SURGERY OF STOMACH AND DUODENUM
Dr. Ahmed RasheedSurgical Anatomy
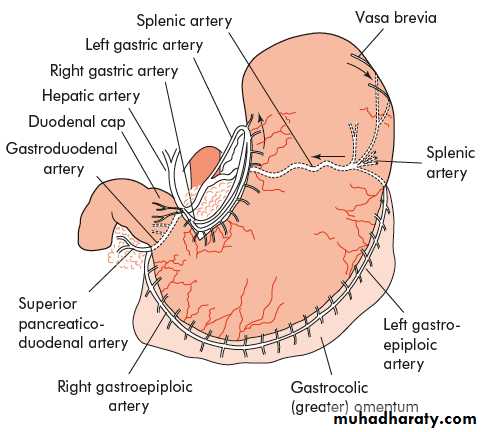
Food reservoir & mechanical digestion.Arterial blood supply
1- Left gastric artery: from CA
2- Right gastric artery: from CHA
3- Gastroduodenal artery ( from hepatic artery) divide into a –superior pancreaticoduodenal A., b- right gastroepiploic artery.
4-Inferior pancreaticoduodenal artery a branch of superior mesenteric artery
5- Left gastroepiploic artery a branch of splenic artery..
6- Short gastric arteries from splenic artery
Venous drainage
1- Lesser curve: right & left gastric (coronary) veins drain into portal vein2- Greater curve: left gastro epiploic vein & vasa brevia join splenic vein
3- G curve: right gastro epiploic vein join superior mesenteric vein
4- vein of mayo
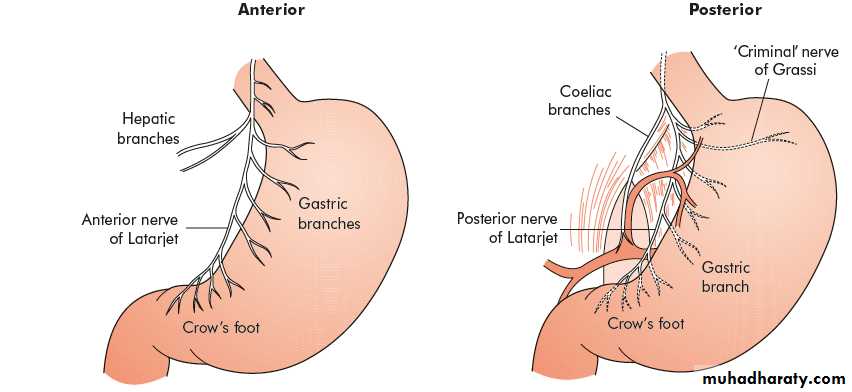
Nerve supply
1-Intrinsic:
a- myenteric plexus of Auerbach,
b- submucosal plexus of Meissner
2-Extrensic:
- Ant. Vagus & post vagus ( afferent sensory; efferent secretomotor).
- Sympathetic from celiac ganglion.
Physiology
1-Parietal cells secrete HCL2-Chief cells secrete pepsin
3- Endocrine cells secrete gastrin (G cell), somatostatin(D cell)..
Investigations of stomach & duodenum
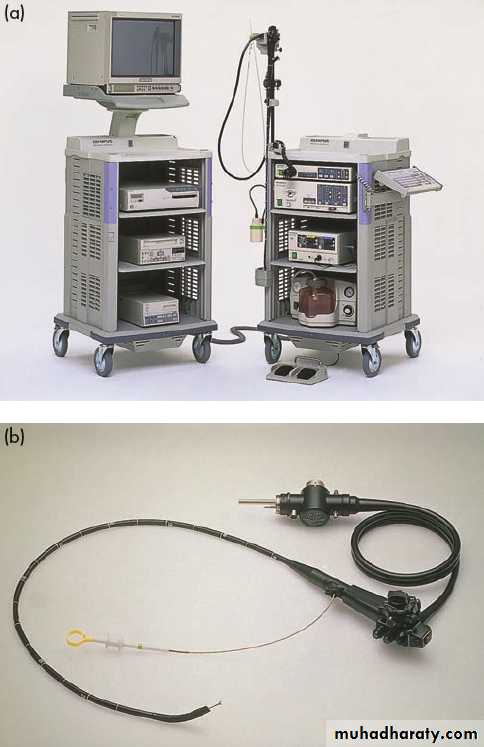
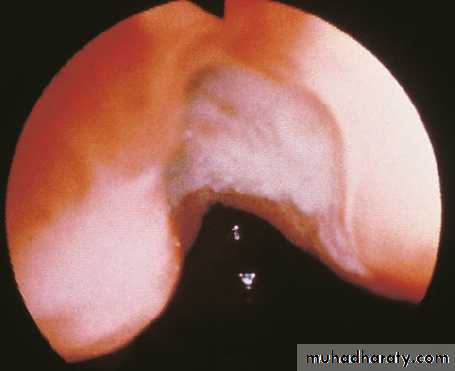
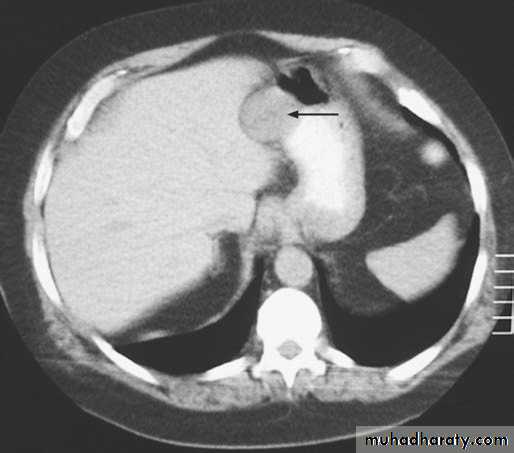
OGD flexible endoscopyEndoscopic ultrasound: more sensitive than CT for tumor staging.
Barium meal
Ultrasound
Computerised tomography scanning (CT Scan) and Magnetic resonant imaging.
Laparoscopy: detect peritoneal metastasis, + U/S to check liver & LN.
