I
Fifth stage
ENT
Lec-2
د.سنمار
15/11/2016
Epistaxis (nosebleed)
Although epistaxis (haemorrhage from the nose) is usually harmless, it may be life-
threatening disease. It affects all ages without sex predilection. Anterior epistaxis is more
common in child or young adult, while posterior nasal bleeding is more often seen in the
older adult with hypertension or arteriosclerosis. The incidence is higher during the winter
months when upper respiratory tract infections are more frequent.
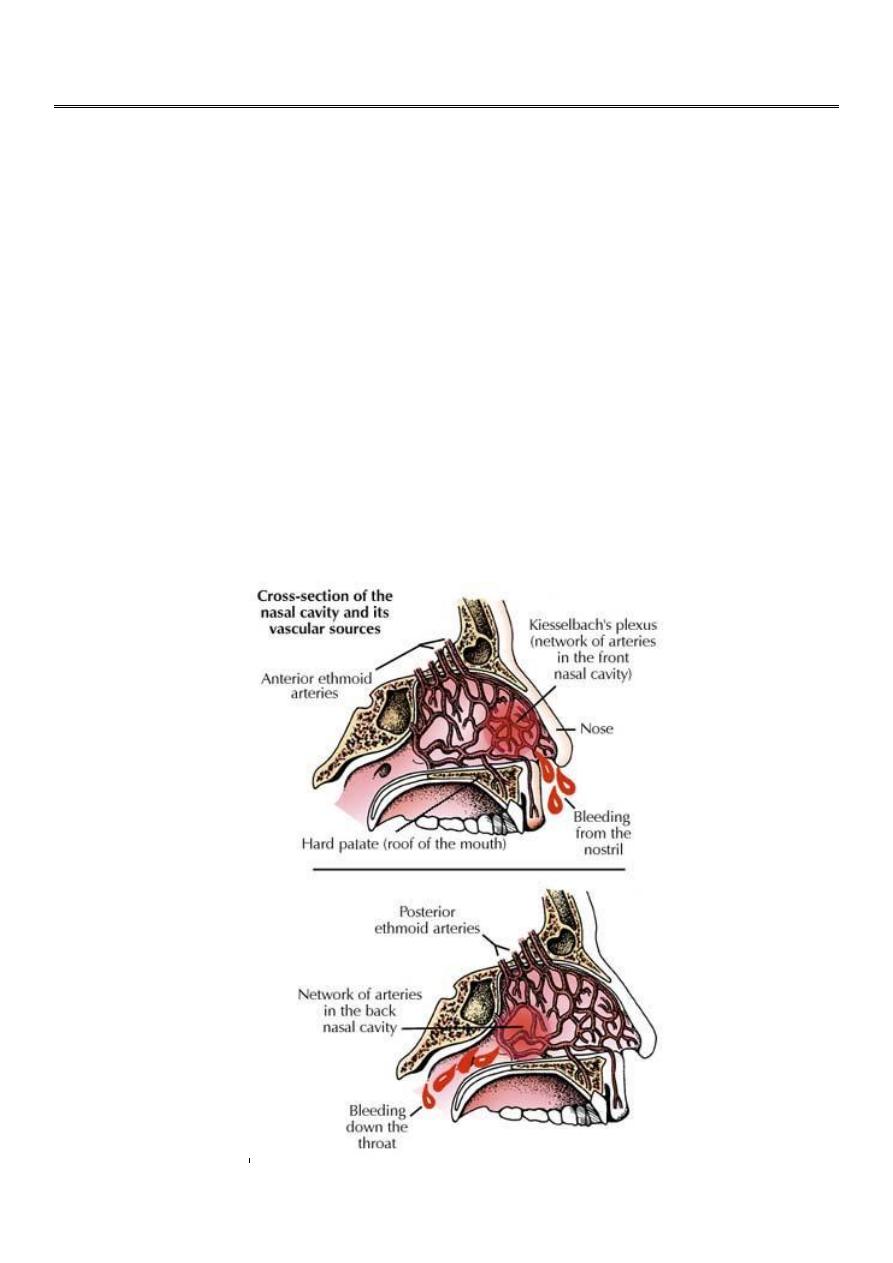
Sources of bleeding;
Bleeding from Kiesselbach`s plexus (Little area) forms about 90 % of cases. The mucosa in
this area is very fragile and is tightly adherent to the underlying cartilage and thus offers
little resistance to mechanical stress.
.
Sources of bleeding
II
Causes of epistaxis;
A. Local causes;
1) Idiopathic.
2) Trauma: Direct injury as nose picking, or nasal operations.
The two most common causes of recurrent epistaxis are idiopathy and trauma.
3) Inflammatory reactions
Local inflammatory reaction as a result of acute respiratory tract infection , allergic
disorders or sinusitis allow overgrowth of virulent bacteria and lead to dryness, crusting
,exposure and haemorrhage.
4) Anatomical and structural abnormalities
Septal deviation leads to abnormalities in airflow, causing certain areas of the mucosa to
be exposed to constant turbulent air currents, and causing the vessels to rupture with the
slightest traumatic insult such as rubbing.
5) Intranasal tumours, benign or malignant
These are rare causes of epistaxis but should not be forgotten (Unilateral obstruction with
haemorrhage in elderly patient may rise the suspicion of malignancy).
B. Systemic causes
1) Cardiovascular
Arteriosclerosis associated with hypertension is a common problem, particularly in the
elderly .The nasal mucosa is often atrophic and cracks easily. This eventually leads to
exposure of an elderly arteriosclerotic vessel, which can easily rupture during a hypertensive
episode, producing severe haemorrhage. Hypertension does not cause the epistaxis but
ensures continued haemorrhage once it starts.
III
2) Drugs: e.g.; warfarin, heparin, NSAIDs, methotrexate, alcohol, dipyridamole…etc.
3) Blood disorders
Leukemia, multiple myeloma, haemophilia and idiopathic thrombocytopenic purpura
(ITP) can lead to severe and persistent nosebleed.
