د.دلال الجراح
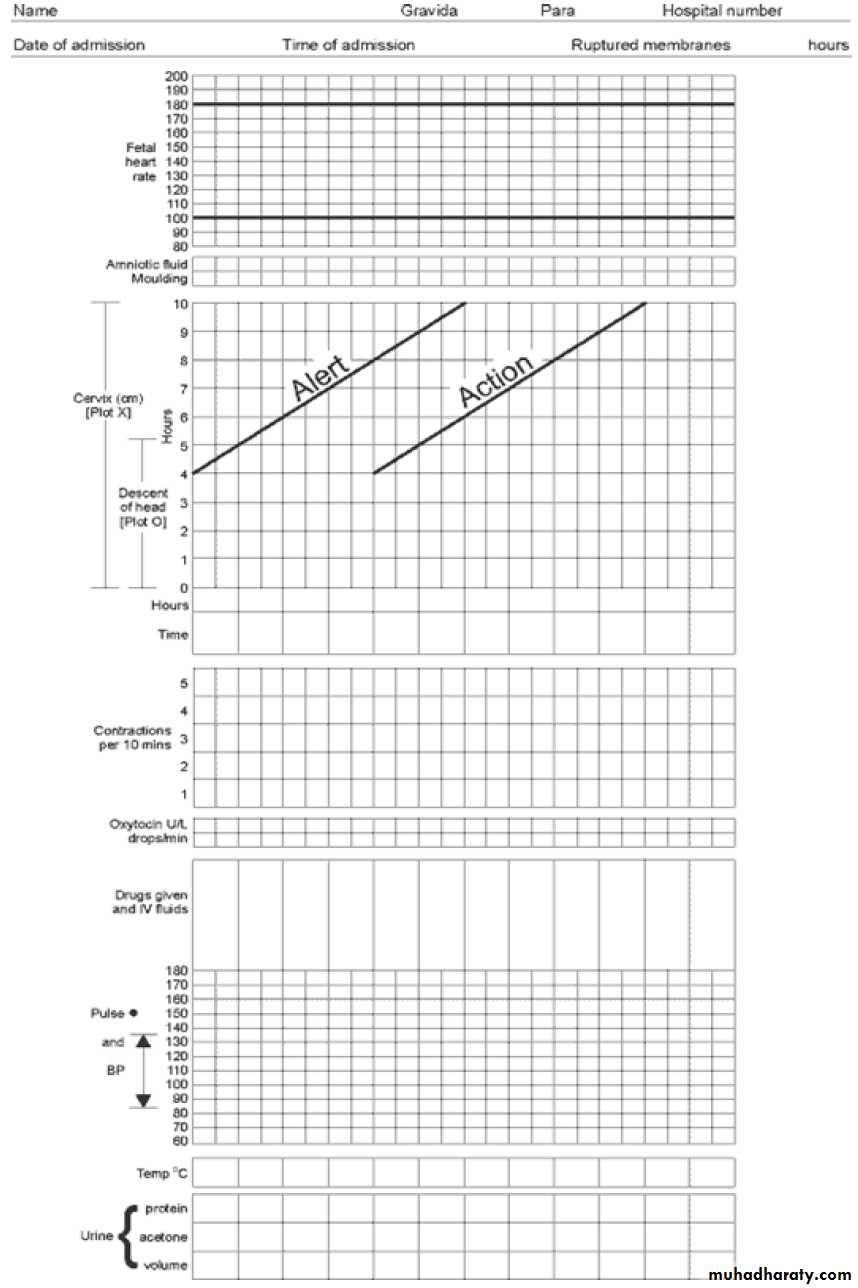
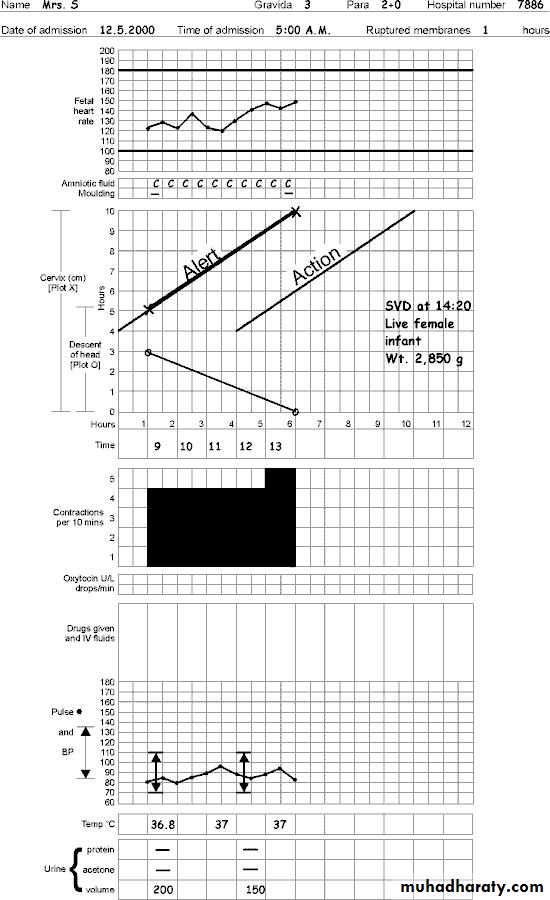
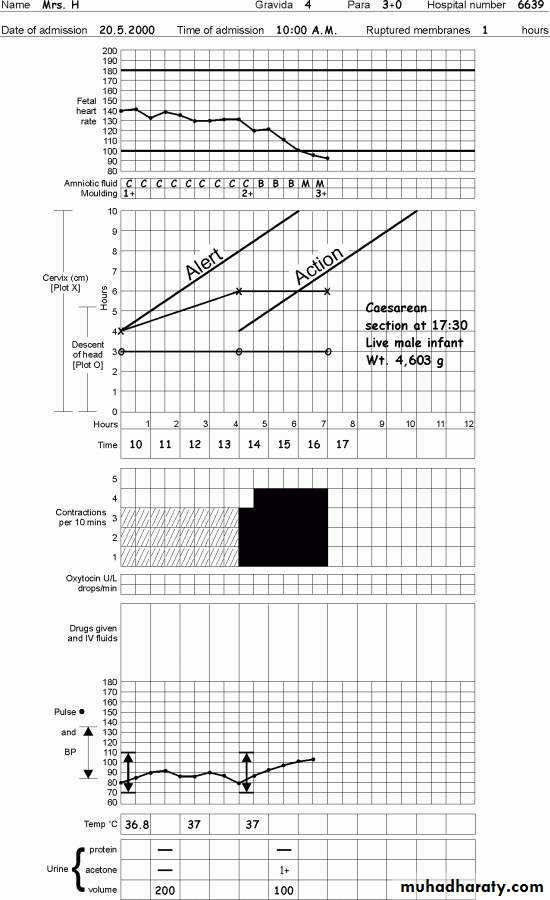
PARTOGRAMDefinition: - is a graph recording of the progress of labor and the condition of the mother and fetus. It was developed and tested by the WHO 1994.
History
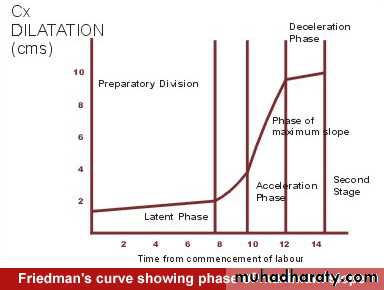
Friedman’s partograph- devised in1954 based on observations of cervical dilatation and fetal station against time elapsed in hours from the onset of labor; latent and active phase. The time onset of labor was based on the patient’s subjective perception of her contractility. Plotting cervical dilatation against time yielded the typical sigmoid or ‘S’ shaped curve and station against time gave rise to the hyperbolic curve. Limits of normal were defined.
