Urinary Catheters
10/9/20161
Urinary CatheterDr. Frederick Foley
Developed in the 1920s by Dr. Frederick FoleyThe urinary catheter was originally an open system with the urethral tube draining into an open container.
In the 1950s, a closed system was developed in which the urine flowed through a catheter into a closed bag.
10/9/2016
2What is a urinary catheter
Urinary catheter is any tube placed in the body to drain and collect urine from the bladder10/9/2016
3
INDICATIONS FOR CATHETERISATION
broadly divided into two main categories:• to obtain drainage or
• to allow the instillation of diagnostic or therapeutic agents
The relief of acute or chronic urinary retention due to either bladder outlet obstruction or neurogenic bladder dysfunction is the most common indication for urethral catheterization
10/9/2016
4
to monitor urinary output
Urinary diversion by a catheter is used to allow healing after lower urinary tract surgery/traumato evacuate the bladder when the urine contains particulate matter, especially in combination with simultaneous irrigation (post transurethral resection, clot/purulent material evacuation)
10/9/2016
5
to collect of microbiologic clean urine (uncooperative patients because of age or mental status or comorbidities that prevent voluntary voiding)
to measure postvoid residual urine volume samples for diagnostic purposes
to provide access to the bladder for urinary tract imaging studies such as cystography, which requires the instillation of radiographic contrast material
10/9/2016
6
UC with a pressure monitoring catheter is used during urodynamic testing for physiologic assessment of voiding function
