Genus Mycobacterium
Presented by :D. Zena Makki Alyouzbaky
Ms.C in Medical Microbiology
Genus Mycobacterium
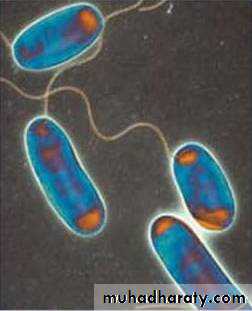
The mycobacteria are rod shaped bacteria,that do not form spores.Although they don’t stain readily, but once stained they resist decolonization by acid or alcohol and are therefore called (acid- fast bacilli).
There are 125 spp of genus mycobacterium, many of them are saprophytes.
Claassification of Mycobacteria:
I- Mycobacterium Tuberculosis Complex ( MTC) :
1-Mycobacterium tuberculosis.
2-Mycobacterium bovis.
3-Mycobacterium africanum.
II-Mycobacterium Other Than Tuberculosis:(MOTT) or tuberculoid bacilli (atypical mycobacteria):
1-M.avium-intracellular complex:
2-M.kansasi.
3-M.scrofulaceum.
4- M.marinium, M.ulcerans.
III-Rapid grower Mycobacteria:
(M.fortuitum-Chelonae complex).
IV-M.leprae: they are strict pathogens cause leprosy and cannot be cultured in vitro.
V-Saprophytic Mycobacterium.
M.tuberculosis:(tubercle bacilli):Microscopical appearance:
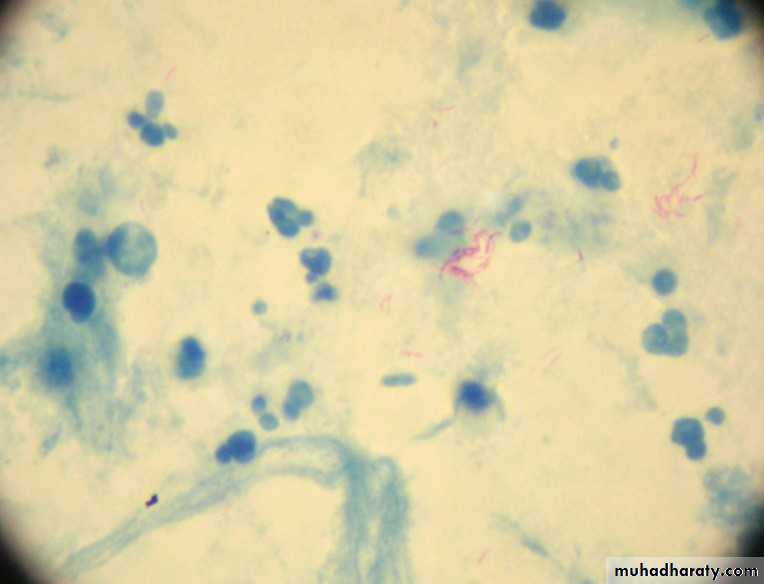
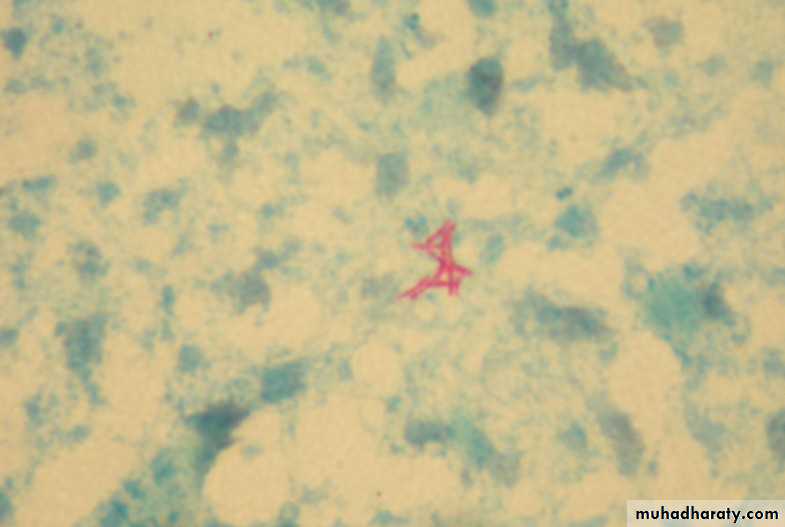
It is long, slender, tapered at the ends, straight or slightly curved or bent (curved),slender rods of 2-4µ length 0.2-0.4 µ width , not stained by Gram stain but stain red by Ziehl-Neelsen stain method .
