Fifth stage
DermatologyLec. 4
د. منار
17/11/2016
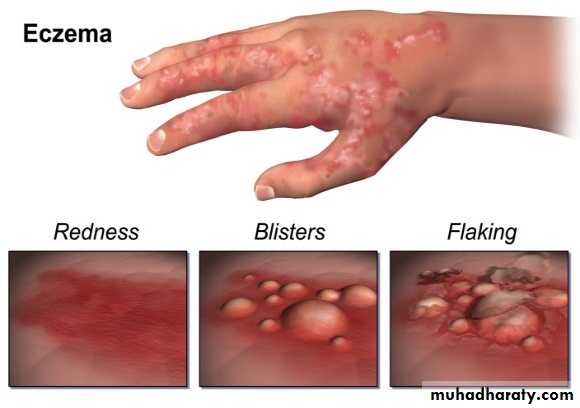
Eczema (Dermatitis)Eczema
Is the most common inflammatory skin disease, the characteristic components of eczematous inflammation are:Erythema
Scale
Vesicle
Stages of Eczematous Inflammation
There are three stages of eczema subacute, acute, and chronic.Stage
Symptoms
Primary and secondary
Treatment
Acute
Intense itch
Vesicles, blisters, intense rednessCold, wet compresses,
Oral or topical steroids,
Antihistamines, ±antibiotics
Subacute
Slight to moderate itch, pain, burningRedness, scaling, fissuring
Topical steroids with or without occlusion, lubrication, antihistamines, ± antibioticsChronic
Moderate to intense itch
Thickened skin, skin lines
accentuated (lichenified
skin), excoriations, fissuring
Topical steroids (with occlusion for best results), Antihistamines, antibiotics,
lubrication
Acute eczematous inflammation, numerous vesicles on an erythematous base
Subacute and chronic eczematous inflammation, the skin is dry, red, scaling, and thickened
Subacute eczema, Erythema and scaling are present, the surface is dry, and the borders are indistinct.Chronic eczematous inflammation, accentuated skin lines differentiate this process from psoriasis.
Classification
The classification of eczematous dermatosis is based on aetiologyExogenous
Endogenous
Exogenous
ExogenousEndogenous
Endogenous
Atopic dermatitis
Seborrheic dermtitis
Discoid eczema
Asteatotic eczema
Gravitational dermatitis
Pompholyx
Lichen simplex
Atopic dermatitis
Seborrheic dermtitis
Discoid eczema
Asteatotic eczema
Gravitational dermatitis
Pompholyx
Lichen simplex
Contact dermatitis
Irritant
Allergic
Infective dermatitis
Photodermatitis
Radiodermatitis
Contact dermatitis
Irritant
Allergic
Infective dermatitis
Photodermatitis
Radiodermatitis
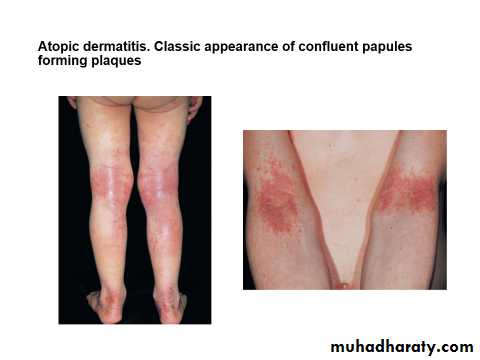
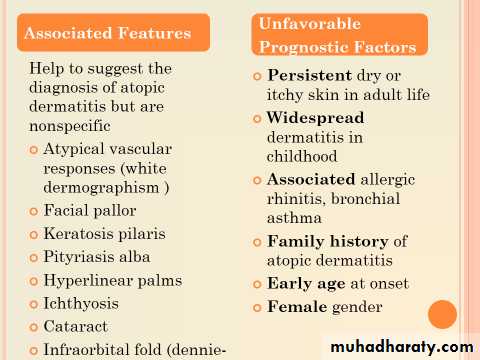
Atopic Dermatitis
The term atopy was introduced years ago to designate a group of patients who had a personal or family history of one or more of the following diseases: hay fever, asthma, very dry skin, and eczema.Atopic dermatitis (AD) is a chronic, pruritic inflammatory skin disease that occurs most frequently in children, but also affects many adults.
AD is often associated with elevated serum immunoglobulin E (IgE) levels and a personal or family history of type I allergies, allergic rhinitis, and asthma.
Prevalence
Approximately 15% to 30% of children and 2% to 10% of adults are affected.