Philpott and Castle-1972: introduced alert and action lines.
Benefits of partogram:Early detection of abnormal progress of labor.
Early decision on acceleration of labor.
Early decision on transfer of patient.
Early recognition of problem with the mother and fetus.
Early recognition of CPD long before labor becomes obstructed.
Reduce incidence of CS rate.
Inexpensive, effective and pragmatic.
Who should not have partogram
Antepartum hemorrhage
Eclampsia
Malpresentation
Preterm labor
Fetal distress
Multiple pregnancy
WHO partogram
COMPONENTS
Part I: patient identification
Part II: fetal condition
Part III: progress of labor
Part IV: maternal condition
Outcome…..
Part I: Patient identification
Enter all details in the appropriate sections on the front of the partogram,
including date and time of admission, name, age, gravidity and parity, EDD, time of ruptured membranes, any relevant obstetric & medical history,
DATE: - Record the commencement date at the top of the partogram. When the date changes at midnight write the new date above the times.
TIME:-
The numbered (0 1 2 3 etc.) full vertical lines are hour lines.Time column in partogram is below the graph of labor progress.
Example\ Note the exact time (e.g. 1450 hours) of the first observation that you wish to record (e.g. fetal heart, vaginal examination, etc.). Go back to the nearestwhole hour – 1400 hours in this example.
Fill in the time scale along the top of the partogram: 1400, 1500, 1600 etc.
(1400 is 0-hour line) and record the observations on the partogram (in this
Example) just to the left of the 1500 line.
1
2
3
4
5
6
7
8
9
1500
1600
1700
1800
1900
Part II: FETAL ASSESSMENT
Upper table of the partogram, includes the followings: -
Fetal heart rate
Membranes and amniotic fluid
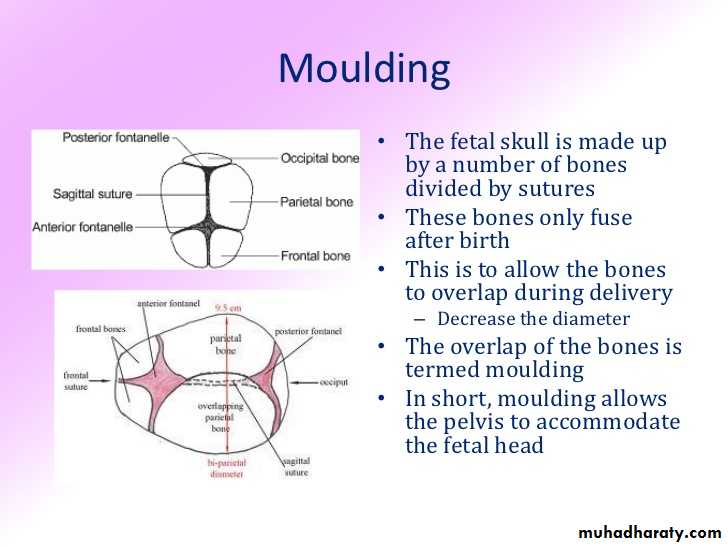
Moulding the fetal skull bones. Caput.
Fetal heart rate.
Record the FHR with a dot • and join the lines as follows:The vertical lines are half-hourly so that the quarter-hourly recordings can be
made. Monitor every 30 minutes in latent phase, and every 15 minutes in active phase. In second stage of labor every 5 minutes. Basal fetal heart rate is 110-160.
Amniotic Fluid.
In the box that correlates with the correct time according to the vertical lines
record half hourly absence or presence, and color of fluid as follows:
I - membranes intact
C – rupture membranes + amniotic fluid is clear
B – rupture membranes + amniotic fluid is blood stained
M – rupture membranes + amniotic fluid has meconium staining.
A- rupture membranes + Absent liquor
Moulding of fetal skull bone.
