د.دلال الجراح
INTRAPARTUM FETAL MONITORINGMeconium and liquor volume:
Reduced liquor volume during labor is associated with an increase incidence of fetal heart decelerations. Reduced liquor volume may reduce the volume of the intervillous space, and predispose to umbilical cord occlusion, both of which increase the risk of fetal hypoxemia.
Meconium in uneventful labor without FHR abnormalities and no risk factors seems to have no great significance. Whereas meconium in presence of complicated labor and FHR abnormalities or any risk factors has a greater risk of fetal hypoxia.
Intermittent auscultation:
During contraction and 1minute after it. Done every 30minutes in latent phase and every 15minutes in active phase.
Abnormal fetal heart in auscultation:
<110BPM in between contractions
< 110 BPM 30 seconds after contractions (late decelerations)
> 160 BPM in between contractions
In these conditions do CTG
Continuous fetal monitoring:
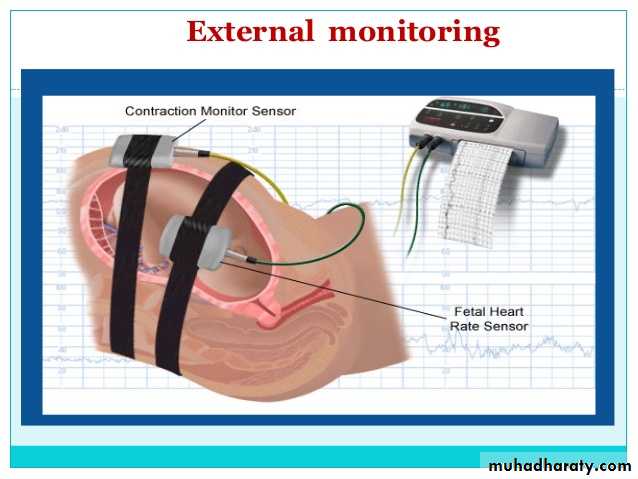
►External cardiotocography CTG:- The fetal heart rate and the activity of the uterine muscle are detected by two transducers placed on the mother’s abdomen and recorded on a paper, it has two components:
Fetal heart rate: -
Most commonly obtained by using an ultrasound transducer which is held against the maternal abdomen by an elastic band. Must be positioned correctly so the FHR will be plotted on the CTG record paper. Fetal body movement or maternal pulsations can interfere with the signal.
Uterine contractions: -
When the uterus contracts, the myometrial muscle shorten and the body of uterus enlarges in diameter. This forward movement of uterus results in an increase in abdominal girth which can be registered on a pressure transducer held firmly on the front of abdomen. Again, an elastic band is used to fit the transducer in its best place over the fundus to respond to maximum forward movement.►Internal continuous monitoring:-
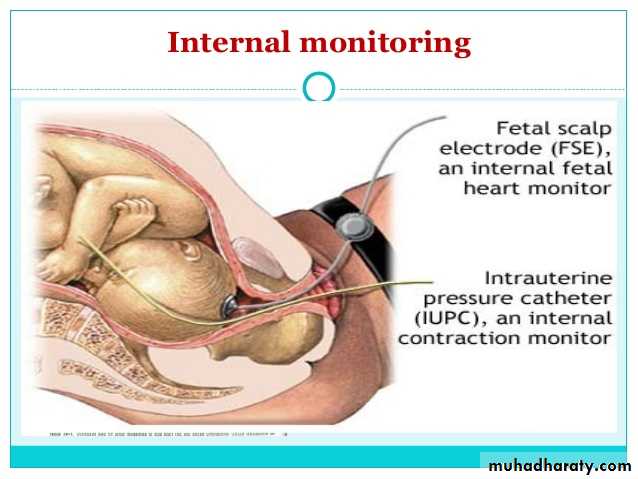
Fetal heart rate:uses an electronic transducer connected directly to the fetal scalp. A wire electrode is attached to the fetal scalp through the cervical opening (the membranes must be ruptured) and is connected to the monitor. Internal monitoring provides a more accurate and consistent transmission of the fetal heart rate than external monitoring by identifying R waves on the fetal ECG, but more expensive and invasive so may be used when external monitoring of the fetal heart rate is inadequate, or closer surveillance is needed.