to allow instillation of pharmacologic agents for local therapy of some bladder pathologies such as chemo/immunotherapy for transitional cell carcinoma (mitomycin, BCG), interstitial cystitis (dimethyl sulfoxide), and intractable hematuria (e.g., alum, formalin instillation)
10/9/2016
7
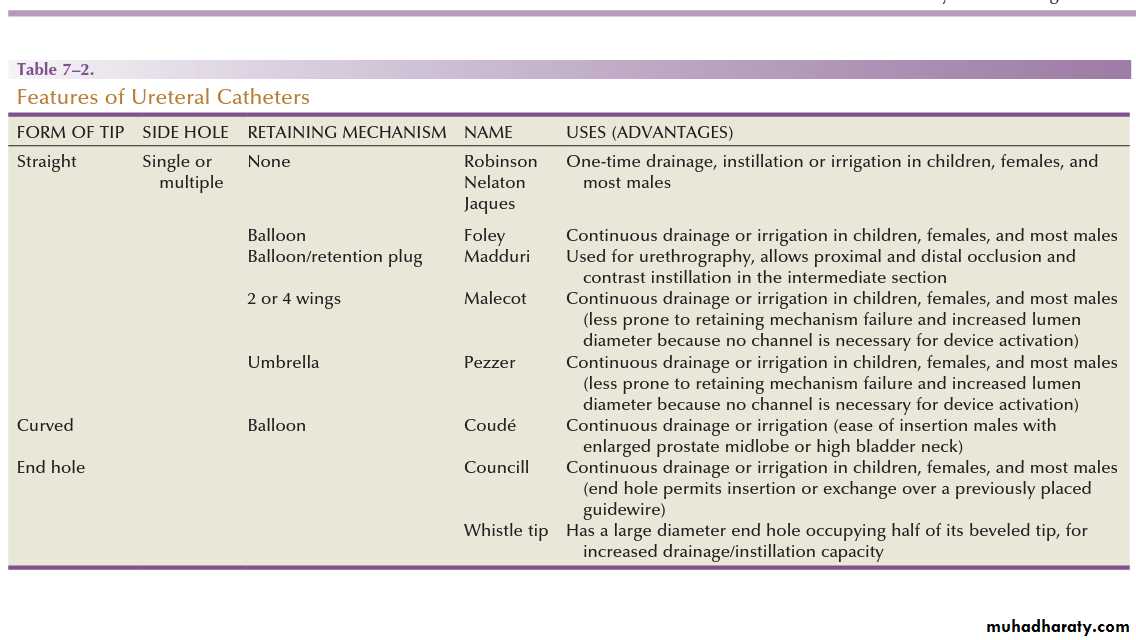
Catheter types
10/9/2016
8Documentation
Details regarding the catheterisation should be recorded in the patient’s notes. For further information please refer to your hospitals policy and procedure manual.10/9/2016
9Matters to consider for Catheterization
• Time and date of catheterisation
• Type of catheter
• Amount of water in balloon
• Size of catheter
• Expiry date of product
• Any problems on insertion
• Description of urine, colour and volume drained
• Specimen collected
• Review date
(Marsden Manual 2001)
10/9/2016
10
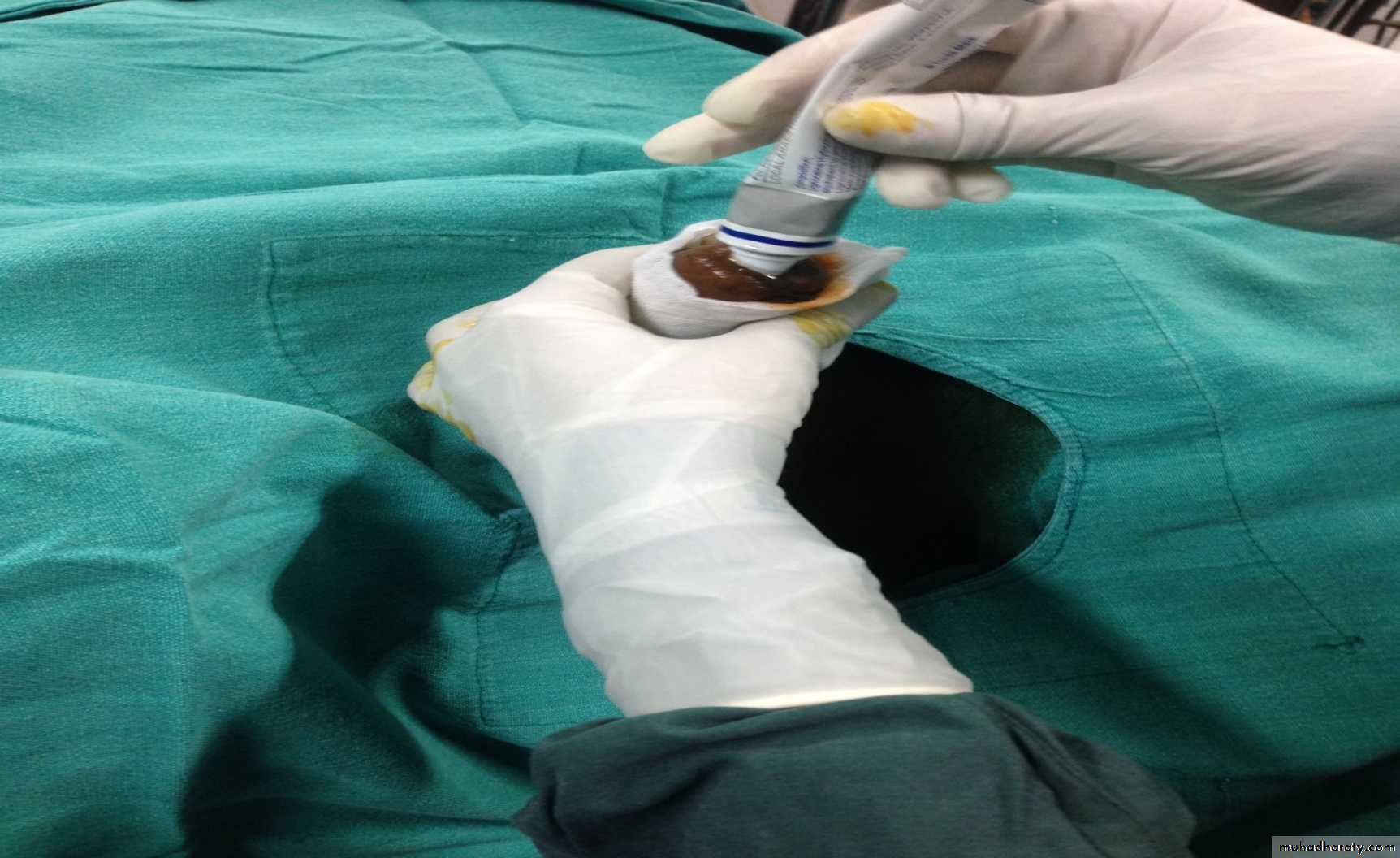
What you Need for Catheterization
1 Dressing trolley2. Catheterisation pack including penile
clamp
3. Sterile gloves
4. Appropriate size catheter
5. Xylocaine jelly syringe
6. Sterile water for the balloon
7. Syringe
8. Specimen jar
9. Antiseptic solution
10. Waterproof Sheet
11. Extra Jug
12. Light source
13. Tape to secure the catheter to the leg
14. Drainage bag
15 Urine bag holder
10/9/2016
11
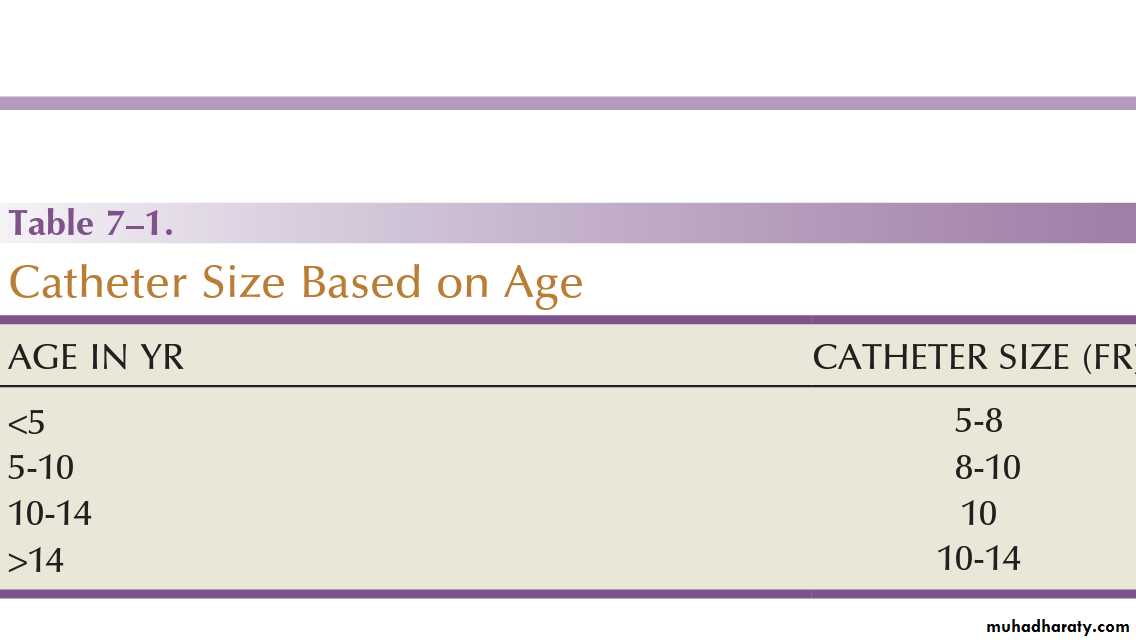
Catheter selection
The size and type of urinary catheter used depends on the indication for catheter insertion, age of the patient, and type of fluid expected to be drainedCatheter size is measured in the Charrière or French scale, whereby one Fr or Ch is equal to 0.33 mm. This measurement indicates the total circumference of the catheter and not the lumen size.
