Acne vulgaris
DR . MANAR GHANEMM.B.CH.B.F.I.C.M.S.
24 NOV. 2016
ACNE VULGARIS
Acne : is a chronic inflammatory disorder of the pilosebaceous unit.It is a polymorphic disorder(comedons, papules , pustules, nodules, pseudocysts, and sometimes scarring)
The sites of predilection face, upper trunk and upper arms.
It usually affect adolescent.
Darker skinned patients at increased risk for developing post-inflammatory hyper-pigmentation and keloids.
Patients can experience significant psychological morbidity and, rarely, mortality due to suicide.
Prevalence: acne may be the most frequent reason for seeing a dermatologist, over 90% of males and 80% of females are affected during their teen age.
Age of onset: acne develops earlier in females than in males that may reflect the earlier onset of puberty.
Mean age at onset of acne was 12 ± years in girls and 15± years in boys.
Etiology and Predisposing factor
Family and genetic history
Excessive production of sebum
Endocrine factor :androgen , premenstrual exacerbation
Microflora (propionobacterium acne ) anaerobic
Diet
Mechanical (post epilation )
Psychological and emotional
Topical drugs and agents :oily cosmetics, some chemicals ,use of anabolic steroids
Puberty and menstrual cycle
Humidity and excessive sweating
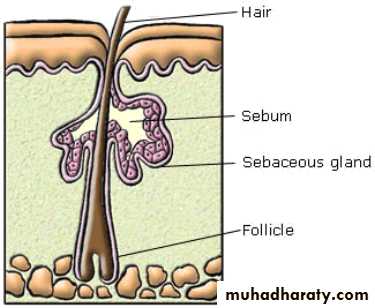
Normal hair follicle
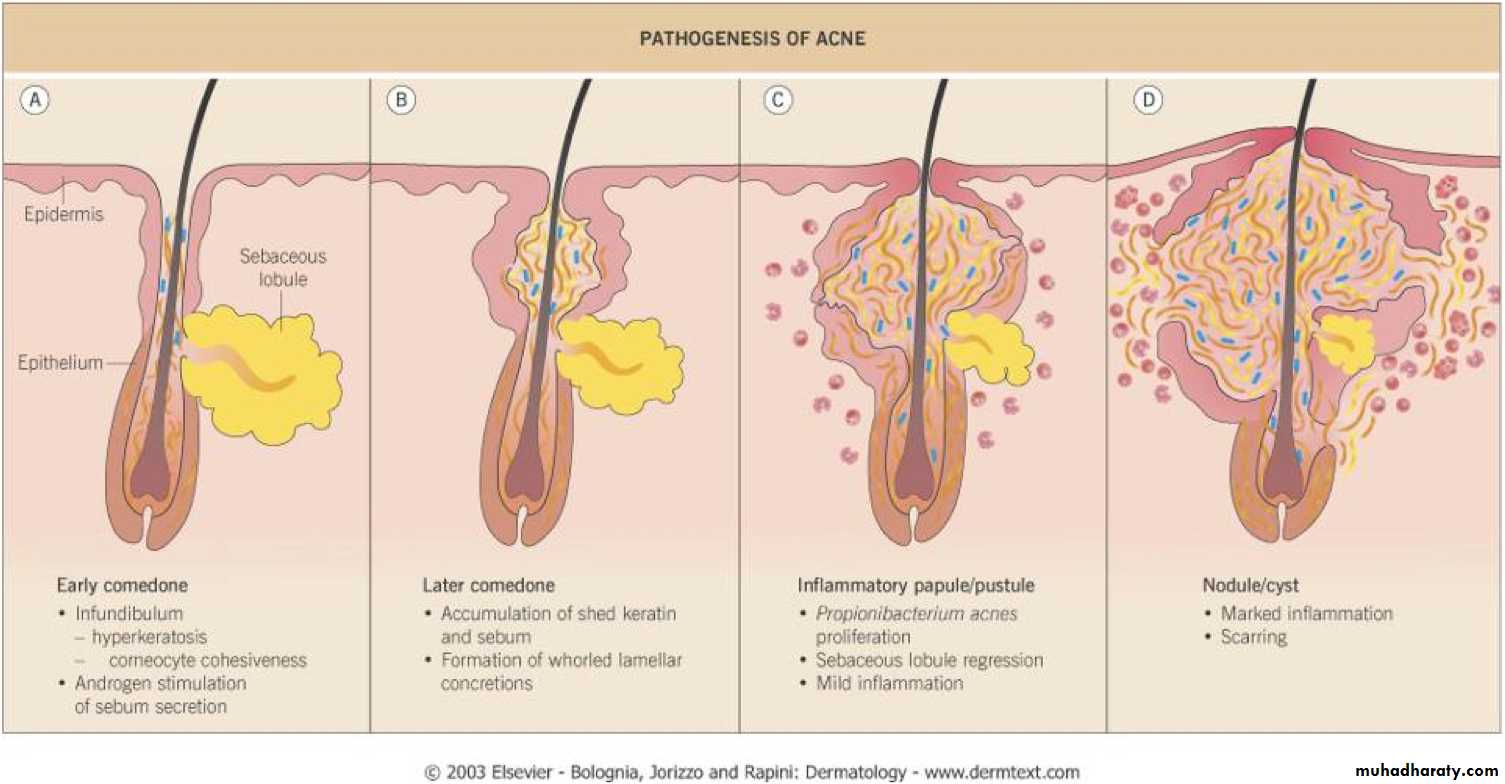
Pathophysiology
Follicular keratinocytes exhibit increased cohesiveness do not shed normally↓
leading to retention and accumulation of sebum.