Uterine activity:
small catheter (Intrauterine pressure catheter) is placed inside the uterus to record intrauterine pressure and so the contractions intensity. In early labor is 30 mmHg and becomes 60-70 mmHg in the second stage
Indications for continuous fetal monitoring: -
Epidural analgesiaMeconium stained liquor
Excessive uterine activity
Induction of labor with oxytocin
Abnormal FHR in intermittent auscultation
Abnormal fetal growth during pregnancy
Vaginal bleeding
High risk pregnancy
Prolonged 1st stage
Fetal response to hypoxia
Chemoreceptors:- the initial response to acute hypoxemia is via the carotid artery chemoreceptors. An acute stimulation of the autonomic nervous system occurs via the carotid sinus nerve. An increase in vagal tone (parasympathetic) results in FHR bradycardia and sympathetic stimulation initiates a peripheral vasoconstriction which results in a redistribution of the fetal cardiac output favoring the brain, heart and adrenal glands.
Humoral responses:- if interruptions to oxygen delivery are long enough or severe enough to stimulate the adrenal gland to secrete catecholamines, the intermittent nature of the acute vagal stimulation tending to slow the FHR will be overcome by the chronic elevation of the catecholamines, the baseline FHR will rise between decelerations.
Analysis of tracings in CTG
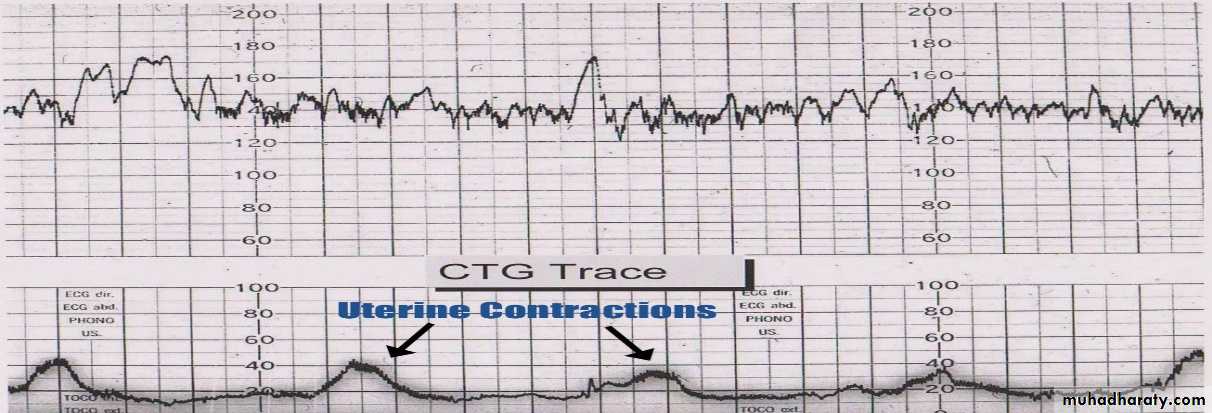
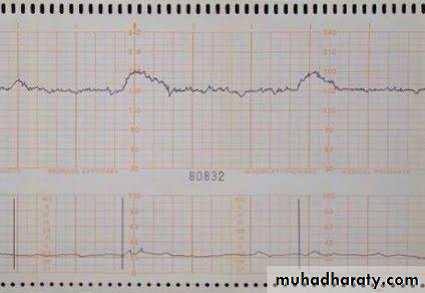
CTG analysis starts with the evaluation of basic CTG features recorded in a paper. The paper speed may be 1cm, 2cm, or 3cm\minute; each hard vertical line represents one minute. Two lines recorded in the CTG paper, the upper one represent the fetal heart pattern and lower one the uterine activity pattern.