About 45% of cases of atopic dermatitis begin within the first 6 months of life, 60% begin during the first year, and 85% begin before 5 years of age.
Up to 70% of children have a remission before adolescence.
Atopic dermatitis can start in adults.Pathogenesis and Immunology
Increase serum IgE evel
Increase histamine level in blood and skin
Increase blood esinophiles
Decrease cell mediated immunity; Patients may develop severe diffuse cutaneous infection with the herpes simplex virus (eczema herpeticum) whether or not their dermatitis is active.
Decrease neutrophil and monocyte chemotaxis
Increase susceptibility to viral and fungal infection, staphylococcal colony may be high and bacterial infection may supervene.
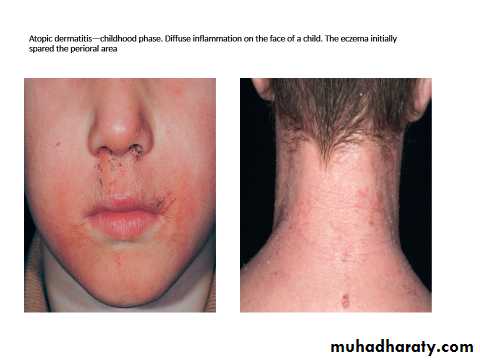
The disease characteristics vary with age:
Infants :Facial and patchy or generalized body eczema, with extensor predilection
Adolescents and adults :
Have eczema in flexural areas and on the hands.
The pattern of inheritance is polygenic.
Phases of Atopic Dermatitis
Infantile phase (3months – 2 years):
Face , forehead, scalp , extensor side of the
Cheek first place
Diaper freq spared
limbs
Itchy dry skin +/- bacterial infection
Usually progress to childhood stage but may resolve in the age of 1- 1.5 yrs.
Childhood Phase (2 to 12 Years):
Inflammation in flexural areas (i.e., the antecubital fossae, neck, wrists, and ankles)Perspiration stimulates burning and intense itching and initiates the itch-scratch cycle.
Tight clothing that traps heat about the neck or extremities further aggravates the problem.
The eruption begins with papules that rapidly coalesce into plaques, which become lichenified when scratched.
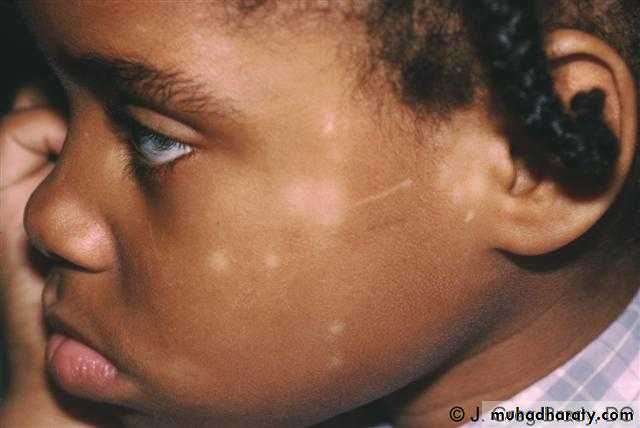
Constant scratching may lead to destruction of melanocytes, resulting in areas of hypopigmentation
If they have been vigorously scratched, they may be bright red and scaling with erosions.
The border may be sharp and well-defined, as it is in psoriasis, or poorly defined with papules extraneous to the lichenified areas.
Hypopigmentation in the antecubital fossae caused by destruction of melanocytes by chronic scratching.
Hypopigmentation in the antecubital fossae caused by destruction of melanocytes by chronic scratching.
Adult Phase (12 Years to Adult)
As in the childhood phase, localized inflammation with lichenificationMostly in flexural areas.
Adults may have no history of dermatitis in earlier years, but this is unusual.
‘
Complications:
Bactereal infections eg. Staoh. aureus infection.