4) Toxic agents: e.g. Heavy metals such as chromium, mercury and phosphorus.
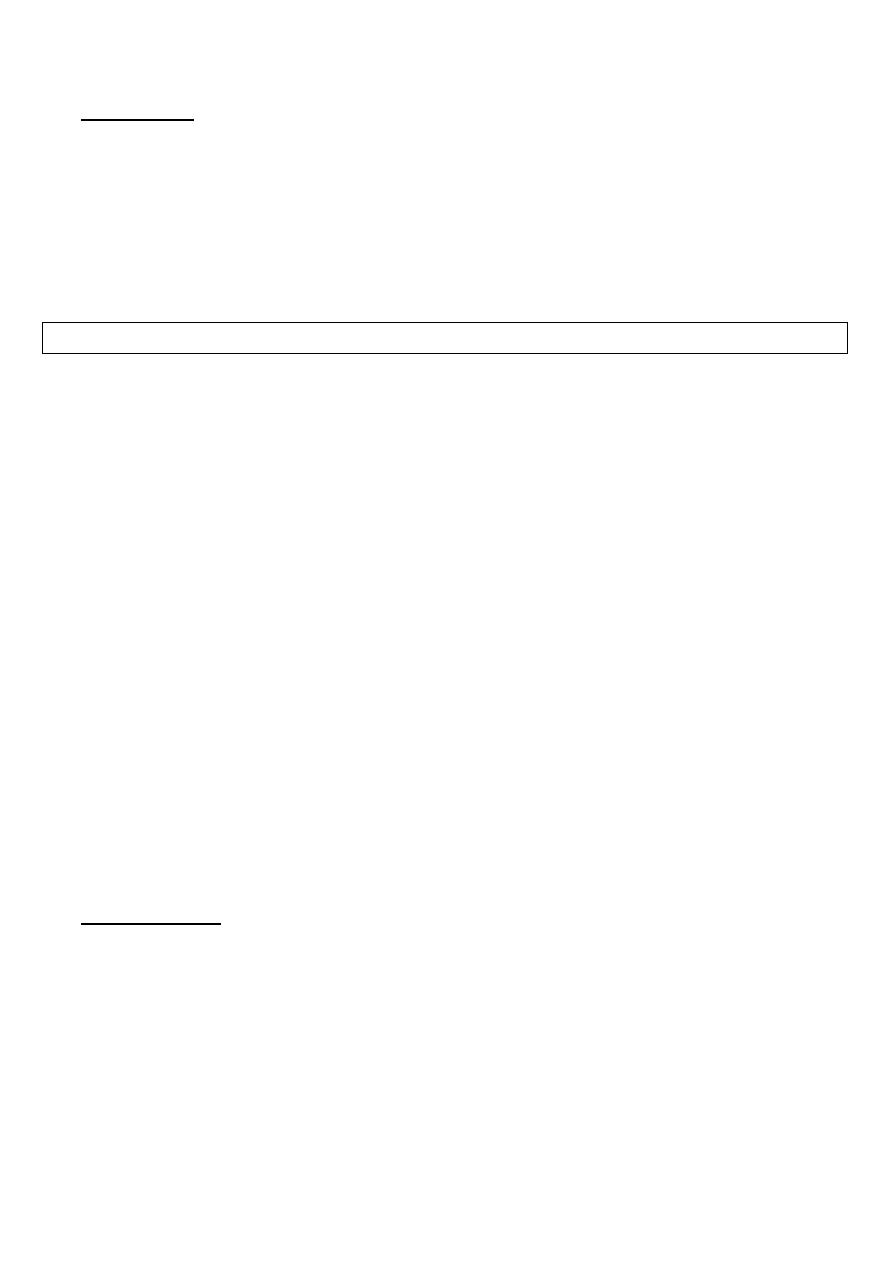
Osler-Weber-Rendu disease
5) Hereditary haemorrhagic
telangiectasia
This disease is also known as Osler-Weber-
Rendu disease and characterized by
abnormal capillaries, is a potent but
uncommon cause of recurrent epistaxis.
The disease can also cause haematuria,
melaena and cerebral haemorrhage.
