DIAGNOSTIC PROCEDURES IN ENDODONTICS
معالجة اسنان \ خامسد. نوفل م(1)
16\11\2016
Diagnosis: is a process of determining the nature of a disease. It is very important for proper treatment.
Differential diagnosis: is the process of differentiating between similar diseases.
For correct differential diagnosis:
Proper knowledge of the disease
Skill and Art on how to apply proper diagnostic methods
Symptoms: are phenomenon of deviation from the normal, and are indicative of an illness like pain, Tenderness
Types:
1. Subjective Symptoms are those which are experienced and reported to the clinician by the patient.
2. Objective Symptoms are those, which are obtained by the clinician through various tests.
Signs: are the abnormal signs that are appear on
the patient with or without clinical examination
like swelling, redness, scar.
Pain history
1-Duration When did your pain start?Have you ever had a pain like this before?
2-Character What type of pain is it?
3-Periodicity When do you get the pain?
Does it come and go?
Is there any particular pattern to the pain?
4-Severity How severe is your pain?
5-Site Where is your pain?
6-Radiation Does your pain spread to other areas?
7-Provoking factors Does anything make your pain worse?
8-Relieving factors Does anything make your pain better?
9-Associated factors Have you noticed anything else about your pain?
Common symptoms
• Lingering tooth sensitivity to cold liquids.
• Lingering tooth sensitivity to hot liquids.
• Tooth sensitivity to sweets.
• Tooth pain to biting pressure.
• Tooth pain that is referred from a tooth to another area, such as the neck, ear.
• Spontaneous toothache, such as that experienced while reading a magazine, watching television, etc.
• Constant or intermittent tooth pain.
• Severe tooth pain.
• Throbbing tooth pain.
• Tooth pain that may occur in response to postural changes, such as when going from a standing to a reclining position.
Correct clinical diagnosis
Good case history: should include1- Chief complaint
2- History of chief complaint
3- Past medical history
4- Past dental history
5- Also includes vital signs, history of presenting illness.