Severe viral infections eg. Herpes simplex infection (eczema herpeticum), widespread infection with the herpes simplex
Poor growth
Local & systemic side effect of steroids
Negative psychological effects
Eczema herpeticum
Differential diagnosis
Scabies
Seborrheic dermatitis
Contact dermatitis (irritant or allergic)
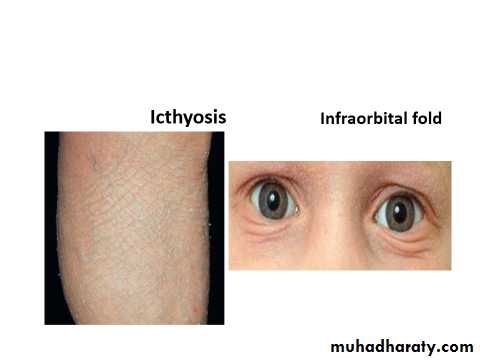
Ichthyosis
Cutaneous T-cell lymphoma
Psoriasis
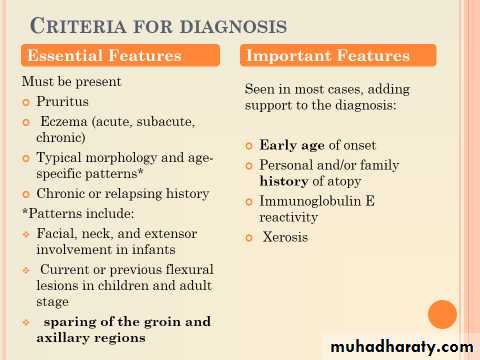
Diagnosis
Diagnosis based on the clinical features (essential, important, associated)Treatment
We have to deal with the psychological impact on the patient and his family , by discussing and reassurance.Avoid triggering factor.
Treat the existing lesions.
Prevention
Avoid wool.
Use 100% cotton.
Use soaps only in axilla, groin, and feet.
Avoid perfumes or makeup that burns or itches.
Do not scratch.
Apply soothing lubricants.
Maintain cool, stable temperatures.
Do not overdress.
Avoid sweating.
Humidify the house in winter.
Avoid cigarettes.
Minimize animal dander—no cats, dogs, rodents, or birds.
Control emotional stress
Diet control is a controversial treatment method
Treatment
Topical steroid with different potency strong on dry chronic lesionSystemic steroid For generalized sever cases
For itching Sedative antihistamine
For infection Antibiotic
Continuously using Vaseline to the skin
Others Tacrolimus, tar, phototherapy
Other Type of Endogenous Eczema
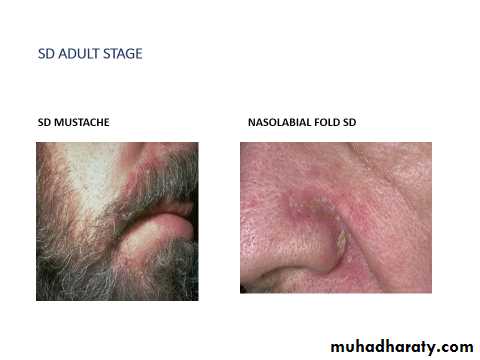
Seborrhic DermatitisA chronic superficial inflammation
Common affect 3-5% of population
On hairy region (pilosebaceous unit)
Affect infant up to third months and after puberty (two phases only).
Etiology:
Androgen increase sebum releaseAlso over active normal flora (pityriosporum ovale) which increase activity in seborrhic area.
Clinical feature
Erythematous patch or plaque covered by greasy yellowish scale, indistinct margin, hair loss uncommon.Most common on scalp, eyebrow, face, mustache, nasolabial folds.
Also central chest (presternal area), axillae and groin.
Itchy lesion
In infant it cover the scalp known as cradle cap
Napkin area is often affected which differ from?
But it spread beyond the area covered by napkin ( not as in contact dermatitis )
Acute onset or wide spread exacerbation of seborrhic dermatitis is commonly seen in HIV infection.
Differential Diagnosis
Psoriasis vulgaris.Dermatophytosis (tinea capitis, tinea faciale, tinea corporis),
Candidiasis (intertriginous).
Tinea amiantacea.
Contact dermatitis
Diagnosis: clinical
TreatmentGeneral measures:
Regular bathing.
Avoid irritant & oily applications.
Topical therapy:
Scalp shampoos containing 2 % ketoconazole,
Ketoconazole or any antifungal cream for the face and body.
Corticosteroids for more severe cases;
Hydrocortisone or low-potency corticosteroid solution, lotion, or gel (for scalp)1 % or 2.5% hydrocortisone cream for other sites.
*The main treatment of seborrhoeic eczema of scalp in infancy is emollients.
Nummular (Discoid eczema)A chronic, intensely pruritic, coin-shaped erythematous scaly plaques
During winter months;
Often seen in atopic individuals.
Age: two peaks in incidence: young adults and old age.
Plaques may be :
Exudative and crust (Wet type).
Or dry scaly (Dry type).