Management;
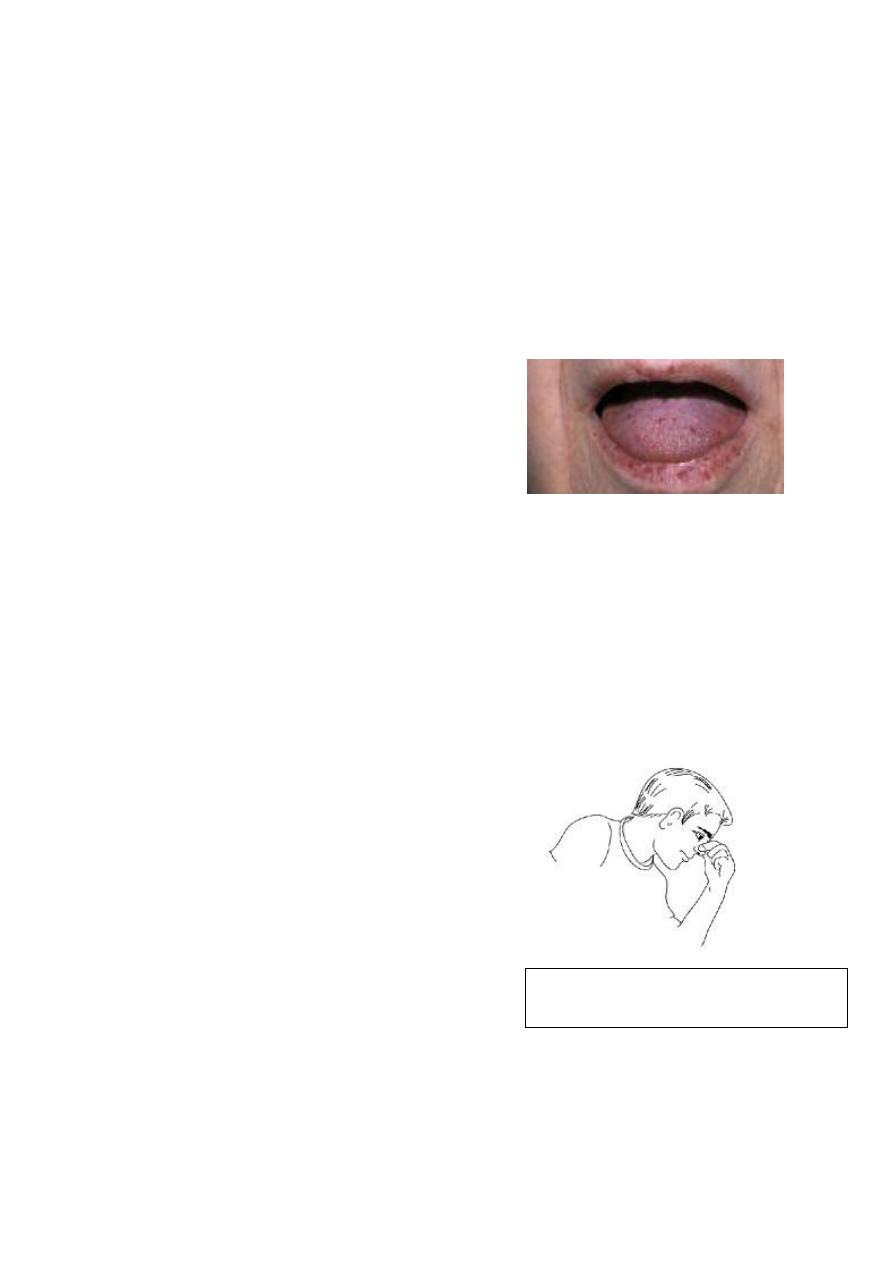
A. First aid management;
1. Arrest of haemorrhage;
Sit upright, lean forward and pinch
the nostrils.
Calming the patient (if necessary
with medication).
The nostrils should be pinched
together (compressing the bony
bridge is useless).
The patient should sit upright to
lower to blood pressure and lean
forward slightly over a container
so as not to swallow blood.
2. Assessment of blood loss;
Recording the pulse and blood pressure.
Look for signs of shock; pallor, raising pulse and sweating.
In severe blood loss;
IV
IV line should be inserted.
Blood taken for cross match.
Administration of suitable plasma expander.
3. Determination of cause;
A. History; trauma (surgical or non surgical), bleeding tendency (Haemophilia,
hereditary haemorrhagic telangiectasia, ITP ...etc), liver disease, renal disease
and use of anticoagulant.
B. Hb, full blood count and clotting screen should be requested in all cases of
severe nosebleed.
4. Determination of site;
This requires removal of clots by suction or by asking the patient to blow his nose
gently. A cotton-wool pledglet soaked in vasoconstrictor (e.g. 1:1000 adrenaline) is very
useful technique. A search is then made in the clean dry nose for the responsible vessel.
B. Control of bleeding;
o Most nosebleeds stop spontaneously or after the simple measures mentioned above.
o If an active bleeding site is identified then cauterization (electrical or chemical-by silver
nitrate or trichloracetic acid) under local anaesthesia is required. Sometimes posterior
