytic digestion of basement membrane by plasminogen activators and matrix metalloproteinases
migration of endothelial cells, initially as a solid cord
proliferation of endothelial cells● organization of the cords of endothelial cells into new blood vessels with lumens.
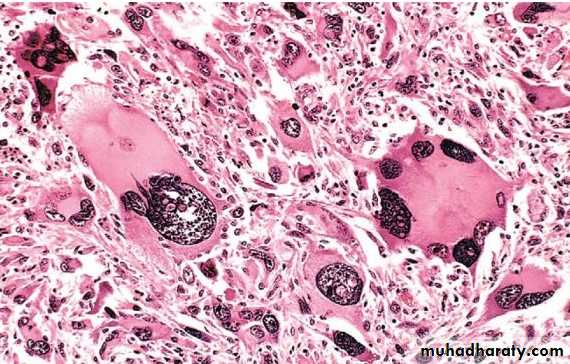
III / vascular Invasion
The thin walls and poorly formed basement membranes of newly formed blood vessels allow the tumor cells to penetrate.
Once tumour cells are free within the lumen of the blood vessel they are carried into the circulation and lodge in a capillary bed.
IV/ Establishment of a New Colony
This involves cell proliferation and the development of a tumour blood supply by stimulation of angiogenesis as previously described.TRANSFORMATIONGROWTHBM INVASIONANGIOGENESISINTRAVASATIONEMBOLIZATIONADHESIONEXTRAVASATIONMETASTATIC GROWTHetc.
PREMALIGNANT CONDITIONS:
Three main groups of lesions can be regarded aspremalignant:
• malignant change in benign tumors :
EXAMPLE/ colonic adenoma , neurofibroma
•
Intraepithelial malignancy/dysplasia ( carcinoma in situ)
The epithelial cells show the cytological features of malignancy but have not yet developed the ability to invade adjacent normal tissues.This process has been known as dysplasia, carcinoma in situ and more recently as ‘intraepithelial neoplasia’.
malignancy developing in chronic inflammation :
chronic damage & repair during chronic inflammation may lead to cancer .Ulcerative colitis colonic cancer
Hashimotos’ thyroiditis lymphomaCirrhosis of liver hepatocellular carcinoma
Clinical Effects of Tumors
Benign tumor
Painless palpable lump (feeling of discomfortEffect of substances produced by tumor cells
e.g/thyroid adenoma leads to hyperthroididism
Pressure effects due to tumor expansion e.g/
pitutatry adenoma may cause hypopitutarisim
Distortion of uterine cavity in leiomyoma
Non –metastatic
Effects Effects of Malignant tumors Metastatic effectsInappropriate secretion of hormones
Direct effectsDirect Effects
Pain due to compress the adjacent structures such as nerves by the mass of malignant tumor .
Haemorrhage from an ulcerated carcinoma may be acute or chronic, thus leading to iron deficiency anaemia
Narrowing (stenosis) or complete obstruction of
a hollow viscusMetastatic Effects
Metastases can cause similar mass effects to primary tumours, but because they are usually multiplethe consequences tend to be more severe
Non-metastatic Effects
Patients with advanced cancer are often wasted (cachectic) with weight loss, anorexia andImmunosuppression
abnormalities of coagulation, for example thrombophlebitis migrans
neurological disorders, for example neuropathy, cerebellar
Degeneration
These effects due to secretion of cytokines like interlukin 1(IL-1) & tumor necrosis TNFα
Inappropriate Hormone Production
Many tumours produce hormones not normally produced by their tissue of origin.Paraneoplastic Syndromes
These occur in about 10% of persons with malignant diseaseThey are related to secretion of hormone or hormone like substances which are produced by certain malignant tumors , they are important for the following resons:
They may represent the earliest manifestation of an occult neoplasm.
In affected patients they may represent significant clinical problems and may even be lethal.