Uterine contractions:-
Individual contractions are seen as peaks on the part of the CTG monitoring uterine activity. You should assess contractions for the following:
Frequency: Record the number of contractions present in a 10 minute period, each big square is equal to 1 minute, so look at how many contractions occurred within 10 squares.
Duration – how long do the contractions last?
Intensity – how strong are the contractions? (Assessed using palpation)
Fetal heart rate trace has 4 components: -
Baseline FHR
Baseline Variability
Accelerations
Decelerations
Fetal Heart rate
Baseline FHR:
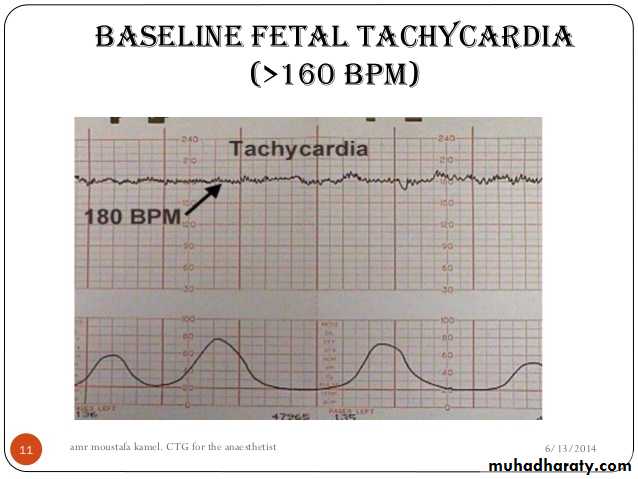
This is the mean level of the most horizontal FHR segments and expressed in beats per minute (bpm). Normal baseline between 110-160 bpm.►Tachycardia:
baseline value of >160 bpm lasting for more than 10minutes. Causes:
Maternal pyrexia
Fetal infection
Drugs: sympatho-mimetic drugs(salbutamol), parasympathetic blockers (atropine)