bleed is visualized by rigid endoscope and also controlled by cautery.
o
Cauterization
o If these measures fail, when the blood vessel cannot be seen or cauterized, then
physical pressure on the blood vessel is necessary to occlude it. This is achieved by
V
packing and clotting mechanism will occlude the blood vessel while the pack in place.
The pack requires to remain in situ for at least 48 hours to allow reasonable clotting.
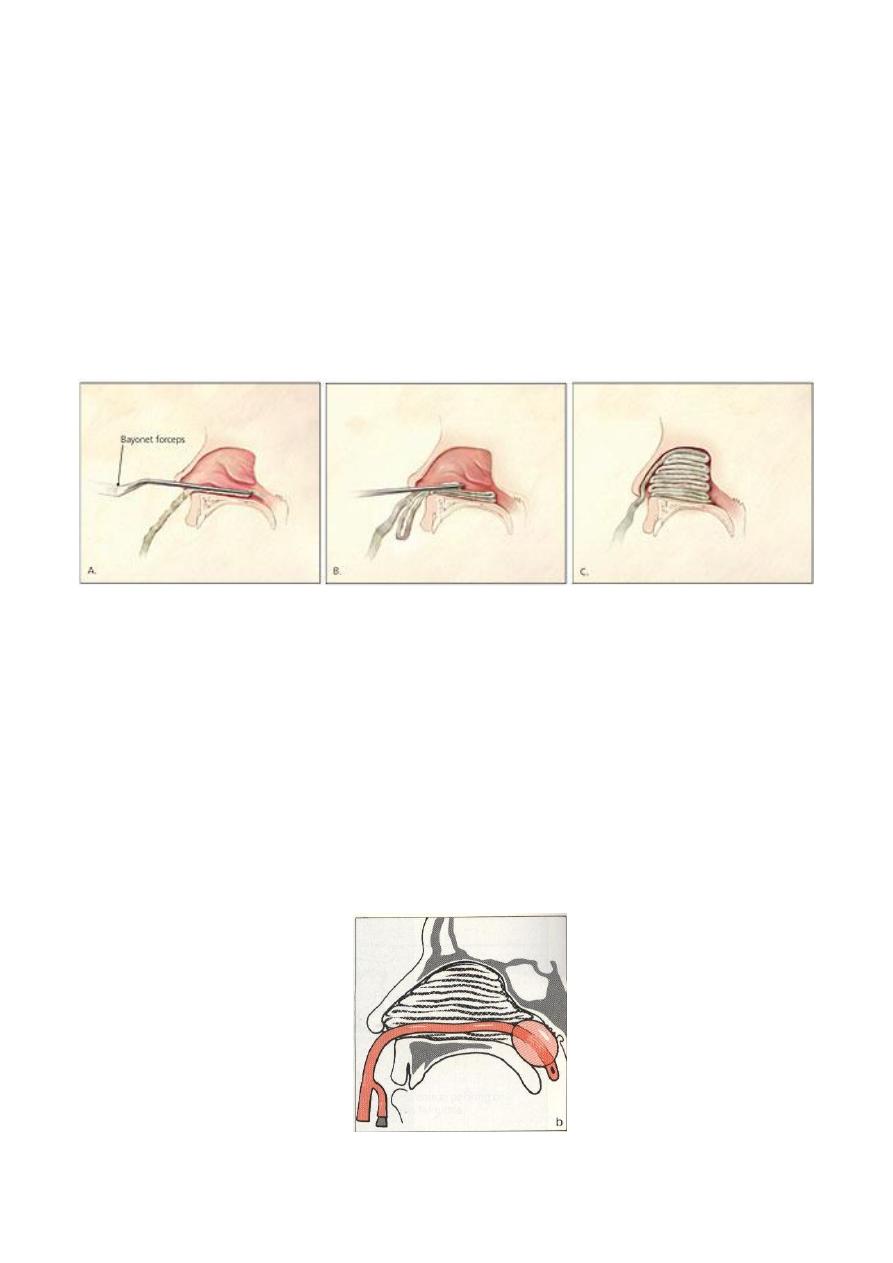
In anterior packing the best pack used is made up of a 0.5 in (1.25cm) is soaked in a
mixture of bismuth iodoform paraffin paste (BIPP). This substance is antiseptic and can
be left in the nose for a considerable time. It is important that the packing should be
built up in layers, starting on the flour of the nose and going as far back as possible,
then gradually building up toward the roof. Vaseline gauze and commercially produced
sponge` tampons` are alternatively used. Prophylactic antibiotics are important to
manage sinusitis from blockage of sinus ostea and to prevent toxic shock syndrome
secondary to toxin producing staphylococcus aureus.
Method of anterior packing
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
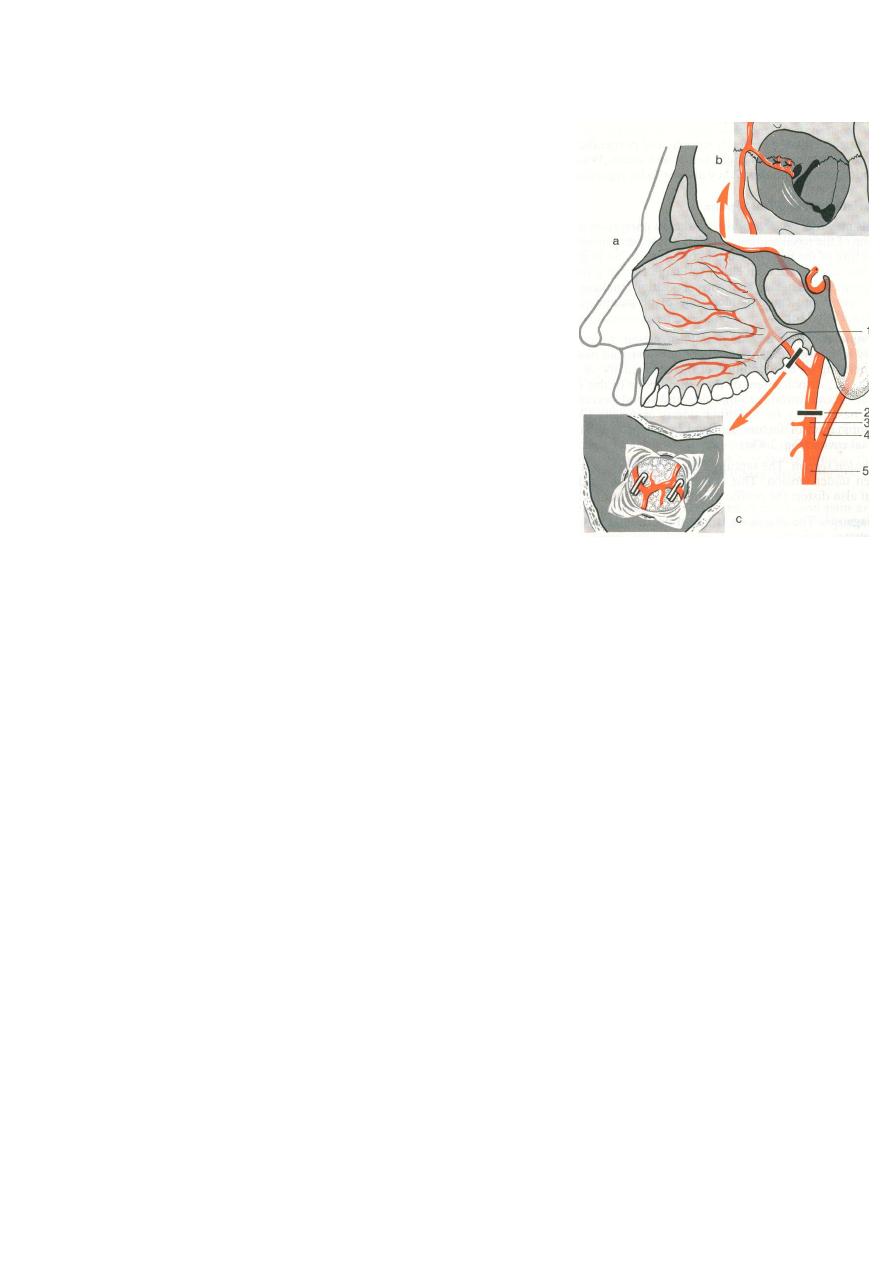
Continued haemorrhage despite anterior pack is probably a result of bleeding from the
posterior branches of sphenopalatine artery and will necessitate the insertion of a postnasal
pack. A simple post nasal pack is a Foley catheter which is inflated once correctly positioned.