PET Scan.
Angiography
SURGICAL PATHOLOGY
1-Congenital hypertrophic pyloric stenosis2-Duodenal atresia
HELICOBACTER PYLORI
Spiral bacteria
- It is important in the aetiology of gastroduodenal diseases such as
1- Chronic gastritis
2- Peptic ulceration
3- Gastric cancer
Types of Gastritis
Type A gastritisAn autoimmune condition; there is circulating antibody against parietal cell mass resulting in hypochlorhydria then to achlorhydria ; a premalignant condition
Deficient secretion of intrinsic factor by parietal cell lead to malabsorbtion of vitamin B12 leading to pernicious anemia which is again premalignant condition.
Type B Gastritis
Associated with Helicobacter pylori, affect the antrum
Can develop peptic ulcer, pangastritis with risk of gastric cancer.
Intestinal metaplasia is associated with chronic pangastritis with atrophy.
Intestinal metaplasia with dysplasia is pre malignant condition that needs regular OGD follow up.
Reflux Gastritis
Occur after gastric surgery ,treatment medical very rare surgical..
Erosive Gastritis
Caused by NSAID & alcohol.
Stress Gstritis
Serious illness or injury, cardiopulmonary bypass
Reduction to blood supply of the superficial mucosa
Can lead to stress ulcer +/- bleeding
Prevention by H2 antagonist +/- barrier agent e.g. sucralfate.
Menetriers Disease
Gross hypertrophy gastric mucosa, mucus production, & hypocholhydria.
Premalignant condition ,only treatment is gastrectomy.
Other forms of Gastritis
Lymphocytic gastritis : T cell infiltration , + celiac disease
Esinophilic Gastritis
Granulomatous Gastritis in Crohn’ dis.
AIDS Gastritis
Phlegmonous (Bacterial) gastritis
PEPTIC ULCER
Common sites: 1-first part duodenum. 2-lesser curve stomach. 3- oesophagus. 4- stoma following gastric surgery. 5- Meckel’s diverticulum.1-Acute peptic
( gastric & duodenal ) ulcer & acute stress ulcer.
Causes: major illness, uremia, food poisoning, bacteraemia, burn, aspirin, steroid & NSAID.
Pathology
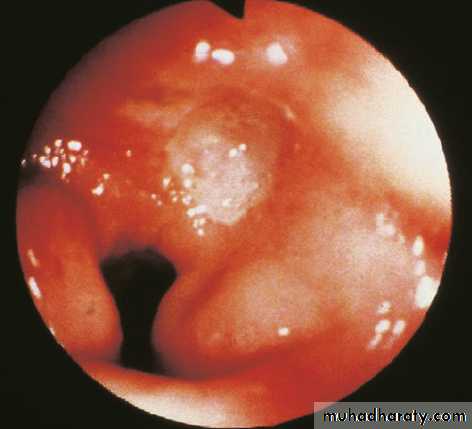
Single or multiple as diagnosed by OGD.it involve the mucous membrane & does not penetrate the muscles, acute ulcer may bleed, or perforate..
Treatment.
Treat the cause plus anti ulcer treatment.
2-Chronic peptic ulcer.
Deeper penetrating ulcer.
A-Gastric ulcer having relatively normal level or below normal gastric acid secretion.
B-Duodenal ulcer occur in presence of very high acid level; also occur in Zollinger Ellison syndrome, genetic factors may be involved, H pylori, social stress.. emotional, smoking, NSAID
DUODENAL ULCER
IncidenceThe incidence of duodenal ulcer & the frequency of elective surgery are falling therapy except in cases of complications:
Use of OGD
Wide spread use of anti ulcer drugs & eradication of H.pyl.
More common in male than female, older age, & developing countries.
Pathology
Occur in first part duodenum it involve the mucosa, muscle coat, leading to fibrosis and pyloric stenosis, it may penetrate post. to pancreas & invade gastro duodenal artery,
Sometimes multiple ulcers,, or ANT,& POST. ulcer called kissing ulcers,,
Ant. ulcer tend to perforate while Post. ulcer tend to bleed.
Big ulcer called GIANT ulcer.(more than 2 cm.)
Chronic duodenal ulcer never become malignant.
Chronic gastric & chronic duodenal ulcer may co exist.
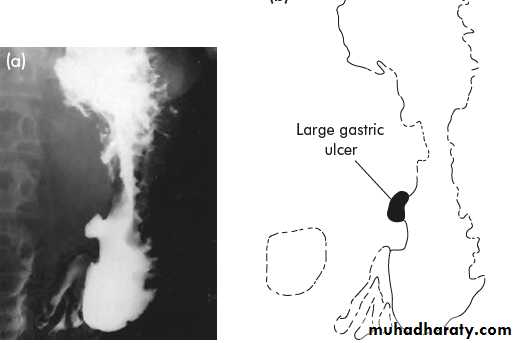
GASTRIC ULCER
IncidenceSame etiological factors
Gastric ulcer is less common than D.U
Sex are equal male to female,
Population is older than d.u.
More prevalent in low socioeconomic patients,,.
Pathology
Usually on the lesser curve of stomach, but it is larger than DU.
Invade mucosa & muscle coat & fibrosis may cause stomach deformity: hour glass stomach or tea pot deformity, may penetrate to pancreas or blood vessel or invade transverse colon ..
Malignancy in gastric ulcer
1-On the long run ch. GU might become malignant ; take multiple biopsies during OGD
2-other type of GU is malignant from the start.
Other types of peptic ulcer
1-stomal ulcer at jujunal site of gastrojejunostomy.
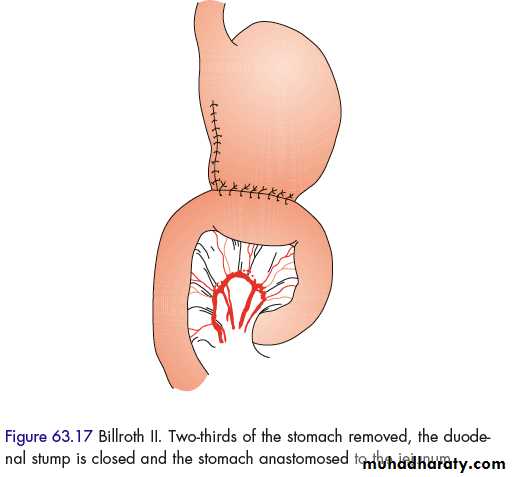
2-Billroth II (polya) gastrectomy.