As a general rule, catheter size should be the smallest size that can accomplish the desired drainage
12 to 14 Fr for clear urine and 20 to 24 for thick pus or blood-filled urine
10/9/2016
12\
10/9/2016
13The use of feeding
tubes as urethral catheters should be discouraged because their
stiffness and length can be a source of complications (ischemic
ulcers, urethral strictures, and knotting in the bladder)
MATERIAL
Modern urinary catheters are most frequently made of latex, rubber, silicone, and polyvinylchloride (PVC).Rubber and latex catheters are often chosen for short-term drainage.
Silicone catheters are indicated when there is rubber/latex sensitivity or allergy and are particularly suited for patients requiring a longer period of indwelling time.
10/9/2016
14
Silicone is relatively inert, causing less tissue reaction, and is associated with less bacterial adherence than other catheter materials (Roberts et al, 1990)
Evidence suggests that the use of silicone catheters is associated with a lower incidence of urinary tract infections compared with those made of latex (Crnich et al, 2007).
10/9/2016
15
COATING
The application of a viable bacterial coating onto catheter surfaces as a method of reducing catheter-associated urinary tract infection (CAUTI) by bacterial interference is a novel approach that has shown promise in a small pilot study involving the use of Escherichia coli–coated cathetersThe rationale is based on natural competition by nonpathogenic bacteria overpowering any pathogenic bacteria that may enter the urinary tract (Trautneret al, 2007). Further study is necessary to confirm if this will be an effective strategy.