6- Thorough clinical examination
7- Relevant investigations / diagnostic tests
Medical conditions requiring Modification of treatment and consultation
• Cardiovascular:• High & moderate risk of Endocarditis
• Pathologic heart Murmers
• Hypertension
• Unstable angina
• Recent myocardial infarction
• Arrythmias
• Poorly managed congestive heart failure.
• Pulmonary: COPD, Asthma, Tuberculosis
• GI & Renal:
• End stage renal disease , Hemodialysis
• Viral hepatitis( B,C,D,E)
• Alcoholic liver disease
• Peptic ulcer disease
• Endocrine & Hematologic:
• STDs, HIV & AIDS
• Diabetes mellitus
• Adrenal insufficiency
• Pregnancy
• Bleeding disorders
• Cancer & leukemia
• Osteoarthritis, rheumatoid arthritis, SLE.
The duration of pain:
When the pain is of a shorter duration (1 minute) Reversible Pulpitis. Excellent chance of recovery without the need for endodontic treatmentWhereas when the pain is of a longer duration, it is considered to be Irreversible Pulpitis
The localization of pain:
1- Do not believe patient finger when pointing to the tooth.
2- Sharp piercing pain can usually be localized and responds to cold
3- Dull pain usually referred / spread over a larger area responds more abnormally to heat
4- Patients may report that their dental pain is exacerbated while lying down or bending over, this occurs because of the increase in blood pressure to the head, which therefore increases the pressure on the confined pulp
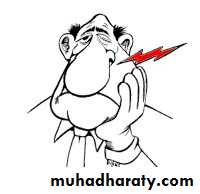
Reversible pulpitis Vs Irreversible pulpitis
Factors which provoke / relieve pain:
Response to a provoking factor (e.g. on mastication) indicates pulp vitality, but stimulation causing extended severe pain suggests irreversible pulpitis..
The clinician should look for:
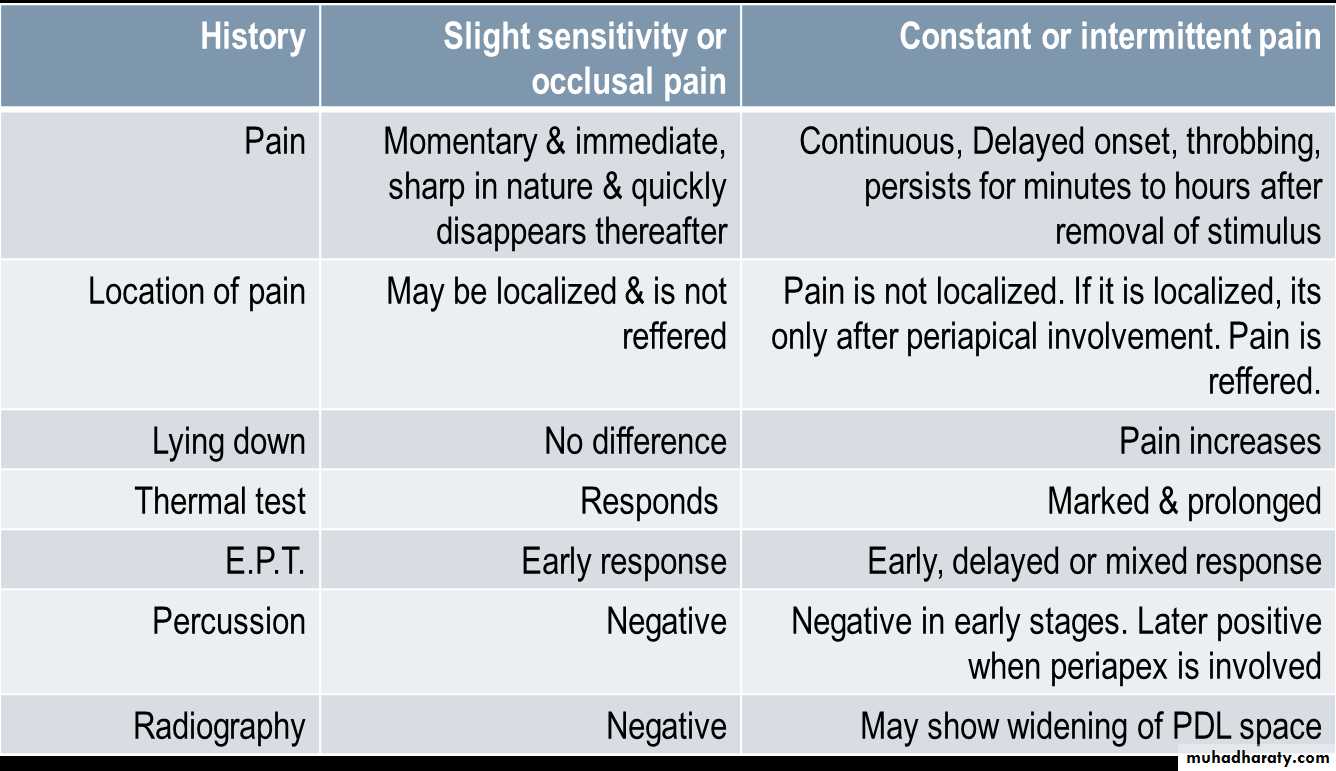
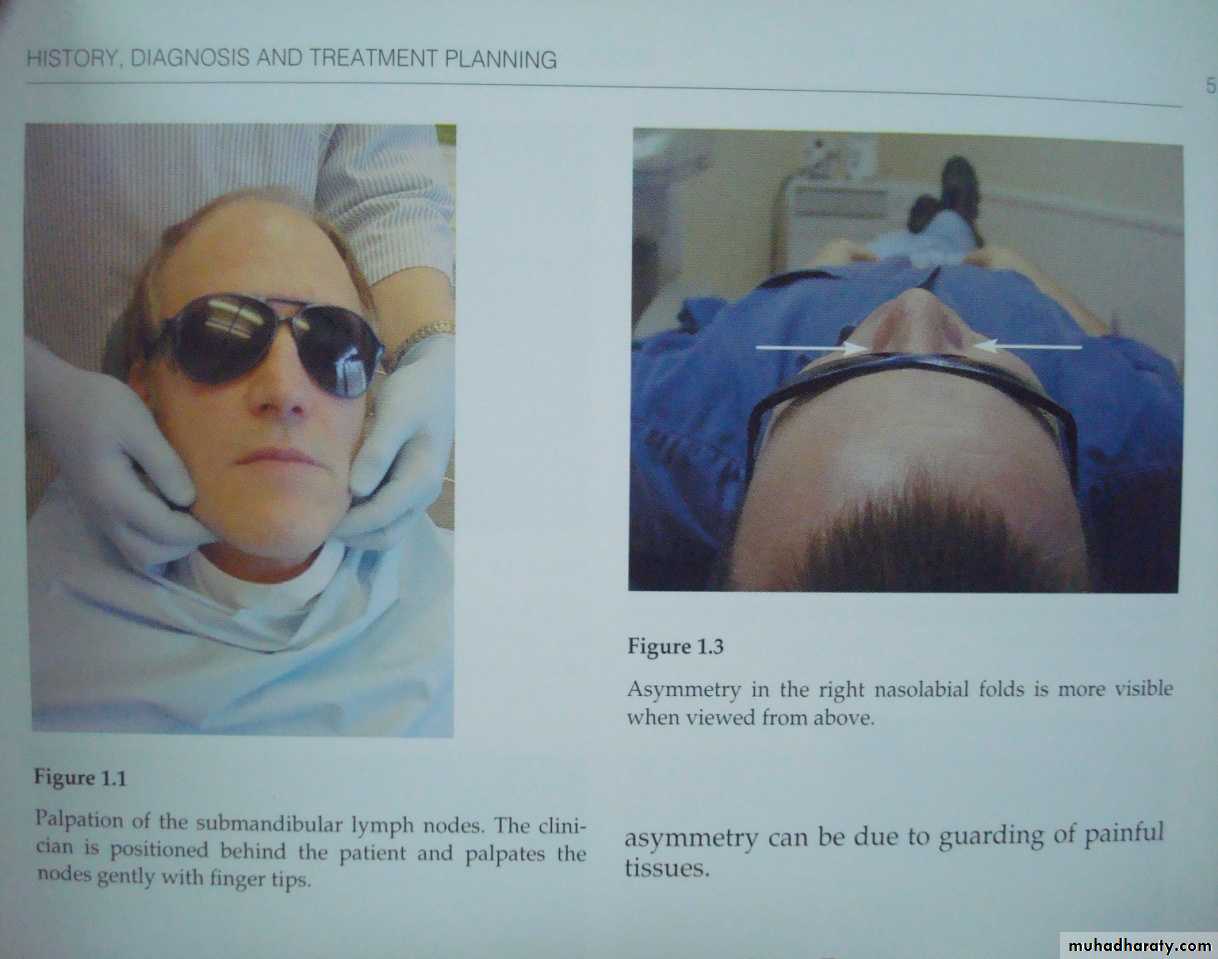
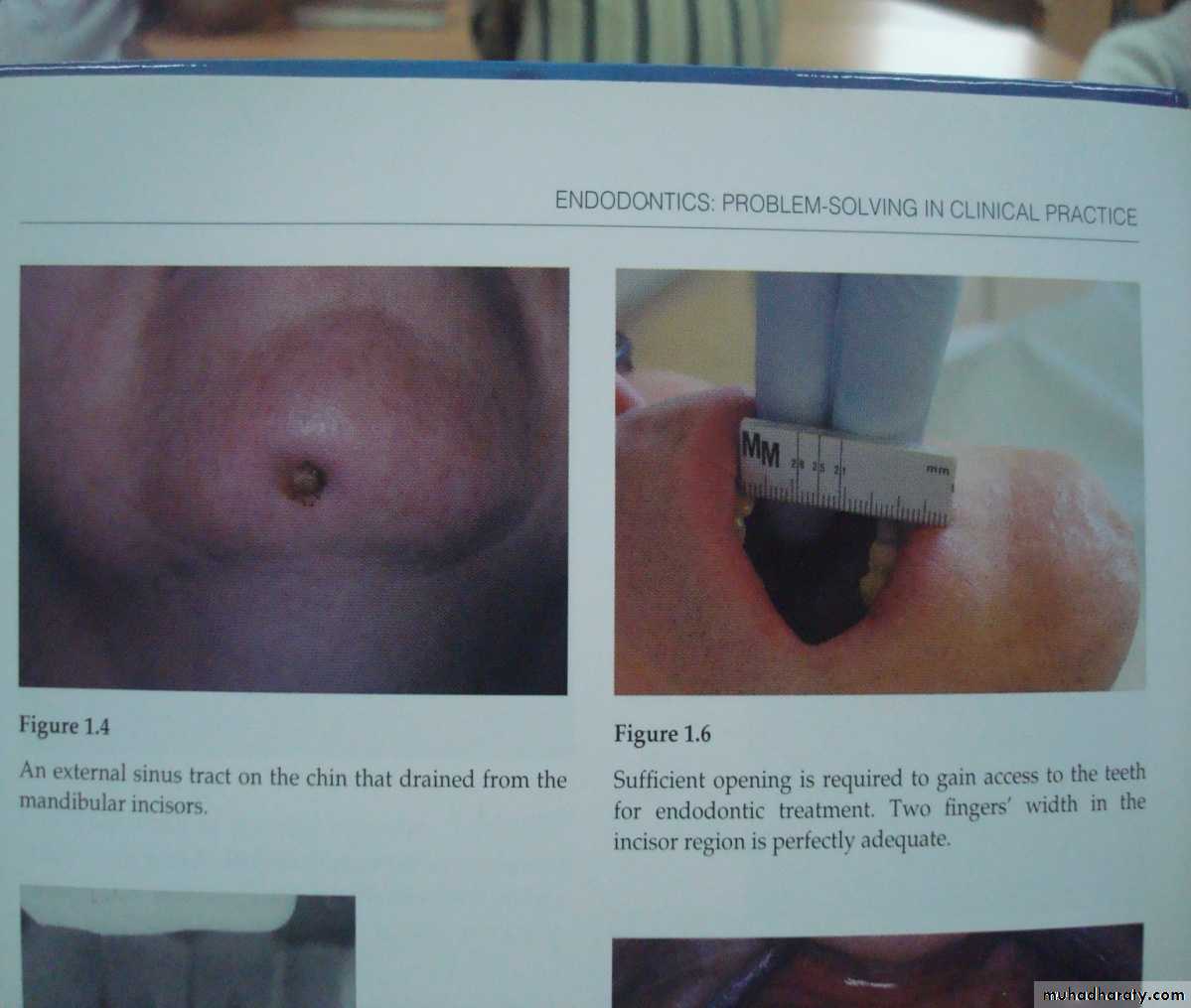
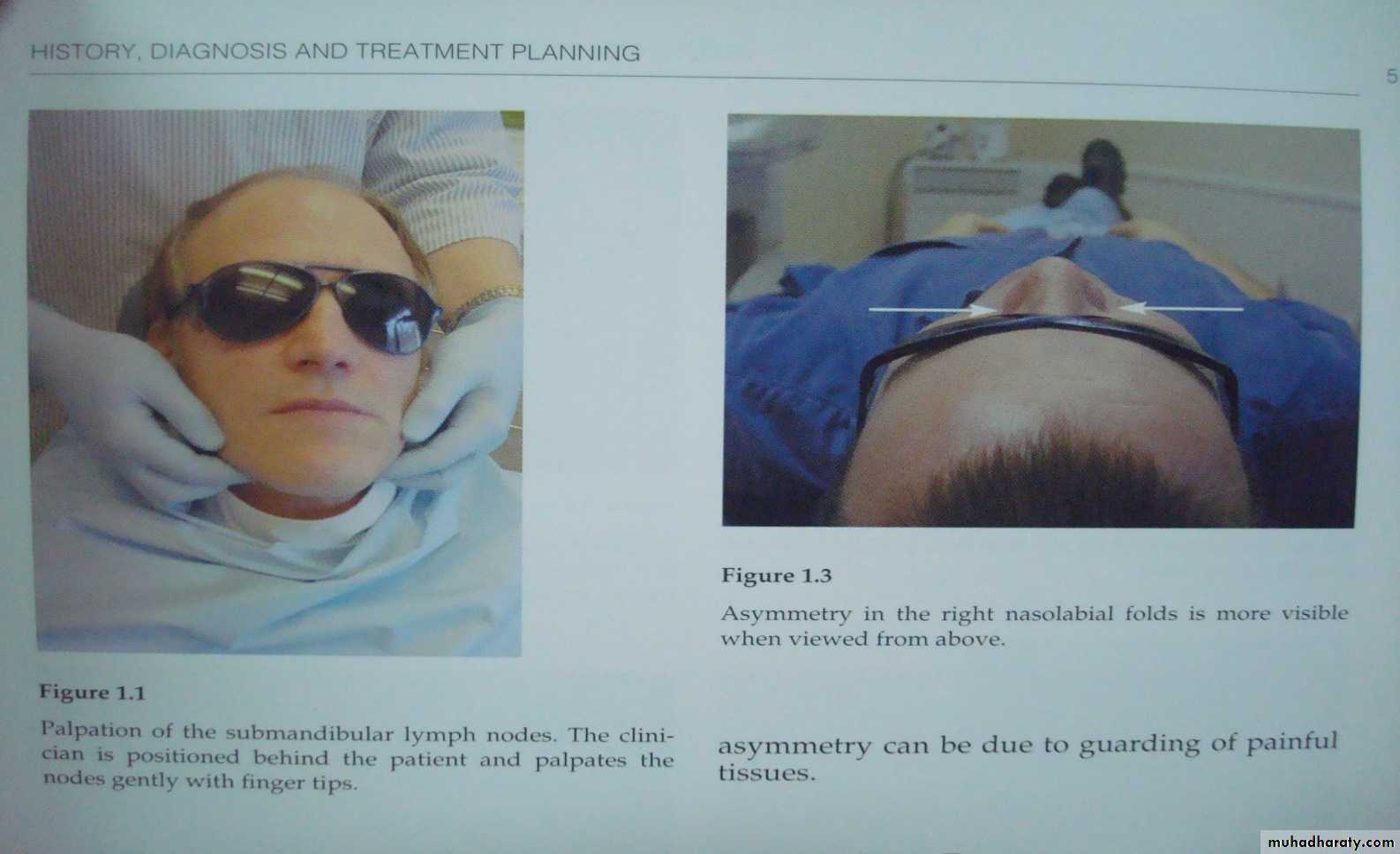
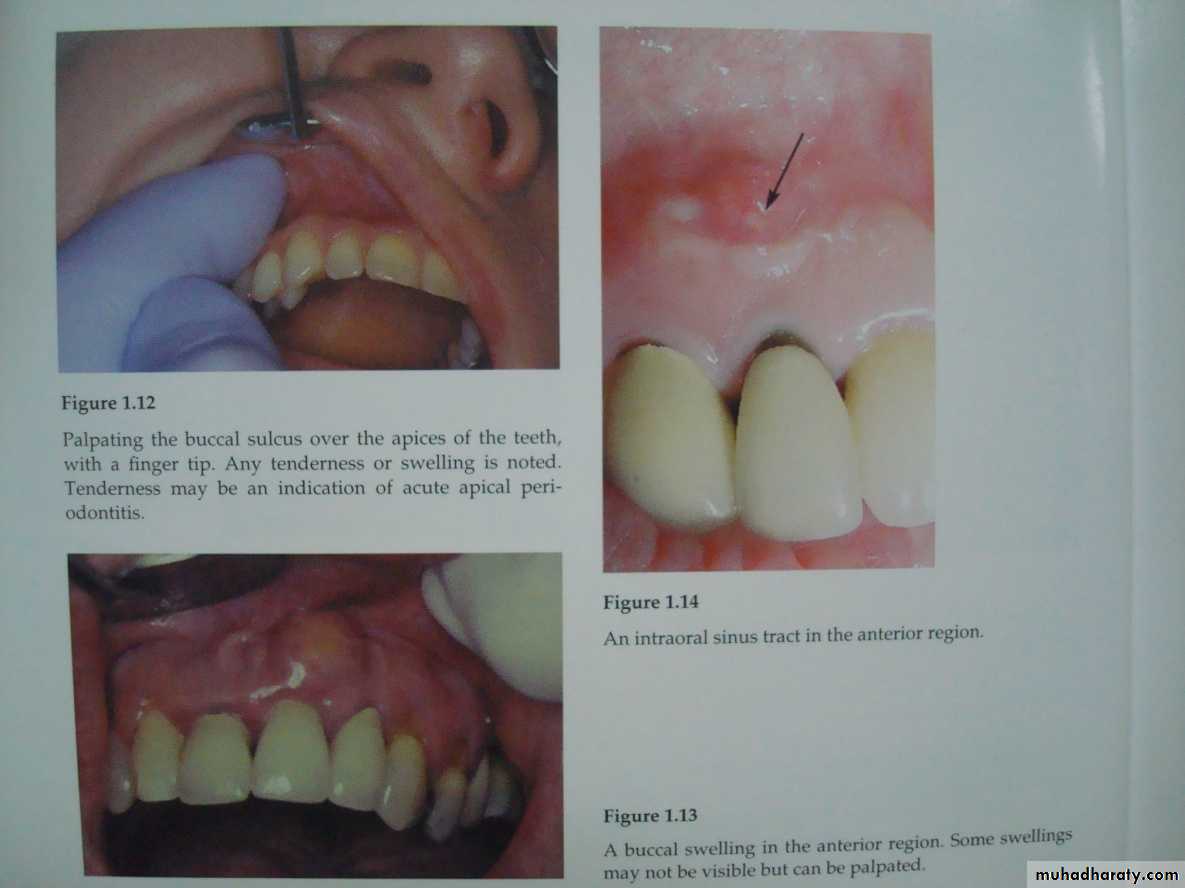
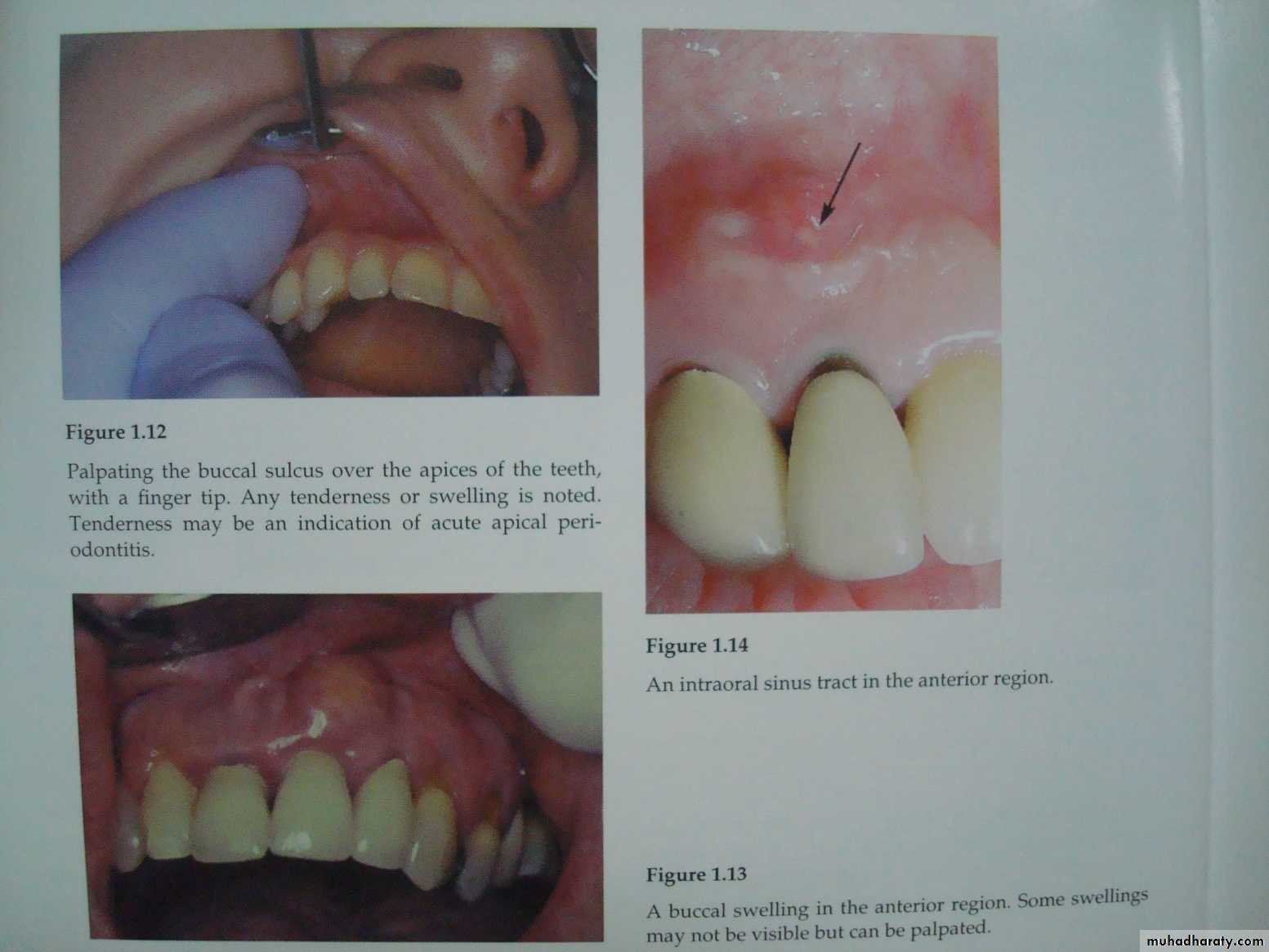
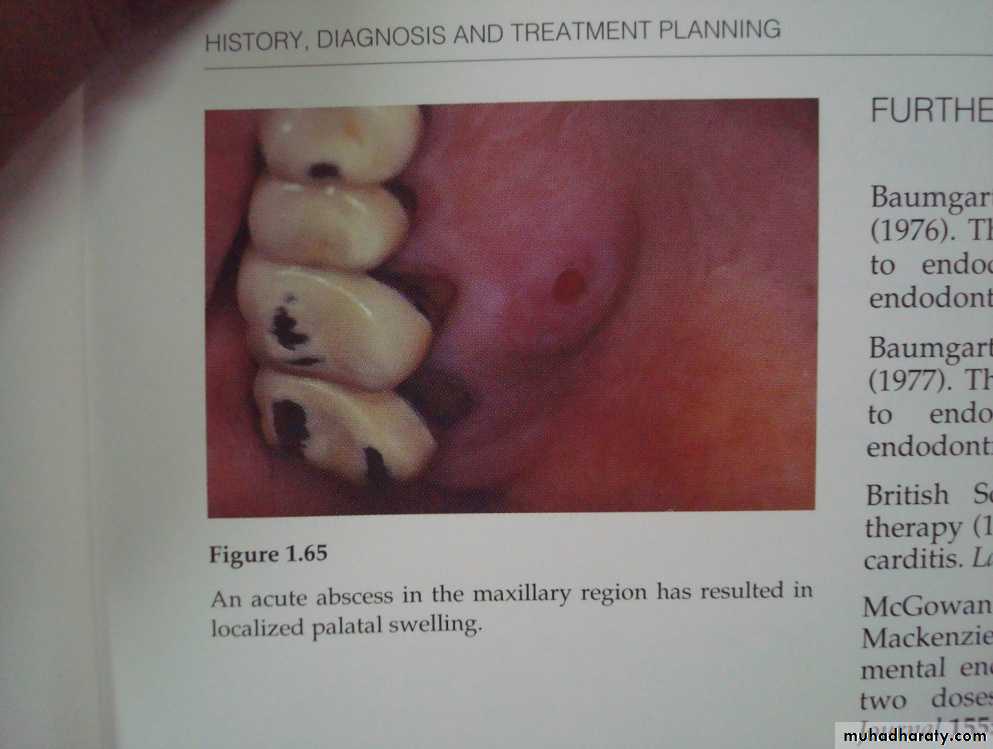
Facial asymmetryLocalized swellings
Lymphadenopathy
Changes in color, bruises/ scars.