3- Prepyloric gastric: risk of cancer so it need biopsy.
Clinical features of gastric & duodenal ulcers
- PAIN in the epigastric region, may radiate to the back, it is intermittent, may last weeks or months with interval of pain free, eating aggravates pain in GU & relieve pain of DU.- PERIODICITY; attack of pain last from 2—6 weeks, attack is more in spring & autumn.
- VOMITING: absent unless there is pyloric stenosis .
- Alteration in weight.
- BLEEDING: either chronic loss presented as anemia; or fresh as hematemesis & melena.
CLINICAL EXAMINATION
Tenderness at epigastric region, stomach splash in case of pyloric stenosis.
INVESTIGATIONS OF PEPTIC ULCER
1--OGD with or without multiple biopsy (CHECK ESOPHAGUS ,,, STOMACH,,DUODENUM),,& STOMA OF GASTROJEJUNOSTOMY to exclude stomal ulcer.2—BARIUM MEAL
3—C.B.P.
TREATMENT OF CHRONIC PEPTIC ULCER
The vast majority of uncomplicated peptic ulcer are treated medically ,,surgical treatment of uncomplicated peptic ulcer has decreased markedly since 1990.due to the use of H2 recepter antagonist or proton pump inhibitor & eradication therapy.
The aim of surgical treatment is to reduce gastric acid secretion,(now it is reserved for the complicated P.U.)
MEDICAL TREATMENT
1 - Cessation of cigarette smoking ,,NSAIDs & Cortisone.
2- H2 receptor antagonist a-cemetidine (tagamet)- b-ranetidine ( zantac ).
3- Mucosal protective agent: sucralfate (ulcar).
4- Proton pump inhibiter (omeprazole )
5- Eradication therapy: flagyl x3, plus amoxil 500mg x3 ; or flagyl plus Clarithromycin 500mg twice a day for 2 weeks.
SURGICAL TREATMENT OF UNCOMPLICATED PEPTIC ULCER
Although it is rare now, if medical Rx fails.Operations for D. U. aim is diversion of the acid away from duodenum,
HISTORICAL SURGICAL PROCEDURES
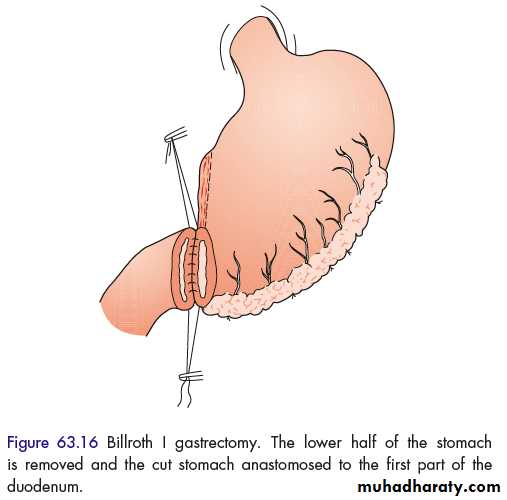
1-BILLROTH I & BILLROTH II (polya) GASTRECTOMY, by Billroth in 1881.
2-GASTRO JEJUNOSTOMY (by Wolfler in 1881) will end with high rate of stomal ulcer.
At present time the operation of choice in cases of DU. are:
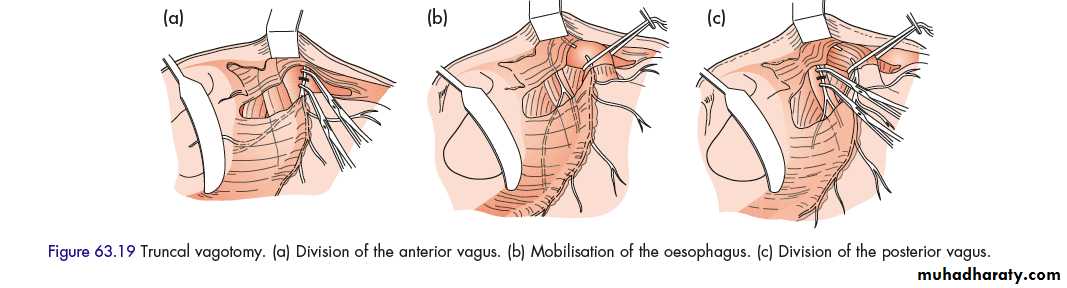
1—Truncal vagotomy (Dragstedt 1943) plus drainage procedure (due to gastric stasis):
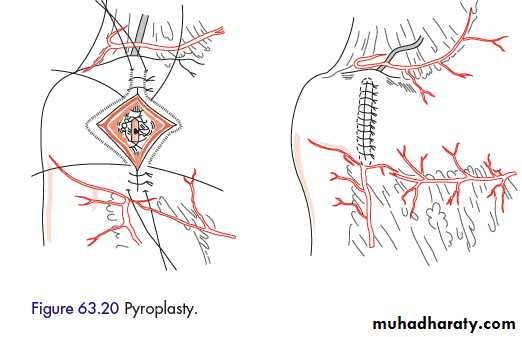
A—PYLOROPLSTY.
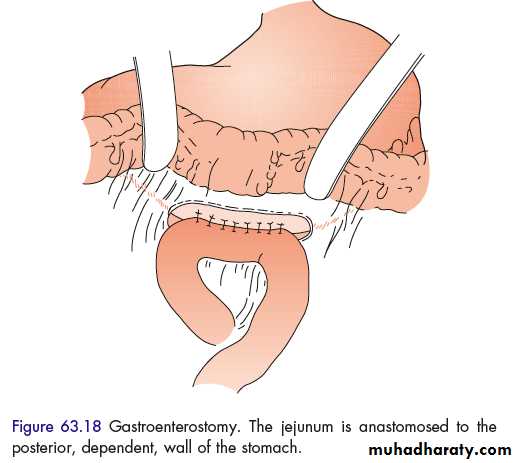
B—GASTROJEJUNOSTOMY: posteriorly at antrum.