Moulding is an important indication of how adequately the pelvis can accommodate the fetal head. The fetal skull is made up by a number of bones divided by sutures, these bones only fuse after birth. This is to allow the bones to overlap during delivery (decrease the diameter). The overlap of the bones is termed moulding. Increasing moulding with head high in the pelvis is an ominous sign of cephalo-pelvic disproportion.
There are 4 different ways to record the moulding on the partogram, immediately beneath those of the state of liquor.
If bones are separated and the suture can be felt easily: record as the letter “O”
If bones are just touching each other: record as +
If bones are overlapping but reducible: record as ++
If bones are overlapping severely and not reducible: record as +++
Moulding may be difficult to assess in the presence of a large caput, but that in itself should alert the attendant to possible CPD.
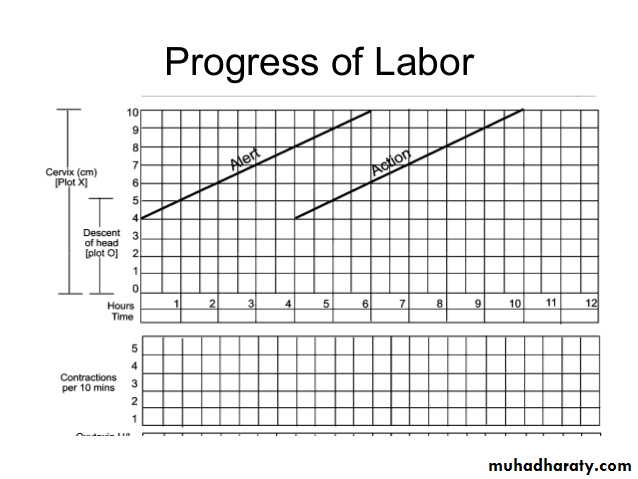
Part III: PROGRESS OF LABOR
Cervical dilatationDescent of fetal head
Uterine contraction
Fetal position
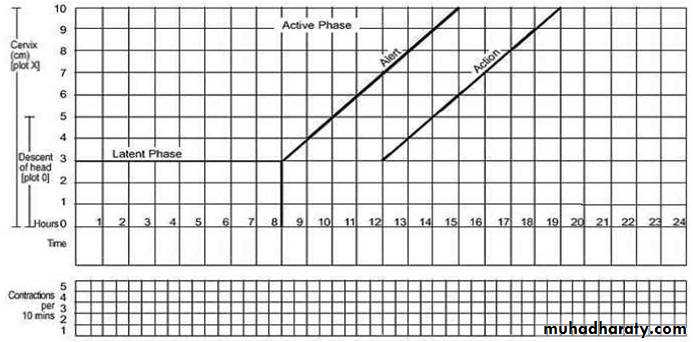
Cervicograph
The cervicograph is that section of the partogram which depicts cervicaldilatation and descent of the presenting part in relation to time. Use of the
cervicograph enables the progress of labor to be ascertained and delay in to
progress readily recognized.
In the center of the partogram is a graph, along the left side are numbers 0-10 against squares: each square represent 1cm dilatation. Along the bottom of the graph are numbers 0-12: each square represent 1 hour.
Dilatation
Record as X for the cervical dilatation starts on the alert line, and at the time the
examination is carried out. Thereafter, vaginal examinations are made every 4 hours, unless contraindicated. However, in advanced labor, women may be assessed more frequently particularly in multiparous.
Descent
Descent of the head is measured by abdominal palpation and is expressed in terms of fifths above the pelvic brim. Record as ‘O’ in the graph for the level of descent at each vaginal examination. When 2\5 or less of fetal head is felt above the level of symphesis pubis, this means that the head is engaged (the vertex has passed or is at the level of ischial spines).
Fetal positions
Occiput transverse positionsOcciput anterior positions
Alert and Action lines
Two lines drawn on the partogram at the time of the first vaginal examination in active labor, i.e., when the woman is 4cm dilated.Alert line: A line drawn from the point of cervical dilatation 4cm (active phase). This line denotes a slowest dilatation rate of 1cm/hour. In normal labor, cervical dilatation should be either on the alert line or to the left of it.
