1 |
P a g e
Ulcers
A) Inspection:
we should note
1) Size and shape of the ulcer (using a tape measure)
2) Number (single or multiple)
3) Location of the ulcer:
• Varicose ulcer → medial aspect of lower third of the leg
• Rodent ulcer → nose
• Tuberculous ulcer → neck
• Trophic ulcer → weight-bearing area (e.g. heel of the feet)
• Bedsore ulcer→ sacrum
• Ischemic dorsum of foot and toe
4) Margin and Edge of ulcer
• Margin is the border or transitional zone of skin around an ulcer.
Types:
o Healing margin [white (outer) – blue (central) – red (Inner)]
o Inflamed margin (red, irregular margin with inflamed
surrounding skin)
o Fibrosed margin (thickened white)
• Edge is the mode of union between the floor and the margin of
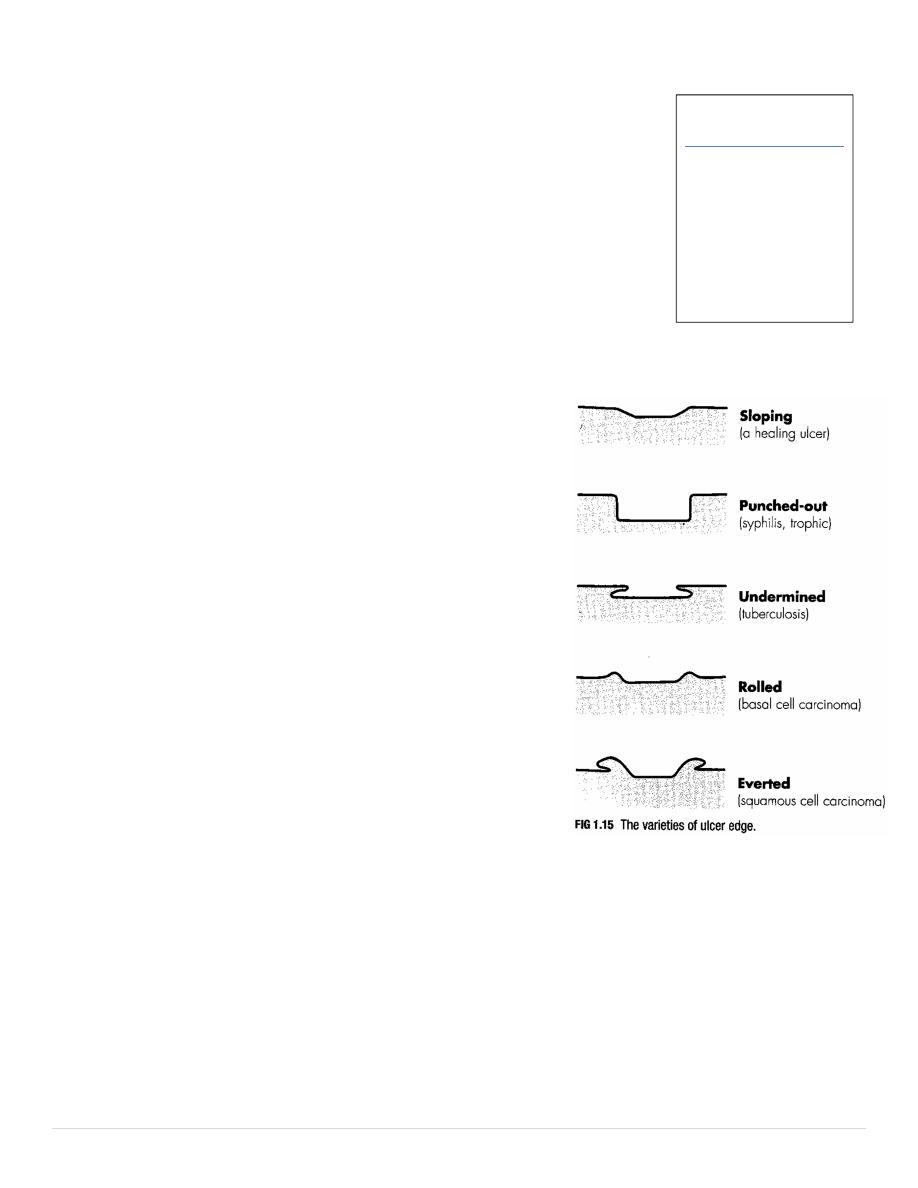
ulcer. Types:
o Sloping edge → healing ulcer
o Punched edge → trophic ulcer
o Undermined edge → tuberculous ulcer
o Everted edge→ malignant ulcer
o Raised edge → rodent ulcer
5) Floor of ulcer: is the exposed surface of the ulcer, we look for
• Type of Granulation tissue
• Amount of Slough (necrotic soft tissue not yet separated from living tissue)
• Nature of Discharge
6) Surrounding skin: if ulcer is spreading and infected the surrounding skin is shiny, red, edematous due to cellulitis
• Dark pigmentation & eczema → varicose ulcer
• Scars and puckering of skin → tuberculous ulcer
• Hypopigmentation → non-healing ulcer
• Large scar→ Marjolin’s ulcer
Inspection
1) Size & Shape
2) Number
3) Location
4) Margin & Edge
5) Floor
6) Surrounding skin
2 |
P a g e
B) Palpation
: for
1) Surrounding skin: for temperature & tenderness
2) Ulcer: edge, floor, base
Edge
• Soft: healing ulcer
• Firm: non-healing ulcer
• Hard: malignant ulcer
Floor:
• Granulation tissue: bleeding on touch? Healthy granulation tissue may show pinpoint hemorrhagic spots, while
malignant ulcer may bleed profusely
• Slough: attached loosely or firmly?
Base (tissue on which the ulcer rests):
• Consistency
• Underlying structures (muscle, fascia or bone?)
3) Test the fixity of the ulcer to the structures in its base
C) Focal examination
1. Regional Lymph node
2. State of arteries, venous circulation, nerves
3. Movement of neighboring joints
Lymph nodes
• Hard, discrete, non-tender → malignant ulcer
• Soft, tender → infective
• Non-tender, matted → tuberculous ulcer
State of arteries, veins, nerves
• If ulcer in lower limb: ask patient to stand and look for varicose veins, varicosities, also test for DVT by calf
tenderness (Moses sign) and Homan's sign (pain on passive dorsiflexion of foot).
• For any ulcer palpate arteries to rule out vascular disease & arterial insufficiency
• Test sensation of skin surrounding ulcer by sharp pin
• In trophic ulcer we should
o Map area of anesthesia
o Search features of Leprosy
o Neurologic exam
Examine joint around ulcer for active and passive movement
D) Systemic examination
• CVS: for CHF which delays ulcer healing
• R.S: for TB & secondaries
• A.S: for splenomegaly
Paplation
1) Surrounding skin
2) Ulcer: edge, floor, base
3) Test the fixity