2- Selective vagotomy plus drainage procedure.
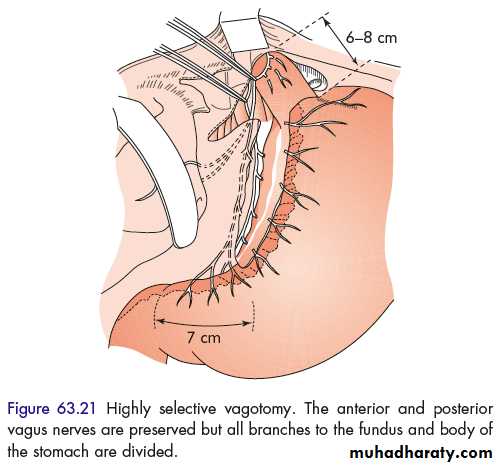
3-Highly selective vagotomy only ( with preservation to the nerve of Latarjet that supply the pylorus).
4- Truncal vagotomy and antrectomy (Billroth I): very low recurrence but more side effects & mortality.
Operations for gastric ulcer
1—BILLROTH I OR BILLROTH II OPERATION PLUS EXCISION TO GASTRIC ULCER FOR HISTOPATHOLOGY TO EXCLUDE MALIGNANCY2—Or Vagotomy plus drainage procedure plus excisional biopsy of the ulcer..
COMPLICATIONS OF PEPTIC ULCER SURGERY
1- Recurrent ulceration –a-either same ulcer, or b-stomal ulcer (complication may cause gastrojejunocolic fistula).2- Bile vomiting: may respond to bile-chelating agents; or may require dismantling of gastrojej., or antrectomy + Roux en Y gastrojejunostomy.
3- Small stomach syndrome.
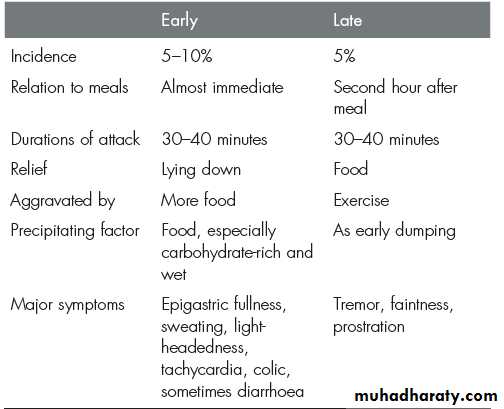
4-Dumping due to rapid gastric emptying:
a—early dumping: osmotic effect of food.
b—late dumping: reactive hypoglycemia.
5-Post vagotomy diarrhea .
6-Malignant changes: bile reflux gastritis then intestinal metaplasia then malignancy.
7-Gallstones formation.
8-Nutritional disorder: wt. loss, anemia, vit.B12 deficiency.
COMPLICATIONS OF PEPTIC ULCER 1-PERFORATION PEPTIC ULCER:
1- Ant. 1st part duodenum most common, 2- Gastric ulcer, 3- prepyloric ulcer.SYMPTOMS
Some give history of D.U. or silent ulcer ,,there will be Sever sudden onset epigastric pain then generalized due to irritant effect of gastric acid & gastric contents of food on the peritoneum, first chemical peritonitis then bacterial peritonitis,
SIGNS
At first temp. subnormal or normal then temp. increase (pyrexia by bacterial peritonitis),pulse increases,
Abdomen moves little or not move with respiration,
Severe abdominal tenderness, abdominal rigidity called board like rigidity,
On percussion dull, on auscultation first bowel sound +ve then become –ve.
P.R. exam elicit tenderness at rectovesical pouch.
In advanced peritonitis: septicemia & septic shock & mortality will be high.
INVESTIGATIONS
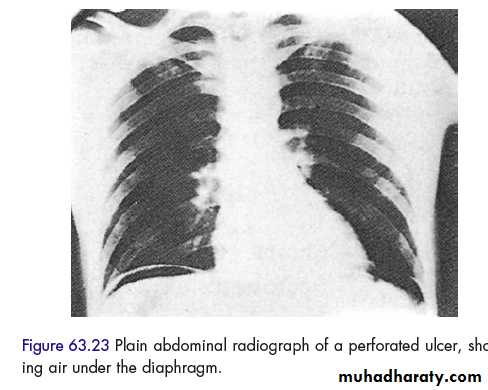
Xray abdomen in erect ,,supine & lateral position,,, shows gas under diaphragm in 70% of chest x-ray,,Blood tests, serum amylase, abdomen ultrasound & C.T.Scan abdomen..
TREATMENT
Resuscitation: antibiotics, tagamet injection, NG tube, Foley’s catheter.
Emergency laparotomy by upper mid line incision, localize the perforation site close the perforation by interrupted sutures with or without omental patch, then peritoneal toilet, then put drain.
Rarely partial gastrectomy indicated:
1-perforation in carcinoma 2-sever bleeding 3-perforation is big & can not be closed.
Postop. period & Follow up by anti ulcer treatment & O.G.D.
Other types of treatment:
- Conservative (small perforation & localized peritonitis)
- Definitive surgical treatment of PU if patient is fit.
2—PYLORIC STENOSIS
Due to fibrosis or cicatrisation of duodenum or sometimes due to oedema associated with prepyloric ulcerAlso called GASTRIC OUTLET OBSTRUCTION DUODENAL STENOSIS.
Other causes of gastric outlet obst:
carcinoma pylorus, adult hypertrophic pyloric stenosis, pyloric mucosal diaphragm.
CLINICAL FEATURES
There is a history of long standing peptic ulcer .
SYMPTOMS
1-Pain, 2- Vomiting (foul) no bile, undigested food.