Gestational age <32 weeks
Fetal hypoxemia
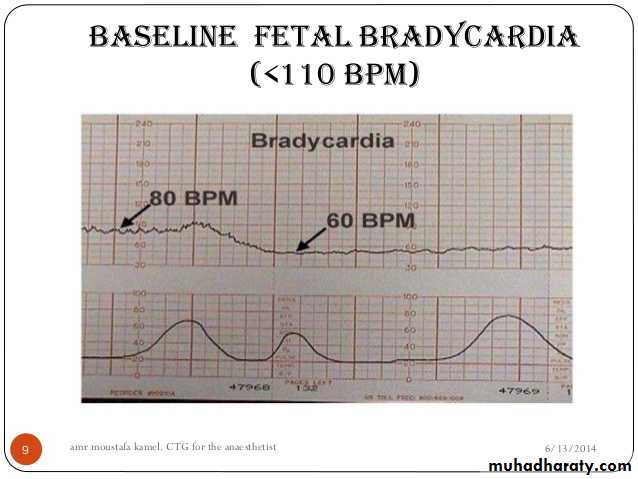
►Bradycardia:
Baseline value below 110 bpm lasting more than 10 minutes. Causes:Cord compression\prolapse
Congenital heart malformation
Drugs like narcotics
Maternal hypotension: postural or epidural analgesia
Rupture uterus
Late fetal hypoxia
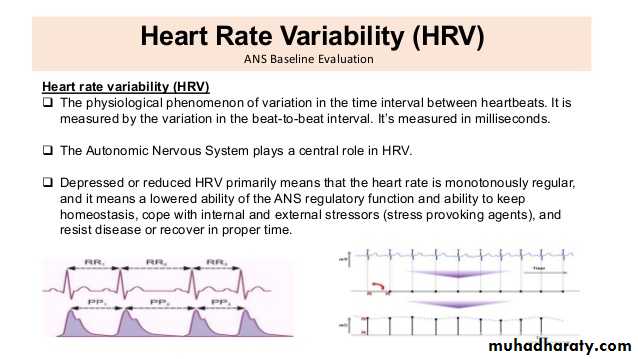
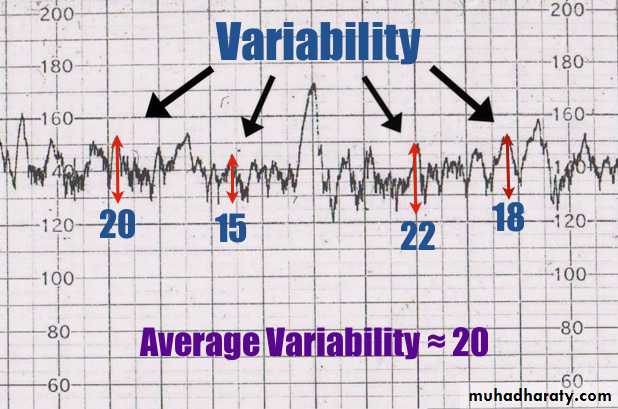
Variability:
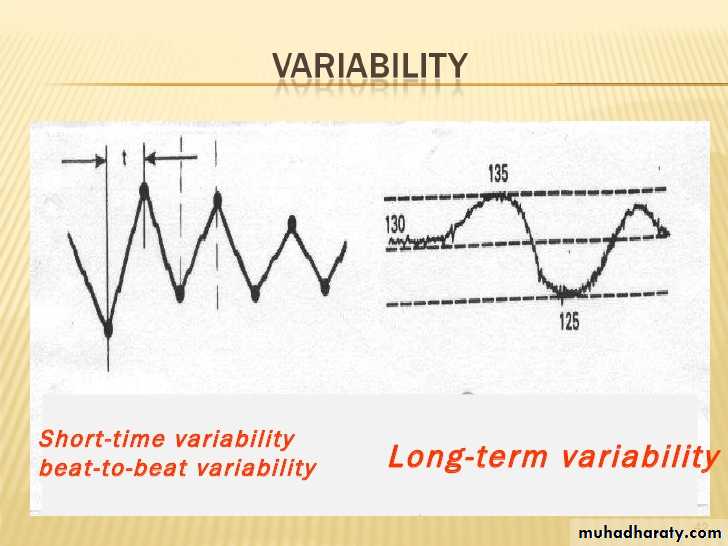
Baseline variability is defined as fluctuations in the fetal heart rate and result in the waviness of the baseline. Two forms of variability;short term variability is measured by the variation in the beat-to-beat interval (R-R interval in fetal ECG) measured by internal fetal electrode.
long term variability, evaluated as the average difference between the highest and lowest rates during a one-minute portion of the CTG trace.