10/9/2016
16NO OF CHANNELS
SINGLE LUMEN: simple drainage or irrigation/instillationDOUBLE LUMEN: to permit addition of a retention balloon
TRIPLE LUMEN: for simultaneous drainage and irrigation(to drain thick fluids like pus or blood)
10/9/2016
17It should be borne in mind, however, that the addition of a multichannel catheter is accomplished by decreasing the overall internal diameter or lumen of the main drainage channel;
a 24-Fr three-way catheter has a smaller internal drainage diameter than a 24-Fr two-way, which has a narrower lumen than a 24-Fr one-way catheter.
10/9/2016
18
TIP SHAPE
BLUNT STRAIGHT TIP: most common (foley)CURVED TIP (COUDE): high bladder neck, prominent median lobe of prostate
END HOLE (COUNCILL): when catheterization over guide wire is required
10/9/2016
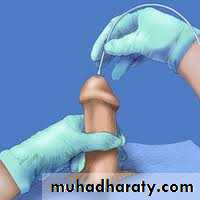
19TECHNIQUE OF CATHETER INSERTION
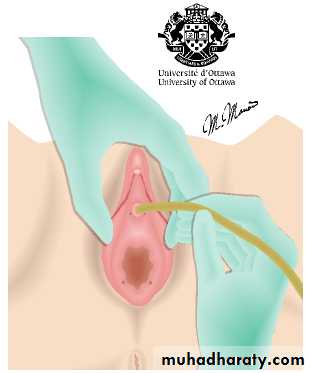
POSITION OF PATIENTMale: supine
Female: a “frog leg” position is most suitable
Use of stirrups – in very obese females
10/9/2016
20
ANESTHETIC
If topical anesthesia is to be used, evidence suggests it requires a minimum of 10 minutes of exposure (depending on the agent), sufficient volume of the agent (20 to 30 mL), and slow instillation time (>3 to 10 seconds)(Schede andThüroff, 2006; Tzortzis et al, 2009) to have the most effect.There is some evidence that cooling to 4° C diminished the discomfort of lignocaine gel instillation, probably due to a cryo-analgesic effect (Thompson et al, 1999; Goel and Aron, 2003).
10/9/2016
21
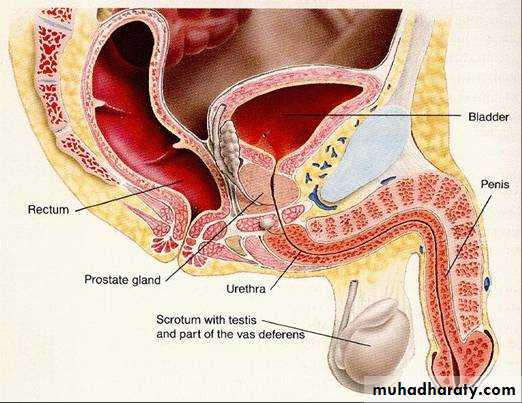
ANATOMIC CONSIDERATIONS
MALE:18 to 20 cm in length
its diameter variable, a mere slit to 6 mm during the passage of urine
follows a sigmoid curse, a proximal curve at the peno-bulbar junction and another at the bulbo-membranous junction
10/9/2016
22FEMALE:
LENGTH: 3.5 to 4 cm longThe meatus is usually in an anterior location and the bladder neck in a posterior location in the horizontal plane, giving the urethra a slight posterior inclination
10/9/2016
23
Structure of Foley Catheter
10/9/201624
PROCEDURE
10/9/2016
2510/9/2016
2610/9/2016
2710/9/2016
2810/9/2016
2910/9/2016
30
10/9/2016
3110/9/2016
3210/9/2016
3310/9/2016
34Gravity will help the Draining of Bladder
Gravity is important for drainage and the prevention of urine backflow. Ensure that catheter bags are always draining downwards, do not become kinked and are secured and below thigh level. Metal or plastic hangers should be attached to the side of the bed. Cloth bags tied to the bed to support the bags are also available10/9/2016
35
Rapid draining leads to Complications
Rapid drainage of large volumes of urine from the bladder may result in hypotension and/or haemorrhage.(Upson 1995) Clamp catheter if the volume drained is 1000mls or greater. After 20minutes release the clamp and allow urine to drain10/9/2016
36Collection of urine from catheterised patients
The process of obtaining a sample of urine from a patient with an indwelling urinary catheter must be obtained from a sampling port. The sample must be obtained using an aseptic technique.This port is usually situated in the drainage tubing, proximal to the collection bag which ensures the freshest sample possible. The use of drainage systems without a sampling port should be avoided (Gilbert, 2006).