SIGNS
1-Wt loss, 2 - dehydration , pale 3-distended epigastric region, 4- visible peristalsis from left to right, 5- succussion splash positive (audible) on shaking abdomen of the patient.
METABOLIC EFFECT
There will be HYPOKALEMIC METABOLIC ALKALOSIS
PARODOXICAL ACIDURIA.
DEHYDRATION PLUS ANAEMIA PLUS VITAMINE DIFICIENCY.
INVESTIGATIONS
1-O.G.D. + BIOPSY. 2- BARIUM MEAL 3-BLOOD+ELECTROLYTES TEST.
TREATMENT
1-N.G TUBE 2- I.V.FLUID +NACL + KCL. 3-WATCH URINE OUT PUT. 4- ANTI ULCER TREATMENT.
MILD CASES DUE TO OEDEMA WILL RESPOND TO CONSERVATIVE.SEVER CASES WILL NEED SURGERY
IF THE ULCER HEALED DO ONLY DRAINAGE BY GASTROJEJUNOSTOMY ONLY.
2-IF THERE IS ACTIVE ULCER DO TRUCAL VAGOTOMY PLUS GASTROJEJUNOSTOMY OR PYLOROPLSTY.
FOLLOW-UP AS FOR PATIENT WITH PERFORATED PEPTIC ULCER.
3—BLEEDING (HAEMATEMESIS & MELENA) OF PEPTIC ULCER
Either 1- slight 2- major bleeding.Sometimes there is history of peptic ulcer, drug intake like NAIDs &ASPIRIN.
THERE IS EROSION OF AN ARTERY IN THE FLOOR OF AN ULCER, LIKE GDA OR SPLENIC ARTERY,IF PATIENT ABOVE 40 YS THERE IS ATHEROSCLEROSIS SO THE ARTERY WILL NOT CONTRACT TO ARREST BLEEDING
SYMPTOMS & SIGNS
FEATURES OF BLEEDING.
TREATMENT
RESUSCITATIONI.V.CANNULA, CVP LINE, BLOOD SAMPLE FOR BLOOD TEST, I.V. FLUID, BLOOD TRASFUSION, INJACTABLE ANTI ULCER TREATMENT, NG TUBE, FOLEY ‘S CATHETER, PULSE & BP CHART, OXYGEN,
SPECIFIC INVESTIGATIONS FOR DIAGNOSIS SPEC. O.G.D.; ANGIOGRAPHY…
CONSERVATIVE TREATMENT: IF BLEEDING STOP CONTINUE MEDICAL TREATMENT +/- MINIMAL INTERVENTION.
MINIMAL INTERVENTION
MANY O.G.D. DEVICES ARE AVAILABLE CAN ACHIEVE HAEMESTASIS : INJECTION DILUTED ADRENALINE ,,OR NACL INJECTION ,OR BY ANGIOGRAPHY TO FIND THE SITE OF THE BLEEDER AND EMBOLIZATION.
INDICATION OF SURGERY:
—IF BLEEDING STOPPED BUT RECCUR AGAIN AFTER ADMISSION TO HOSPITAL .—IF BLEEDING NEVER STOP SINCE ADMISSION TO HOSPITAL & PATIENT RECEIVE MORE THAN 6 UNITS BLOOD.
SURGICAL TREATMENT
AIM OF SURGERY IS TO STOP THE BLEEDING.For POST. D.U:
DO LAPARATOMY BY UPPER MIDLINE INCISION, MOBILIZE THE DUODENUM, DO LONGITUDINAL INCISION 3,5 CM STOMACH SITE 2,5 CM DUODENUM SITE, BY CUTTING PYLORIC SPHINCTOR
MULTIPLE INTERRUPTED UNDERRUNING SILK SUTURES,
THEN DO PYLOROPLASTY,
EITHER DO TRUNCAL VAGOTOMY OR CONTINUE GIVING ANTI ULCER TREATMENT
- ON RARE OCCASION THERE WILL BE A NEED TO DO LIGATURE TO GASTRODUODENAL ARTERY OR TO DO PARTIAL GASTRECTOMY.
IN BLEEDING GASTRIC ULCER PROCEDURE THE SAME
1-EITHER ARREST BLEEDING +BIOPSY,, OR, 2—EXCISION BIOPSY TO THE ULCER AND CLOSE STOMACH.
HAEMATEMESISS & MELAENA (UPPER GASTROINTESTINAL BLEEDING)
CAUSES
1- CHRONIC PEPTIC ULCER 60%
2- ACUTE PEPTIC ULCER 26% (EROSION)
3- OESOPHAGEAL VARICES 4%
4- MALLORY –WEISS TEAR (SYNDROME) 4%: Longitudinal tear below the GEJ due to repetitive strenuous vomiting.
5- TUMOUR O.5%
6- VASCULAR e.g.DIEULAFAYS DISEASE O.5%
7- OTHERS 5% e.g.PURPURA,,HAEMOPHILIA
MANAGEMENT
- SAME RESUSCITATION PLUS INVESTIGATIONS
- SPECIFIC TREATMENT ACCORDING TO THE CAUSE
GASTRIC NEOPLASMS
BENIGN TUMOURS.LEIOMYOMA
NEUROFIBROMA
POLYP( S): Metaplastic (H. pylori), Inflammatory, Fundic gland polyp( + use of PPI), Adenoma (10%, premalignant), Carcinoid.
GASTRIC CANCER
GASTRIC CANCER IS ONE OF THE MOST COMMON CAUSES OF DEATH IN THE WORLD.
THE OUTCOME IS GENERALY POOR, OWING TO THE ADVANCED STAGE AT TIME OF PRESENTATION.
EARLY PRESENTATION OF GASTRIC CANCER IS ASSOCIATED WITH VERY HIGH CURE RATE.
INCIDENCE
Variable worldwide, high incidence in Japan.
MEN AFFECTED MORE THAN WOMEN.
INCIDENCE INCREASE WITH AGE.
IN THE WEST GASTRIC CANCER IS CONTINUING TO FALL BY 1%PER YEAR.THIS REDUCTION AFFECT CANCER ARISING FROM BODY & PYLORUS, WHILE THERE IS INCREASE IN CANCER IN THE PROXIMAL STOMACH.