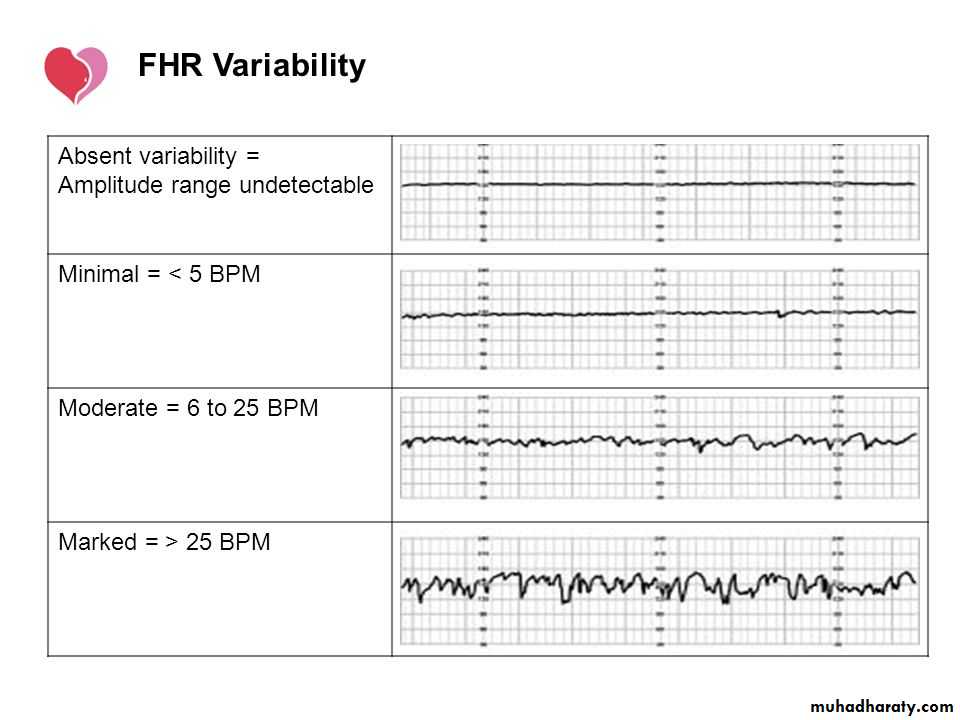
Types of variability: -
Normal variability (moderate variability): a bandwidth amplitude of 5-25 bpm, which reflect normal fetal autonomic nervous system.Reduced variability (minimal variability): variability amplitude below 5 bpm
Absent variability: Amplitude range undetectable
Marked variability: > 25 bpm.
Causes of reduced variability:
Fetal sleeping (commonest 20-30 minutes)
Hypoxia\acidosis, which result in decreased sympathetic and parasympathetic activity.
Gestational age <30 weeks
Parasympathetic blockers
Maternal sedation (opioids and hypnotics)
Accelerations:
Abrupt increase in FHR above the baseline of more than 15 bpm in amplitude, and lasting more than 15 seconds but less than 10 minutes.Presence of 2 or more accelerations on 20-30 minutes CTG trace means reactive and good sign of fetal health.
The absence of accelerations in an otherwise normal CTG is of uncertain significance because accelerations rarely occur during fetal sleep.
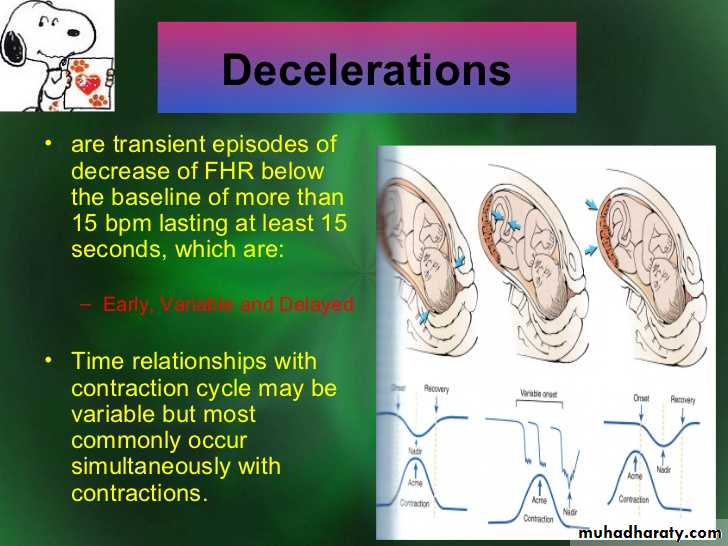
Decelerations:
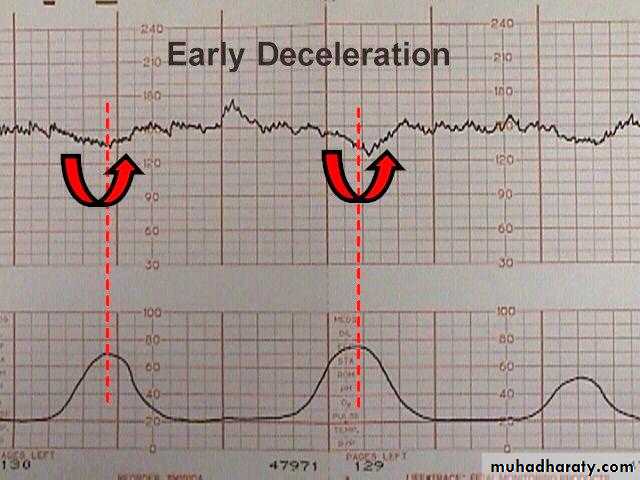
Decreases in the FHR below the baseline of more than 15 bpm in amplitude, and lasting more than 15 seconds. 4 types:-Early decelerations:
Decelerations that are shallow, short-lasting and are coincident with contractions. They are believed to be caused by vagal stimulation from fetal head compression (physiological) and do not indicate fetal hypoxia\acidosis.