Clinical examinationExtra Oral Examination
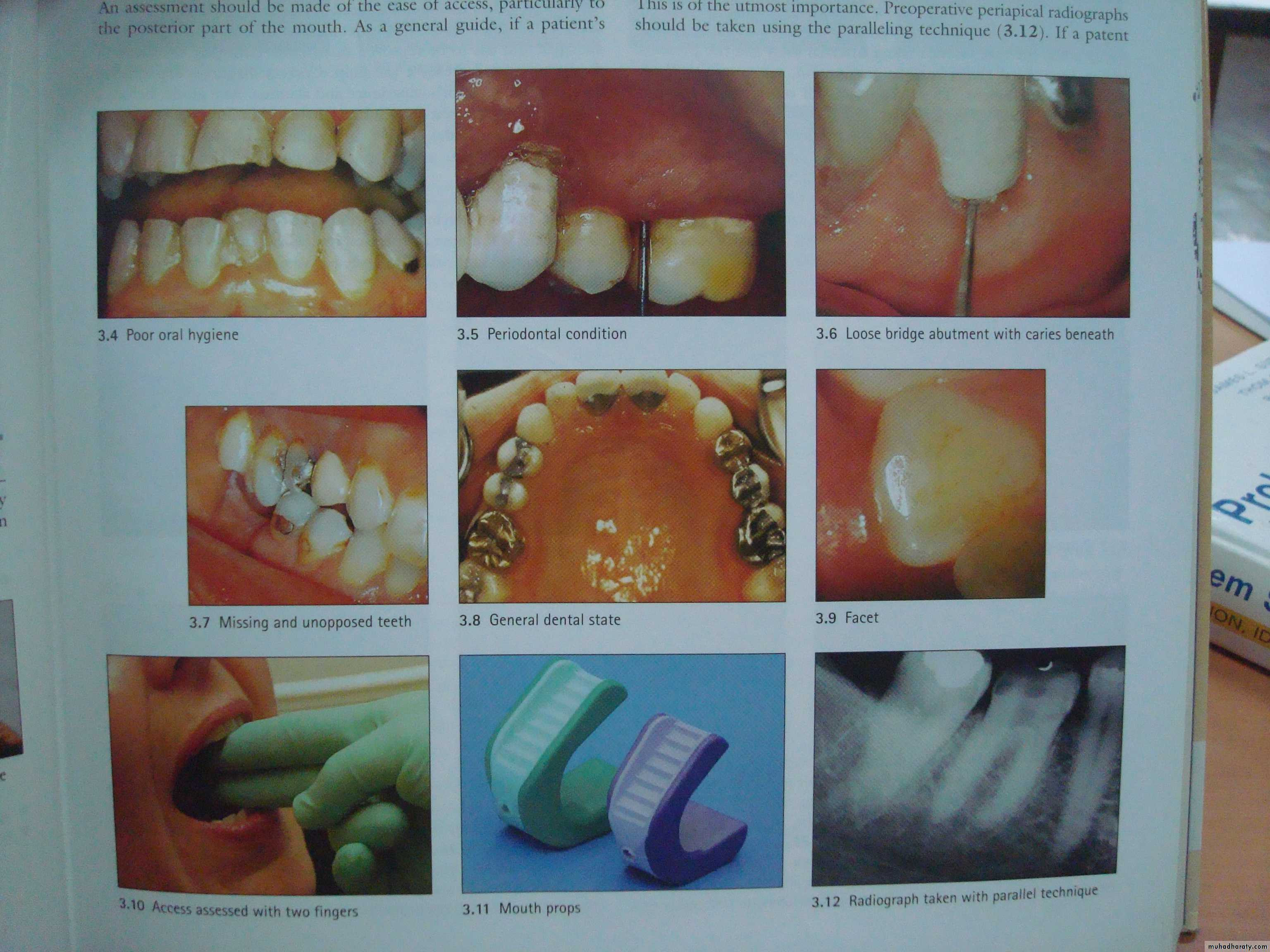
VISUAL AND TACTILE INSPECTION
Soft tissue:-Color- the normal color of gingiva is coral pink. Change from this is easily visualized in inflammatory conditions. Contour- change in normal contour (eg, of scalloped gingiva) occurs with a swelling. Consistency- On inspection (most commonly gingiva) appears healthy, firm, resilient, while a soft, fluctuant or spongy tissue is more indicative of a pathological state.Hard tissue:
Color- Normal teeth show life like translucency & sparkle that is missing in pulp less teeth which appear more or less opaque. Note: This discoloration however could be due to a variety of other reasons like old amalgam restorations, tetracycline stains etc.Contour- This examination should also include the visualization of contours of affected teeth, such as fractured teeth, wear facets, improperly contoured restorations, or altered crown contours as these factors can have a marked effect on the respective pulps.
Consistency- Change in the consistency of hard dental tissues is related to the presence of caries, external and internal resorption
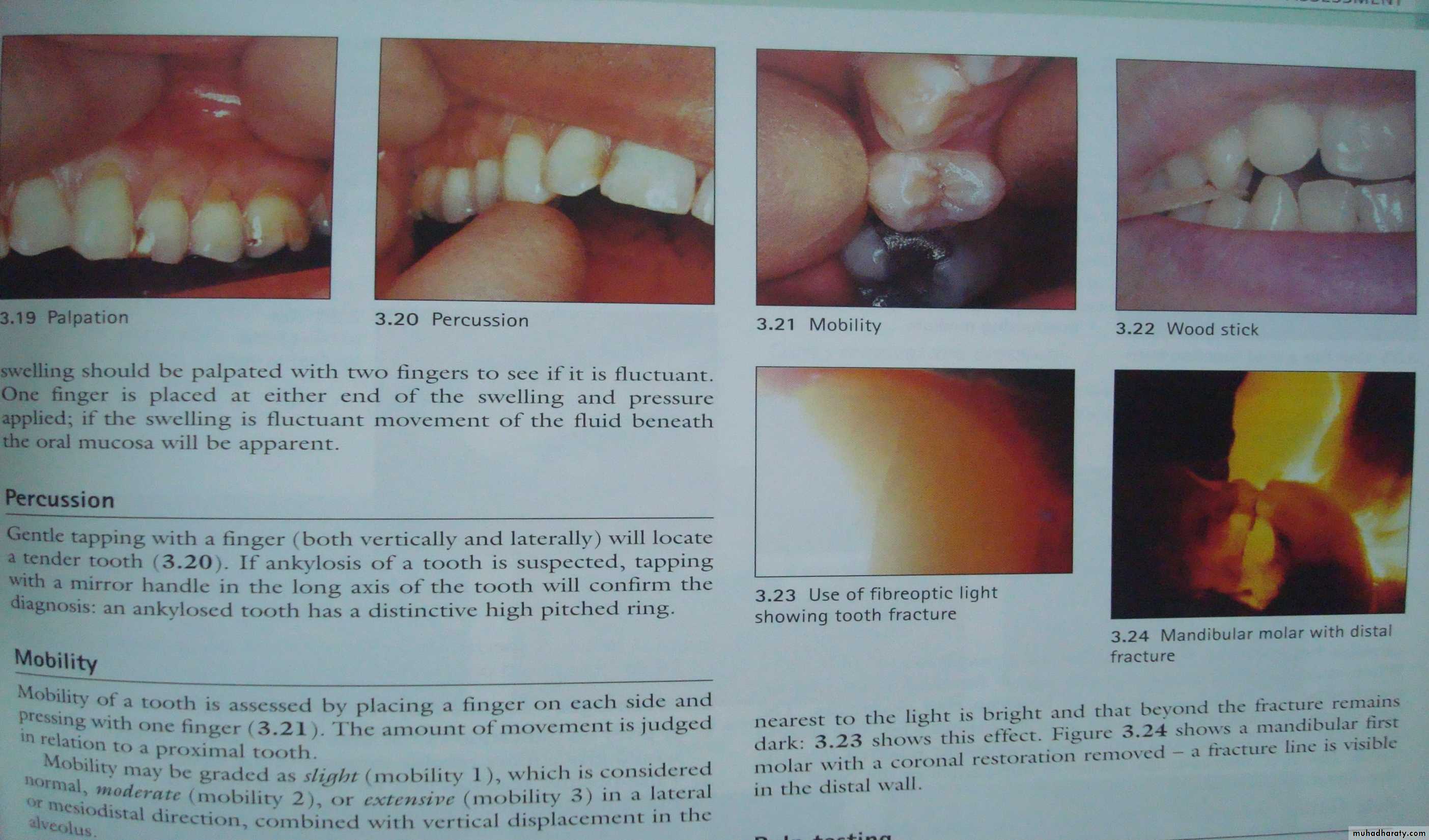
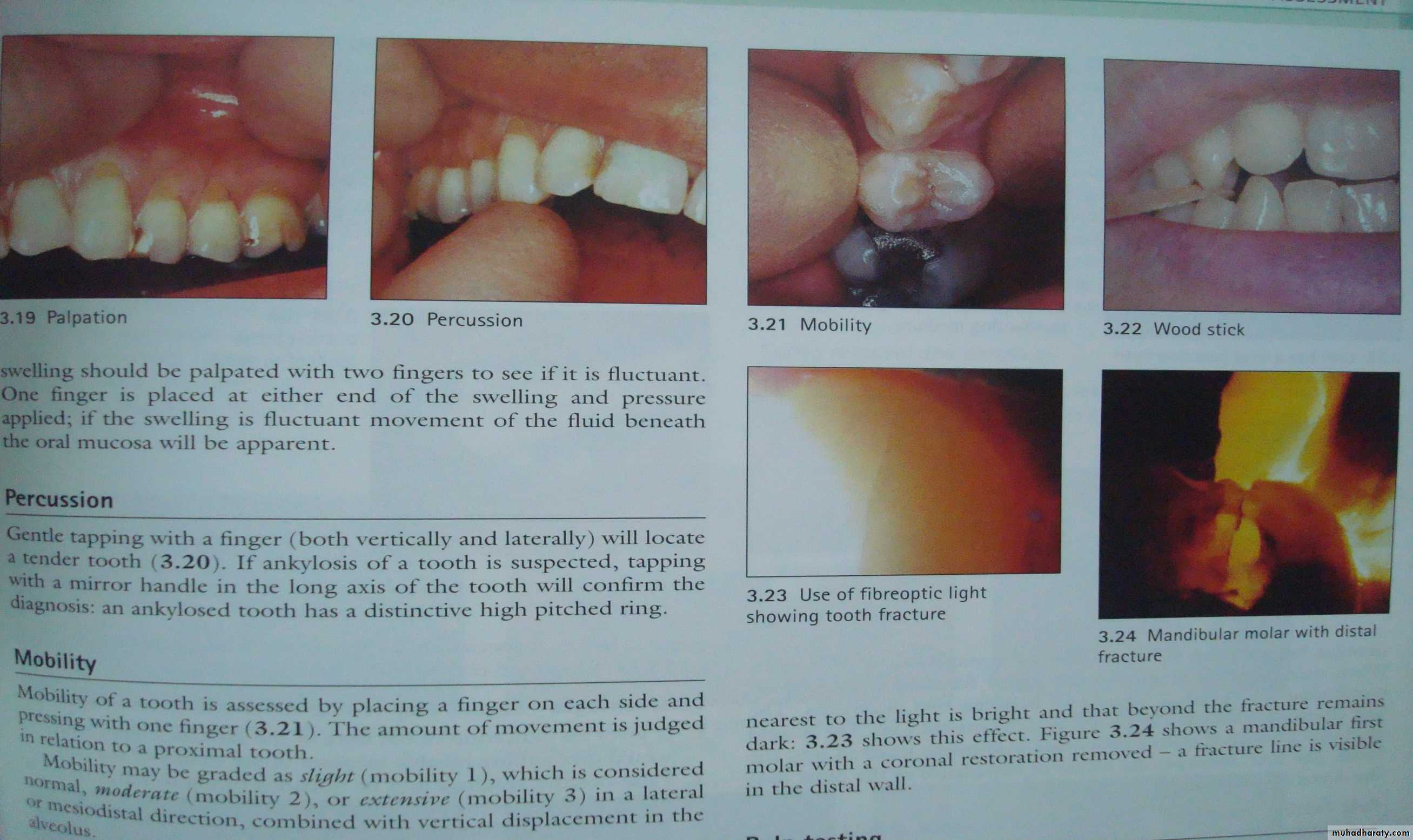
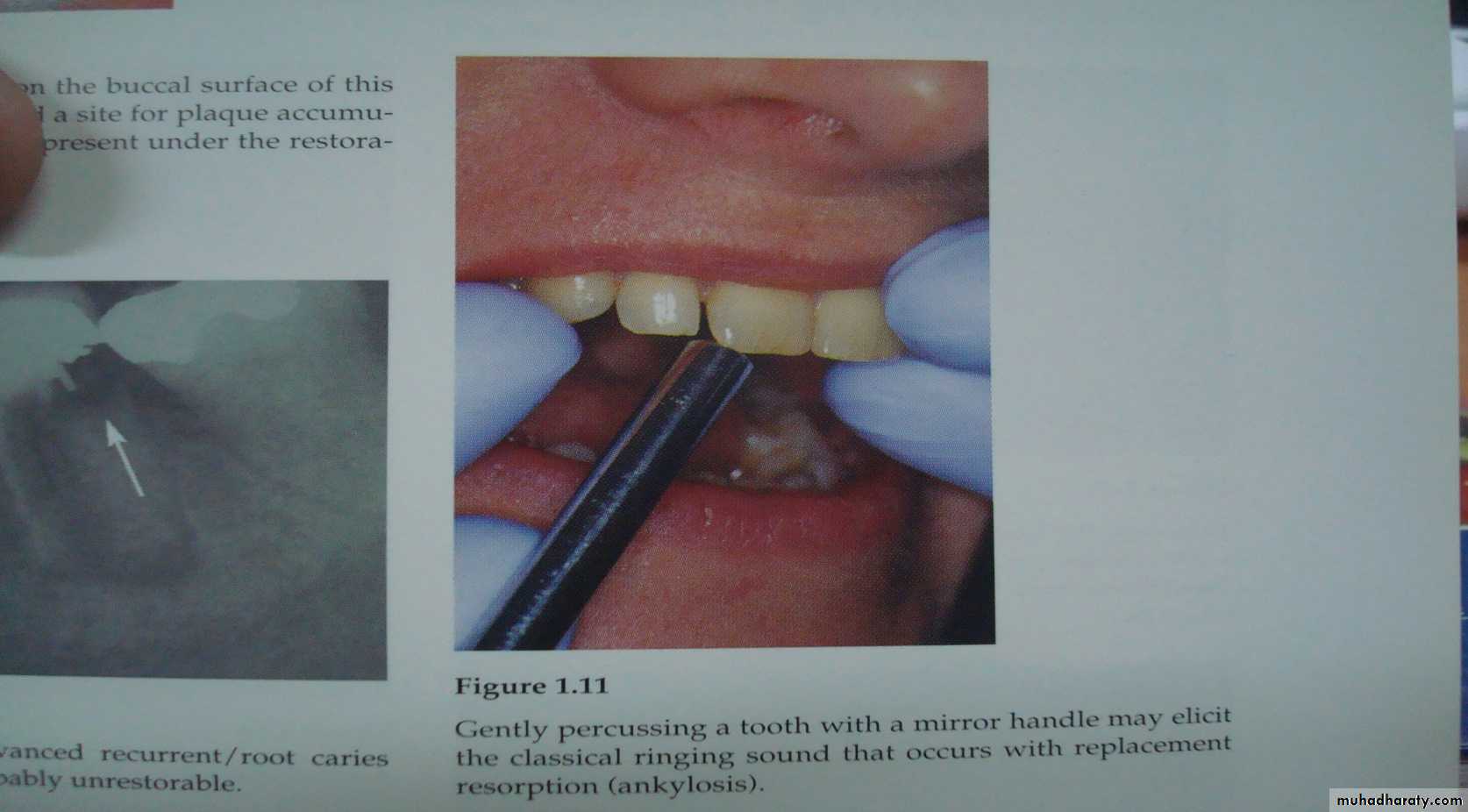
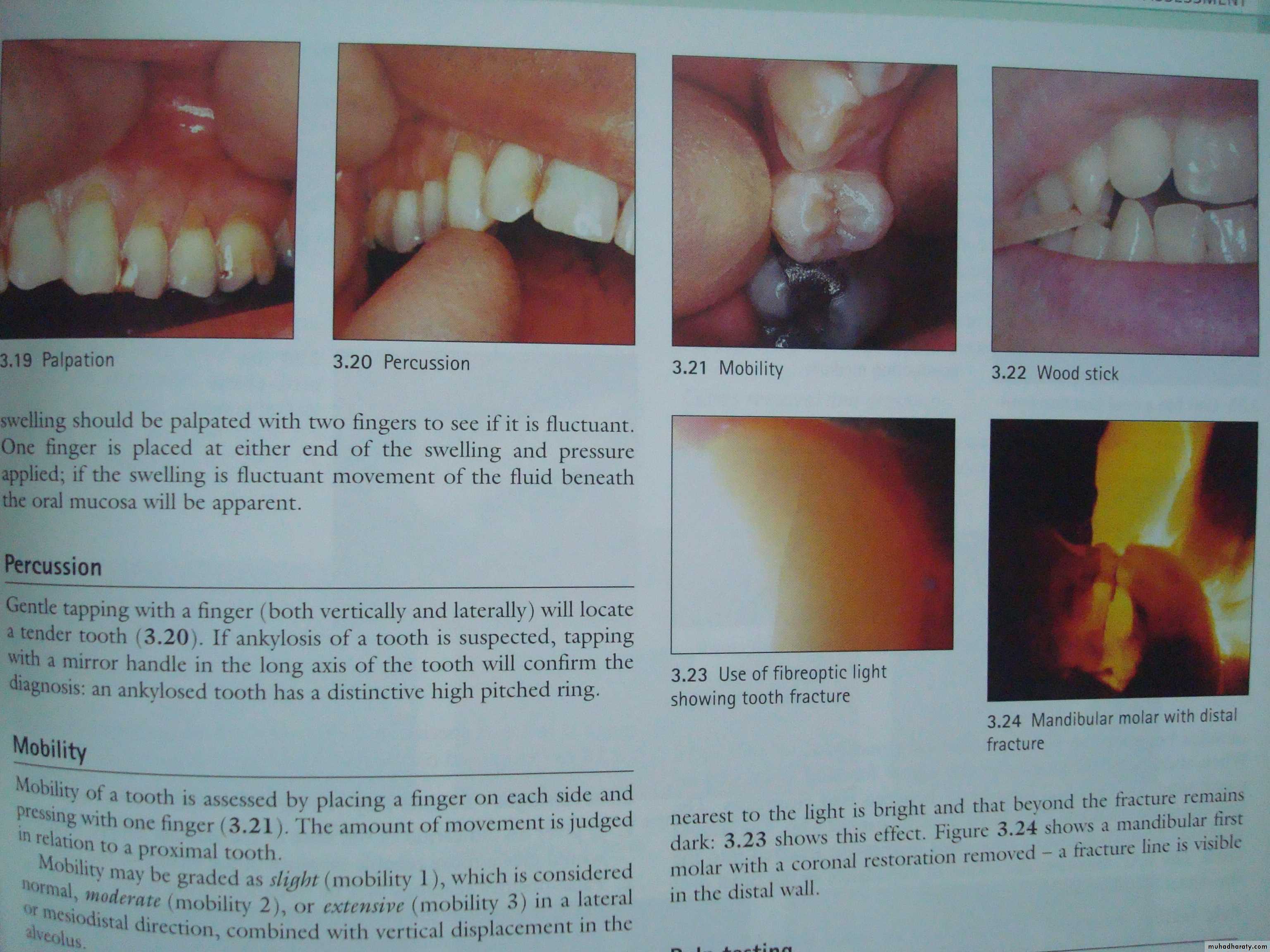
PERCUSSION
Before percussing instructions are to be given to the patient to raise his/ her hand in order to let the clinician know when and whether the tooth feels “TENDER”, “DIFFERENT” or painful on percussion.Before percussing the teeth the quadrant of the involved tooth is percussed using the index finger with quick blows of low intensity.