CANCER OF BODY, PYLORUS ARE MORE COMMON IN LOW SOCIOECONOMIC GROUP.
PROXIMAL GASTRIC CANCER AFFECT HIGH SOCIOECONOMIC GROUP..
PROXIMAL GASTRIC CANCER NOT ASSOCIATED WITH H,PYLORI
BODY & PYLORUS CANCER IS ASSOCIATED WITH H. PYLORI..
AETIOLOGY
1- H.PYLORI ASSOCIATED WITH BODY & PYLORIC TUMOR.H.PYLORI CAUSE GASTRITIS , THEN GASTRIC ATROPHY, & INTESTINAL METAPLASIA
2- PERNICIOUS ANAEMIA & GASTRIC ATROPHY ARE RISK FACTOR.
4-GASTRIC POLYP.
5-AFTER GASTRIC SURGERY eg. BILLROTH II, PYLOROPLASTY, GASTROJEJUNOSTOMY,WILL INCREASE THE RISK 4 TIMES, DUE TO REFLUX BILE GASTRITIS.
7—CIGARETTE SMOKING, DUST INGESTION,,
8—INGESTION OF SPIRIT CAUSE GASTRITIS ON LONG RUN CHANGE TO CANCER.
9—GENETIC FACTOR,
CLINICAL FEATURES
SYMPTOMSDYSPEPSIA,
POOR APPITITE, WEIGHT LOSS.
DISTENSION,
BLEEDING,
ANAEMIA,
DYSPHAGIA,VOMITING,
LUMP AT EPIGASTRIC REGION
SIGNS
EPIGASTRIC TENDERNESS,
?MASS,
STOMACH SPLASH,
DEHYDRATION,,FEATURES OF PYLORIC OBSTRUCTION,
THROMBOPHLEBITIS OF SUPERFICIAL Vs. OF THE LEG (Trousseau’ s sign),
ENLARGED LEFT SUPRACLAVICULAR LYMPH NODES(Troisier‘sign),
LIVER METASTASIS CAUSE JAUNDICE,
ASCITES.
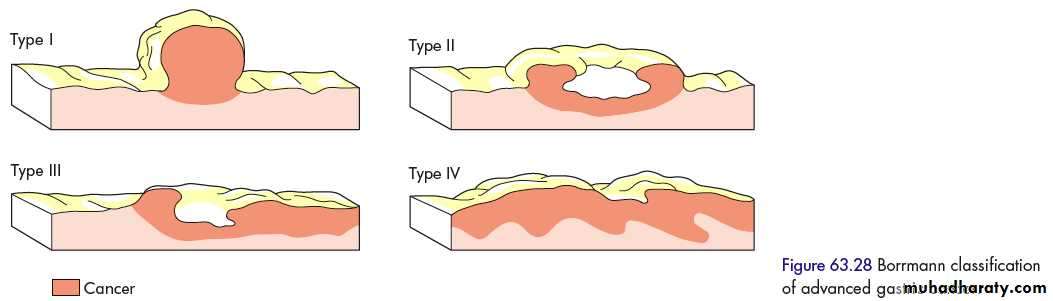
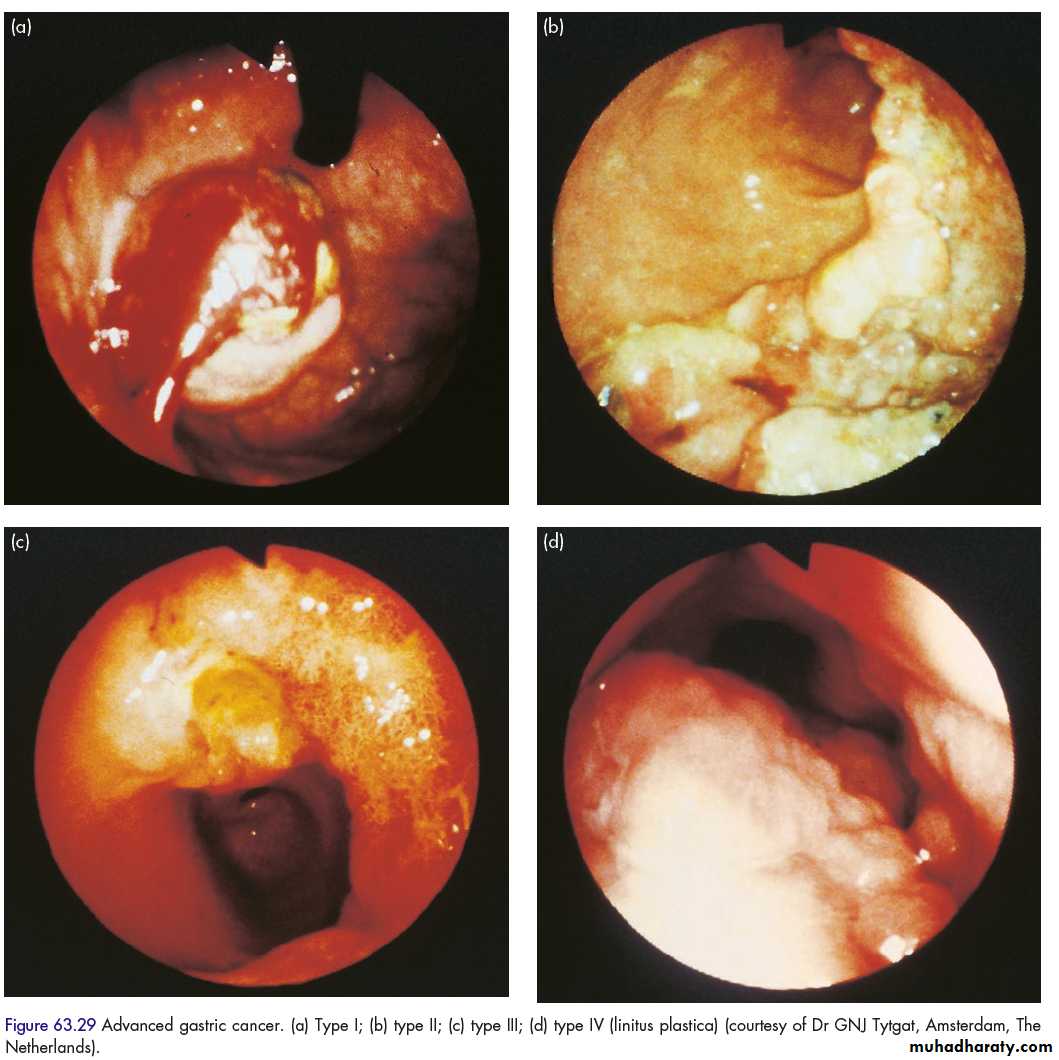
PATHOLOGY
1—INTESTINAL GASTRIC CANCER (Arise in intestinal metaplasia)
A—POLYPOIDAL.