Staining may be irregular with granules appearing darker than other parts of bacterial cells.
The bacilli appear red in sharp contrast to the blue counter stained background.
if smear is prepared from culture the bacilli appear short, thick and tend to arranged in a sort of bundles (cord formation).
Cultivation of Mycobacteria:
Mycobacteria need special media for growth & there are three types of culture media for cultivation:1-Agar base media (oleic acid albumin media) e.g. Dubos medium and Middle brook 7H10, these media used for the observation of the colonies morphology & used for susceptibility test.
2-Egg-base media:
Lowenstein Jensens medium (L-J medium) & Stonebrink s medium, contain defined salt, glycerol & complex organic material in form of fresh egg, egg yolk, potato flour & other ingredient in various combinations.
Malachite green is included in the media to inhibit other bacteria .
This media used for primary isolation of Mycobacteria because they need small inoculum size.
3-Liquid media:
These media enriched with either ascitic fluid or bovine albumin fraction V.e.g. Sula medium.
L-J media
Growth characteristics:
M.are obligate aerobesIncrease CO2 tension enhances growth
Incubation at 37C for up to 8 weeks ,because growth rate of M.is much slower than other bacteria .
Saprophytic M.,tend to grow more rapidly (<7days)& to proliferate well at (22-33C) & to produce more pigment &to be less acid fast than pathogenic one.
According to the growth rate on culture media mycobacteria can be classified into:
1. Slow grower: Need more than 7 days to grow & these slow grower can be differentiated according to the type of the growth on solid mediae.g. Egg base media:(L-J media):
M.tuberculosis that need 2-3 weeks to grow & growth describe as tough, rough, easily detach from the surface of the culture media creamy colonies, (Eugonic growth)
M.bovis need 5-6 weeks to grow & the growth describe as (dysgonic growth) with easily emulsify adhere to the surface & have smooth surface.
2. Rapid grower: need less than 7 days to grow & the colonies appear with in few days.
e.g. M.fortuitumMycobacterium tuberculosis on culture media (eugonic growth)
MOTT can be differentiated according to the pigment production in relation to the light exposure , here we have three groups:
Photochromogen: forming yellow pigments after exposure to light, e.g. (M.kansasi)
Scotochromogen: a yellow pigment will be formed in the dark, which change to red after exposure to light. e.g.(M.scrofulaceum).
Non-chromogen: non pigmented slow grower mycobacteria under all conditions of incubation.
e.g. (M.avium-intracellular) complex
Saprophytic Mycobacterium: these mycobacterium are found free living & not associate with human disease
(M.pheli,M.gordonae,& M.smegmatus),first two species present in plants , water, soil, while the third one present in the sebaceous secretion of the human beings.
Reaction of M.to chemical &physical agent
M .are more resistant to chemical agent than other bacteria because of the hydrophilic nature of the cell surface &their clumped growth, so malachite green & A.B like penicillin could be incorporated in the media without inhibiting tubercle bacilli.M.can survive in acids& alkalies these can be used to decontaminate clinical specimens
Mycobacteria resist dryness & can survive for long period in dried sputum.
Constituents of tubercle bacilli
A- Lipids :Mycobacterial cell wall is rich in lipids in form of mycolic acid (long chain fatty acids C78-C90) ,waxes & phosphatides, Can cause(granuloma formation). Lipids are to same extent responsible for acid fastness & their removal by hot acids destroy acid fastness which depends on both integrity of cell wall & presence of lipids .
Analysis of lipids by (gas chromatography) aid in classification of different species.
B- Proteins :
Each type of mycobacterium contains several proteins that elicit tuberculin reaction .
(protein bound to wax ) fraction can up on injection induce tuberculin sensitivity & they can also elicit the formation of variety of antibodies.
• C- Polysaccharides
Mycobacteria contain variety of polysaccharides. They can induce immediate type of hypersensitivity reaction & can serve as antigens in reaction with sera of infected persons.
Pathogencity of mycobacterium :
M.tuberculosis & M.bovis are equally pathogenic for human.
Rout of infection:
Inhalation of mycobacterium in droplets reach the alveoli & cause pulmonary T.B.
Ingestion of contaminated poultry products with M. bovis . Lead to cervical & mesenteric lymphadenitis.