• The teeth should be tapped (with the index finger) in a random fashion so that the patient cannot “anticipate” when the tooth will be percussed
Percussion is done in both vertical and horizontal directions.
Change the sequence of percussion in successive tests to eliminate bias. Percussion must start gently then gradually increased.
Responses to percussion
Positive response is indicative of periodontitis (pericementitis) which could be due to:1-Teeth undergoing rapid orthodontic movement.
2-High spot in recent restorations.
3-Lateral periodontal abscess.
4-Partial/total Pulpal necrosis.
Negative response may be seen in cases of
1-Sound teeth
2-Chronic periapical inflammation
3-Acute pulpitis
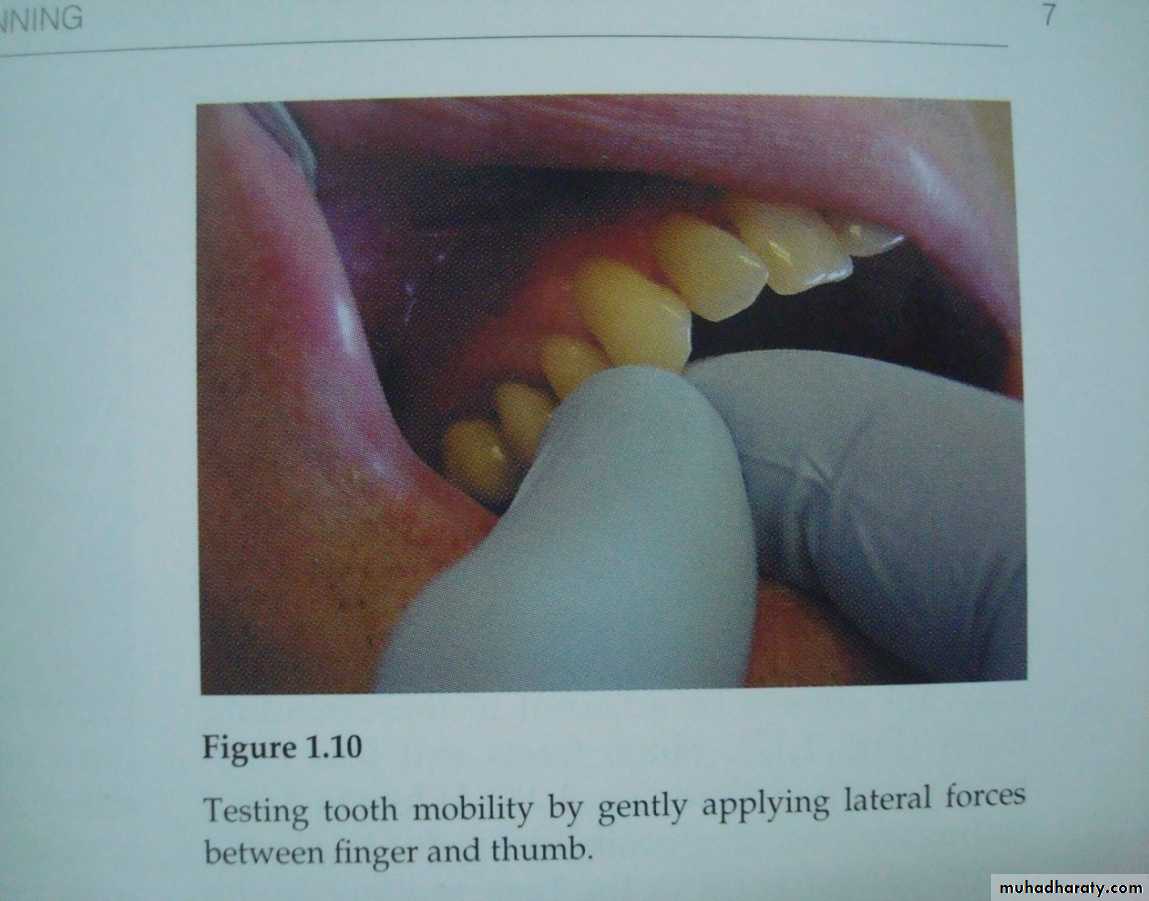
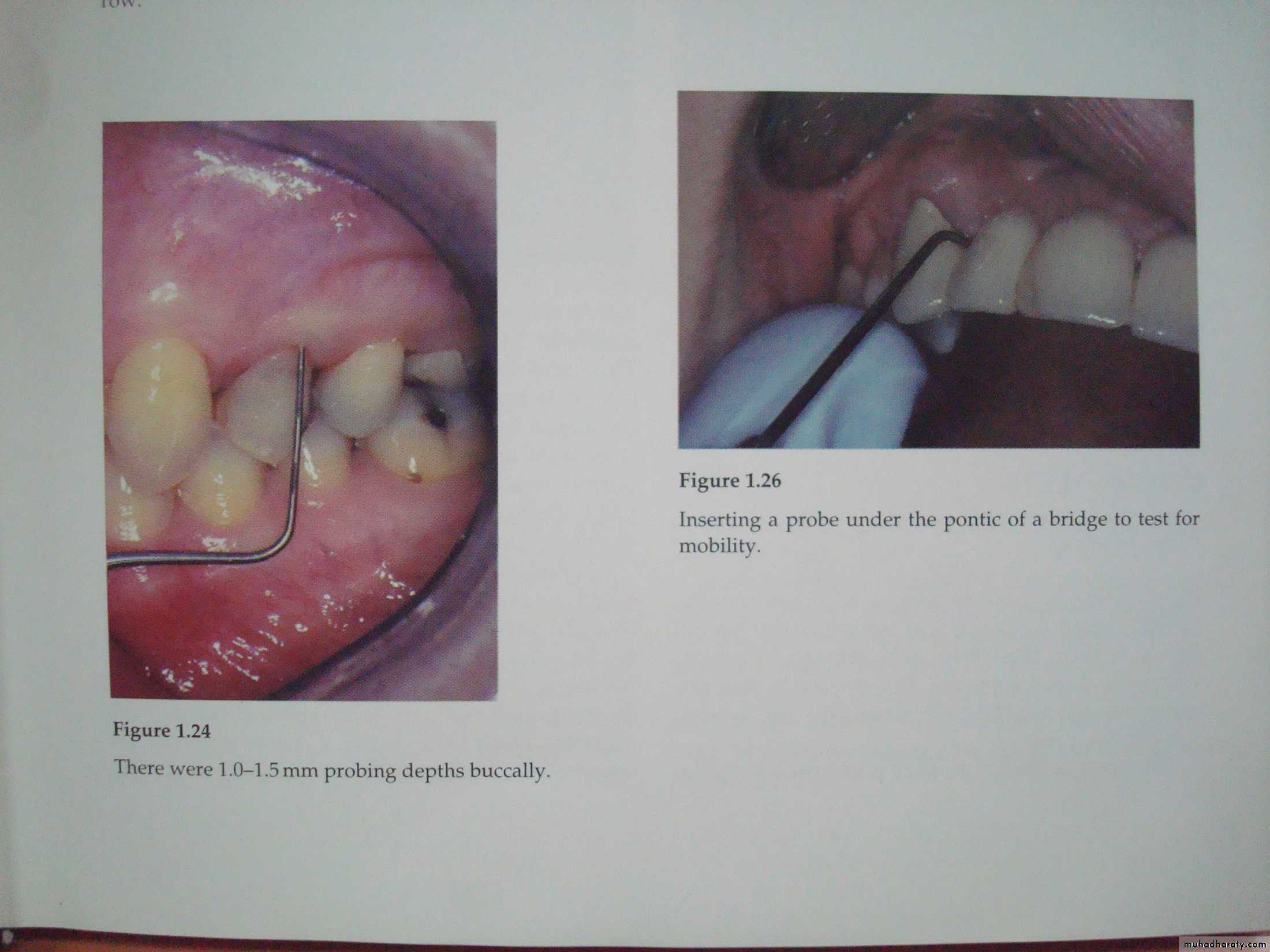
MOBILITY AND DEPRESSIBILITY TESTs
To evaluate the integrity of the attachment apparatus surrounding the tooth.Moving the involved tooth laterally in socket using handles of two instruments, using two index fingers is missleading.
The test for Depressibility is similar and is performed by applying pressure in an apical direction on the occlusal/incisal aspect of tooth and observing vertical movement if any.
Wrong
RightGRADES OF MOBILITY
0 - Non mobile/ mobility within physiologic limits.
1 - Mobility within range of 0-0.5mm.
2 - Mobility within range of 0.5-1.5mm with lateral movements.
3 - Mobility more than 1.5 mm with lateral movements and can be Intruded / depressed into the socket.
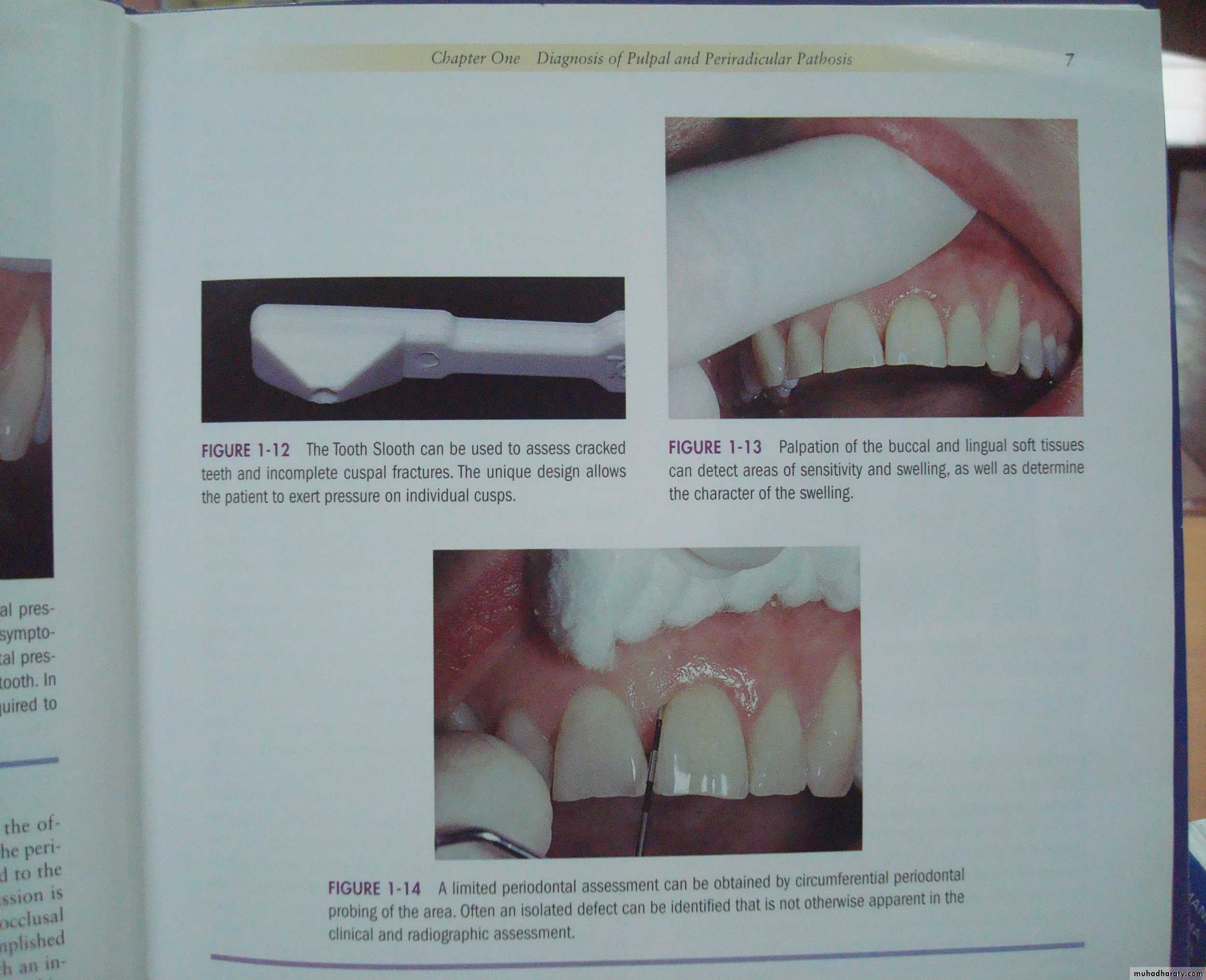
PERIODONTAL EXAMINATION
Periodontal examinationFurcation involvement.