This can be performed without general anaesthesia. The post nasal pack must be associated
with anterior pack.
o
o
o
o
o
o
o
o
o
o
o
o
o
Postnasal pack by Foley's catheter
o
o
o
o
o
o
VI
If bleeding continues despite anterior and posterior packing, then we have to go through
the following steps;
1. Examination under general anaesthesia. Any
septal deviation which might hide bleeding
points or prevent adequate packing is dealt
with. Nasal endoscopy may help to locate the
offending blood vessel. If, despite a thorough
search, no obvious bleeding site can be found,
a more thorough packing of anterior and
posterior nasal fossae should then be
performed.
2. If, despite anterior and posterior packing under
general anaesthesia the bleeding continue or
recurs, surgical ligation of the arterial supply of
the nose may be necessary. Three main surgical
procedures are described ;
1) Anterior ethmoidal artery ligation.
2) Maxillary artery ligation.
3) External carotid artery ligation.
Arterial ligation
Nasal Fractures
Usually caused by a blunt trauma to the nose and occasionally by penetrating wounds.
This
can occur in isolation or in combination with fractures of the maxilla or zygomatic arch.
We should not forget that the patient may also have received a head injury.
Clinical Picture
1. Deformity, black eye and swelling.
2. Pain and headache.
3. Epistaxis.
4. Nasal obstruction due to septal haematoma or septal dislocation.
5. Crepitus and nasal mobility.
Remember to inquire regarding preexisting deformity.
Investigations
X.ray is important medicolegally but of little value clinically.
Treatment
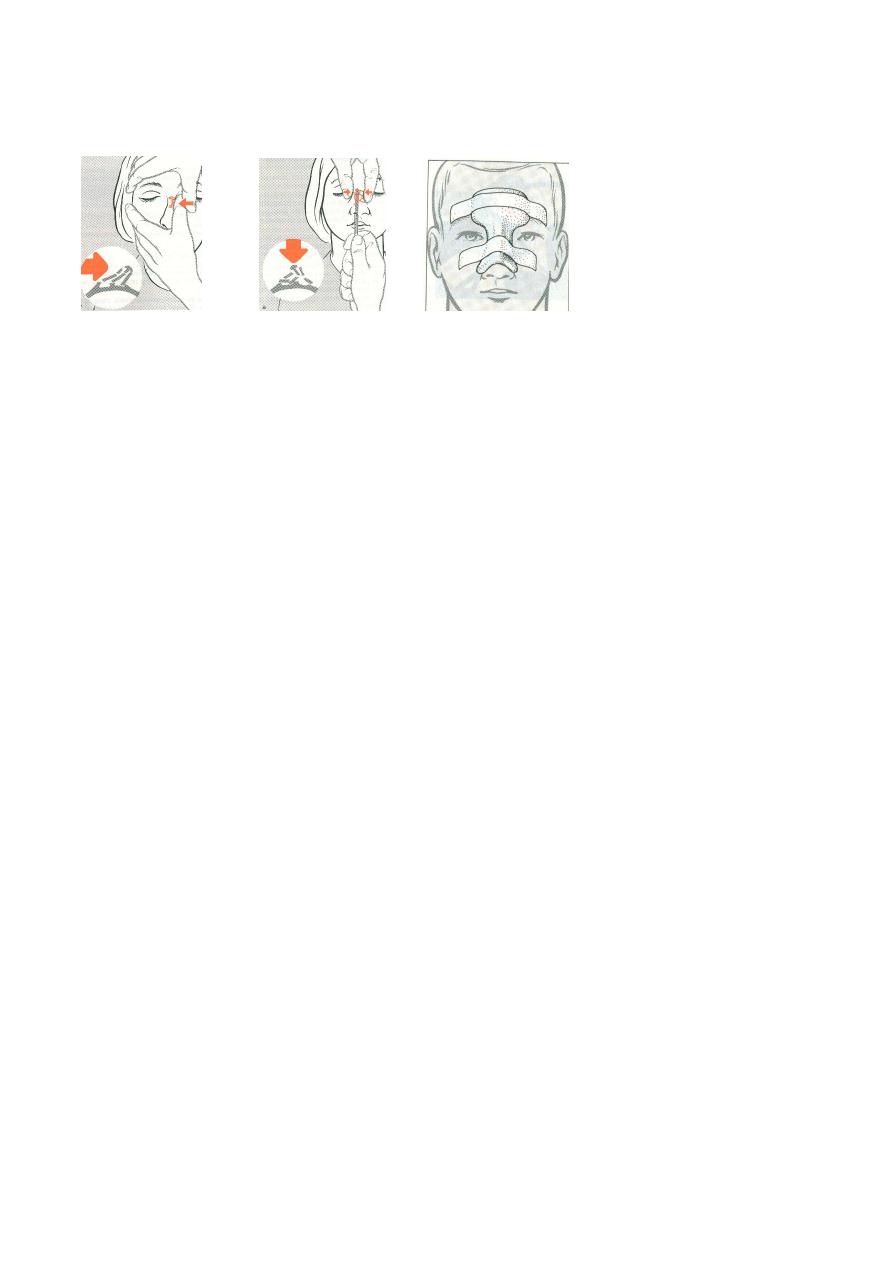
Early (hours): Before swelling appear----- immediate reduction (Open fracture or
septal haematoma requires immediate treatment.).
VII
Intermediate (Days): When oedema obscures the deformity -----Wait 5-6 days till the
swelling subside.
Late ( months or years): Septorhinoplasty for persistent deformity
Reduction of fracture and dorsal splint
A protective dorsal splint is placed for about 7 days. Intranasal packing is used to
prevent depression of unstable bone fragments. Treatment becomes more difficult
after 10-14 days in adult and 7-10 days in children, as the bones begin to set.