They may mimic metastatic disease
Causal mechanism
Underlying cancerClinical syndromes
• ACTH or ACTH-like substance
Small-cell carcinoma of lung
Cushing SyndromePancreatic carcinoma
Neural tumors
Parathyroid hormone–related protein (PTHRP), TGF-α, TNF, IL-1Squamous cell carcinoma
Hypercalcaemia
Breast cancer
Renal carcinomaAdult T-cell leukemia /lymphoma
Causal mechanismUnderlying carcinoma
Clinical Syndromes
Insulin or insulin-like substance
Ovarian carcinoma
hypoglycaemia
Fibrosarcoma
Other mesenchymal sarcomas
ErythropoietinGastric carcinoma
Renal carcinoma
polycythemiaCerebellar hemangioma
Hepatocellular carcinomaTUMOUR STAGING AND GRADING
Methods are used to asses the aggressiveness of malignant tumors and the spread of themnecessary for prognosis of the malignant tumor and choice the proper treatment
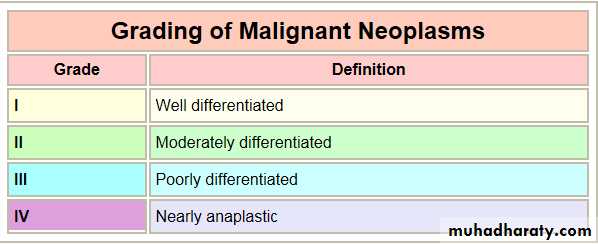
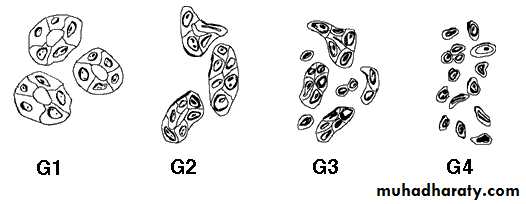
Grading of malignant tumors
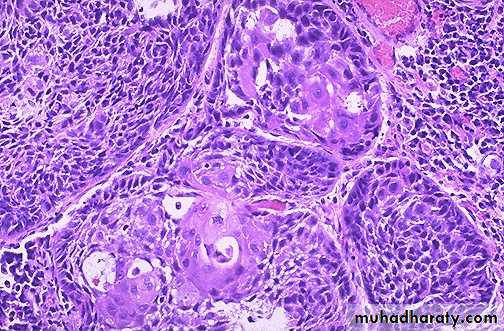
Grading of a cancer is based on the degree of differentiation of the tumor cells & the resemblance of cancer cells to tissue of origin.The main parameters that look for :
mitotic activity
nuclear pleomorphism
degree of differentiation
extent of necrosis
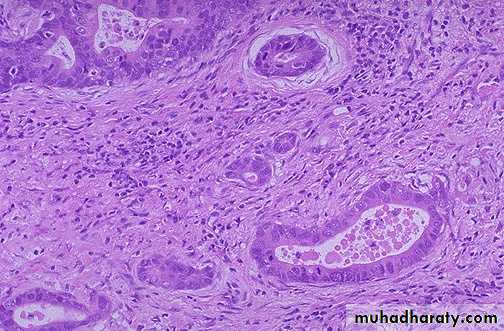
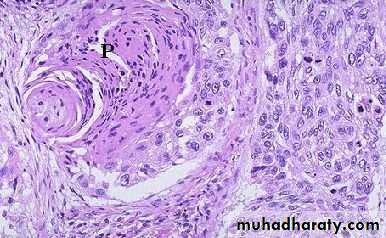
WELL?
(pearls)MODERATE?
(intercellular bridges)
POOR?
(WTF!?!)