A lateral canal - portal of entry for toxins- Pulpal degeneration.Thermal and electric pulp tests must be performed along with periodontal examination to distinguish between disease of Pulpal and Periodontal origin.
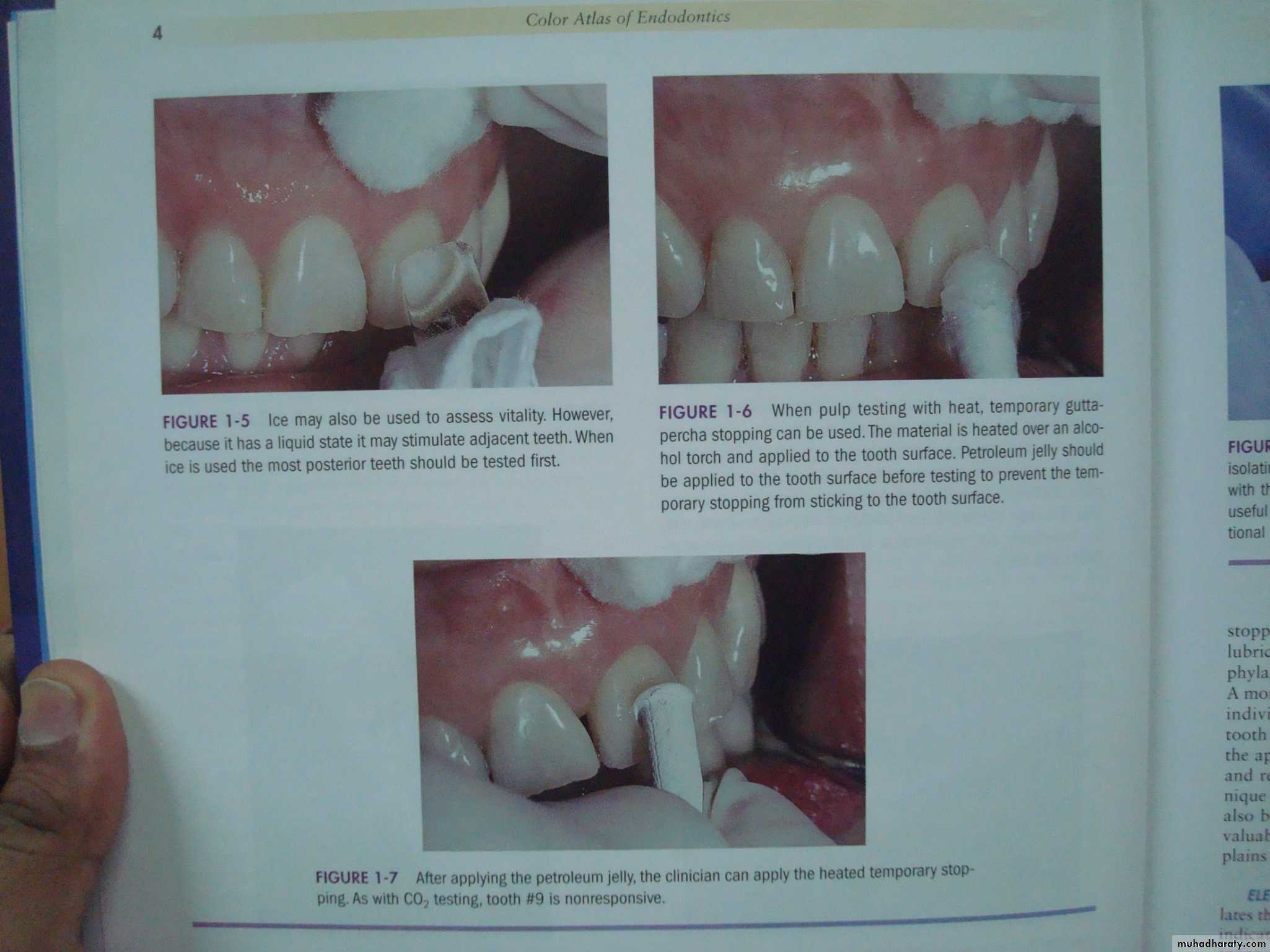
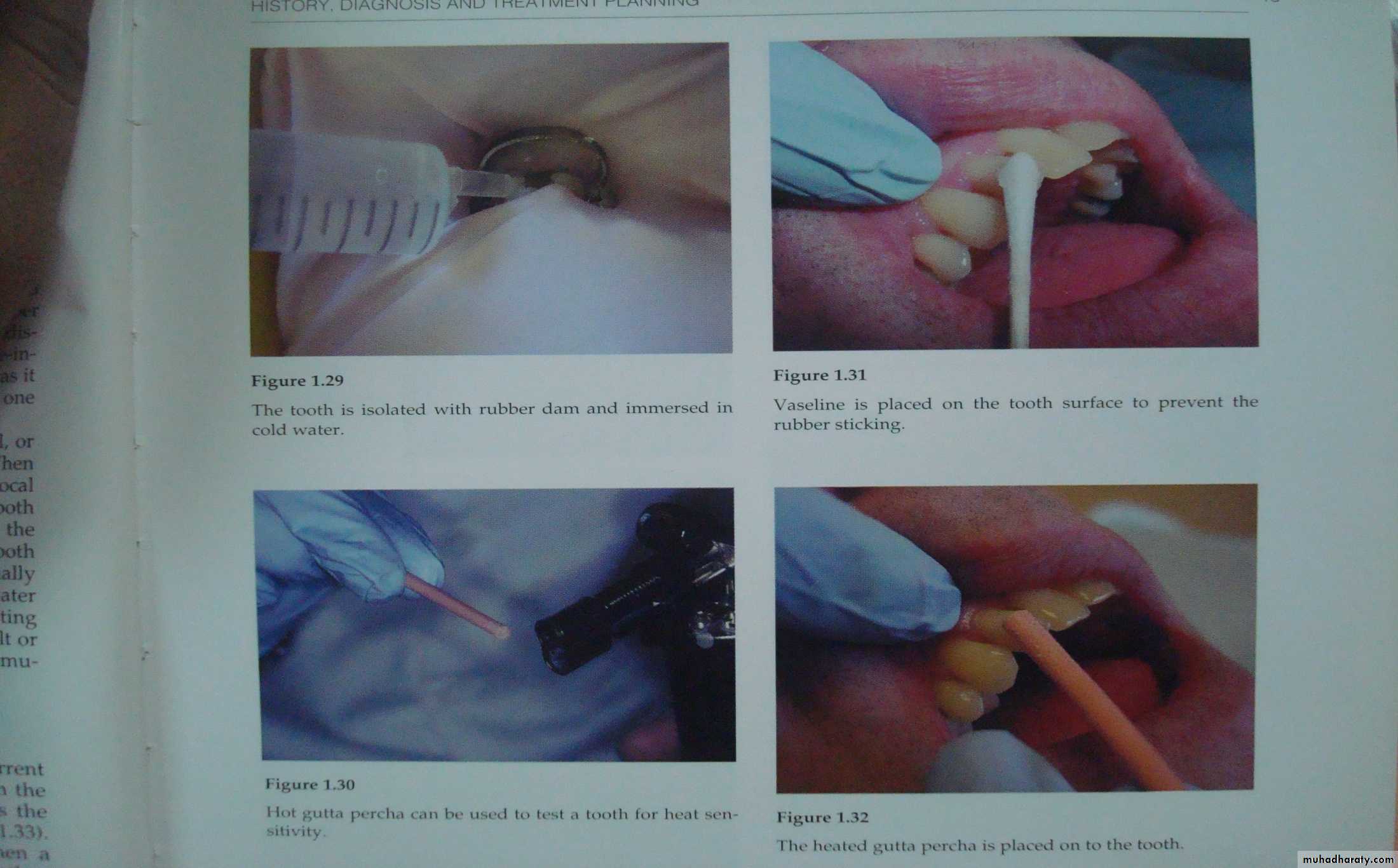
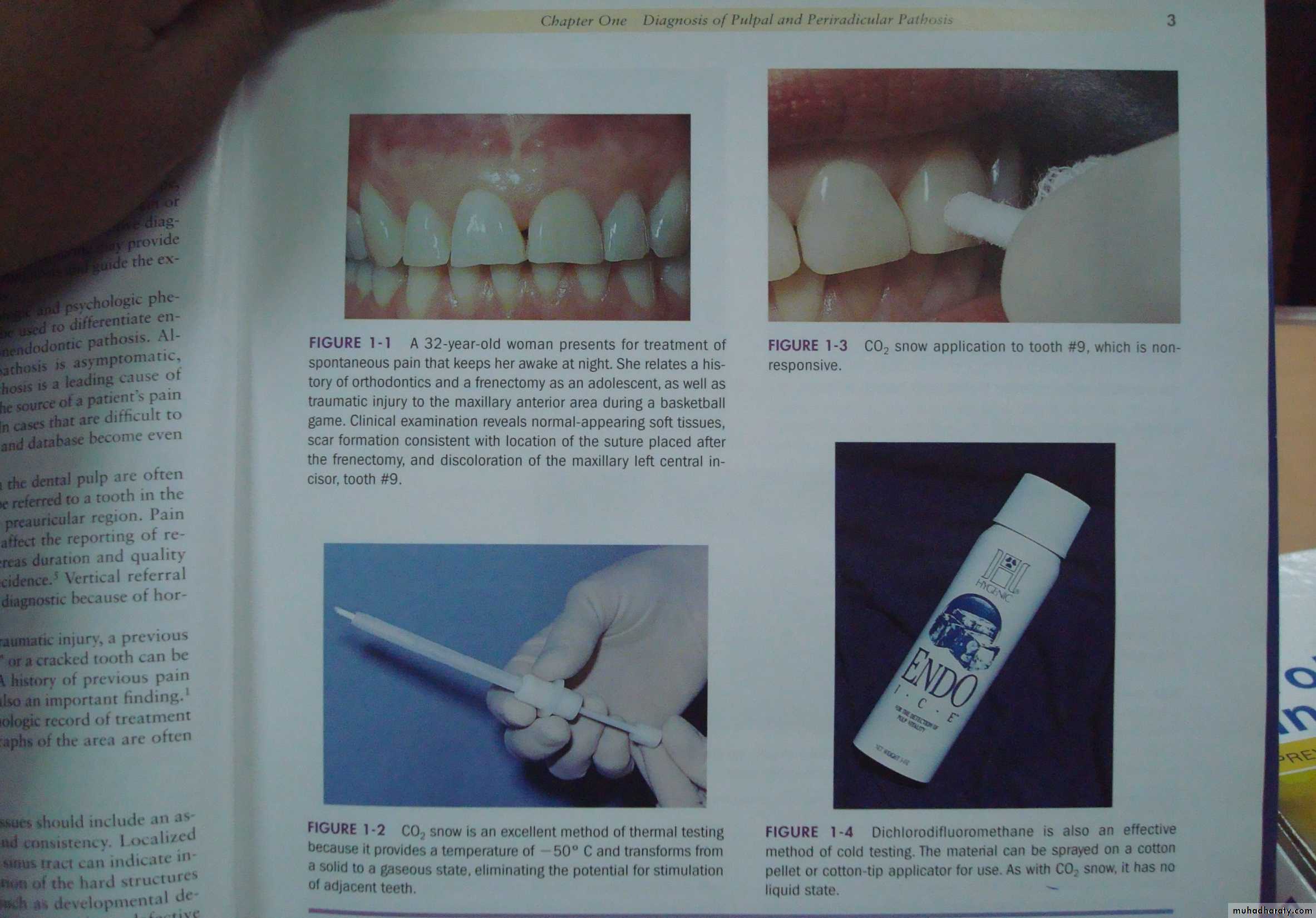
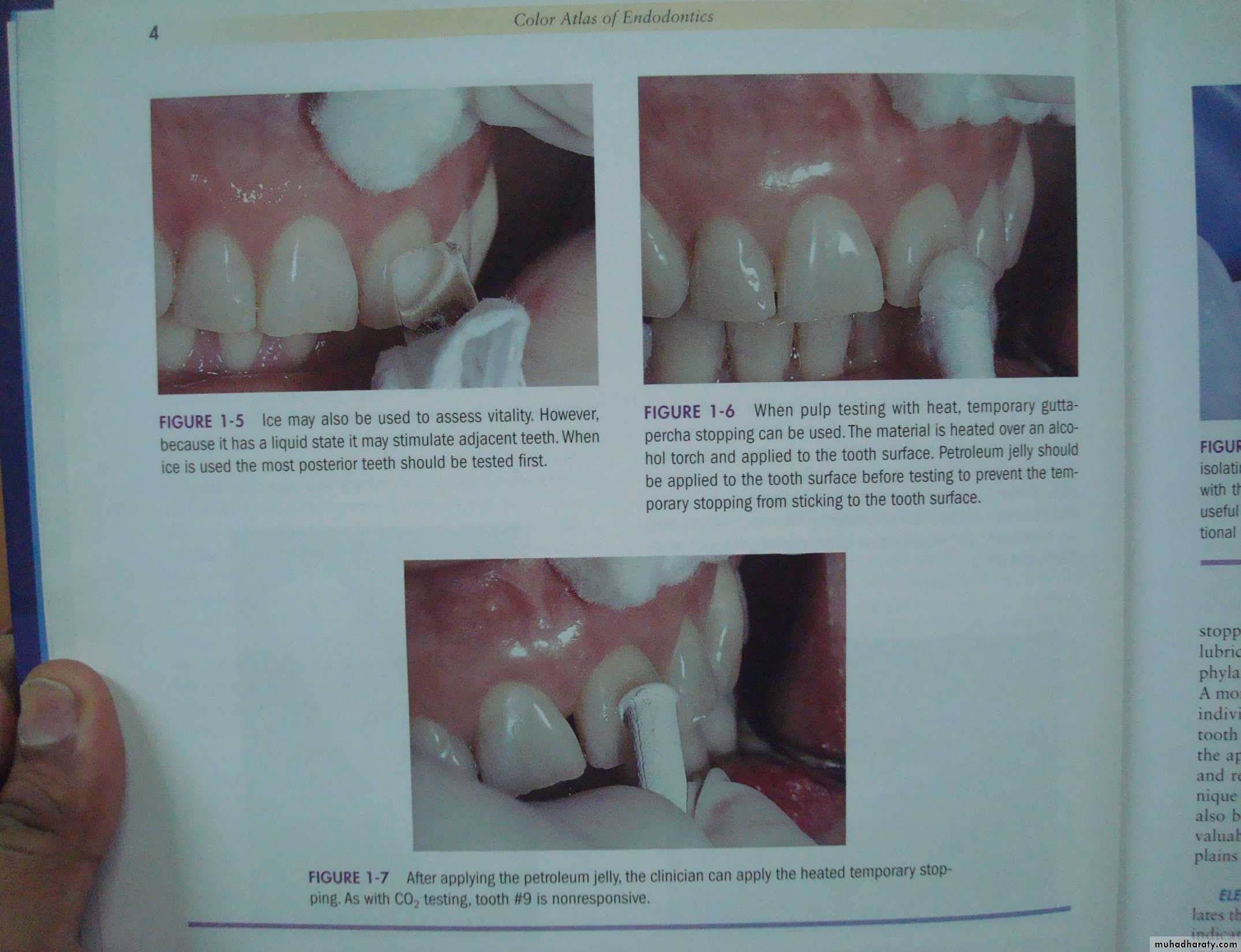
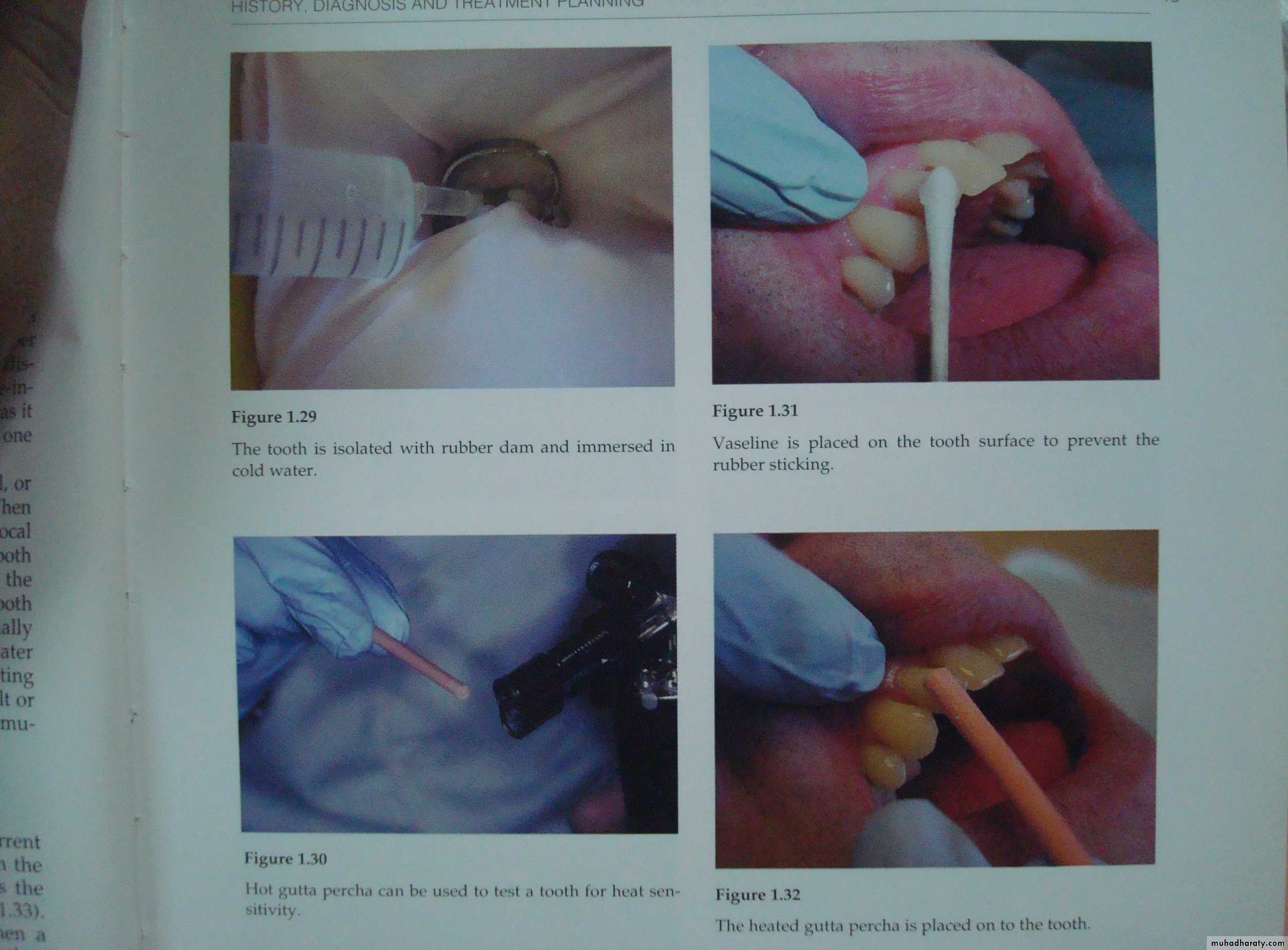
The heat test can be performed using different techniques such as:
1. Hot air 2. Hot water 3. A hot burnisher 4. Hot gutta-percha 5. Hot compound 6. Polishing of crown with a rubber cupThermal test
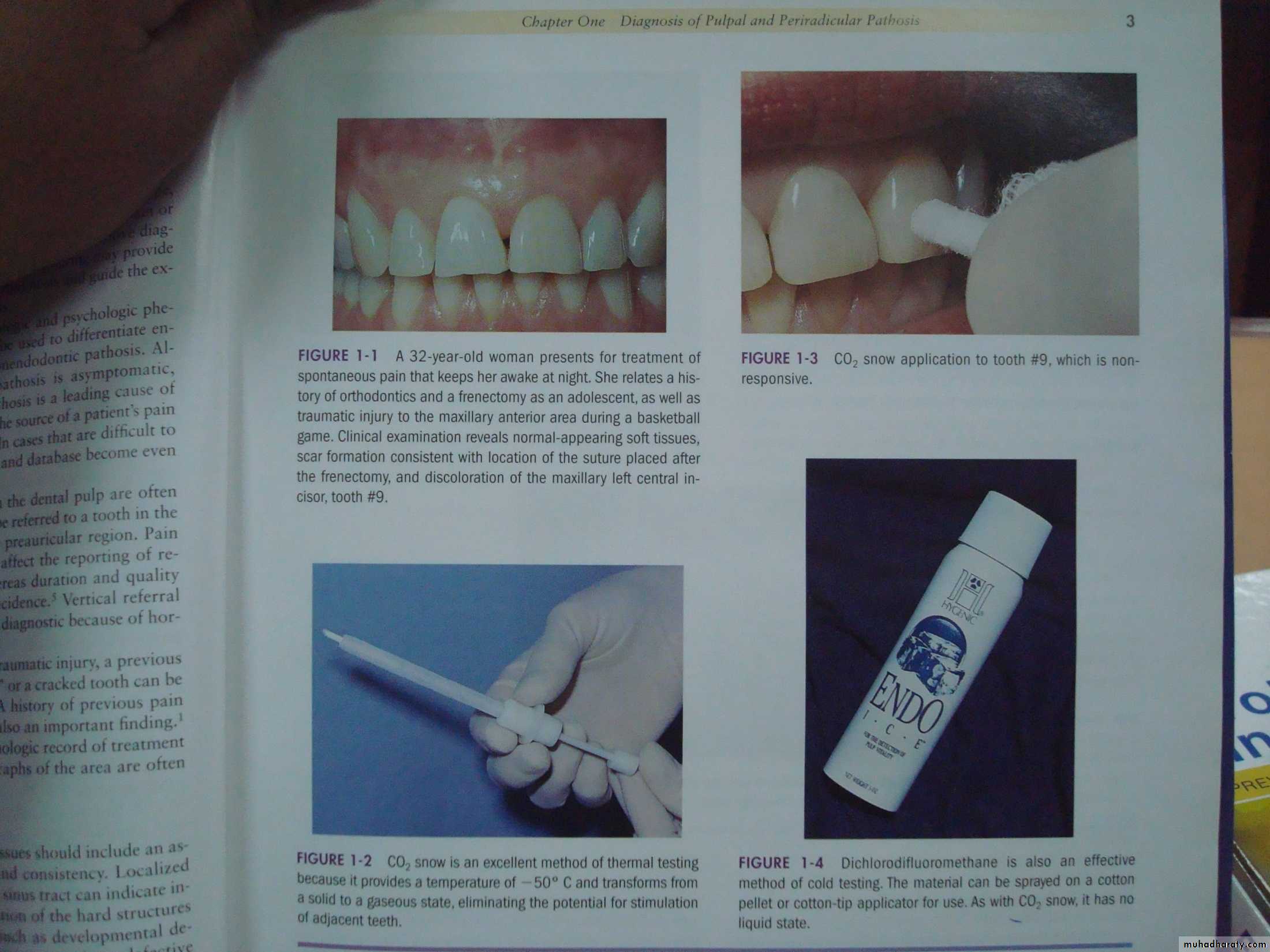
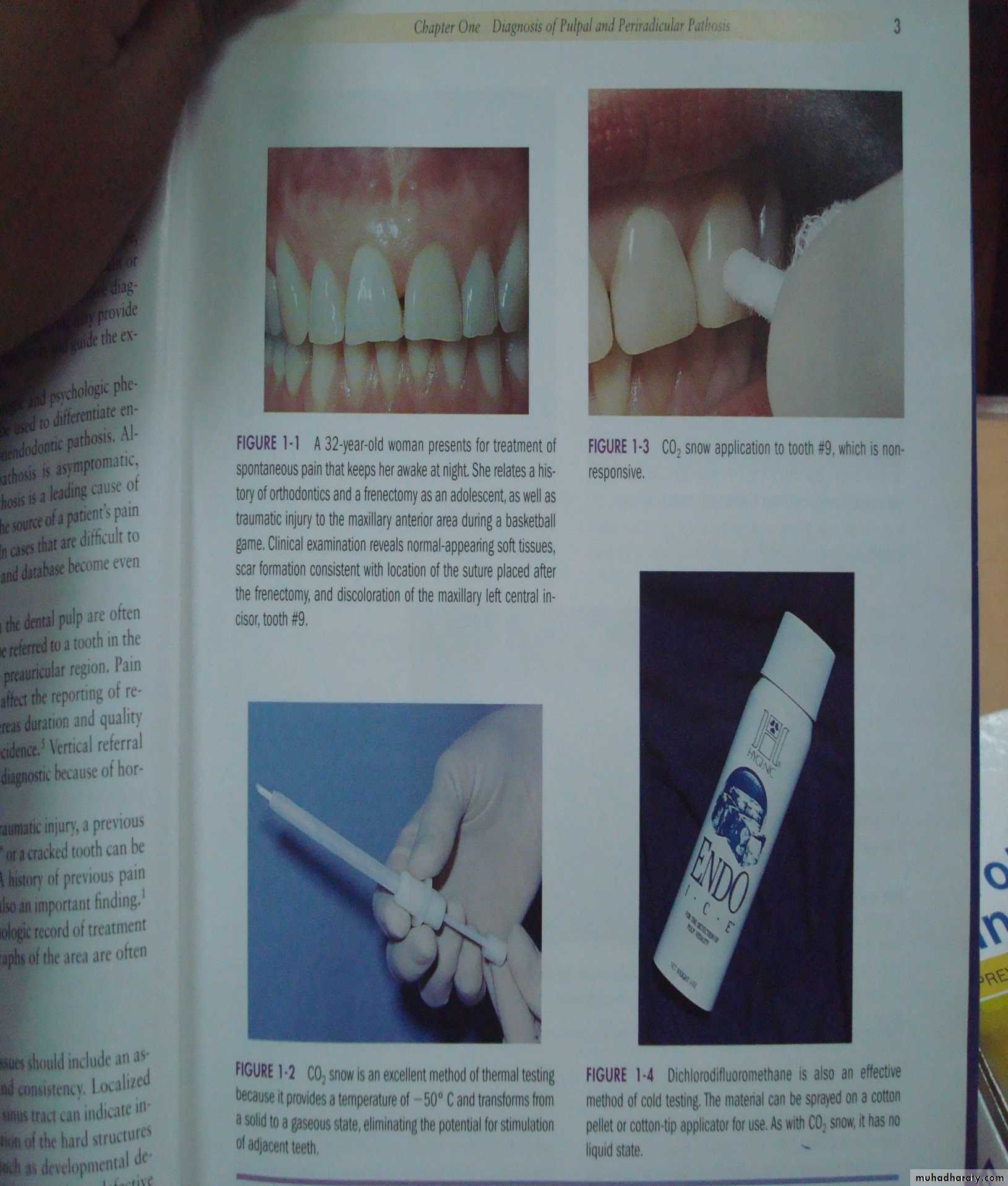
Cold TestIsolating the quadrant with the tooth to be tested.
1- Cold water
2 -cold air from a 3-way syringe directed against the crown of 3-previously dried tooth.
4- Use of ethyl chloride spray.
5- Ice Stick
6- CO2 snow
Correct placement
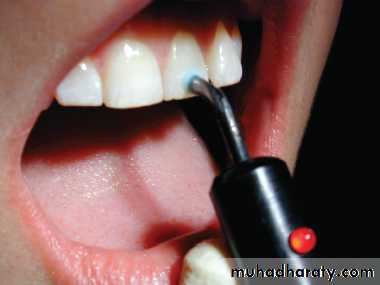
ELECTRIC PULP TESTING
Technique
Test should be first described to the patient .Teeth to be tested should be isolated with cotton rolls, saliva ejector and air dried.
Check the E.P. tester for proper functioning.Apply an electrolyte on the tooth surface tooth paste).
Avoid contact of the electrolyte or electrode with any restorations or the adjacent gingival tissue as this could lead to a false response.
Retract the patient’s cheek or lip with free hand, away from the tooth electrode.
Advantages of E.P.T
1-Intensity of stimulus is comfortable to the patients.2-The digital display of many E.P.Testers provide instant, easy and reliable information.
3-In some E.P. Testers, a red indicator light flashes on and off when maximum stimulus is reached.
