1
Fifth stage
Medicine
Lec-3
.د
فاخر
26/11/2016
RHEUMATOID ARTHRITIS
Treatment
Goal of treatment
reduce inflammation and pain,
preservation of function,
prevention of deformity.
Pharmacological therapy
*simple analgesic drugs
*NSAIDs
*Topical creams
*Opioid analgesics
*Amitriptylin:
'disease-modifying antirheumatic drug' ((DMARD
*Corticosteroids
Local injections
Surgery
2
General Principles
Undelayed use of DMARDs
The major goal is full remission
Remission is infrequent with a single DMARD
DMARDs combinations can add benefits with little or no increase in adverse effects
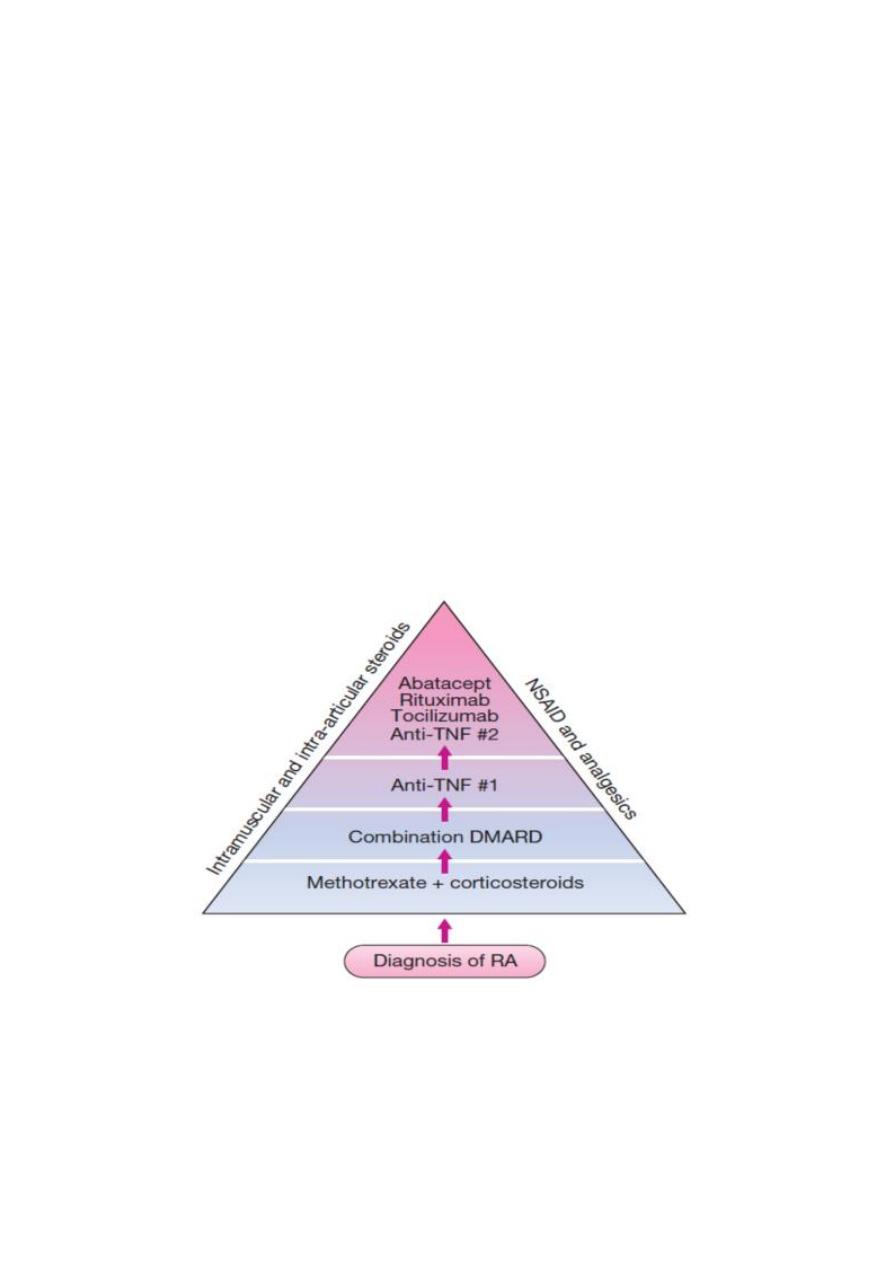
The mainstay of treatment in RA comprises the earlyuse of small-molecule disease-
modifying antirheumaticdrugs (DMARDs), and corticosteroids for induction of
remission.