Foreign bodies in the Nose
They are much more common in children. The F.B. may be organic or inorganic. An
inflammatory reaction follows accompanied by nasal discharge.
Clinical Picture
1. Unilateral foul smelling nasal discharge. In a child, unilateral purulent discharge is
pathognomonic of foreign body.
2. Epistaxis.
3. Pain.
.
Investigations
X – ray if the foreign body is radiopaque.
Treatment
Removal of the FB by a probe, hook or forceps, sometimes G.A. is required.
Rhinolith
Hard masses in the nasal cavity consist of deposits of phosphate, and carbonate of
calcium and magnesium around a central nucleus called the nidus.
Aetiology
The nidus may be
1. F.B.
VIII
2. Dried blood and pus.
Clinical Picture
1. Unilateral offensive nasal discharge.
2. Unilateral nasal obstruction.
3. If it is long standing, it leads to atrophy of the nasal mucosa.
Examination; Probe --- hard mass can be felt.
Investigations; X - ray
Treatment; Removal under G.A.
Disorders of nasal septum
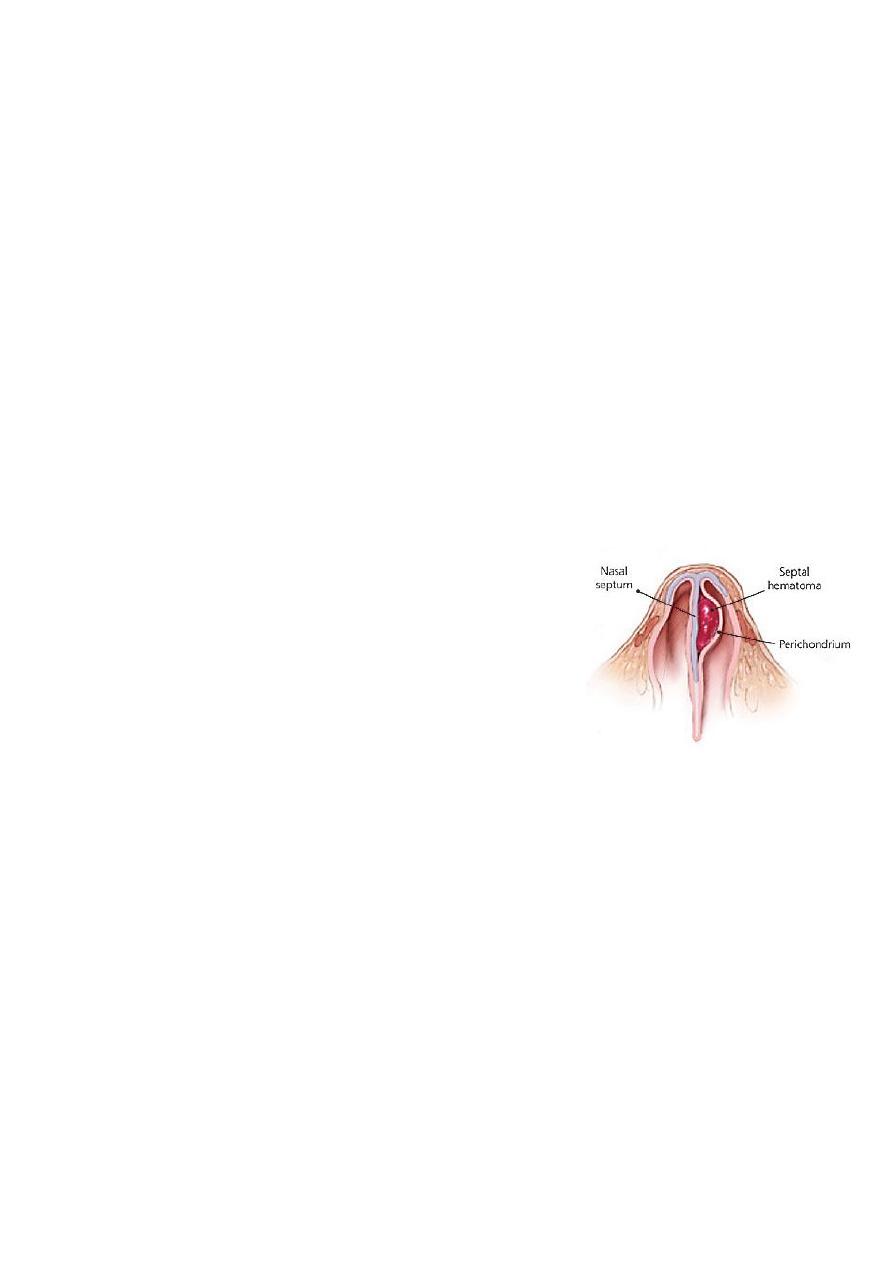
1. Septal haematoma:
Collection of blood beneath the mucoperichondrium or
mucoperiosteum of the nasal septum.
Therefore
haematoma. separate the cartilage from its blood supply
may cause cartilaginous atrophy and necrosis.
Aetiology
1.
Trauma to the nose. 2. Septal surgery. 3. Blood dyscrasia.
Clinical Picture
1. Nasal obstruction 2. Septal swelling.
Complications
1. Infection of the haematoma with septal abscess ,cartilage necrosis and perforation.
2. External deformity (Saddle-nose)

IX
Treatment; The haematoma must be incised and drained followed by application of a pack
in the nasal cavity with antibiotic cover.
2. Septal Abscess:
Is collection of pus beneath the mucoperichondrium or the mucoperiostium.
Aetiology
1. Complication of haematoma. Blood provide excellent bacterial medium and result in
septal abscess
2. May follow furunculosis, measles or scarlet fever.
Clinical Picture
Nasal obstruction, fever, pain and tenderness over the nasal bridge.
Examination
Symmetrical swelling of the nasal septum.
Complications
1. Cartilage necrosis leading to perforation and external deformity.
2. Cavernous sinus thrombophlebitis.
Treatment
1. Drainage+packing+antibiotics.
2. Plastic surgery for external nasal deformities.
3. Septal deviation:
Generally a few adults have a complete straight septum. Only gross deflections causing
symptoms require treatment.