10/9/2016
37
Specimens for Culturing Should not be Cultured from Urine bags
Specimens should not be collected from the tap from the main collecting chamber of the catheter bag as colonisation and multiplication of bacteria within the stagnant urine or around the drainage tap may have occurred.10/9/2016
38Care of Inserted Catheters
Every day , wash around the catheter and perineum with soap and water; rinse and dry these areas well. you may shower while wearing the catheterSitting in the tub, however , is not recommended. Good personal hygiene pre vents the accumulation of bacteria, reduces the risk of infection, and prevents odour
10/9/2016
39
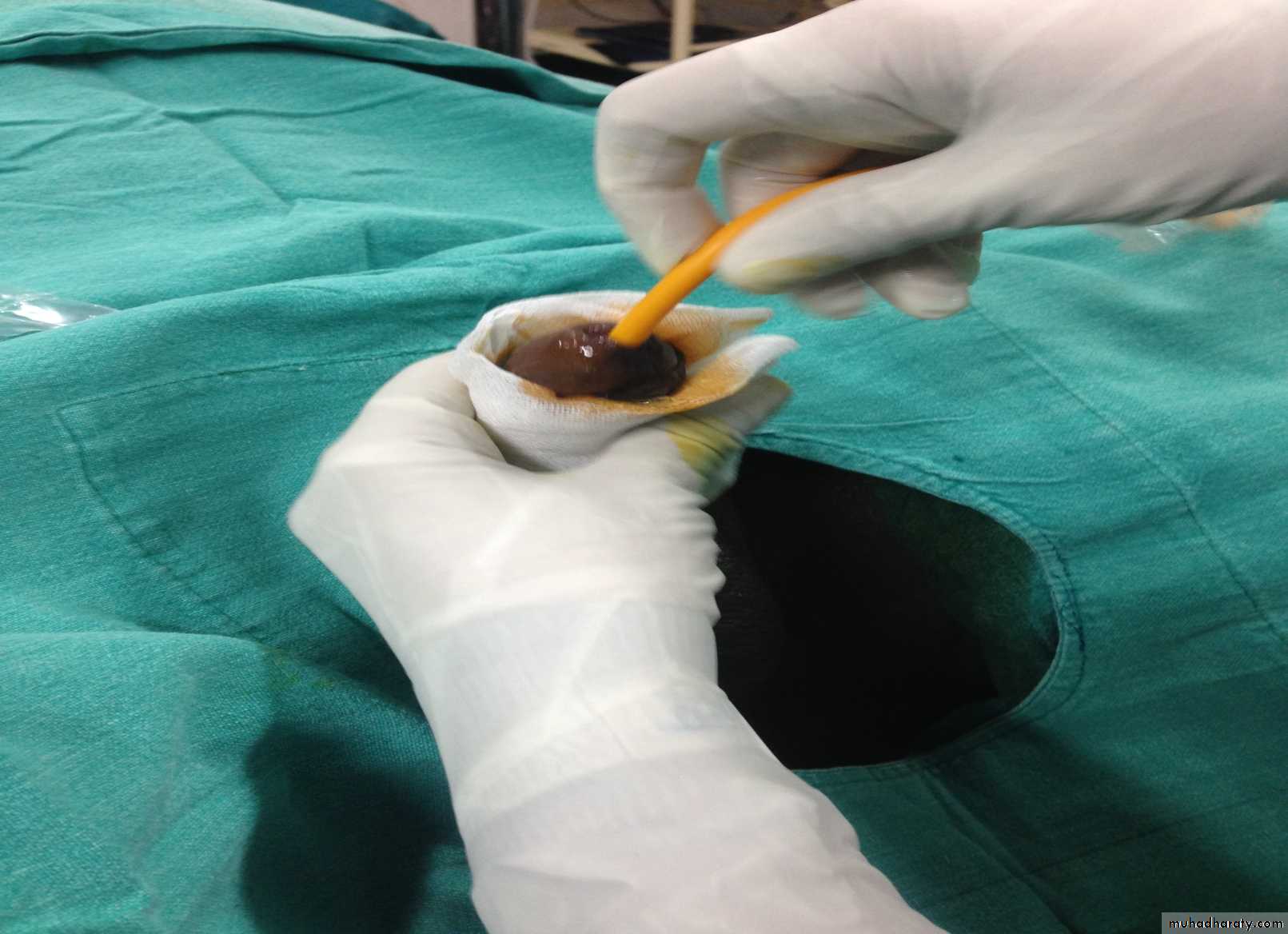
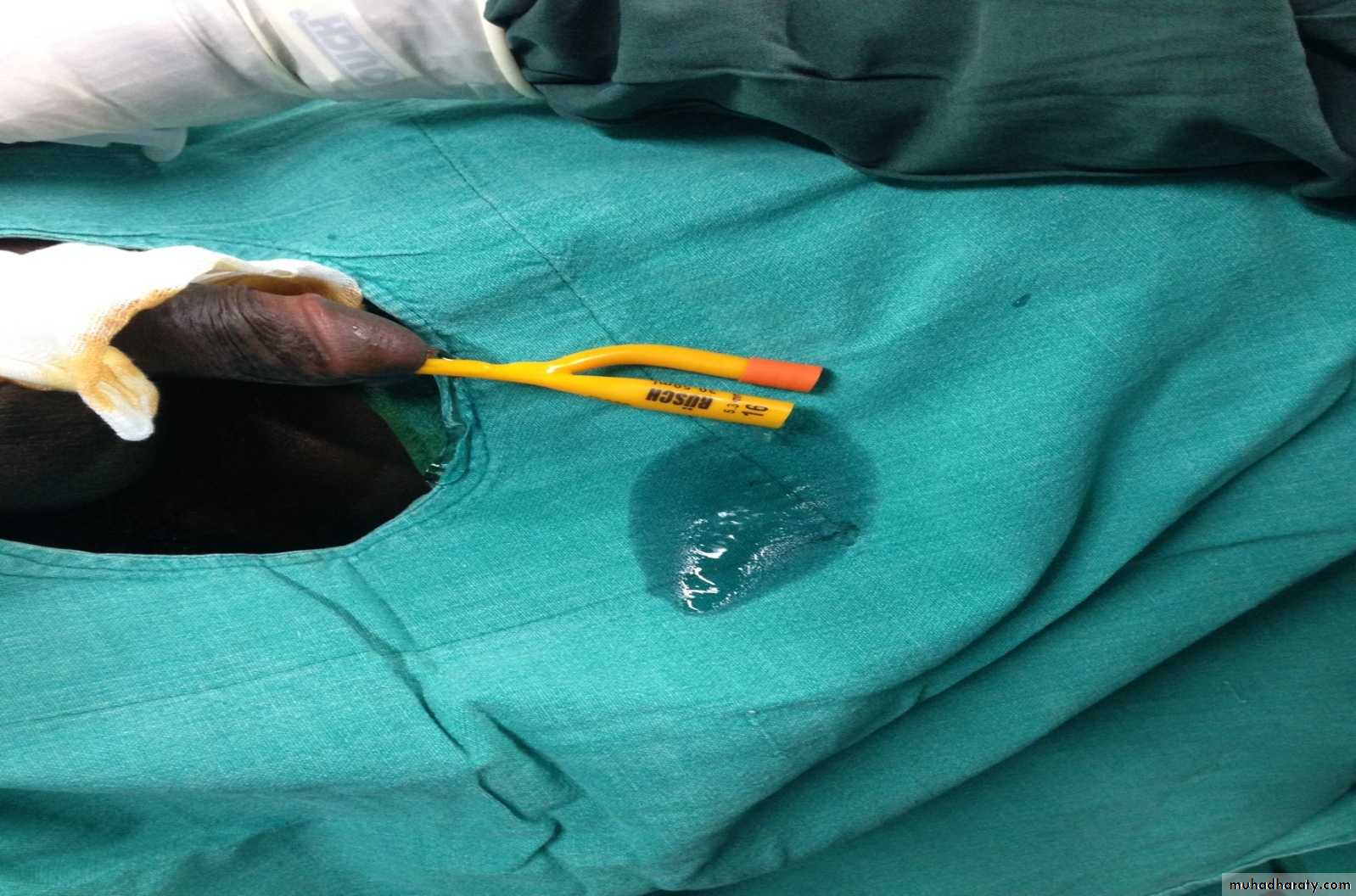
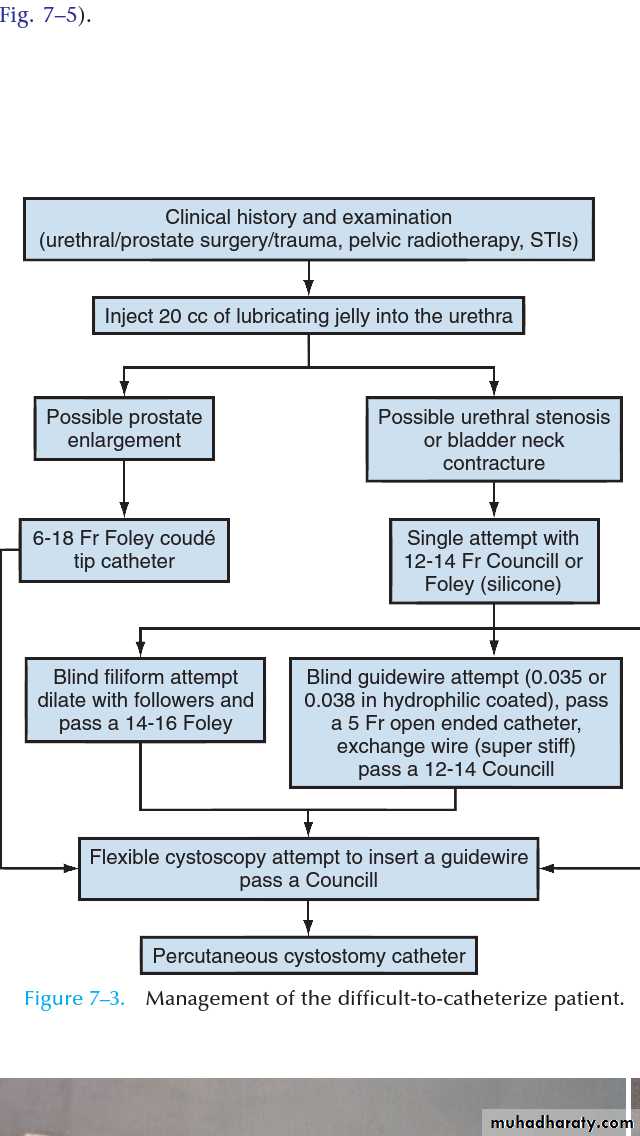
DIFFICULT CATHETERIZATION
10/9/2016
40COMPLICATIONS