There is evidence that early use of DMARDtherapy improves clinical outcome in RA. Partial
or nonresponseto DMARD therapy should prompt escalationof the dose or use of an
additional DMARD, with progressionto biological drugs if necessary
3
SIMPLE ANALGESIA
Paracetamol (1 g 6-8-hourly) is the oral analgesic of choice because of its efficacy, lack of
contraindications or drug interactions, long-term safety, low cost and availability.
Paracetamol inhibits prostaglandin synthesis centrally in the brain but has little effect on
peripheral production of prostaglandins
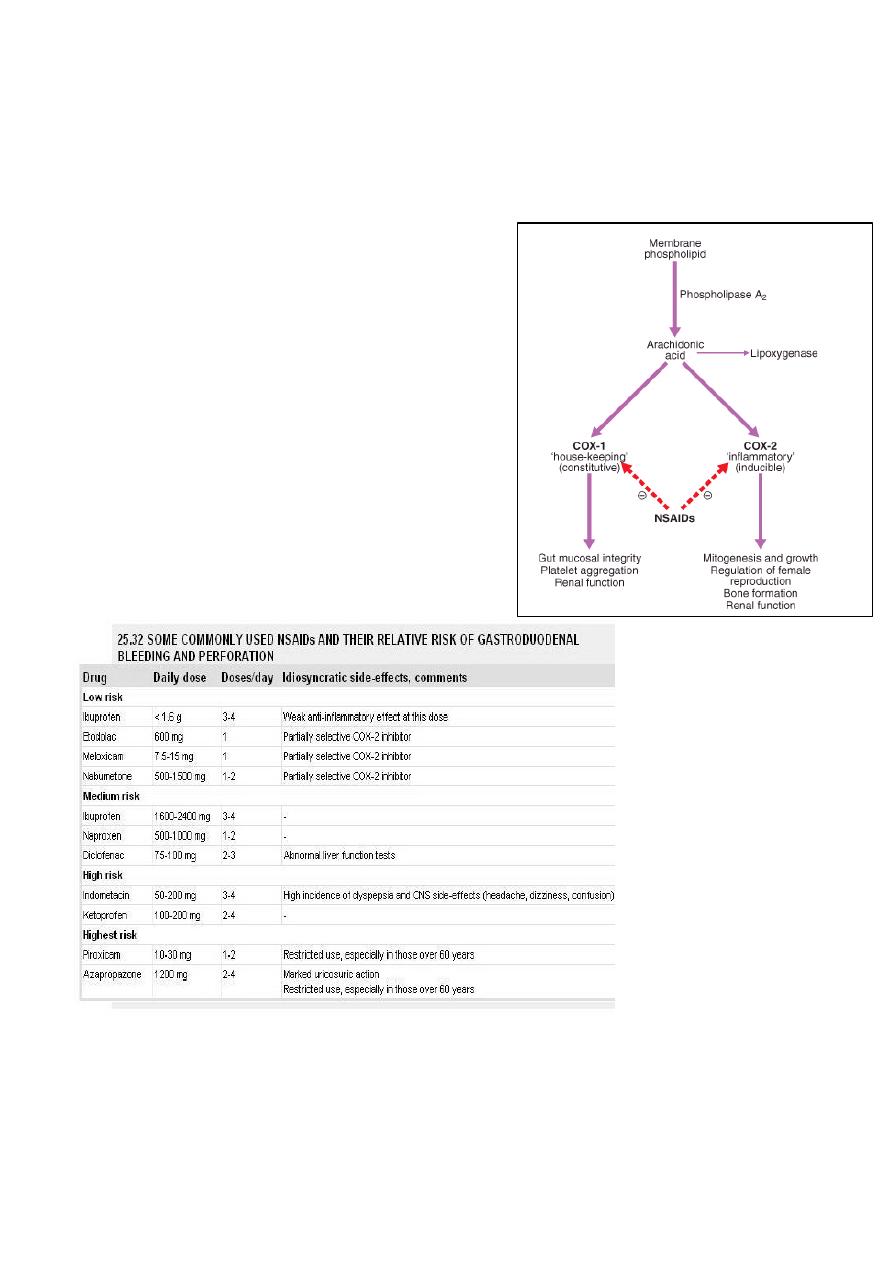
NON-STEROIDAL ANTI-INFLAMMATORY
DRUGS (NSAIDS)
These are among the top five most prescribed drugs
in many countries. Oral NSAIDs are often effective
for the pain and stiffness of inflammatory disease.
Long-acting NSAIDs given at night are particularly
helpful for marked inflammatory early morning
stiffness. NSAIDs may also reduce bone pain due to
secondary malignant lesions.