B—ULCERATIVE
2—DIFFUSE GASTRIC CANCER INFILTRATES DEEPLY IN STOMACH WITHOUT OBVIOUS MASS (LINITIS PLASTICA) OR CALLED (LEATHER BOTTLE STOMACH). BAD PROGNOSIS.
MICROSCOPICALLY IT IS COLUMNAR CELL
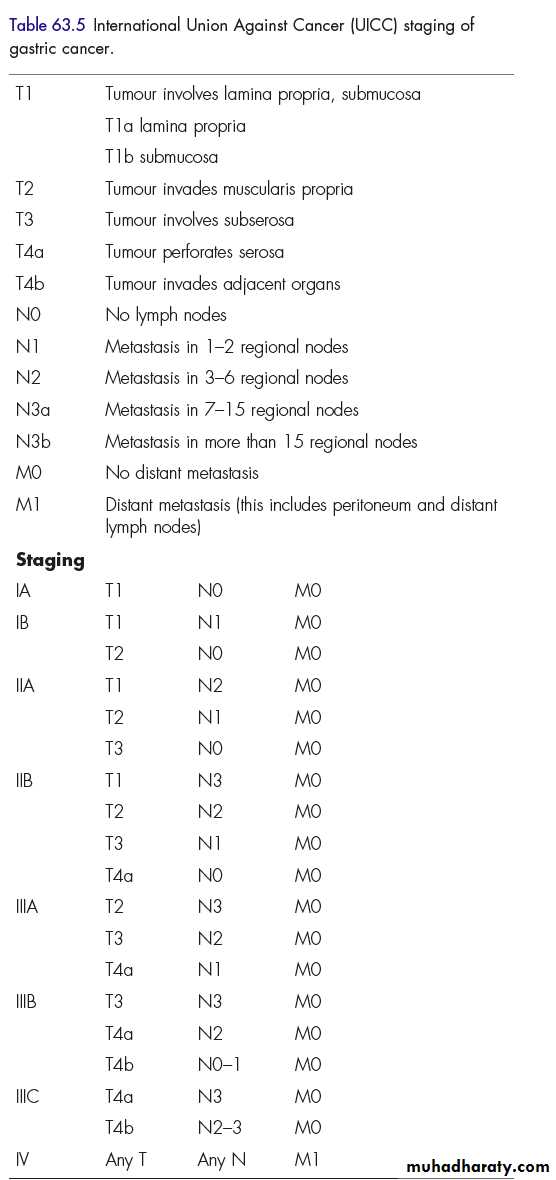
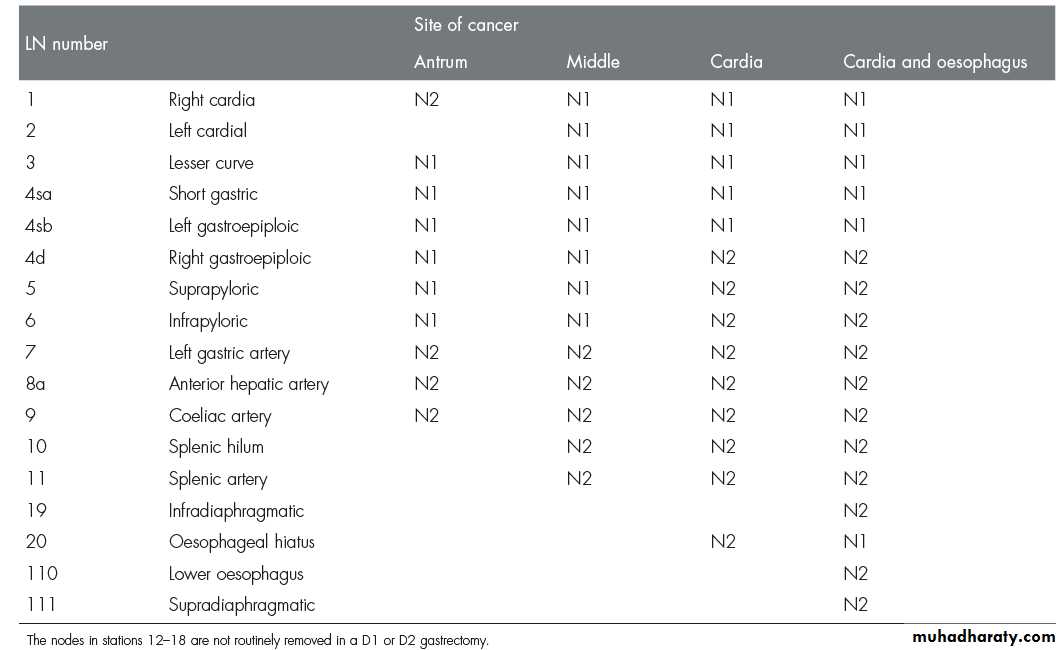
MOST COMMON SITE IS AT PROXIMAL STOMACH , WHILE IN JAPAN IT IS MORE DISTAL.STAGING CARCINOMA STOMACH (TNM)
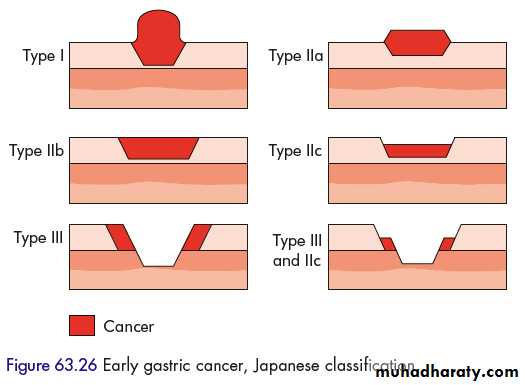
Early cancer: limited to mucosa & submucosa i.e T1, any N.Advanced cancer involves the musculais.
