1
Dr.Amina Zakaria Al-tutunji
M.B.Ch.B, MD.
Obstetrics and Gynecology
College of medicine/ University of Mosul
2016-2017
Lec7
Childhood gynecological disorders
A. Normal findings in pediatric patient
-A mucoid vaginal discharge
-A introitus that is located more anteriorly than normal & a clitoris that is more prominent than normal
-A vaginal epithelium that is erythematous with an alkaline pH
-A small uterus (2.5-3 cm) in length
-A redundant hymen that may protrude on standing & that remains the same size until 10y of age.
B. Normal findings in an adolescent patient
-Intact hymen in those not sexually active
-Postpubertal gynecologic examination in an adolescent is similar to an adult female .
Vulvovaginal leasions
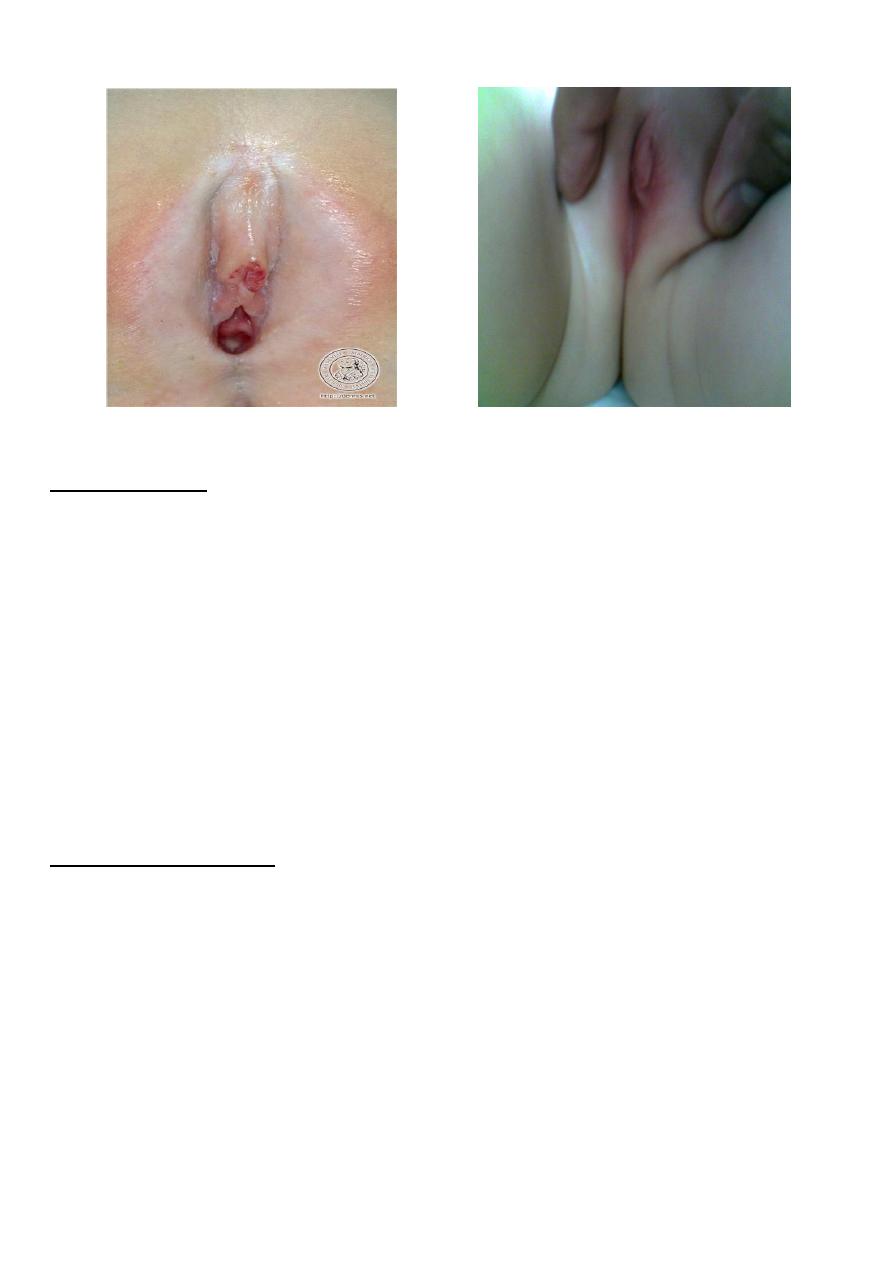
A. Lichen sclerosus atrophicus
Clinical picture: vulvar itching, A white, papular lesion resembling leukoplakia may cover the vulva and
perianal regions .
Etiology: Causes are unknown .
Diagnosis: Biopsy
Management:This condition is benign and can be self-limiting. Improved hygiene is the first line of
therapy.See fig.1
B.Trauma
Clinical picture: tears, abrasions, ecchymoses & hematomas are common in preadolescent girls. The
incidence is highest in children between 4 and 12 years of age .