The major drawback of NSAIDs is gastrointestinal toxicity. Prostaglandins of the E series
play a major role in gastroduodenal defence mechanisms. By depleting mucosal
prostaglandin levels, aspirin and NSAIDs impair this 'cytoprotection', resulting in mucosal
injury, erosions and ulceration. NSAIDs are an important aetiological factor in up to 30% of
gastric ulcers.
4
IMPACT OF NSAID-INDUCED GASTRIC BLEEDING
Endoscopic evidence of peptic ulceration is found in 20% of NSAID users even in the
absence of symptoms
1% of patients with RA or OA are hospitalised each year with gastrointestinal bleeding
Annual mortality in people in the US and in the UK higher than deaths from diseases such as
myeloma, asthma, cervical cancer or Hodgkin lymphoma
RISK FACTORS FOR NSAID-INDUCED ULCERS
*Age > 60 years
*Past history of peptic ulcer
*Past history of adverse event with NSAIDs
*Concomitant corticosteroid use
*High-dose or multiple NSAIDs
*Individual NSAID-highest with piroxicam, ketoprofen; lower with ibuprofen
PRINCIPAL INDICATIONS FOR ORAL OR PARENTERAL CORTICOSTEROID
1-For rapid, short-term (1-3 months) control of marked synovitis or systemic inflammation
while awaiting efficacy from slow-acting antirheumatic agent
2-For life-threatening (e.g. vasculitis) or organ-threatening (e.g. kidney, lung, eye)
inflammatory multisystem disease
3-For primary treatment of polymyalgia rheumatica
4-For control of inflammatory disease during pregnancy

5
CORTICOSTEROIDS IN RHEUMATOID ARTHRITIS
Systemic corticosteroids have disease-modifying activity, but their primary role is in the
induction of remission in patients with early RA who are starting synthetic DMARD
treatment.
Various regimens have been usedbut there is little evidence to suggest that one is superior
to another.
One strategy is to give a high dose oforal prednisolone initially (60 mg daily) and to reduce
and stop this gradually over a period of 3 months as theDMARD starts to take effect.
LOCAL INJECTIONS
Intra-articular corticosteroids are primarily indicated when there are one or two ‘problem
joints’ with persistent synovitis despite good general control of the disease. Although
corticosteroids are very useful, they alsohave significant adverse effects (p. 776). In the
contextof RA, osteoporosis is probably the most importantsince this is a known
complication of RA, even in the absence of corticosteroid therapy. Accordingly DEXA
scanning followed by bone protection should be considered in any patient with RA who is
expected to be on more than 7.5 mg prednisolone daily for more than 3 months
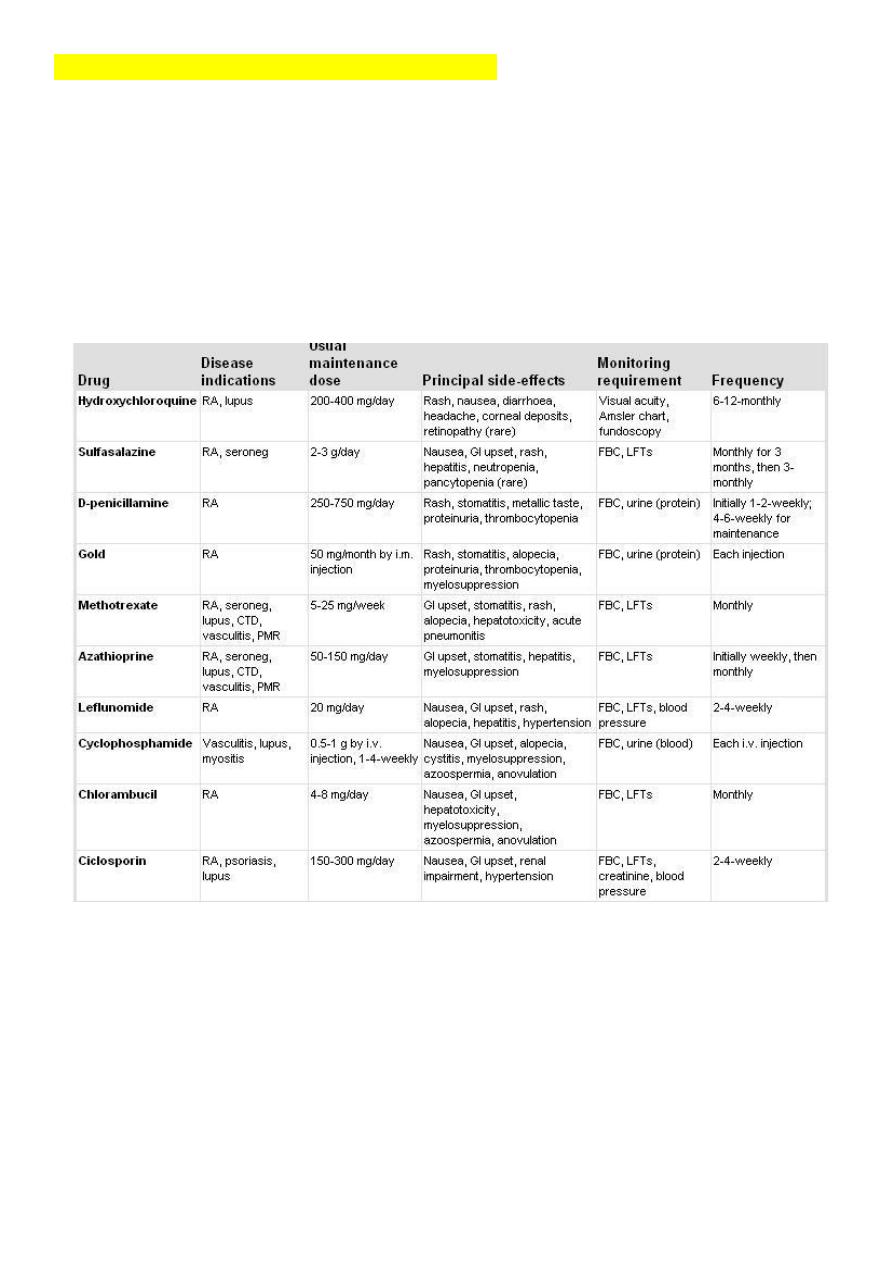
Disease-modifying antirheumatic drug "DMARDs"
Classification of DMARDs
1-Non-Immunosuppressive agents (“joint effective agents”)
2-immunosuppressive agents (“joint & systemic effective”)
3-Biological agents
6