↓
Androgens stimulate enlargement of sebaceous glands and increased sebum production
the abnormal keratinaceous material and sebum collect in the microcomedon. (so ccommedon formed which is a non inflammatory acne )
↓
bacterial proliferation (Propionibacterium acnes)
↓
Infection and inflammation
What goes wrong ??
The types of lesions in Acne:
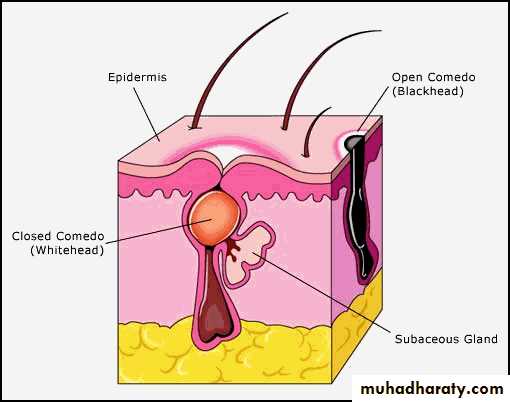
A – Non inflammatory lesions: (comedones) which consist of:White heads (closed comedones).
Black heads (open comedones).
B – Inflammatory lesions include:
The superficial lesions are usually papules and pustules.The deep lesions are deep pustules, nodule, pseudocysts & Sinuses
Clinical types
Closed comedone(whitehead):
a clogged follicle. Whiteheads usually appear on the skin as small, round, white bumps.
Open comedone (blackhead) a plugged follicle that opens and turns dark at the surface of the skin.
Blackheads do not indicate the presence of dirt.
Papules inflamed lesions that appear as small, pink bumps on the skin.
Pustules (pimples) inflamed pus filled lesions that are red at the base.Cysts and nodules large, inflamed, pus filled lesions deep under the skin that can cause pain and scarring.
Acne varients
• Neonatal acne• Persistant acne
• Late onset acne (chin of female )
• Acne conglobata (nodulocystic acne )
• Fulminante acne (fever + acne )
• Acne excorié ( hair epilation )
• Gram negative folliculitis. ( S.E. of tetracycline )
• Cosmetic Acne (make up )
• Drug induced acne (steroid acne )
• Endocrine acne.
Neonatal acne
Steroid acne
Local symptoms :
pain especially if acute inflammationSystemic symptoms
most often absent
Classification according to severity :
Comedonal acne: Only comedons
Mild acne: Less than 20 pustules.
Moderate to severe acne: More than 20 pustules
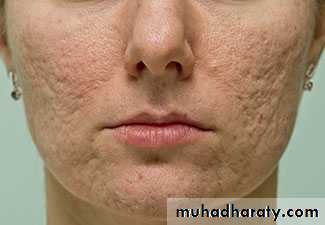
Complications of acne:1- Scarring.2-Psychological impact.
Ddx :1-Rosocea.
2-Perioral dermatitis.
3-Pitrosporum folliculitis.
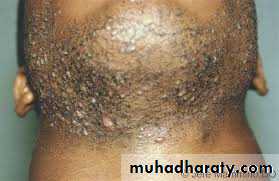
4-Folliculitis barbae and Psudofolliculitis barbae.
5-Acneform drug eraption
6-Acneform secondary syphilis.
Perioral dermatitis
Psudofolliculitis barbae
Treatment
A-General measures.B-Topical treatment.
C-Systemic therapy.
The choice of therapy.
Mild acne : topical therapy.Moderate acne : topical and oral therapies.
Severe acne: isotretinoin unless it is contraindicated.
A - General measures:
Gentle cleansing.Avoidness of comedogenic applications.
Reassurance .
B- Topical treatments:
1- Those directed towards microorganisms.
2- Those directed towards comedogenesis.
1- Topical treatments directed towards microorganisms:
Topical antibiotics:erythromycin (1.5-2% gel or cream).
clindamycin (1% lotion)
Benzyl peroxide.