Prolonged contact with activly infected persons is needed to get infection
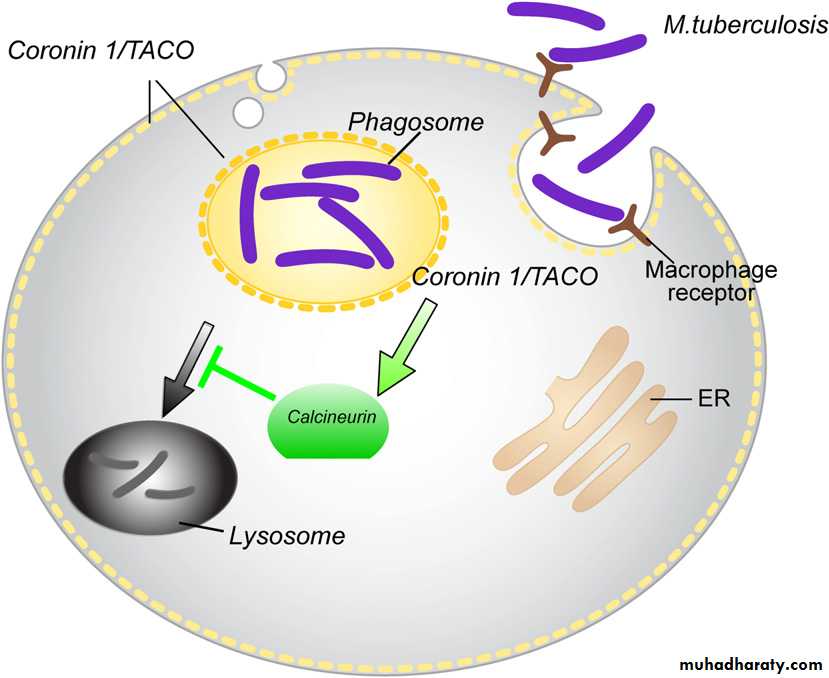
After inhalation MO escape from the defence mechanism of bronchi because of their small size and go to the terminal alveoli where they are engulphed by microphages and multiply and remain latent for long peroid.
MTC prefere hilar lung tissue because of their
high oxygen tention
Sites of TB Disease
Pulmonary TB occurs in the lungs85% of all TB cases are pulmonary
Extrapulmonary TB occurs in places other than the lungs, including the:
Larynx
Lymph nodes
Brain and spine
Kidneys
Bones and joints
Miliary TB occurs when tubercle bacilli enter the bloodstream and are carried to all parts of the body
Stages of MTB infection are divided into:
1.Latency
2.Primary disease
3.Post-primary (adult active-type)disease
4.Extrapulmonary disease
Latent TB:
Infected persons do not show any signs or symptoms.They are not infectious.
chest radiographs that do not reveal any abnormalities or signs of healed TB disease
Represent a vast and significant reservoir of potential disese. However, if they are identified, they can be treated by chemoprophylaxis.
LTBI can be successfully eradicated in the majority of patients Therefore, the accurate detection and adequat treatment of LTBI are fundamental element needed to reduce the incidence of tuberculosis, particularly among high risk population
Primary TB
Initially infection with M involve middle &lower lung field &the focus is usually single .cell mediated immunity develops in the healthy person controlling the infection &cause the patient to remain asymptomatic .
Scar of the (primary complex focus of infection + satellite L. adenopathy) may calcify & the bacilli in the lesion slowly die although few may remain viable for years.
Post-primary (adult active-type)disease
A-as progression of 1ry infection:If the tubercle bacilli not controlled at site of infection , phagocyte bacilli will diffuse through lymphatic & blood stream to any organ of the body , apex of lung , kidney , bones & bone marrow ,L.N, brain ,meninges &intestine.
B-Reactivation of latent infection: May occur 20 yrs or longer after the 1ry infection following deterioration of immune resistance to M.tuberculosis.
Disseminated (miliary) T.B
It is characterized by numerous small graunulomatous tubercle.
Very young or elderly individuals & immuno compromised patients are mostly affected.
Laboratory diagnosis of Mycobacterium:
Spesmin collection and processing:
Contaminated specimens: sputum, stool (in AIDS pat) gastric fluid, urine early morning.
Sterile specimen: CSF, blood, joint aspirate.
Processing of specimens:
Digestion and decontamination agents and concentration.
• 2. Staining using Ziehl Neelsen stain (hot stain), Kinyoun stain (cold stain) and fluorochrome procedure (auramin, rodamin) which is more sensitive mo appear orange.