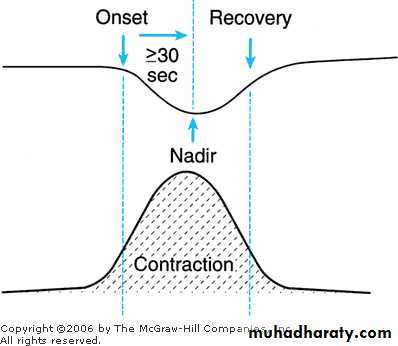
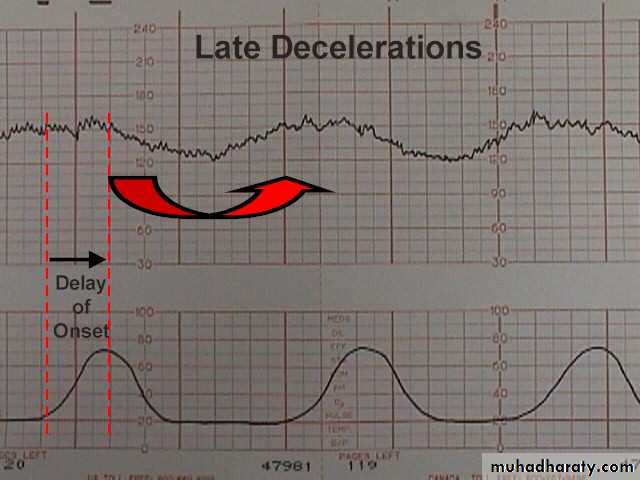
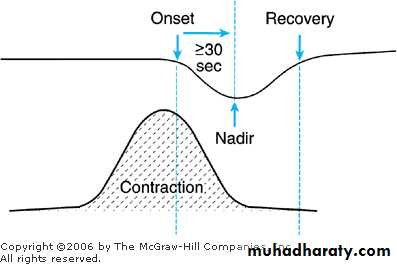
Late deceleration ( U-shaped):
Decelerations with a gradual onset and\or a gradual return to the baseline (> 30 seconds). Late decelerations start after the peak of contraction, and return to the baseline after the end of contraction.