SPREAD OF GASTRIC CANCER
1-DIRECT INVADE THE WALL THEN, LIVER, PANCREAS, COLON, OMENTUM.2-LYMPHATIC SPREAD BY PERMIATION & EMBOLIZATION.
3-BLOOD-BORNE METASTASIS.
4-TRANSPERITONEAL SPREAD.
INVESTIGATIONS
TREATMENT OF GASTRIC CANCER
1-PALLIATIVE SURGERYGASTROJEJUNOSTOMY
ENDOSCOPIC STENTING.
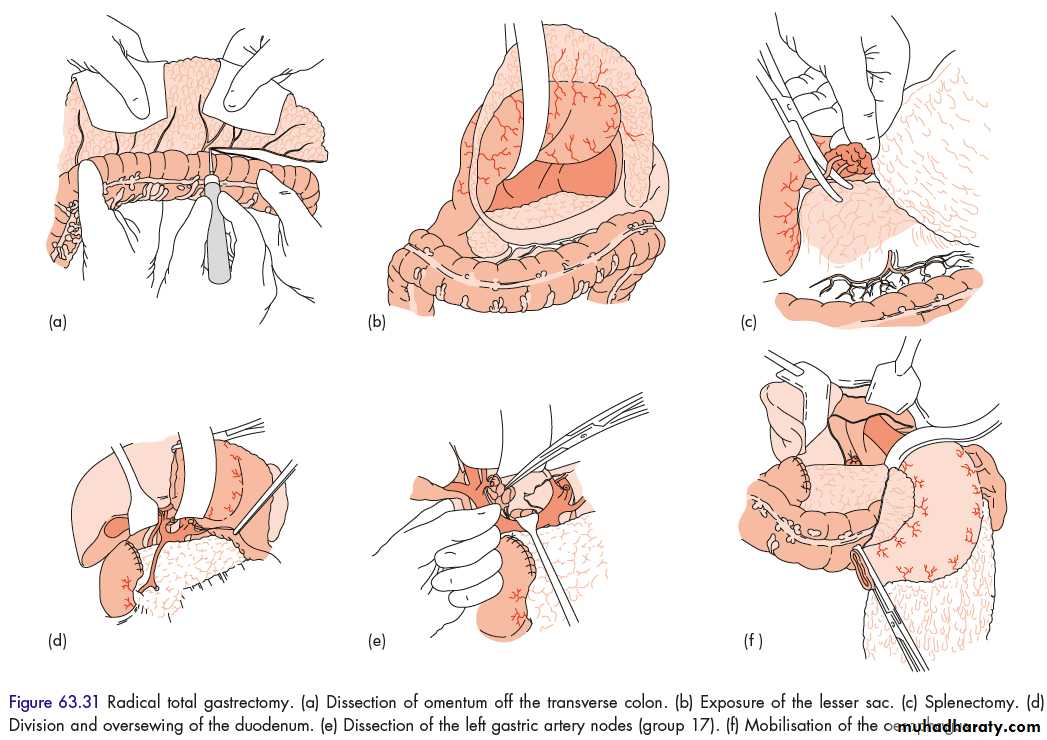
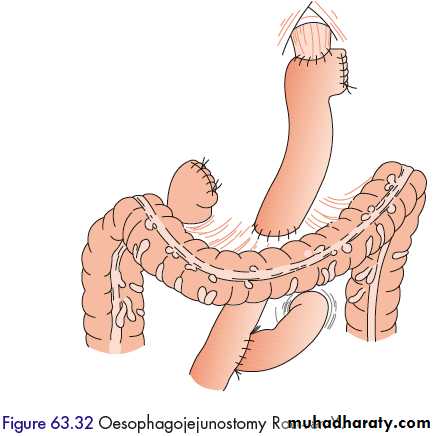
2-RADICAL RESECTION
TOTAL GASTRECTOMY + ROUX EN Y ESOPHAGOJEJUNOSTOMY.
SUBTOTAL (BILLROTH II) GASTRECTOMY for distal cancer.
Gastric cancer is chemosensitive: given as neoadjuvant therapy ( Cis-platinum, Epirubicin, 5-FU).
GASTROINTESTINAL STROMAL TUMOURS
GIST comprise 1–3 per cent of all gastrointestinal neoplasia, 50 % affect the stomach.equally in males and females.
associated with a mutation in the tyrosine kinase c-kit oncogene.
mucosa overlying the tumour ulcerates, leading to bleeding, or that they are noticed incidentally at endoscopy.
Because the mucosa overlying the tumour is normal, endoscopic biopsy can be uninformative; Targeted biopsy by endoscopic US is more helpful.
Tumours over 5 cm in diameter should be considered to have metastatic potential.
treated by wedge excision.
These tumours are sensitive to the tyrosine kinase antagonist imatinib.GASTRIC LYMPHOMA
1- Primary gastric lymphoma: ~5 % of gastric neoplasms; B cell derived, arising from the mucosa-associated lymphoid tissue (MALT)2- Stom. involvement in generalized lymphoma.
most common in the sixth decade.
Symptoms: pain, weight loss and bleeding. Acute presentations of gastric lymphoma, such as haematemesis, perforation or obstruction, are not common.
form a diffuse mucosal thickening, which may ulcerate
Diagnosis made by endoscopic biopsy.
Surgery for localized disease, & chemotherapy for systemic disease.
Early lymphoma may regress by H.pylori eradication.
THANK YOU