UTIs account for 40% of all nosocomial infections. The major risk factor is the use of urethral catheters, which are responsible for up to (80%) of UTIs in the hospital setting (Ha and Cho, 2006)
Risk factors for CAUTIs:
patients requiring more than 6 days of catheterization,
female gender
active nonurinary infection sites
preexisting medical conditions
Malnutrition
renal insufficiency
catheter insertion other than in the operating room
drainage tubing or a bag elevated above the level of the bladder(Maki and Tambyah, 2001).
10/9/2016
41
hematuria,
urethral and meatal stricturesurethral perforation
Allergic reactions including anaphylaxis (Thomas et al, 2009; Wyndaele,2002).
Especially at risk are patients with long-term indwelling
Catheters
Malignant neoplasms (2.3% to 10%)
stone formation (46% to 53%),
bladder neck and urethral erosions (Igawa et al, 2008).
10/9/2016
42
A unique complication: Inability to remove catheter from the bladder, reasons being
Due to encrustations,
Entrapment by sutures, or
Inability to disengage/deflate the retaining balloon
10/9/2016
43HOW TO MANAGE THIS CONDITION?
Encrustations:Mild encrustations-gentle traction will solve the problem
Significant encrustations-a semirigid ureteroscope and the holmium:YAG laser to remove the stone fragments
10/9/2016
44Entrapment by suture(recent bladder or prostate surgery)
semirigid ureteroscopy along the catheter and using the holmium:YAG to release the suture have also been described (Bagley et al, 1998; Nagarajan et al,2005).Because the suture materials used in bladder and prostate surgery are often absorbable, waiting for suture dissolution is another option.