Action line: A line parallel and 4 hours to the right of the alert line.
A vaginal examination is performed 4 hours after the initial one or earlier if
clinically warranted. If subsequent examination shows dilatation between Alert line and Action line a repeat vaginal examination is carried out in 2 hours. Between the alert and action line, in health center, the women must be transferred to a hospital with facilities for CS, artificial rupture of membrane ARM may be performed if membranes are still intact
At or beyond action line; Conduct full medical assessment. Consider intravenous infusion\bladder catheterization\ analgesia. Options: Deliver by CS or augmentation of labor if no contraindication.
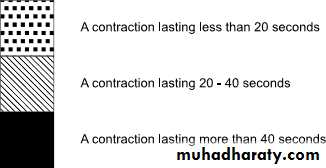
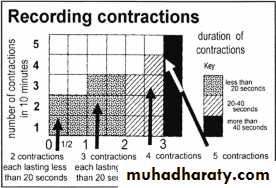
Contractions
Observation of contractions are made every hour in latent phase and every half hour in active phase.
There are 2 observations made of contractions:
The frequency, how often are they felt?
The duration, how long do they last?
The frequency of contractions is assessed by the number of contractions in a 10-minutes period. The duration of the contractions is from the time the contraction is first felt abdominally to the time when the contraction passed off, measured in seconds.
On the partogram below the time line, there is an area of 5 blank squares high going across the length of the graph; and at the left-hand side is written “contractions per 10 minutes”. Each square represents 1 contraction, so that if 2 contractions are felt in 10 minutes, 2 squares will be shaded.
Use the key for shading to demonstrate the strength of contraction are 3: -
Weak and > 20 seconds duration
Moderate and 20-40 seconds duration
Strong and <40 seconds duration
Contractions that lead to labor have the following characteristics:
May start as infrequently but usually accelerate over time, increasing in frequency that occur every 2-3 minutes.
Tend to last longer ≥40 seconds and are more intense than Braxton-Hicks contractions
Lead to cervical changes.
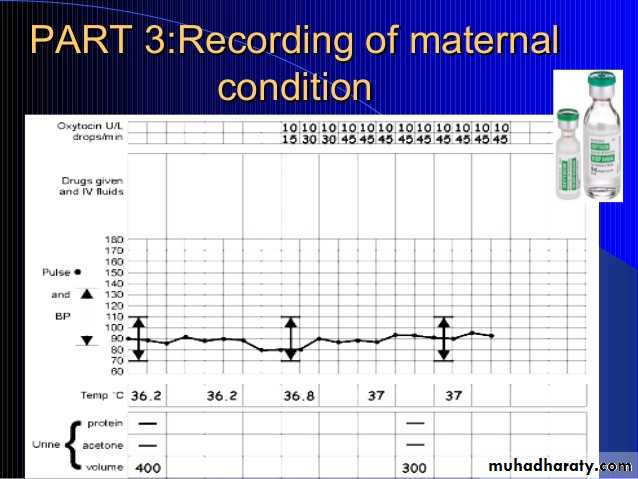
Part IV: MATERNAL condition
DrugsVital signs
Urine monitoring
Record maternal blood pressure, pulse, temperature, on the graph at the partogram. Using the measurements down the left side of the graph record
Drugs used:
Oxytocin administration: -There is a separate area for recording oxytocin titration just below the column for contractions. All entries are recorded in relation to the time at which the observations are made.
→ Units\L: record half hourly in black the number of units per liter of intravenous fluid.
→ Drops\min: record half hourly in black the number of drops per minute that has infused.
Other drugs: - record the fluid type, total volume and any medication added also according to the time.
Vital signs:
Blood pressure- Every 4 hours and recorded as vertical line marked with arrows
Pulse - marked with a ×- Every 30 minutes
Temperature- recorded every 2 hours
Urine monitoring:
Urine volume, analysis for protein and acetone every time urine is passed