Distribution: lower legs, trunk, hands and fingers or generalized
Pathophysiology: unknownDifferential diagnosis:
Psoriasis
Tinea corporis
Herald patch of pityriasis rosea
Diagnosis: clinical, biopsy shows eczema
Treatment:Avoid irritant as soap, wool
Emollient as vasaline
Medium potency topical steroid
If superadded infection so topical and even systemic antibiotic if wide spread
If itching antihistamine
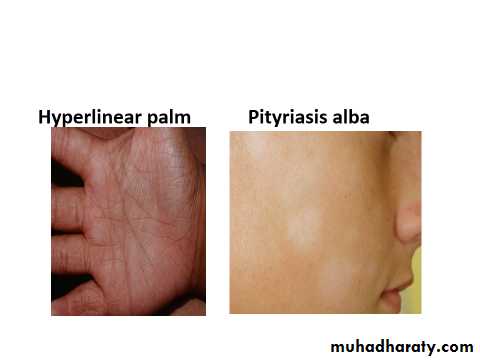
Pityriasis Alba
Thought to be photoallergyAppear on exposed parts
On children and adolescents
Self-limiting
Reassure the family with mild topical steroid, and sun avoidance
Asteatotic Dermatitis
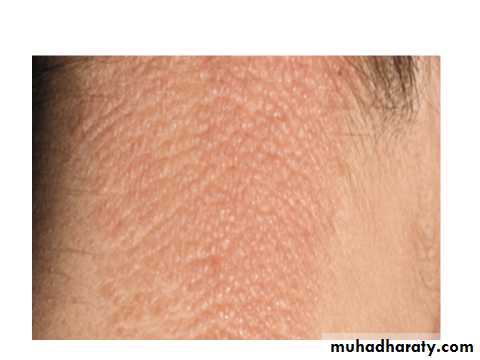
Eczematous lesion that occurs in the winter and in old persons
On the legs, arms, and hands but also may be on the trunk.
Itchy, erythematous scaling dry, “cracked,” fissured skin.
Very often the eruption results from too frequent bathing ,frequent washing with soap , especially in winter when the humidity is low, also in patient taking diuretics
Treatment
Avoid over-bathing with soap
Avoid soap and irritant wool
Emollient vaseline twice daily
Steroid may be used
Gravitational eczema
Previously misnamed as stasis or varicosity dermatitis (thought to be due to stasis, but there is NO stasis.Due to Increased hydrostatic ( venous ) pressure and capillary damage with GOOD blood supply , especially seen on the leg
Due to faulty valve and increase capillary pressure with widening of the epithelial pores
Lead to:
Extravasated fluids lead to edemaAnd RBCs lead to hemosiderosis , brownish black discoloration
Fibrinogen which will converted into fibrin lead to vasoconstriction that cause bad nutrition , so any truma may lead to persistant leg ulcer
Most common site is proximal to the medial malleolus
As an itchy ill-defined, erythematous patches with fine scaling, sometimes with excoriations, on lower legs, especially around varicosities.
Complications:
Contact dermatitis from medicationInfection
Ulcer
Inverted champagne bottle look to the leg may result from prolong disease ulceration and fibrosis.
Treatment:
Leg elevationWeight reduction
Topical steroid
Treatment of secondary bacterial infection (avoid topical neomycin because it cause sensitization)
Pomphylox
Lesions: very itchy deep seated tiny vesicles along the sides of the fingers, palms, sides, toes, and soles. May coalesce and become bullae, which weep and become painful dry, hyperkeratotic and fissured.Age: Majority under 40 years (range 12 to 40 years).
Sex: Equal ratio.
Associations: It is more common in atopic
Treatment: with potent topical steroid under cover, Antihistamine
Lichen Simplex Chonicus (Neurodermatitis)
Definition: A pruritic eczematous condition resulting from habitual continued rubbing and scratching at a localized area of the skin, associated with a period of anxiety.Age: Over 20 years.
Sex: More frequent in women.
Lesion: Characteristicly itchy lichenified plaque, well defined, unilateral flesh coloured, pink or hyper pigmented.
Pruritus, often in paroxysms and it becomes a pleasure to scratch.
Often the rubbing becomes reflexive and a subconscious habit.
Lightly stroking the involved skin with a cotton swab generates a strong desire to scratch the skin
The constant scratching leads to a vicious cycle of: scratch → release histamine → itch → scratching
Distribution: especially: back of neck (female), just below elbow, back of hand, genitalia, buttock, and lower leg.
Diagnosis: clinical, biopsy - rarely required, shows eczema.
Differential diagnosis: hypertrophic lichen planus.
Treatment:
Relive anxietyStop scratching??
Super potent topical steroids under occlusion