10/9/2016
45
Inability to deflate a foley balloon: a stepwise approach is followed
One should first attempt to place another 1 to 2 mL of fluid in the balloon to ensure normal balloon contour, which may be important with the large-volume balloons
the next step is to cut the inflation port
insert a surgical steel wire (24 or 28 gauge; often included as an obturator for small-caliber ureteral catheters) or the stiff end of a 0.035-inch hydrophilic-coated guidewire through the valve inflation lumen
10/9/2016
46ultrasound-guided needle puncture can be conducted with a lon spinal needle (22 gauge) using either a transrectal, transvaginal, or suprapubic surface probe (Daneshmand et al, 2002)
open surgery
10/9/2016
47
Overinflation of the balloon not recommended-painful to the patient and may cause bladder injury and fragmentation and retention of the balloon fragments (Gülmez et al,1996)
Use of chemical instillations such as ether or toluene to induce balloon rupture should be discouraged because these agents can cause chemical cystitis (Patterson et al,2006)
10/9/2016
48
REFERENCES
Bagley DH, Schultz E, Conlin MJ: Laser division of intraluminal sutures. J Endourol. 12 (4):355-357 1998 9726402Bjerklund Johansen T, Hultling C, Madersbacher H, et al.: A novel product for intermittent catheterisation: its impact on compliance with daily life—international multicentre study. Eur Urol. 52 (1):213-220 2007 17166653
Chung C, Chu M, Paoloni R, et al.: Comparison of lignocaine and water-based lubricating gels for female urethral catheterization: a randomized controlled trial. Emerg Med Australas. 19 (4):315-319 2007 17655633
Crnich CJ, Drinka PJ: Does the composition of urinary catheters influence clinical outcomes and the results of research studies?. Infect Control Hosp Epidemiol. 28 (1):102-103 2007 17301937
Daneshmand S, Youssefzadeh D, Skinner EC: Review of techniques to remove a Foley catheter when the balloon does not deflate. Urology. 59 (1):127-129 2002 11796297
Davenport K, Keeley FX: Evidence for the use of silver-alloy-coated urethral catheters. J Hosp Infect. 60 (4):298-303 2005 15936115
De Ridder DJ, Everaert K, Fernández LG, et al.: Intermittent catheterisation with hydrophilic-coated catheters (SpeediCath) reduces the risk of clinical urinary tract infection in spinal cord injured patients: a prospective randomised parallel comparative trial. Eur Urol. 48 (6):991-995 2005 16137822
Ellis H: The Foley catheter. J Perioper Pract. 16 (4):210-211 2006 16669367
Garbutt RB, McD Taylor D, Lee V, Augello MR: Delayed versus immediate urethral catheterization following instillation of local anaesthetic gel in men: a randomized, controlled clinical trial. Emerg Med Australas. 20 (4):328-332 2008 18782206
Garcia MM, Gulati S, Liepmann D, et al.: Traditional Foley drainage systems—do they drain the bladder?. J Urol. 177 (1):203-207 2007 17162043
Goel R, Aron M: Cooled lignocaine gel: does it reduce urethral discomfort during instillation?. Int Urol Nephrol. 35 (3):375-377 2003
10/9/2016
49
Gülmez I, Ekmekcioglu O, Karacagil M: A comparison of various methods to burst Foley catheter balloons and the risk of free-fragment formation. Br J Urol. 77 (5):716-718 1996 8689117
Ha US, Cho YH: Catheter-associated urinary tract infections: new aspects of novel urinary catheters. Int J Antimicrob Agents. 28 (6):485-490 2006 17045784
Ho KJ, Thompson TJ, O’Brien A, et al.: Lignocaine gel: does it cause urethral pain rather than prevent it?. Eur Urol. 43 (2):194-196 2003 12565779
Igawa Y, Wyndaele JJ, Nishizawa O: Catheterization: possible complications and their prevention and treatment. Int J Urol. 15 (6):481-485 2008 18430150
Jahn P, Preuss M, Kernig A, et al. Types of indwelling urinary catheters for long-term bladder drainage in adults. Cochrane Database Syst Rev 2007;(3):CD004997.
Johnson JR, Kuskowski MA, Wilt TJ: Systematic review: antimicrobial urinary catheters to prevent catheter-associated urinary tract infection in hospitalized patients. Ann Intern Med. 144 (2):116-126 2006 16418411
Lee SJ, Kim SW, Cho YH, et al.: A comparative multicentre study on the incidence of catheter-associated urinary tract infection between nitrofurazone-coated and silicone catheters. Int J Antimicrob Agents. 24 (Suppl 1):S65-S69 2004 15364311
Madineh SM: Avicenna’s canon of medicine and modern urology. Part III: other bladder diseases. Urol J. 6 (2):138-144 2009 19472137
Maki DG, Tambyah PA: Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 7 (2):342-347 2001
10/9/2016
50
Thank you
10/9/201651