Aetiology
1- Trauma: Either birth trauma or external injury.
X
2- Developmental errors: The developing septum buckles because it grows faster than its
surrounding skeletal framework.
Symptoms
1- Nasal obstruction which may be unilateral or bilateral.
2- Recurrent sinus infection due to interference with sinus ventilation and drainage.
3- Headache due to malventilation of the frontal sinus (vacuum headache).
4- Epistaxis result from a prominent vessel over a bony spur.
Examination
1. External nasal deformity.
2. The deviation may be S or C shaped.
3. Signs of sinus infection.
Treatment;
1- Mild no Rx.
2- Symptomatic:
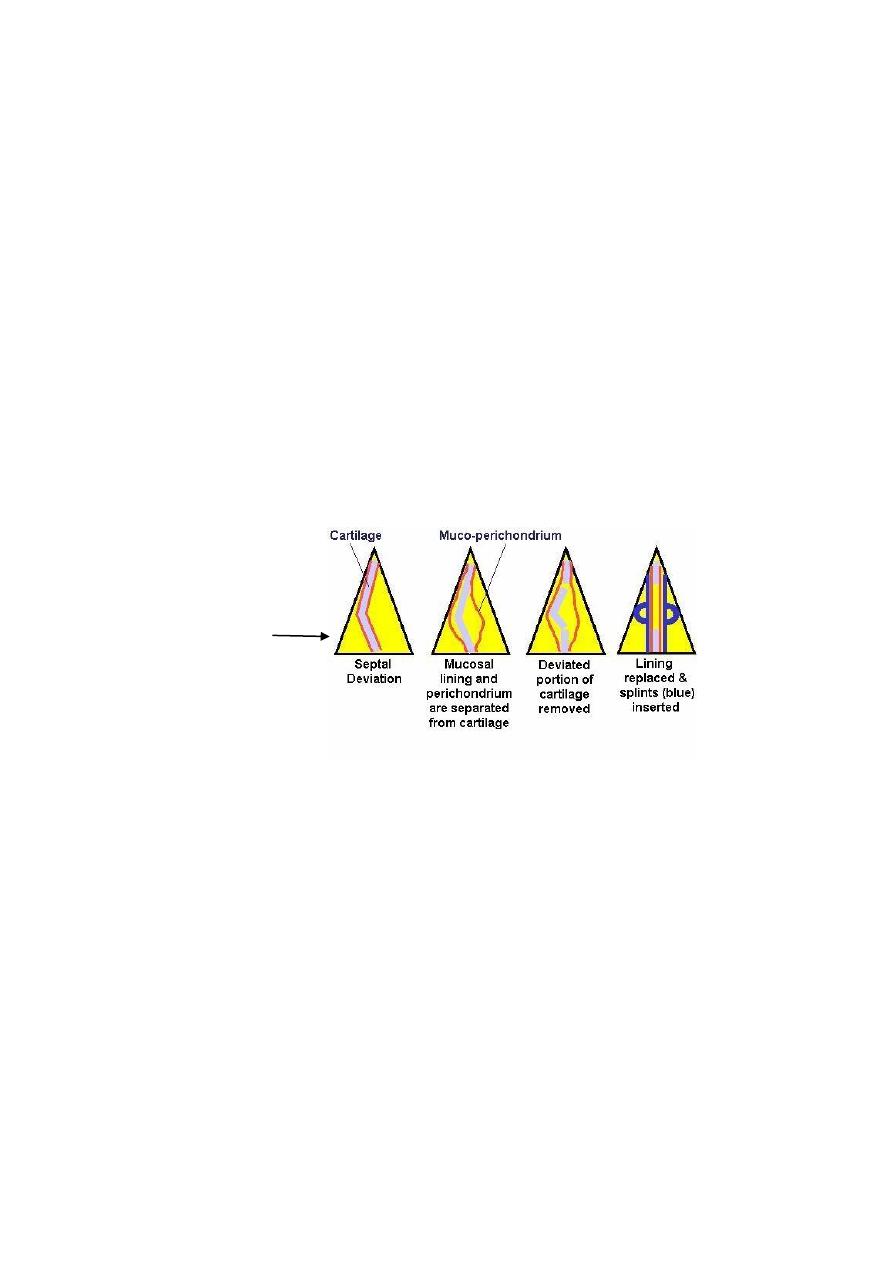
a) Submucous resection SMR
b) Septoplasty: i.e.;
4. Ulceration and perforation of the septum:
Aetiology;
1) Trauma; surgical, repeated cautery, digital trauma(nose picking)
2) Malignant disease.
3) Chronic inflammation; TB, syphilis
4) Poisons; industrial, cocaine addicts, topical corticosteroid, topical decongestants.
5) Idiopathic.
If small the perforation may produce an irritating whistling noise with respiration and if
larger it produces a considerable crusting with subsequent bleeding.
Treatment;