4-Gives a quantitative reading and can be compared with the normal reading of control tooth.
Disadvantages of E.P.T.
1-Cannot be used on patients having cardiac pace maker.2-Some E.P.T equipments are very expensive.
3-E.P.T is not useful for recently erupted teeth with immature apex this may be because the relationship between the odontoblasts and the nerve fibers of the pulp has yet to develop.
4-Recently traumatized teeth cannot be tested.
5-No indication is given regarding state of the vascular supply which would give a more reliable measure of the vitality of the pulp.
6-Readings from posterior teeth with partially vital pulps may be misleading.
Misleading results
A. False Positive Responses: When the pulp is necrotic but patient gives a positive response.
B. False Negative Responses: When the pulp is vital, but the patient is unresponsive to the E.P.T.
Reasons for False Positive Response:
1-Conductor / electrode in contact with a metallic restoration or gingiva along with the current to reach the attachment apparatus.2-Patient anxiety.
3-Liquefaction necrosis-This may conduct the current to the attachment apparatus and the patient may slowly raise his hand near the highest range.
4-Failure to isolate or dry the teeth
5-In multi-rooted teeth where the pulp may be partially necrotic.
Tests which determine vascularity of pulp
Reasons for a False Negative Response:1- Patient heavily pre-medicated with analgesics, narcotics, alcohol, tranquilizers.
2- Inadequate contact with enamel.
3- Recently traumatized tooth.
4- Excessive calcification in the canal.
5- Recently erupted tooth with an immature apex.
The results obtained / tabulated through the E.P. T conducted should not be thoroughly relied upon. These results should be co-related with those obtained with other vitality tests such as the thermal tests etc.
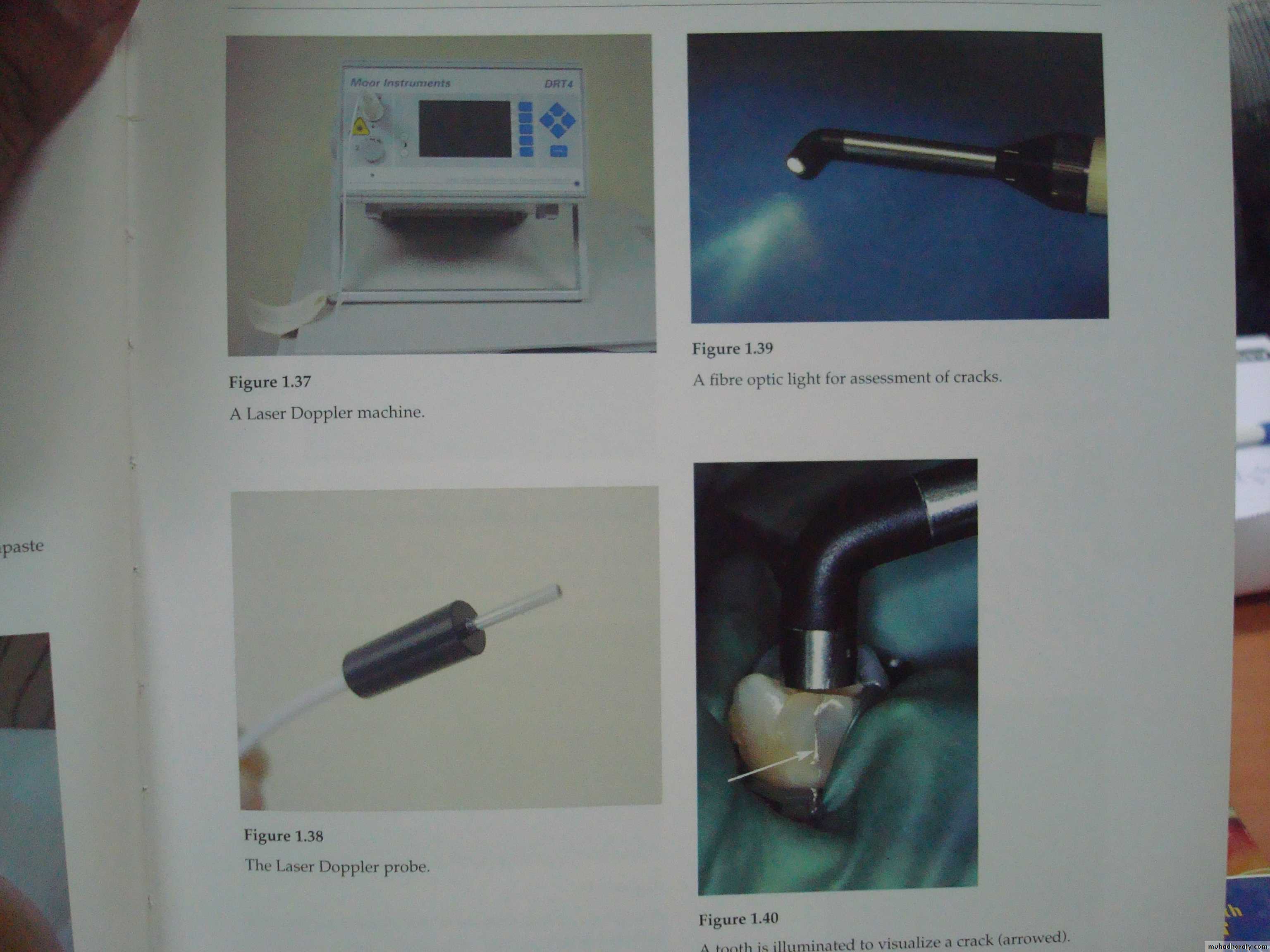
1- Laser Doppler flowmetery
2- Pulse Oximetery
Anesthetic Test
1- Restricted to patients who are in pain at the time of the test and when the usual tests have failed to help identify or localize the offending tooth.
2- The objective is to anesthetize a single tooth at a time until the pain disappears and is localized to specific tooth.
3- If the source of pain cannot be differentiated ie. ,maxillary / mandibular, then mandibular block is implemented.
4- further localization of the affected tooth is done by an intraligamentary injection.
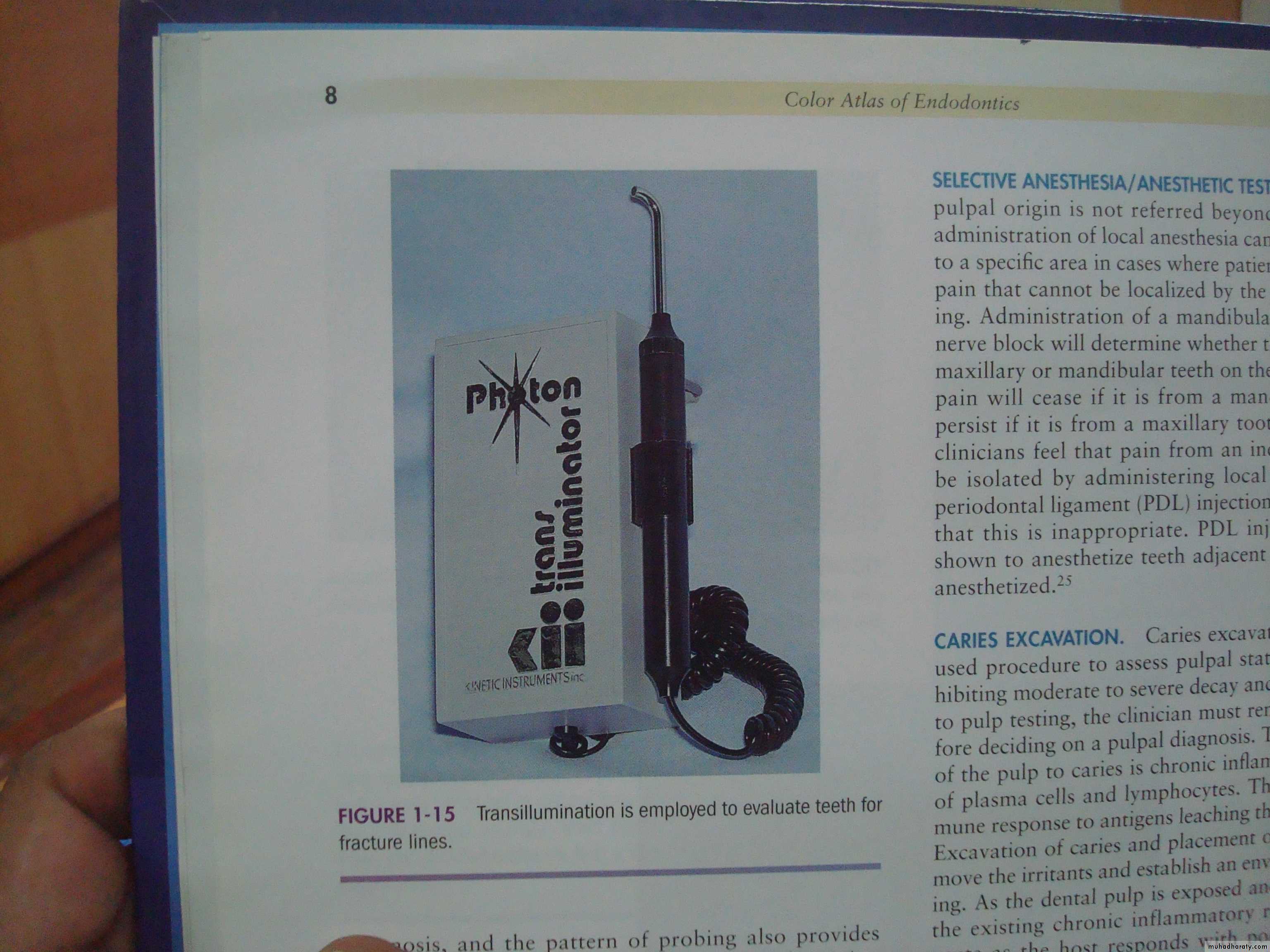
Transillumination Test
Technique
1-Light from a fiberoptic is applied from the buccal surface to illuminate the tooth to detect the fractured lines when present2-From the contact area to detect contact caries.
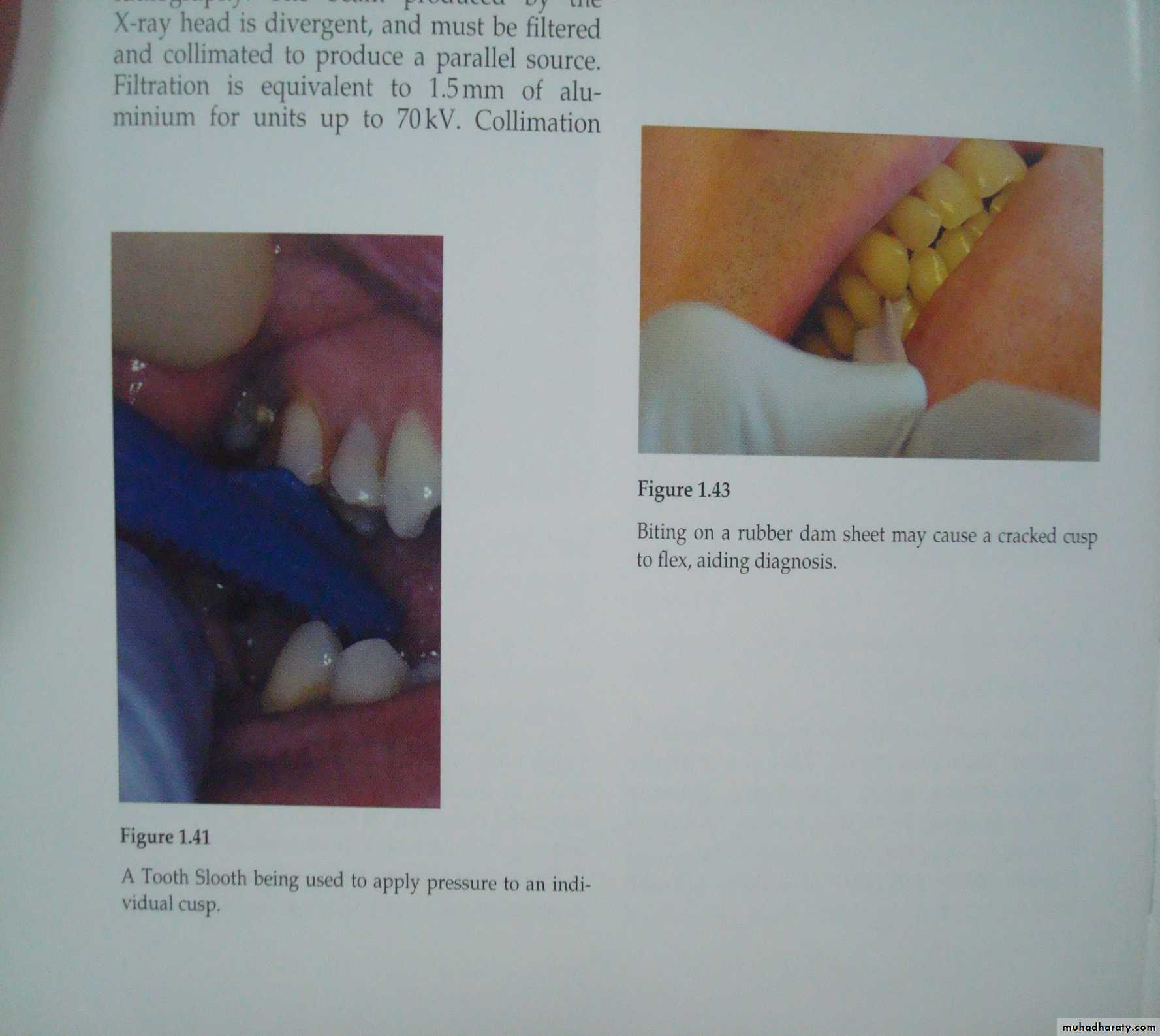
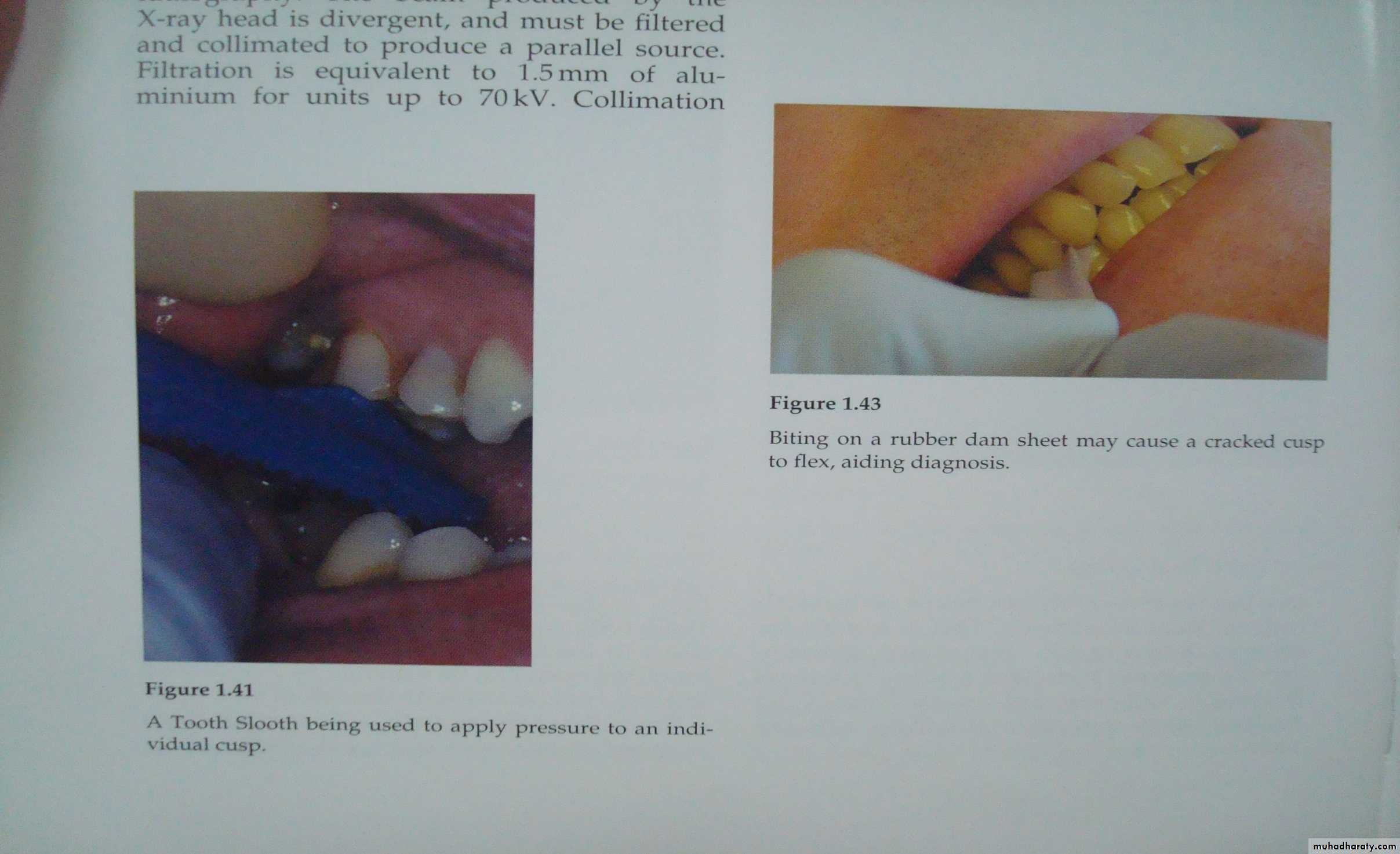
BITING TEST
An orangewood stick is placed on the occlusal/incisal aspect (on each cusp in case of posteriors) of the tooth and the patient is asked to bite.