• 3. Culture usually using 3 media 2 L J media and MB 7H10. Incubation at (35-37 C)in 5-10% CO2 for up to 8 weeks. If cultures are negative in the presence & positive acid – fast stain or slowly growing atypical M. cultures should be incubated at a lower temp (24-33C) for 12 weeks .
• 4. Differentiation between species of mycobactria Is done by:
conventional methods for identification of mycobacteria include observation of growth rate, colony morphology, pigmentation, biochemical profiles. These methods require (6-8 weeks) for identification.Molecular probe: provide rapid, sensitive, specific method to identify mycobacteria.
DNA fingerprinting .
PCR has (55-90%) sensitivity with 99% specificity
Cont.....DX
5. Tuberculin Test :1-it is delayed hypersensitivity reaction to M. Tuberculosis antigens. -(PPD) (purified protein derivative)
The test is considered positive if the injection 0.1 ml is followed by indurations (15mm)or more in diameter. The skin test should be read in (48-72)hours. Positive test tend to persist for several days while weak reactions may disappear rapidly.
-Tuberculin skin test (TST) may be negative in the presence of tuberculosis infection when (anergy) develops due to over whelming T .B , measles ,Hodgkin's disease , sarcoidosis ,AIDS or immuno suppression .
-A positive tuberculin test indicates that an individual has (been infected in the past & continue to carry viable mycobacteria) but it does not mean that active disease or immunity to the disease is present.
CONT......DX
Furthermore, some people infected with MTB may have a negative reaction to the TST if many years have passed since they became infected. They may have a positive reaction to a subsequent TST
Because the initial test stimulates their ability to react to the test. This is commonly referred to as the “booster phenomenon”and may incorrectly be interpreted as a skin test conversion (going from negative to positive). For this reason, the “two-step method” are recomende for TST.
If the first TST result in the two-step baseline testing is positive, consider the person infected and evaluate and treat the person accordingly. If the first test result is negative, the TST should be repeated in 1–3 weeks. If the second test result is positive, consider the person infected and evaluate and treat the person accordingly; if both steps are negative, consider the person uninfected and classify the TST as negative at baseline testing
Cont.....DX
6. Interferon Gamma Releasing Assays (IGRAs) The recently developed IGRAs are in vitro tests designed to detect immune response to specific MTB antigens which are not present in the BCG or certain non- tuberculous mycobacteriumTwo tests are commercially available T-SPOT TB and the other QFT-GIT (Quantiferon gold in tube )
Treatment:
Simultaneous administration : of at least 2 drugs to avoid the emerge of resistant strain of -M.tuberculosis . Treatment should be continued for several months.1st line anti T.B drugs : Isoniuazid (INH), Rifampicin , ethambutol, pyrazinamide & streptomycin.
2nd line antiT.B: Kanamycin ,cycloserine, ciprofloxacin, ofloxacin, ethionamide, , rifabulin , riomycin .
Standard 9 months regimens are based on INH &rifampicin given daily.
Prevention & control :
1-Effectine treatment of patients with active T.B & follow up.2-Drug treatment of asymptomatic tuberculin positive persons in age group who are more prone to develop complication (e.g children).
3-Immunization : BCG
4-The eradication of T.B in cattle& pasteurization of milk have greatly reduced M.bovis infection.
Legionella
• A naturally occurring bacterium
• Found in most water systems
• Often present in mains water
• Easily colonises most domestic water systems – hot and cold
• G negative bacilli
Requirements for Growth?
• Optimum temperature range of 20 - 45 ⁰C• Food source (other bacteria & sediments)
• Prefers stagnant conditions
Route of Infection?
• Primarily through inhalation of aerosols, fine droplets & mists• Can be contracted by choking on contaminated water
• Statistically most susceptible
• - 50 to 70 year olds
• - Males
• - Smokers
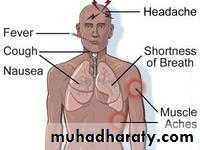
Legionnaire’s Disease
• Potentially fatal form of pneumonia –• 5-30% fatality rate
• Incubation period 2-10 days ( typically 3-6days ).
•
Treatment
• Monitor temperatures; 20-45⁰C = risk range• Every 2 weeks - heat water to 60⁰C for 5 mins
• Add disinfectants / Chloros as advised
• Empty out the water system, thoroughly clean & refill with fresh water every month
• Clean & disinfect spray heads every month
• Flush rarely-used outlets weekly