The most common mechanism of injury are sexual abuse,straddle injuries, accidental penetration, sudden
abduction of the extremities & pelvic fractures .
Management: A vaginoscope is used to visualize the vagina to locate sources of bleeding . A large vaginal
laceration may result in an expanding hematoma in the retroperitoneal space. Superficial abrasions and
lacerations of the vulva, if not actively bleeding , can be cleaned and left alone. antibiotic therapy is advised
as prophylaxis.
C. Labial agglutination
Clinical picture: Adhesion of the labia minora in the midline is the usual presentation. This vertical line of
fusion distinguishes labial agglutination from imperforated hymen or vaginal atresia. The agglutination
encourages retention of urine & vaginal secretions & can lead to vulvovaginitis or urinary tract infection.
Management: If a symptomatic, improved hygiene may be all that is necessary.Treatment is indicated if there
is a chronic vulvovaginitis or difficulty urinating, Lubrication of the labia with a bland ointment,Topical
estrogen & Surgical separation is rarely necessary. See fig.2
2
Fig.1 lichen sclerosis
Fig.2 labial agglutination
D.Vaginal Discharge
Clinical Picture: A mucoid discharge is common in infants for up 2 weeks after birth; it result from maternal
estrogen. It is also a common finding in prepubertal girls, who experience increased estrogen production by
maturing ovaries.
Pathologic discharge may result from any of the following conditions:
-Infections with organisms, such as E.coli, Proteus, Pseudomonas.
-Hemolytic streptococcal vaginitis.
-Monial vaginitis.
-Foreign body.
Managment: Conservative management is advisable, as follows:
-Culture to identify causative organisms.
-Urine analysis to rule out cystitis.
-Proper hygiene.
-Perianal examination with transparent tape to test for pinworms.
In cases of persistent discharge, examination under anesthesia is indicated to rule out foreign body.
E.Vaginal bleeding in infancy:
Female infant may have vaginal bleeding during the 1st week of life. Mainly due to withdrawal of maternally
derived estrogens which had crossed the placenta in pregnancy.
Causes of Vaginal Bleeding in Children:
-Foreign body.
-Trauma.
-Genital tumors.
-Urethral prolapse.
-Vulvovaginitis.
-Condyloma acuminata.
-Precocious puberty.
-Exogenous hormone usage.
3
Special problems of the adolescent
1-menstrual problem.
2-primary dysmenorrhoea.
3-primary amenorrhoea.
3-Hairsutism.
Menstrual problem in adolescence are very common as normal ovulatory cycles can take many years before
established & may manifest themselves in a number of ways due to immaturity of
hypothamo-pitutary-ovarian axis. in 75% of cases is an immature hypothalamic–pitutary axis resulting in
anovulation .
It takes 2-3 years from the time of menarche for women to develop ovulatory cycles.This phenomenon is
extremely important for the gynaecologist to understand, as the management of these cases is usually without
active treatment but by support & understanding of the condition.
1.Menstrual disturbance
can be either:
a. Heavy menstruation:
The periods may be very heavy & occasionally result in marked anaemia.
**if patient not anaemic it is unnecessary to offer any treatment other than explanation & reassurance &
follow up at 6 months intervals until the pattern of menstruation is established.
**If patients does become anaemic then explanation is required & some control of menstrual loss must be
undertaken & can be achieved by either cyclical progestogens for 21 days in every 28 days or COCP. These
therapies should be stopped on an annual (yearly) basis to assess the establishment of normal pattern of
menstruation thereafter no need for medications.
**Any girl who continues to have menorrhagia uncontrolled by these treatment should have:
-Transabdominal pelvic USG.
- Investigations for blood dyscarisia.
There is no real place for curettage & it should be avoided.
b.Very scanty and infrequent period:
Investigations may be required by assessing levels of gonadotrophins & by USG of the ovary. in some
circumstance, diagnosis of PCOS may be made & may need OCP to control cycle.
2.Primary dysmenorrhoea
:
Is defined as cramp-like pain in the lower abdomen associated with menstrual flow.
Etiology;Primary dysmenorrhea accounts for most cases & is attributed to increased prostaglandin production
with menses in the presence of normal anatomy .
Clinical picture: Sever, cyclic, cramp-like pain located in the lower abdomen & pelvis is associated with
menses. Pain may radiate to the thighs & back & be accompanied by nausea , vomiting & diarrhea.
Managment;
First-line therapy is prostaglandin inhibitors [NSAIDs]
If the symptoms are not adequately, start oral contraceptives or obtain a pelvic U/S to evaluate for abnormal
anatomy depending on the loction, progression & severity of symptoms.
Laparoscopy is recommended if medical treatment fails to control the symptoms .
*Secondary dysmenorrhea results from pathological conditions such as endometriosis & anomalies with
obstruction in a portion of the outflow tract which leads to pain. Examples uterus didelphys with obstructed
hemivagina.