GRADING for Squamous Cell Carcinoma
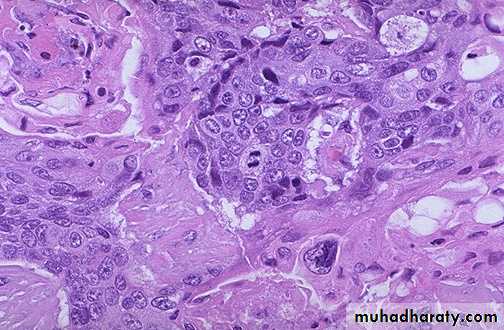
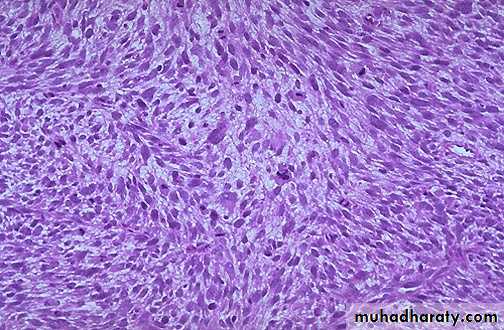
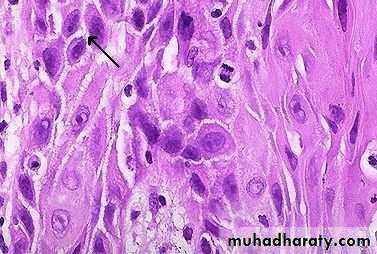
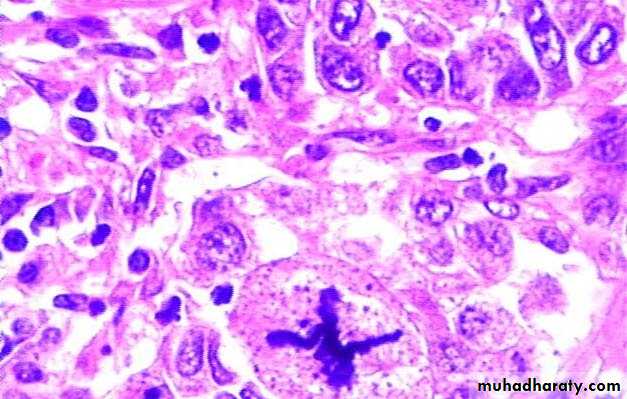
Anaplasia :
lack of differentiation of malignant cells
The features of anaplasia
Pleomorphism : different of size and shape in both cells and nucleus
Abnormal nuclear morphology : the nuclear-to-cytoplasm ratio may approach 1 : 1 instead of the normal 1 : 4 or 1 : 6.
Mitoses : not only increase in the proliferative rate but atypical, bizarre mitotic figures
Tumor Giant cell formation : possessing only a single huge polymorphic nucleus and others having two or more large, hyperchromatic nuclei
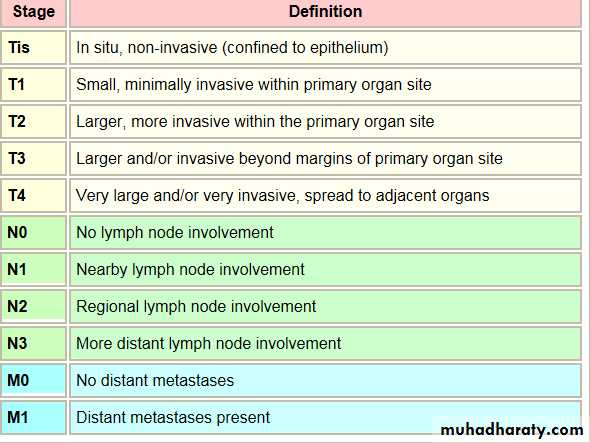
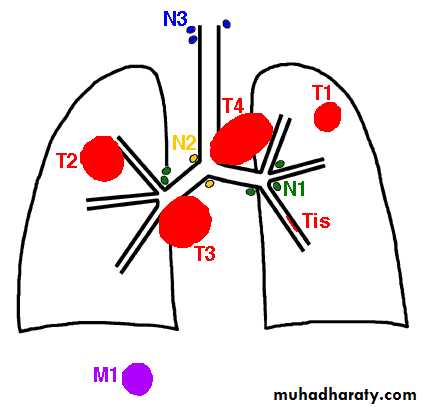
The staging of cancers
is based on the size of the primary lesion, its extent of spread to regional lymph nodes, and the presence or absence of blood-borne metastases.The main staging system have used is TNM staging
T for primary tumor (T1-T4 ) T0 is referred to carcinoma in situ
N for regional lymph node involvement (N1-N3)
M for metastases (M0-M1)
PATHOLOGICAL DIAGNOSIS OF TUMORS
Although clinical, radiological and biochemical findings all contribute towards the diagnosis of a tumour,the final diagnosis is made in almost all cases by microscopic examination
Biopsies for Histopathological Assessment
For large tumor , wedge sections will be removed & examined microscopicallydeep-seated ones under radiological control, can be sampled by needle biopsy in which a thin core of tissue is removed
Examination of individual tumor cells in body fluid or by using needle aspiration (breast lump ,thyroid)
Additional techniques :
Some of tumors are undifferentiated and very difficult to reach the diagnosis by H&E stainSo we need additional techniques to reach final diagnosis and give the proper treatment.