1. Treat the cause.
2. Medical: alkaline nasal douche + 25% glucose in glycerine.
3. Surgical closure but with poor success rate.
Repositioning of the
deviated cartilage with
minimal resection
XI
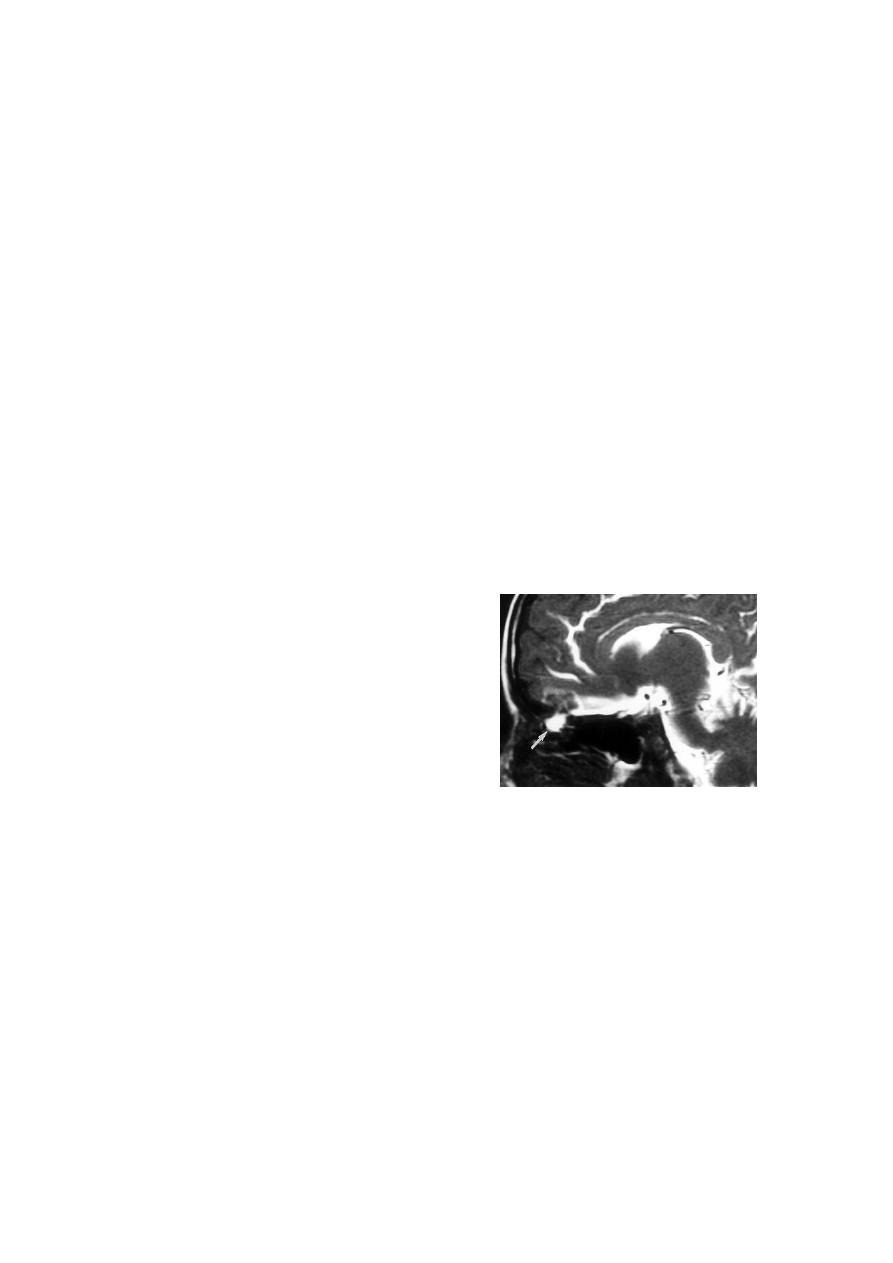
Cerebrospinal fluid (CSF) Rhinorrhoea
Aetiology
1- Trauma: fracture of the base of the skull e.g. the cribriform plate and the posterior wall
of the frontal sinus
2- Spontaneous: Destructive lesion involving the floor of the anterior cranial fossa
Clinical Picture
1- Watery fluid drips from the nose which increase in bending forward.
2- Meningitis.
Examination
1- Handkerchief test: The fluid associated with rhinitis contains mucous which stiffens a
handkerchief while CSF does not.
2- Nasal endoscope to see the site of the lesion.
Investigations
1- Identification of glucose in the secretion.
2- Injection of radioactive material into CSF via
lumber puncture.
3- CT. scan of the base of the skull.
Treatment
1- Medical
a- Bed rest in head up position.
b- Systemic antibiotics.
c- Avoidance of nose blowing and avoidance of nasal packing.
d- Reduction of CSF production rate by drugs ( acetazolamide , frusemide ) or by
repeated lumber puncture.
2- Surgical: if no response to medical treatment after 10-14 days, then;
a- Treat the cause.

XII
b- Craniotomy and fascial graft of the leaking site.
Oroantral fistula
A fistula that communicates the oral cavity with the maxillary sinus.
Aetiology
1- Dental extraction , particularly of the 1
st
upper molar teeth.
2- Malignant tumours of the antrum.
3- Penetrating wound.
4- Fistula following Caldwell-Luc operation.
Clinical Picture
1- Foul sinusitis and discharge of pus into the mouth.
2- Regurgitation of food particles and air into the nose.
Examination
1- Leakage of air from the fistula when the patient blows with a closed nose and open
mouth.
2- A probe can be passed from the mouth to the antrum.
Treatment
1- Immediate following dental extraction
suturing.
2- Late
Remove any retained food particles, control infection and then closure using a
mucoperiosteal flap.
Choanal Atresia
Congenital atresia of the posterior nares due to persistence of the bucconasal
membrane, usually unilateral but bilateral cases can occur and observed at birth because the
neonate is obligate nasal breather.
XIII
The obstruction either composed of bone (most commonly) or membrane.
The condition occurs in 1 out of every 7,000 to 8,000 live births.
Clinical Picture
Females are commonly affected than males.
Bilateral
Neonatal emergency leads to asphyxia because the infant is obligate nasal
breather and commonly associated with other congenital anomalies.
Unilateral-(60%) with a right-sided predominance
nasal obstruction and excessive nasal
discharge in the affected side which may be not noticed for some years.
Examination
1. Total absence of nasal air flow by mirror test and cotton test.
2. Plastic catheter or probe can’t be passed through the affected side to the nasopharynx.
3. Fibroptic endoscopy.
Investigations
Contrast radiography by instillation of radioopaque substance in the affected side.
CT scan to see the thickness of a bony atresia.
Treatment
Unilateral elective perforation of the occlusion usually prior starting of school.
Bilateral
oral airway
surgical intervention.

XIV