Late decelerations are indicative of a chemoreceptor-mediated response to fetal hypoxia (due to reduction in O2). Causes:
Fetal compromised (IUGR)
Reduced placental blood flow (abruption, uterine hyperstimulation)
maternal hypotension (supine, epidural analgesia)
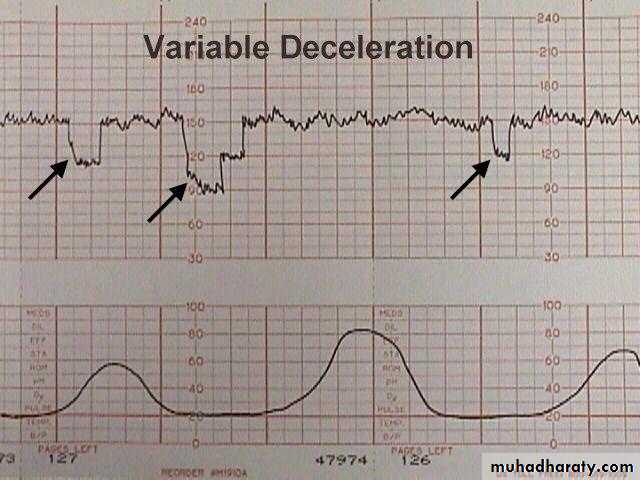
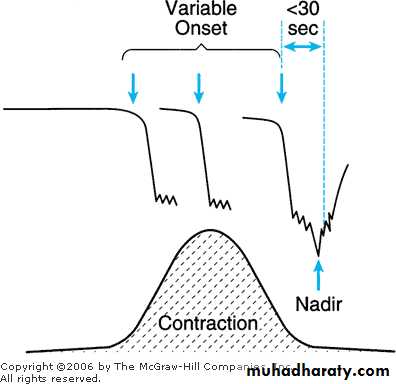
Variable deceleration:
decelerations that exhibit a rapid drop, rapid recovery to the base line, varying in size, shape, and relationship to uterine contractions.Variable decelerations constitute the majority of deceleration during labor attributed to umbilical cord compression:- (oligohydramnios, true knot, cord prolapse, cord around the neck, and cord entanglement)
Types of decelerations and their common causes
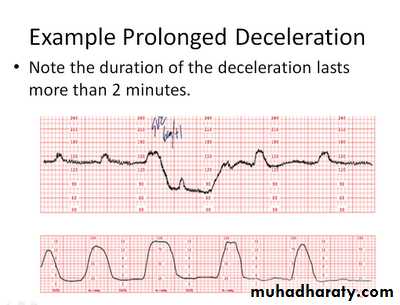
Prolonged decelerations:An isolated deceleration greater than 15 bpm lasting more than 2 minutes but < 10 minutes. These are likely indicate hypoxemia\acidosis, and require emergent intervention.
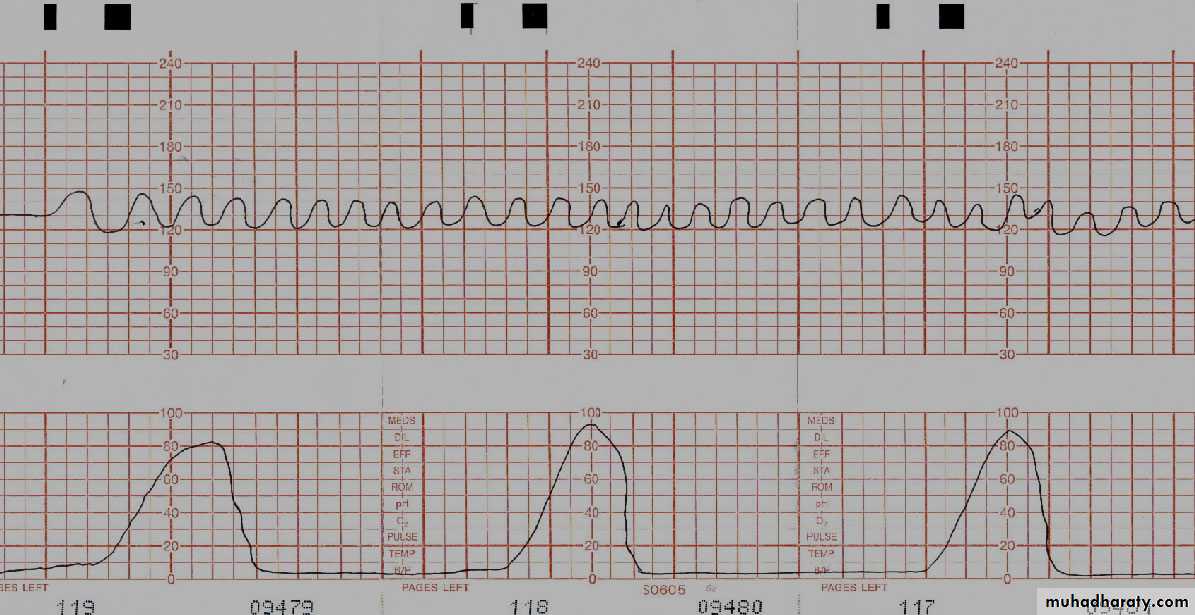
Sinusoidal Pattern:
A regular, smooth, undulating signal, with an amplitude of 5-15 bpm, and a frequency of 2-5 cycles per minute. This pattern lasts more than 20 minutes, and coincides with absent accelerations.The pathophysiology basis of sinusoidal pattern are:
Severe fetal anemia, as is found in:
● Rh isoimmunization
● Feto-maternal hemorrhage
● Twin-to-twin transfusion
● Rupture vasa Previa
Hydrocephalus and gastroschiasis
Fetal hypoxia