Electron microscope
Immunohistochemical stains : special technique which is depended on antigen –antibody reaction .(using antibodies to cell constituents)
In-situ hybridization have been used to detect gene expression as a way of determining tumor type
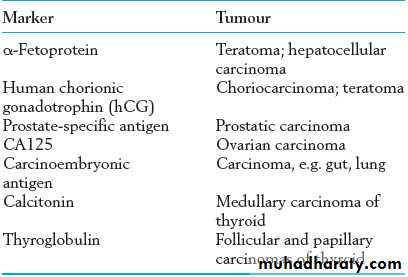
Tumor Markers
These substances are produced by tumor cells, are
detectable in the blood, and are of value in diagnosis and in monitoring progress following treatment.Causes of Neoplasia
The origin for many neoplasms is obscure. However, there are several theories of origin:Causes of Neoplasia : cont.
Also they are found the incidence of cancers are increased in older personsracial predilections (American women have breast cancer more often than Japanese women; Japanese men have stomach cancer far more often than American men).
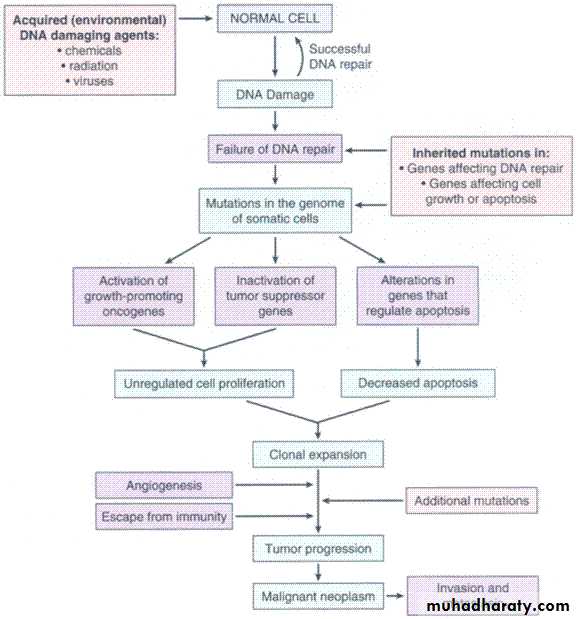
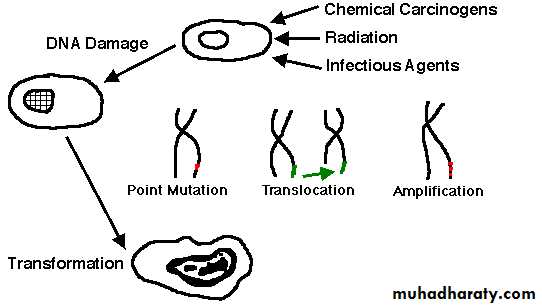
Carcinogenesis is a multistep process :
InitiatorsInitiation that lead to irreversible DNA damage(lethal damage)
Example : Alkylating agent like cycophosphamide
Promotors
Lead to proliferation of abnormal (mutagenic cells) but they there appears to be a "dose-threshold" concentration of promoter below which neoplasia will not occur
like hormone therapy estrogen(diethylstilbesterol)
MOLECULAR BASISof CANCER
Four classes of normal regulatory genesPROTO-oncogenes ((gene responsible for cell growth)
Tumor suppressor genes
DNA repair genes
Apoptosis genes
Defect (over expression) in proto-oncogene (growth factors) leads to uncontrolled cell proliferations )
e.g / RAS overexpression in many human cancer
Loss of tumor supprresor genes (P53)
Limitation of apoptotic genes (BCL2)Defects in DNA repair genes
TRANSFORMATION &PROGRESSIONSelf-sufficiency in growth signals
Insensitivity to growth-inhibiting signals
Evasion of apoptosis
Defects in DNA repair: “Spell checker”
Limitless replicative potential: Telomerase
Angiogenesis
Invasive ability
Metastatic ability
HOST DEFENSES
IMMUNE SURVEILLENCE CONCEPTCD8+ T-Cells
NK cells
MACROPHAGES
ANTIBODIES
How do tumor cellsescape immune surveillance?
Mutation, like microbes↓ MHC molecules on tumor cell surface
Immunosuppressive agents
Antigen maskingApoptosis of cytotoxic T-Cells (CD8), i.e., the tumor cell KILLS the T-cell!