To identify the fractured tooth /cracked tooth syndrome.
STAINING
Remove the filling from the suspected tooth and place 2% Iodine in the cavity preparation. The iodine stains the:1-Fracture line dark.
2-Canal orifice
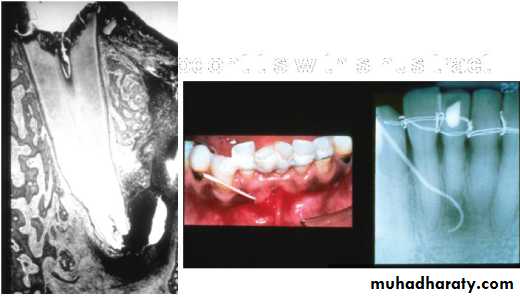
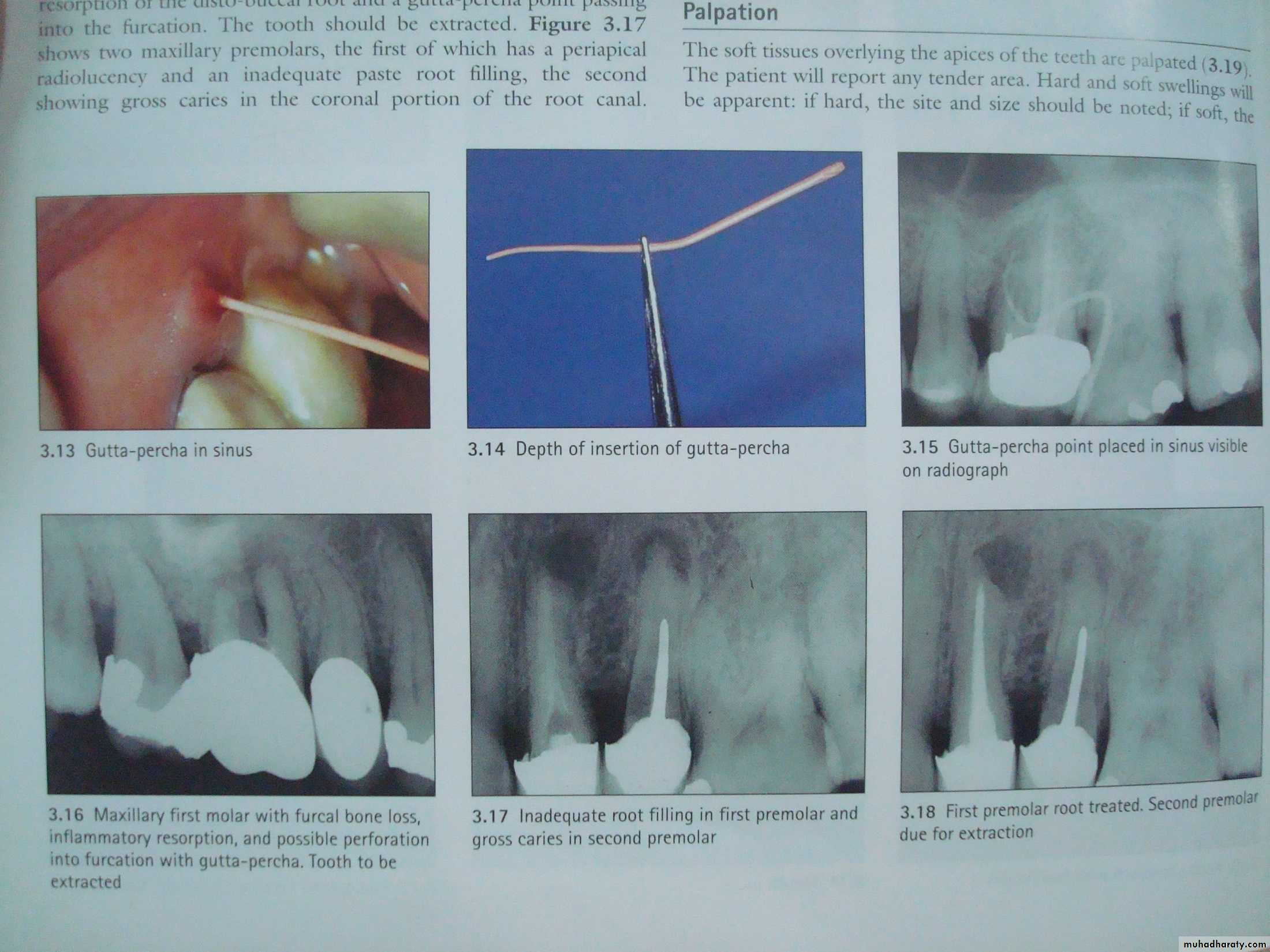
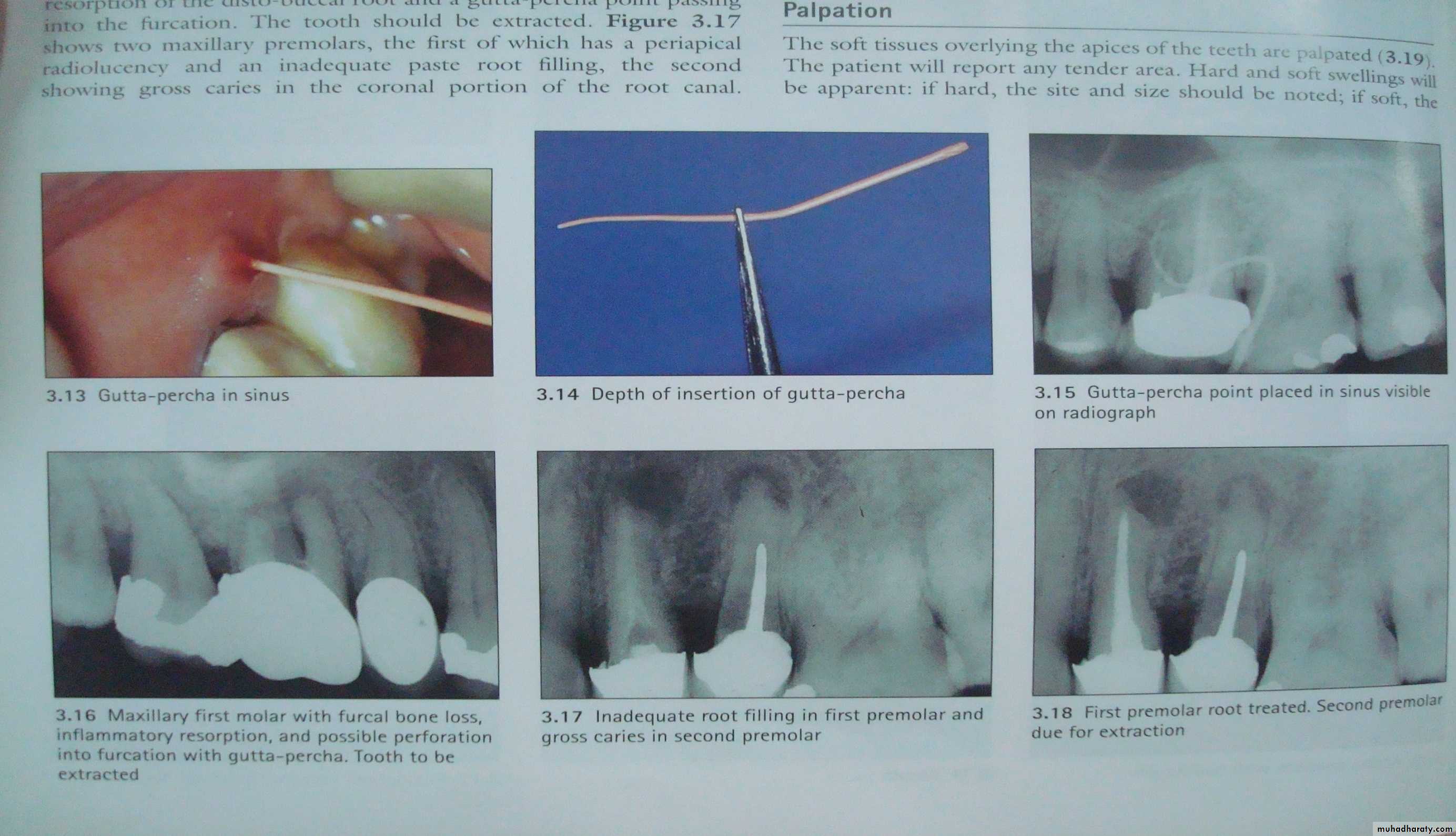
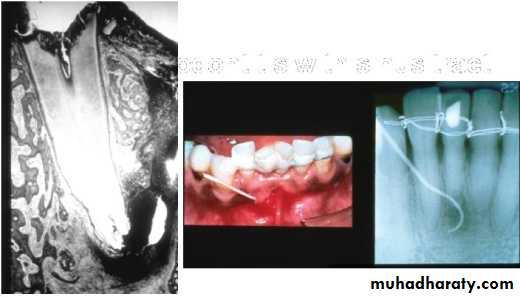
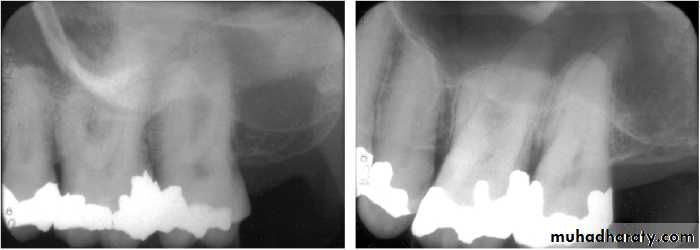
Gutta Percha POINT TRACING
Can localize the endodontic lesion to the specific tooth.Aids in the differential diagnosis between a periodontal and an endodontic lesion.
Placing a gutta percha point through the sinus/fistula tract and take a radiograph.
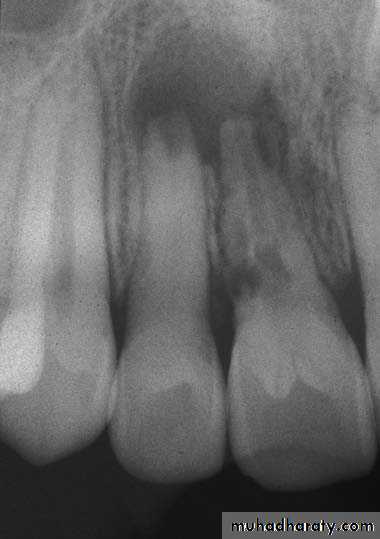
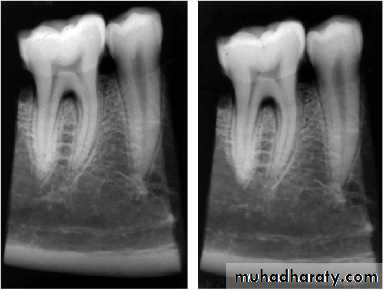
Radiographs IMPORTANCE
Provides information on the extent of caries in to the pulpNo. of root canals and accessories
The course & shape of the canals
Length of the root
CalcificationsResorptions
PDL status8. Nature of periapical area & alveolar bone
9. Root fractures10. Differentiation of pathosis
11. Location of perforations12. Post obturation evaluation
13. Evaluate healing after RCT
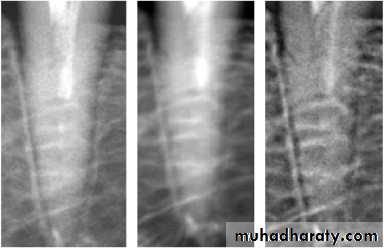
14. Medico legal recordsLimitations1-2 D image of 3D object
• State of pulpal health can not be ascertained
• P/A pathology is evident only after much destruction(33%)• Vertical root fracture can not be diagnosed
• Bony trabculae misinterpreted for horizontal root #
• Extend of caries is usually less than the actual extent as is true for P/A pathology
•
Anatomic structure can mimic P.A. pathology
Anatomic noise
Other radiographic methods
• Xeroradiography• Radiovisiography (RVG)
• Cone beam computerized tomography (CBCT)
• Magnetic Resonance Imaging (MRI)
• Ultrasound imaging