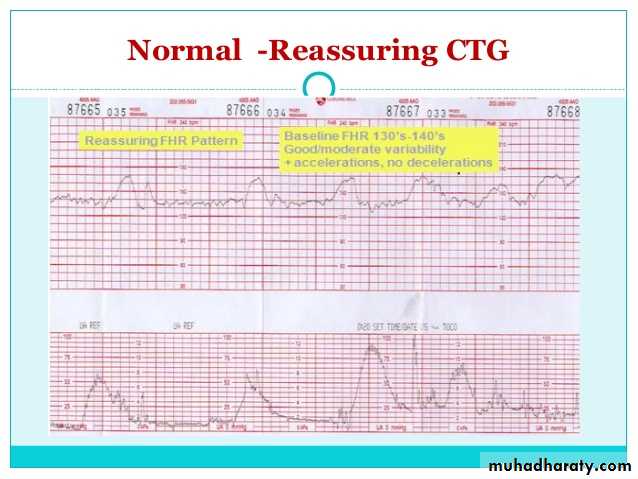
Classification of intrapartum CTG
Normal CTG:- include all the followingBaseline rate 110-160 bpm
Baseline variability 5-25 bpm
+\- Accelerations
+\- Early deceleration
No late or variable deceleration
Suspicious CTG\equivocal: presence one of the following:
Baseline heart rate 160-170 bpm or 100-110 bpmReduced variability <5 bpm for >40 minutes (> 40 minutes means beyond fetal sleep time)
sporadic Late decelerations
Uncomplicated Variable deceleration (depth <60 bpm, duration <60 seconds)
A combination of 2 or more of these factors results in abnormal (pathological) CTG
Abnormal CTG\ Ominous:
Absent baseline variability + any of the following:
recurrent late decelerations,
recurrent variable decelerations,
abnormal baseline (>170, <100 bpm)
Prolonged bradycardia
Sinusoidal pattern
Complicated variable decelerations (>60 bpm, >60 seconds)
Management with suspicious CTG:
Turn onto left lateral position: minimize aortocaval and umbilical cord compression
IV fluid
Facial oxygen
Stop oxytocin
Tocolytics, e.g., terbutaline, magnesium sulfate.
Management of abnormal CTG: or asphyxia
All the above measures +
Confirmed by internal fetal monitoring.
Fetal scalp sampling and PH
If FHR not restored to normal within 30 minutes, then prompt delivery and CS.
Fetal blood sampling: small cut in the scalp and collect the blood by microtube. Normal fetal PH > 7.25:
If PH between 7.2 and 7.25 then repeated within 30 minutes
If < 7.2 repeat immediately
If still low deliver by CS.