1-Non-Immunosuppressive agents (“joint effective agents”)
Sulfasalazine
Hydroxychloroquine
Gold salts (e.g. sodium aurothiomalate)
D- penicillamine
2-immunosuppressive agents (“joint & systemic effective
Methotrexate
Azathioprine
Leflunomide
Ciclosporine
Other cytotoxic drugs
Methotrexate
Methotrexate is the anchor DMARD in RA. It is usually given as a starting weekly oral dose
of 7.5–10 mg and this is increased in 2.5 mg increments every 2–4 weeks until benefit
occurs or toxicity is limiting. The maximum recommended dose is 25 mg. The benefits of
methotrexate usually start to appear within 1–2 months but a 6-month course should be
given before concluding that it has been ineffective.
The most common adverse effects
are nausea, vomiting and malaise within 24–48 hours ofadministration.
Patients who experience these can sometimes be successfully treated with subcutaneous
methotrexate.
Folic acid (5 mg/week) reduces the incidence of adverse effects without reducing efficacy.
7
Cyclophosphamide, azathioprine, and cyclosporine
are immunosuppressive drugs that are effective agents in treating RA. In addition to the risk
of both common and unusual infections, cyclophosphamide carries a risk of bladder and
late lymphoid malignant disease; the latter risk may also be present with azathioprine.
Among the oldest of are gold salts. Given as weekly injections, gold thiomalate or
thioglucose is effective in controlling disease in many patients; a few patients go into true
and complete remission. However, many patients experience side effects, including bone
marrow suppression, glomerulonephritis, and rash.
8
3- Biological Treatment (Anticytokines)
These drugs are more effective than standard DMARDs (with a faster onset of action,
greater clinical efficacy and sustained benefit) but because of their cost many countries
have set restrictive guidelines for their use.
Current UK recommendations are that they should be initiated only in active RA when an
adequate trial of at least two other DMARDs (including methotrexate) has failed.
1- Anti-TNF therapy (Infliximab)
is the first-line biological drug in RA.
Several agents are available.
With the exception of infliximab, which must be prescribed with methotrexate to reduce
the risk of neutralizing antibodies developing, these agents can be used as monotherapy. In
clinical practice, however, most are co-prescribed with methotrexate, as this is more
efficacious.
The main adverse effects are serious infections and reactivation of latent tuberculosis
2- Competitively blocks binding of IL-1 to its receptor (Anakinra)
3- Monoclonal antibody that binds CD20 antigen on B-cells surface (Rituximab)
EXAMPLES OF COMMON USEFUL SURGICAL PROCEDURES FOR MSK DISORDERS
Soft tissue release decompression
Carpal tunnel(Median nerve) compression
• Synovectomy
• Joint replacement arthroplasty
• Arthroplasty