2-Topical treatment directed towards comedogenesis:
Retinoids:1- Anti-seborrheic effect.
2- Anti-comedonal effect.
3- Anti-inflammatory effect.
4- Inhibiting the growth of P. acne .
Tretinoin may be used as solution, cream or gel. It is available in 0.025% , 0.05% and 0.1% concentration
Tazarotene (0.1% gel) applied once daily.
Adapalene: Adapalene (0.1% gel).
Azelaic acid: cream with 20%
C) Systemic Treatment of acne:
1-Those directed against microorganisms (antibiotics).2-Those directed against comedogenesis and seborrhea (retinoids).
3-Those acting on hormonal bases S(antiandrogens).
Systemic antibioticindications
Moderate or severe inflammatory acne.Acne resistant to topical treatment.
Acne that covers large area of the body.
Tetracycline: Tetracycline dose for an adult is 250 mg four times daily.
Doxycycline: It is usually given in a dose of 100 mg once or twice daily .Minocycline : The usual dose is 50-100 mg once or twice daily.
Erythromycin and Azithromysin
Clindamycin: In a dose of 75-150 mg.
Isotretinoin : is the single most effective treatment.
Indications:1- Severe acne.
2- Moderate unresponsive acne.
3- Acne with scarring.
4- Acne with severe depression or dysmorphophobia.
5- High sebum excretion rate.
6- Some unusual variants, such as acne fulminans, gram-negative folliculitis .
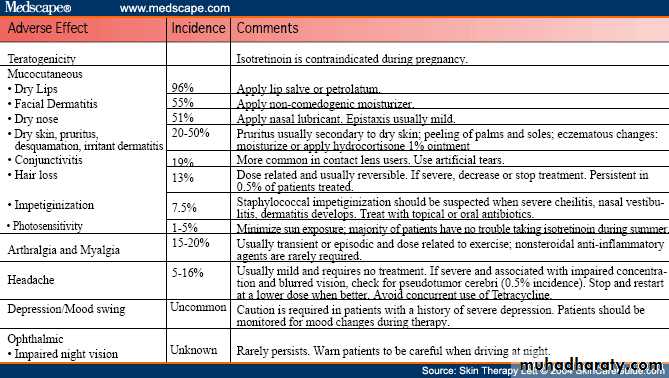
Side Effect of Isotretenoin
Teratogenic ( contraindicated to be pregnant)Dryness of skin and mucous membrane
Lip
Face and body
Nose – bleeding
Conjunctivitis
Hair lossImpetiginization
Photosensitivity
Arthralgia and myalgia
Depression
headache
Hormonal therapy
Indicated forAcne is not responding to conventional therapy.
If there are signs of hyperandrogenism.
A- Androgen production inhibitors
glucocorticoids and oral contraceptives.
B-Androgen receptor blockers: cyproterone acetate, spironolactone and flutamide.
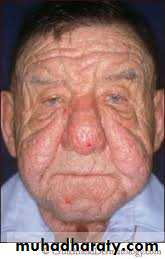
Rosaceaداء الوردية
Rosacea(latin: “like roses”) is a chronic inflammatoy disorder of the facial pilosebaceous units, with an increased reactivity of capillaries to heat, leading to flushing and telangiectasia...
Clinically
Stages of evolutionEpisodic (flushing) in response to (hot liquids), spicy foods; alcohol ,exposure to sun, heat and emotional stress.
Stage i: persistent erythema with telangiectases
Stage ii: persistent erythema, telangiectases, papules, tiny pustules
Stage iii: persistent deep erythema, dense telangiectases, papules, pustules, nodules;
marked sebaceous hyperplasia edema of the central part of the face "glandular rosacea“ causing disfigurement of the nose (Rhinophyma) (enlarged nose) }
Age of incidence between 30 to 50 years,
Sex females predominantly;Race WHITE peoples.
Distribution characteristic is a symmetrical localization on the face
Eye lesions “red” eyes :
Chronic blepharitis, conjunctivitis, and episcleritis. Rosacea keratitisDifferential diagnosis
Acne: (note: in rosacea no comedones)Perioral dermatitis
Folliculitis
SLE ( no papule and pustule )
Course :
Prolonged.Recurrences are common.
After a few years, the disease tends to disappear spontaneously.
Management
Reduction of alcoholic and hot beverages.
Topical :
Metronidazole gel or cream, 0.75 %, twice daily
orTopical antibiotics (e.g., erythromycin gel).
Systemic: oral antibiotics:
Tetracycline, 250mg 4td. until clear; then gradually reduce to once-daily doses of 250 to 500 mg.Minocycline and doxycycline: 50 to 100 mg twice daily.
Oral Isotretinoin